Abstract
Study Objectives:
The purpose of this study was to examine whether or not insomnia symptoms were associated with measured dyslipidemia.
Methods:
This was a population-based multiyear cross-sectional study, using data from 2005–2008 United States National Health and Nutrition Examination Surveys. Survey participants ages 20 y and older self-reported the frequency of difficulty falling asleep, prolonged nocturnal awakening, and undesired early morning awakening over the preceding month. One-time venipuncture was performed and a low-density lipoprotein cholesterol (LDL-C) of ≥ 160 mg/ dL, triglycerides of ≥ 200 mg/dL, and a high-density lipoprotein cholesterol (HDL-C) of < 40 mg/dL denoted dyslipidemia. Descriptive statistics and multiple logistic regression were used.
Results:
Data on LDL-C, triglycerides, and HDL-C was available for 4,635, 4,757, and 9,798 individuals, respectively. There were no significant associations between having any insomnia symptom at least five times in the past month and high LDL-C (odds ratio [OR] 1.20, 95% confidence interval [CI] 0.92–1.55) or low HDL-C (OR 0.92, 95% CI 0.82–1.04) in unadjusted analyses, or with high triglycerides after adjusting for covariates (OR 1.03, 95% CI 0.78–1.37). Recipients of sleeping pills who also had insomnia symptoms had significantly increased adjusted odds of elevated LDL-C (OR 2.18, 95% CI 1.14–4.15).
Conclusions:
Insomnia symptoms were generally not associated with dyslipidemia, but receipt of sleeping pills in the setting of insomnia was associated with elevated LDL-C. Further research is needed to confirm a possible link between sleeping pill use and dyslipidemia and to delineate if an association with atherosclerosis exists with specific types of sleeping pills or with all sedative medications more broadly.
Citation:
Vozoris NT. Insomnia symptoms are not associated with dyslipidemia: a population-based study. SLEEP 2016;39(3):551–558.
Keywords: insomnia, lipids, sedatives, sleep, population health
Significance.
Although some previous studies have reported that insomnia symptoms are associated with cardiovascular disease, this large, population-based study generally found no association between insomnia symptoms and measured dyslipidemia. No relationship between insomnia symptoms and dyslipidemia was found even when different markers of insomnia severity were considered, such as different categories of insomnia symptom frequency, the presence of concomitant daytime fatigue, and the presence of concomitant short sleep time. One notable and novel positive finding was that individuals with insomnia symptoms who were receiving sleeping pills were more likely to have elevated low-density lipoprotein cholesterol after adjusting for covariates. Further research is needed to confirm a possible link between sleeping pill use and dyslipidemia.
INTRODUCTION
Insomnia symptoms (i.e., difficulty falling asleep, prolonged nocturnal awakening, and undesired early morning awakening) are a common problem in the general population. It is estimated that insomnia symptoms occur in about 30% of the general American population five times per month or more.1–3 Insomnia symptoms are commonly chronic in duration, with well over 50% of individuals reporting ongoing symptoms years after baseline assessment.4,5 Insomnia is associated with daytime fatigue, impaired daytime functioning, and decreased quality of life.6,7
There is a growing interest among the public and health care professionals to know whether or not insomnia might also be linked to the development of cardiovascular disease.8 Although not consistently demonstrated,9–11 insomnia has been found to be associated with hypothalamic-pituitary-adrenal axis and sympathetic nervous system activation,12,13 which provides a biologic rationale for insomnia to possibly lead to the development of coronary artery disease. Some previous studies have shown that insomnia symptoms are associated with significantly increased risk of coronary artery-related events or mortality.14–20 However, many other studies have found no association between insomnia symptoms and these outcomes.21–28 Few studies have specifically evaluated for a possible link between insomnia symptoms and dyslipidemia.18,29 Zhan et al.29 reported a 25% increased odds of elevated total cholesterol level among women experiencing insomnia symptoms three or more times per week compared to women experiencing no insomnia. If a true link between dyslipidemia and insomnia symptoms exists, this would potentially support the findings of some previous studies that reported a relationship between insomnia and coronary artery-related events or mortality. Furthermore, if insomnia symptoms were found to be associated with dyslipidemia, this would have potentially important implications on the management of insomnia patients.
The purpose of this study was to evaluate for a possible association between insomnia symptoms and measured dyslipidemia using a large, population-level American database.
METHODS
Study Design
A population-based multiyear cross-sectional design was used.
Data Sources
This study combined data from the 2005–2006 and 2007– 2008 National Health and Nutrition Examination Surveys (NHANES). The NHANES is a cross-sectional survey that is undertaken in the US by the Centers for Disease Control and Prevention every 2 y and each survey sample represents the total noninstitutionalized civilian US population residing in the 50 states and District of Columbia. Sociodemographic and health information is collected from participants in person by trained professionals. Participants are interviewed in their homes and examined in a mobile examination centers where blood samples are obtained and physical examinations are performed. A detailed description of the survey design and methodology is available.30 Although NHANES databases are available prior to 2005–2006 and after 2007–2008, information on sleep health was only collected for the 2005–2006 and 2007–2008 NHANES cycles.
Identification of Insomnia Symptoms
NHANES participants were questioned regarding the frequency of difficulty falling asleep, prolonged nocturnal awakening, and undesired early morning awakening over the past month. These symptoms are contained in the insomnia definition of the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-V).31 Individuals were classified as having insomnia symptoms if they responded affirmatively to experiencing at least one of the following symptoms: difficulty falling asleep, prolonged nocturnal awakening, or undesired early morning awakening, at least five times in the past month. Although the presence of insomnia symptoms were established by self-report, clinical practice guidelines32 indicate that insomnia is primarily diagnosed by history and that polysomnography is not indicated in the routine evaluation of insomnia. Although insomnia symptom questions were asked of participants ages 16 y and older, individuals ages 20 y and older were included in this study because certain covariate data (e.g., education level, smoking, alcohol use) was only available for this age group. Nonresponse to the insomnia questions was very low (< 0.3% of participants from both survey cycles) and these individuals were excluded.
Identification of Dyslipidemia
One-time venipuncture was performed on participants and the following were measured enzymatically: total cholesterol; triglycerides; and, high-density lipoprotein cholesterol (HDL-C). A description of the laboratory measurement methodology used is available.33 Low-density lipoprotein cholesterol (LDL-C) was estimated from measured values of total cholesterol, triglycerides, and HDL for participants who underwent a morning-time fasting blood draw of at least 8.5 h or more. LDL-C was estimated according to the Friedewald calculation: [LDL-C] = [total cholesterol] – [HDL-C] – [triglycerides/5].33 Although LDL-C was calculated using the Friedewald equation, and not directly measured itself, this approach is commonly used in the ‘real-world’ and excellent correlation has been found between Friedewald and directly measured LDL-C in nonfasting individuals (coefficient = 0.97).34 Because the Friedewald equation may not be accurate when triglycerides are ≥ 400 mg/dL, individuals with such triglyceride levels were excluded from the LDL-C analysis (i.e., n = 122 or 2.6% of combined 2005–2008 NHANES samples). Although triglyceride and HDL-C data from individuals who were not fasting were included when evaluating these two outcomes, nonfasting lipid levels have been found to have similar prognostic value as fasting ones.35,36 An LDL ≥ 160 mg/dL (equivalent to 4.14 mmol/L) and triglycerides ≥ 200 mg/dL (equivalent to 2.26 mmol/L) were selected as cutoffs to denote abnormal levels in this study, because both these lipid levels have been recognized as “high” by US national lipid guidelines.37,38 An HDL < 40 mg/dL (equivalent to 1.03 mmol/L) was selected as abnormal, because this HDL cutoff has been recognized as “low” by US national lipid guidelines.37 LDL-C, triglyceride, and HDL-C data were missing on 9.1%, 7.2%, and 9.1% of participants from the two combined NHANES cycles.
Covariates
Based on a review of the literature, variables that were potential confounders, that is, associated with both insomnia and dyslipidemia, were identified.2,3,39–41 These variables are presented in the online supplement. One specific covariate that was considered was sleeping pill use. NHANES asked the following question to survey participants: “In the past month, how often do you take sleeping pills or other medication to help you sleep?”. This question was not limited to any particular class(es) of sedatives and potentially included both prescription and over-the-counter medications. Individuals who responded affirmatively to having used any sleeping pill one time or more in the past month were classified as having received sleeping pills.
Sensitivity Analyses
Several sensitivity analyses were performed and these are described in the online supplement.
Statistical Analysis
Forced entry multiple logistic regression was used to examine the association between insomnia symptoms and high LDL-C, high triglycerides, and low HDL-C. Unadjusted odds ratios (OR) and 95% confidence intervals (CI) were first calculated. A second regression model was run for each dyslipidemia measure including the following covariates: sex, age, race, education level, total household income, ever smoking, alcohol consumption over the past year, depressed mood and anhedonia over the previous 2 w, body mass index, doctor-diagnosed hypertension, current receipt of antihypertensive medication, doctor-diagnosed dyslipidemia, current receipt of lipid-lowering medication, doctor-diagnosed diabetes, current receipt of diabetes pills or insulin, current receipt of any sleeping pill, and frequency of reported snoring and/or apneas. A third regression model was run, including all of the variables in the second model, plus frequency of reported daytime fatigue and frequency of daytime sleepiness. Because symptoms of daytime fatigue and sleepiness are included on the Berlin Questionnaire that screens for obstructive sleep apnea, and yet they may also be consequences of insomnia, they were included separately in a third regression model to evaluate for possible over-adjustment.
NHANES uses a complex sampling design, employing stratification and multistage clustering. To account for the unequal probabilities of selecting respondents, all point estimates were appropriately weighted using the survey sample weights provided. Combined new sample weights were appropriately created given that two NHANES cycles were used. To account for the effects of stratification and clustering on variance estimates, Taylor linearization procedures were performed on all confidence intervals using stratum and cluster variables provided by NHANES. All analyses were performed on SAS version 9.3. Because this study involved analysis of legally and publically accessible anonymized data, research ethics approval was not needed as per the Tri-Council Policy Statement.42 Ethics approval to conduct NHANES and documented consent from survey participants was obtained by the Centers for Disease Control and Prevention.
RESULTS
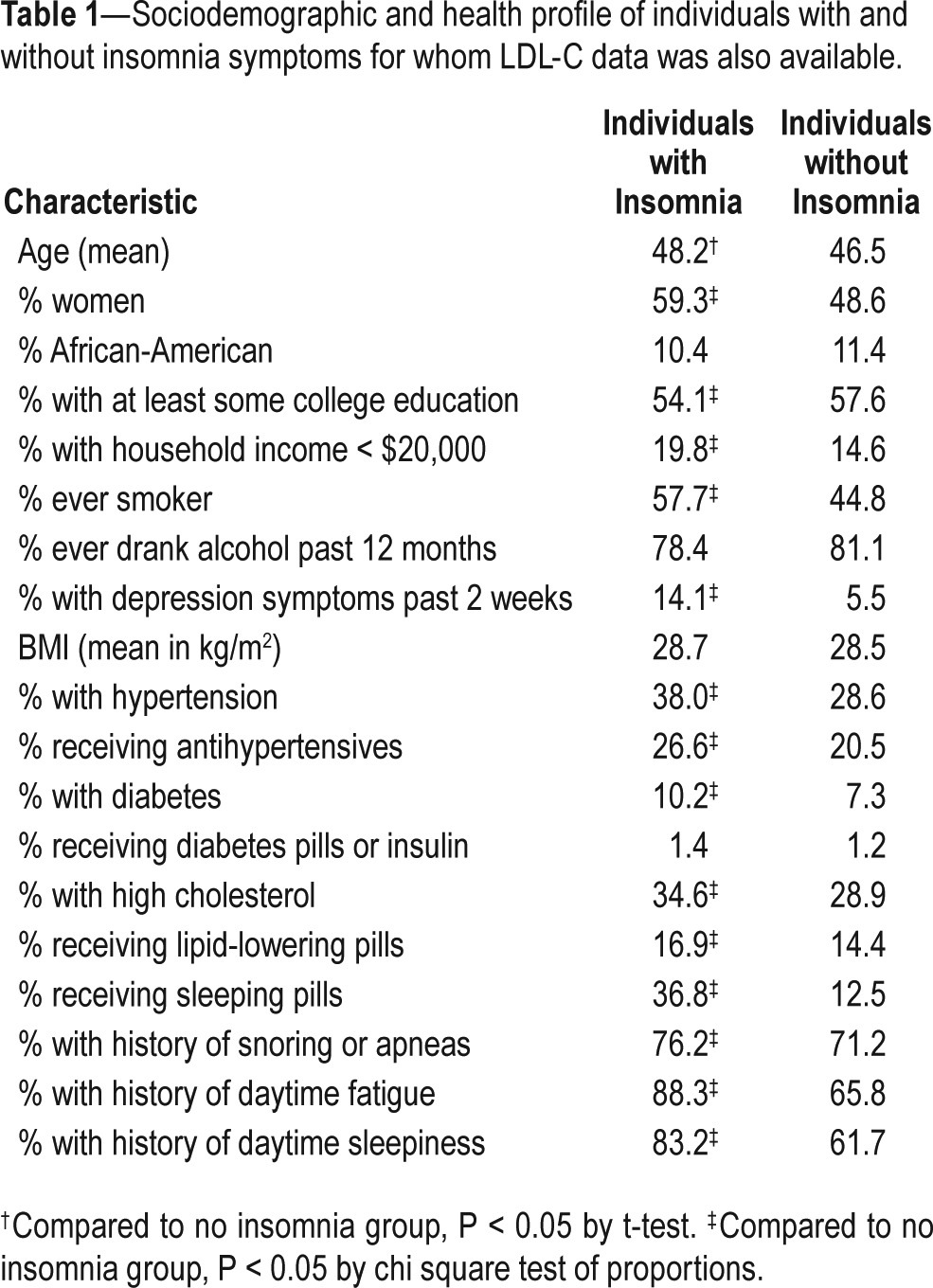
Among individuals ages 20 y and older for whom insomnia data was available, data on LDL-C, triglycerides, and HDL-C was available for 4,635, 4,757, and 9,798 individuals, respectively. From these total numbers, 10.7% had elevated LDL-C, 16.3% had high triglycerides, and 22.1% had low HDL-C. Sociodemographic and health covariate data among individuals with and without insomnia symptoms are presented in Table 1.
Table 1.
Sociodemographic and health profile of individuals with and without insomnia symptoms for whom LDL-C data was also available.
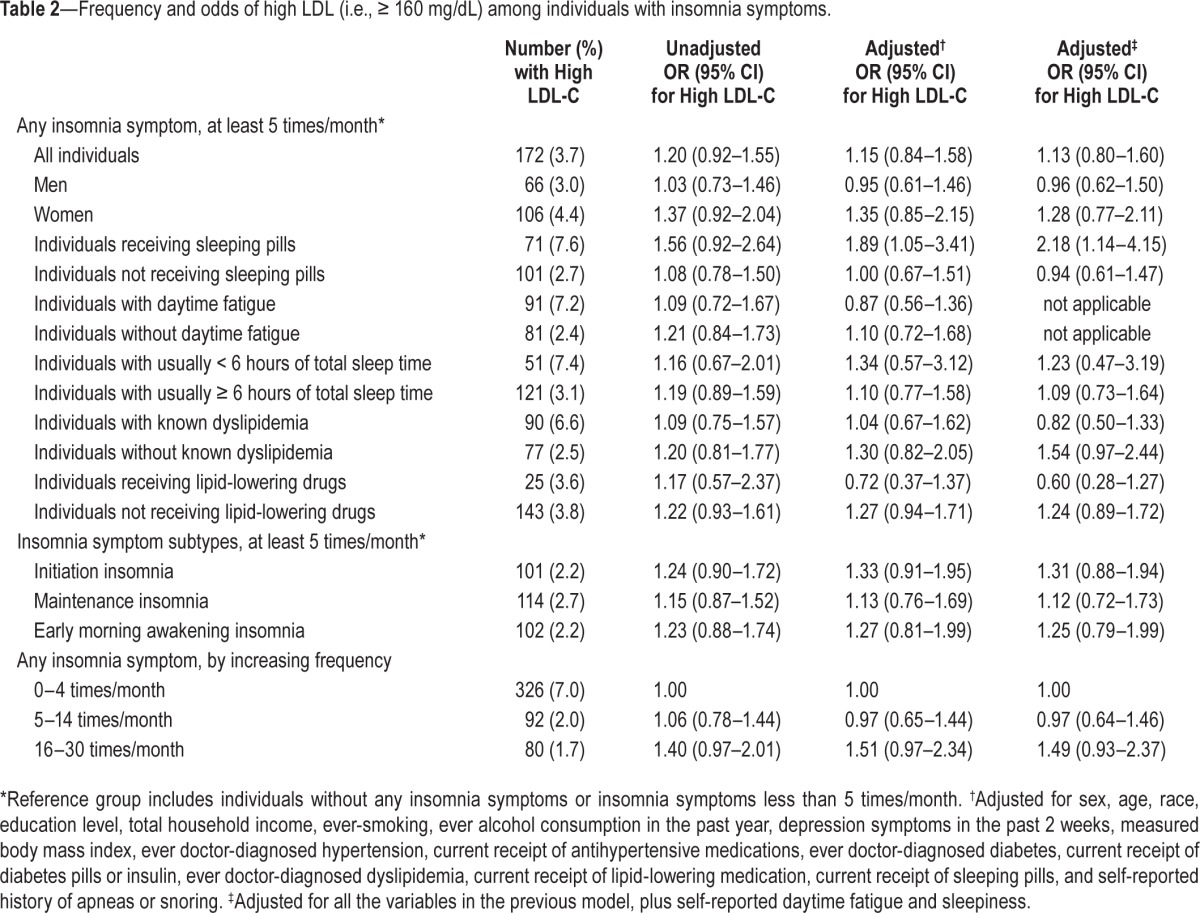
There were no significant associations between having any insomnia symptom at least five times in the past month and high LDL-C, either before or after covariate adjustment, including when distinguishing by sex (Table 2). Insomnia symptoms were not associated with high LDL-C, when distinguishing by insomnia symptom subtype or by insomnia symptom frequency. There were no significant associations between insomnia symptoms and high LDL-C, regardless of the presence or not of diagnosed dyslipidemia or the recent receipt or not of lipid-lowering medication. There were also no significant associations between insomnia symptoms and high LDL-C, regardless of the presence or not of concomitant daytime fatigue or short sleep time. Among individuals who were not receiving sleeping pills, insomnia symptoms were not associated with high LDL-C. However, among recipients of sleeping pills, there were increased adjusted odds of elevated LDL-C among those with insomnia symptoms (OR 2.18, 95% CI 1.14–4.15).
Table 2.
Frequency and odds of high LDL (i.e., ≥ 160 mg/dL) among individuals with insomnia symptoms.
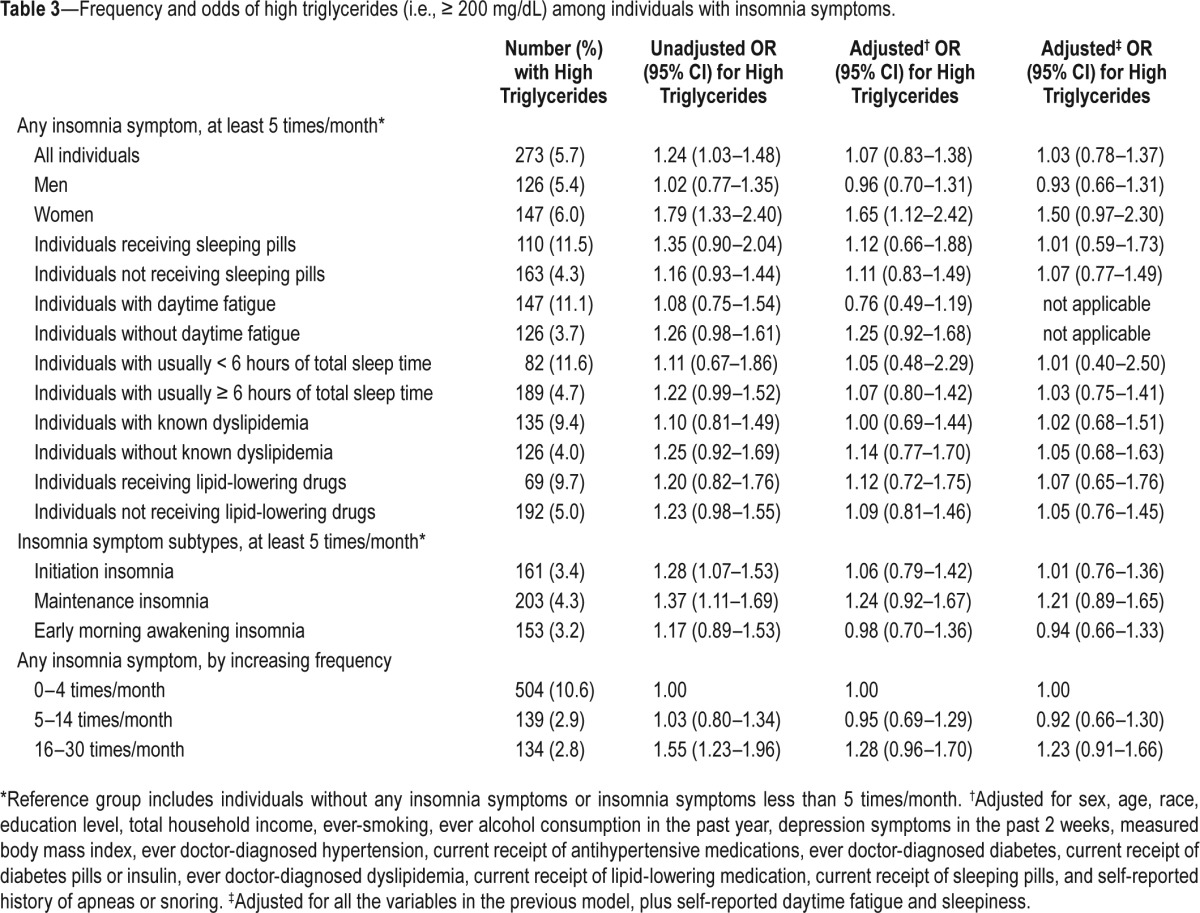
In unadjusted analyses, having any insomnia symptom at least five times in the past month was associated with increased odds of high triglyceride level (OR 1.24, 95% CI 1.03–1.48) (Table 3). However, this association became nonsignificant after adjusting for covariates (OR 1.07, 95% CI 0.83–1.38). No significant association was observed between men with insomnia symptoms and high triglycerides. Among women with insomnia symptoms, there were significantly increased odds of high triglycerides even after adjusting for covariates (OR 1.65, 95% CI 1.12–2.42), but this association was rendered nonsignificant after additionally controlling for daytime fatigue and sleepiness symptoms (OR 1.50, 95% CI 0.97–2.30). However, among the subgroup of women experiencing insomnia symptoms 16 to 30 times in the past month, there were increased odds of elevated triglycerides, even after controlling for daytime fatigue and sleepiness (OR 1.98, 95% CI 1.19–3.30). Sleep initiation insomnia and sleep maintenance insomnia were associated with increased unadjusted odds of high triglyceride level, but these associations became nonsignificant after covariate adjustment. Individuals having any insomnia symptom 16 to 30 times in the past month had increased unadjusted odds of high triglycerides, but this association also became nonsignificant after covariate adjustment. None of the remaining sensitivity analyses yielded significant results, including ones relating to the concomitant presence (or not) of daytime fatigue and short sleep time.
Table 3.
Frequency and odds of high triglycerides (i.e., ≥ 200 mg/dL) among individuals with insomnia symptoms.
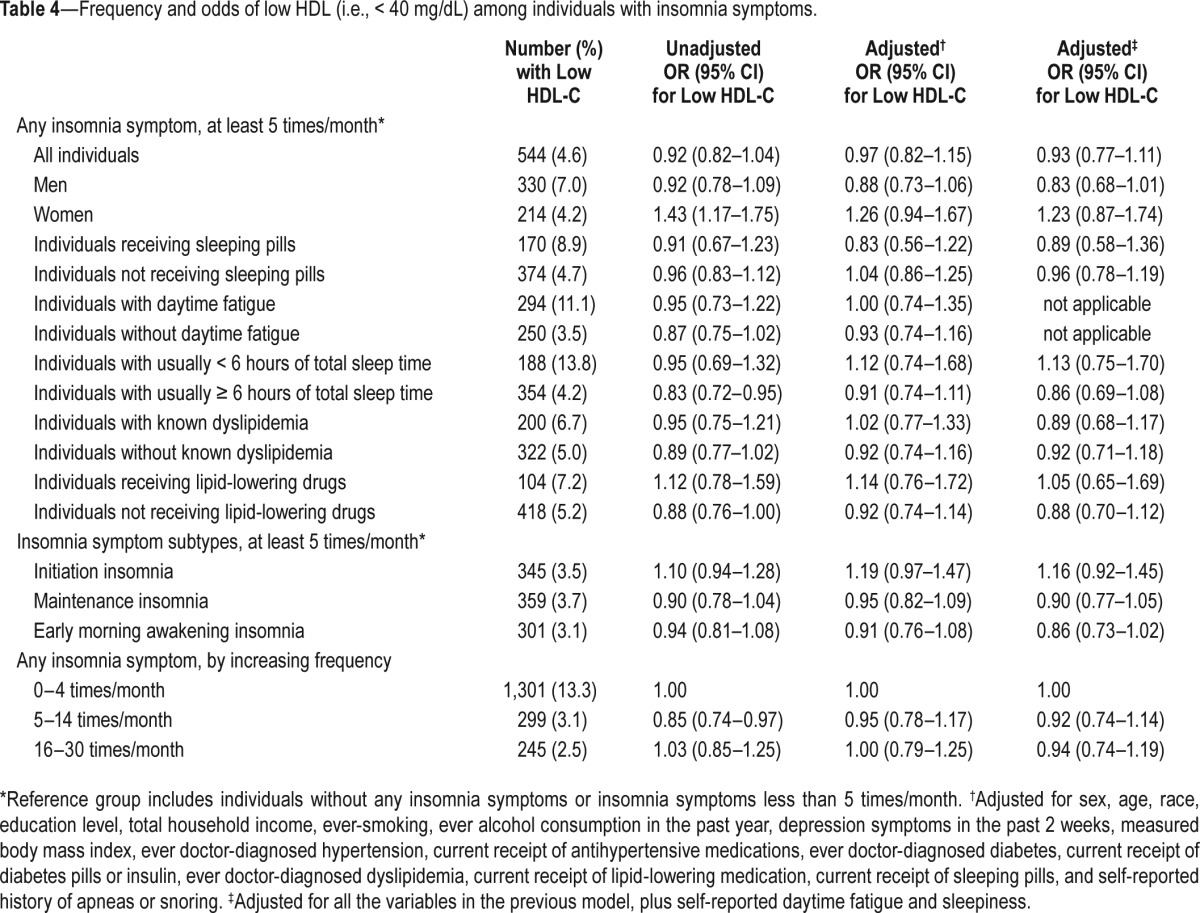
There were no significant associations between having any insomnia symptom at least five times in the past month and low HDL-C, either before or after covariate adjustment (Table 4). Among women with insomnia symptoms, there were significantly increased unadjusted odds of low HDL-C (OR 1.43, 95% CI 1.17–1.75), but this became nonsignificant after adjusting for covariates (OR 1.26, 95% CI 0.94–1.67). No significant association was observed between men with insomnia symptoms and low HDL-C. The remaining sensitivity analyses yielded non-significant results.
Table 4.
Frequency and odds of low HDL (i.e., < 40 mg/dL) among individuals with insomnia symptoms.
DISCUSSION
Insomnia symptoms were generally not found to be associated with dyslipidemia. Negative results were observed even when considering different categories of insomnia symptom frequency, the presence (or not) of concomitant daytime fatigue, and the presence (or not) of concomitant short sleep time, all of which would be considered markers of insomnia severity. One notable and novel positive finding was that individuals with insomnia symptoms who were receiving sleeping pills were 118% more likely to have elevated LDL-C after adjusting for covariates. In contrast, individuals with insomnia who were not receiving sleeping pills were no more likely to have elevated LDL-C compared to their noninsomnia counterparts.
The results of this study are largely in keeping with the few other published studies on this topic.18,29 Using population-level data from China involving more than 10,000 individuals, Zhan et al.29 found no significant associations between insomnia symptoms and measured dyslipidemia whatsoever among men, and there were no significant associations between insomnia symptoms and high LDL-C, high triglycerides, or low HDL-C among women.29 The only significant result was a 25% increased odds of elevated total cholesterol level among women experiencing insomnia symptoms greater than or equal to three times per week compared to those women experiencing no insomnia.29 However, Zhan et al.29 did not adjust analyses for some potentially important confounders, such as sleeping pill use and obstructive sleep apnea. Although the current study did not examine for total cholesterol, no significant associations between insomnia symptoms and dyslipidemia were found in subgroup analyses relating to sex or insomnia symptom frequency. In a small Taiwanese community-based sample, Chien et al.18 found that individuals experiencing insomnia symptoms nearly every day had, somewhat surprisingly, significantly lower total cholesterol levels compared to those experiencing insomnia symptoms less often. There were no significant trends between increasing insomnia severity and LDL-C, triglyceride, and HDL-C levels.18
The finding that insomnia symptoms do not appear to be associated with dyslipidemia potentially calls into question whether a true relationship exists between insomnia symptoms and coronary artery-related events and mortality. Multiple prospective cohort studies have previously reported that insomnia symptoms are not linked to coronary artery disease.21–28 Among studies reporting an association between insomnia and coronary artery-related events or mortality, findings were often limited to specific subgroups, such as individuals experiencing a particular insomnia symptom subtype14–16,20 or a particular frequency of insomnia symptoms.18–20 In the current study, subgroup analyses relating to insomnia symptom sub-types and insomnia symptom frequency yielded negative results. Previous studies reporting a positive association between insomnia and coronary artery disease may be explained by the fact that analyses were not adjusted for some potentially important confounders, such as obstructive sleep apnea and sleeping pills use. Obstructive sleep apnea is an important potential confounder because it is linked with both coronary artery disease and insomnia. An estimated 40% to 50% of individuals with obstructive sleep apnea have concomitant insomnia39 and an even higher proportion of individuals with insomnia may have coexisting obstructive sleep apnea.43 In the current study, analyses were adjusted for all the items contained in the Berlin Questionnaire, which is a validated screening instrument for obstructive sleep apnea,44 although no significant associations between insomnia and dyslipidemia were largely present even at the unadjusted level, before controlling for such variables. Sleeping pill use is another potential important confounder because it is associated with both insomnia and mortality,45,46 although again in this study results were generally negative even before adjusting for this variable. Some previous studies included the experience of ‘nonrestorative sleep’ alone as qualification for having insomnia and reported significantly increased risk of coronary artery disease in relation to it.19,20 The current study did not consider ‘nonrestorative sleep’ as an insomnia symptom, as this is a contentious issue in the sleep medicine community,47 with some advocating that ‘nonrestorative sleep’ alone should be considered as something distinct from insomnia.47,48 Moreover, in contrast to the previous DSMIV definition of insomnia, the more recent DSM-V definition no longer considers ‘non-restorative sleep’ alone as indicative of insomnia.31 It is possible that there may still be a link between insomnia and coronary artery-related events or mortality, even though the relationship between and insomnia and dyslipidemia may be negative. For example, through hypothalamic-pituitary-adrenal axis and sympathetic nervous system activation, insomnia may predispose to either hypertension and/or diabetes, which may then in turn contribute to developing coronary artery disease. However, previous analyses of NHANES data2,3 and other population-level databases17,49 have been mainly negative for a link between insomnia and hypertension.
The observations that sleeping pill use in the setting of insomnia is associated with significantly increased odds of LDL-C, but having insomnia symptoms and not receiving sleeping pills is not, are novel findings. Several previous population-based studies have reported that sedative medication use is associated with increased all-cause mortality,45,46 but possible links with cardiovascular-specific mortality are unknown. The finding of elevated LDL-C levels among recipients of sleeping pills who have insomnia may in part explain the sedative medication-mortality association through possible increased coronary artery-related events and mortality. The observed link between sleeping pill receipt and elevated LDL-C is particularly concerning, given the dramatic rise in the use of sedative medications in the general population in recent years.50,51 It could be argued that the confounding by indication underlies the association between sleeping pill receipt and elevated LDL-C, that is, individuals receiving sleeping pills may have a greater severity of insomnia than those not using such medications, and therefore, the presence of more severe insomnia may be driving the finding of increased LDL-C. However, no association was observed between elevated LDL-C and other markers of insomnia severity in the current study (i.e., frequent insomnia symptoms, insomnia symptoms coupled with daytime fatigue, and insomnia symptoms coupled with short sleep time).
Strengths of the current study are that it was based on recent, large, nationally representative US data, objective (and not patient-reported) measures of dyslipidemia were considered, a broad range of covariates were controlled for in the analysis, and multiple sensitivity analyses were conducted, including ones that evaluated for dyslipidemia among subgroups of individuals who likely had more severe insomnia. There are several limitations. First, this study was based on cross-sectional and not longitudinal data. Second, it may be argued that generally no association was found between insomnia symptoms and dyslipidemia because dyslipidemia may develop over time in response to chronic insomnia and insomnia symptoms only within in the preceding month were considered in this study. However, the majority of individuals with insomnia symptoms in this study likely had long-standing symptoms, as previous studies have shown that the majority of insomnia is chronic in nature.4,5 Furthermore, individuals with combined insomnia and daytime fatigue may reflect a subgroup that more likely has insomnia of chronic duration and these individuals were at no further increased risk of dyslipidemia compared to the reference group. Third, because insomnia symptoms were self-reported in this study, there may be some degree of misclassification of individuals with and without insomnia due to recall or social desirability biases. However, the presence of insomnia symptoms in the ‘real world’ is established by patient report and not by some objective testing and this is supported by clinical practice guidelines.32 Fourth, analyses were adjusted by the items contained in the Berlin Questionnaire and not by polysomnography-confirmed obstructive sleep apnea. Nonetheless, the Berlin Questionnaire is a validated screening instrument for obstructive sleep apnea,44 and furthermore, there were generally no associations observed between insomnia symptoms and dyslipidemia in unadjusted analyses, even before controlling for items contained in the Berlin Questionnaire. Fifth, it may be argued that the odds of women with insomnia symptoms having elevated triglycerides becoming nonsignificant after additionally controlling for daytime fatigue and sleepiness reflects overadjustment, because daytime fatigue and sleepiness may be consequences of insomnia. This is an unavoidable limitation because daytime fatigue and sleepiness are also items contained in the Berlin Questionnaire that screens for obstructive sleep apnea. The absence of associations between women with insomnia symptoms and high LDL-C or low HDL-C favors that there is likely no true link between dyslipidemia and women experiencing insomnia. Finally, it was beyond the scope of the current study to delineate if elevated LDL-C was associated with the use of specific types of sleeping pills or with all sedative medications more broadly. Further research will need to be undertaken to clarify the possible link between receipt of sedative medications and dyslipidemia.
In conclusion, this study was generally negative for a relationship between insomnia symptoms and dyslipidemia, even when having considered different forms of dyslipidemia, different insomnia symptom subtypes, and different markers of insomnia severity (including symptom frequency, concomitant daytime fatigue, and concomitant short sleep time). The lack of an association between insomnia and dyslipidemia potentially calls into question whether a true relationship exists between insomnia symptoms and coronary artery-related events and mortality, as some previous studies have reported.14–20 Receipt of sleeping pills in the setting of insomnia was found to be associated with significantly increased elevated LDL-C, even after adjusting for many covariates, raising further and novel potential safety concerns regarding the use of sedative drugs. Further research is needed to confirm a possible link between sleeping pill use and dyslipidemia and to clarify if an association with atherosclerosis exists for specific types of sleeping pills or with sedative pharmacotherapy more broadly.
DISCLOSURE STATEMENT
This was not an industry supported study. The author has indicated no financial conflicts of interest. This work was undertaken at St. Michael's Hospital, University of Toronto, Toronto, Ontario, Canada.
REFERENCES
- 1.Ancoli-Israel S, Roth T. Characteristics of insomnia in the United States: results of the 1991 National Sleep Foundation Survey. Sleep. 1999;22:S347–53. [PubMed] [Google Scholar]
- 2.Vozoris NT. The relationship between insomnia symptoms and hypertension using United States population-level data. J Hypertens. 2013;31:663–71. doi: 10.1097/HJH.0b013e32835ed5d0. [DOI] [PubMed] [Google Scholar]
- 3.Vozoris NT. Insomnia symptom frequency and hypertension risk: a population-based study. J Clin Psychiatry. 2014;75:616–23. doi: 10.4088/JCP.13m08818. [DOI] [PubMed] [Google Scholar]
- 4.Foley DJ, Monjan A, Simonsick EM, Wallace RB, Blazer DG. Incidence and remission of insomnia among elderly adults: an epidemiologic study of 6,800 persons over three years. Sleep. 1999;22:S366–72. [PubMed] [Google Scholar]
- 5.Vgontzas AN, Fernandez-Mendoza J, Bixler EO, et al. Persistent insomnia: the role of objective short sleep duration and mental health. Sleep. 2012;35:61–8. doi: 10.5665/sleep.1586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roth T, Ancoli-Israel S. Daytime consequences and correlates of insomnia in the United States: results of the 1991 National Sleep Foundation Survey II. Sleep. 1999;22:S354–8. [PubMed] [Google Scholar]
- 7.Ustinov Y, Lichstein KL, Wal GS, Taylor DJ, Riedel BW, Bush AJ. Association between report of insomnia and daytime functioning. Sleep Med. 2010;11:65–8. doi: 10.1016/j.sleep.2009.07.009. [DOI] [PubMed] [Google Scholar]
- 8.Phillips BA. Insomnia, hypnotic drug use, and patient well-being: first, do no harm. Mayo Clin Proc. 2012;87:417–8. doi: 10.1016/j.mayocp.2012.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Monroe LJ. Psychological and physiological differences between good and poor sleepers. J Abnorm Psychol. 1967;72:255–64. doi: 10.1037/h0024563. [DOI] [PubMed] [Google Scholar]
- 10.Johns MW, Gay TJA, Masterton JP, Bruce DW. Relationship between habits, adrenocortical activity and personality. Psychosom Med. 1971;33:499–508. doi: 10.1097/00006842-197111000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Adam K, Tomeny M, Oswald I. Physiological and psychological differences between good and poor sleepers. J Psychiatr Res. 1986;20:301–6. doi: 10.1016/0022-3956(86)90033-6. [DOI] [PubMed] [Google Scholar]
- 12.Vgontzas AN, Bixler EO, Lin HM, et al. Chronic insomnia is associated with nyctohemeral activation of the hypothalamic-pituitary-adrenal axis: clinical implications. J Clin Endocrinol Metab. 2001;86:3787–94. doi: 10.1210/jcem.86.8.7778. [DOI] [PubMed] [Google Scholar]
- 13.Irwin M, Clark C, Kennedy B, Christian Gillin J, Ziegler M. Nocturnal catecholamines and immune function in insomniacs, depressed patients, and control subjects. Brain Behav Immun. 2003;17:365–72. doi: 10.1016/s0889-1591(03)00031-x. [DOI] [PubMed] [Google Scholar]
- 14.Eaker ED, Pinsky J, Castelli WP. Myocardial infarction and coronary death among women: psychosocial predictors from a 20-year follow-up of women in the Framingham Study. Am J Epidemiol. 1992;135:854–64. doi: 10.1093/oxfordjournals.aje.a116381. [DOI] [PubMed] [Google Scholar]
- 15.Nilsson PM, Nilsson JA, Hedblad B, Berglund G. Sleep disturbance in association with elevated pulse rate for prediction of mortality--consequences of mental strain? J Intern Med. 2001;250:521–9. doi: 10.1046/j.1365-2796.2001.00913.x. [DOI] [PubMed] [Google Scholar]
- 16.Mallon L, Broman JE, Hetta J. Sleep complaints predict coronary artery disease mortality in males: a 12-year follow-up study of a middle-aged Swedish population. J Intern Med. 2002;251:207–16. doi: 10.1046/j.1365-2796.2002.00941.x. [DOI] [PubMed] [Google Scholar]
- 17.Phillips B, Mannino DM. Do insomnia complaints cause hypertension or cardiovascular disease? J Clin Sleep Med. 2007;3:489–94. [PMC free article] [PubMed] [Google Scholar]
- 18.Chien KL, Chen PC, Hsu HC, et al. Habitual sleep duration and insomnia and the risk of cardiovascular events and all-cause death: report from a community-based cohort. Sleep. 2010;33:177–84. doi: 10.1093/sleep/33.2.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Laugsand LE, Vatten LJ, Platou C, Janszky I. Insomnia and the risk of acute myocardial infarction: a population study. Circulation. 2011;124:2073–81. doi: 10.1161/CIRCULATIONAHA.111.025858. [DOI] [PubMed] [Google Scholar]
- 20.Li Y, Zhang X, Winkelman JW, et al. Association between insomnia symptoms and mortality: a prospective study of U.S. men. Circulation. 2014;129:737–46. doi: 10.1161/CIRCULATIONAHA.113.004500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Meisinger C, Heier M, Löwel H, et al. Sleep duration and sleep complaints and risk of myocardial infarction in middle-aged men and women from the general population: the MONICA/KORA Augsburg cohort study. Sleep. 2007;30:1121–7. doi: 10.1093/sleep/30.9.1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Elwood P, Hack M, Pickering J, et al. Sleep disturbance, stroke, and heart disease events: evidence from the Caerphilly cohort. J Epidemiol Community Health. 2006;60:69–73. doi: 10.1136/jech.2005.039057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schwartz SW, Cornoni-Huntley J, Cole SR, et al. Are sleep complaints an independent risk factor for myocardial infarction? Ann Epidemiol. 1998;8:384–92. doi: 10.1016/s1047-2797(97)00238-x. [DOI] [PubMed] [Google Scholar]
- 24.Appels A, de Vos Y, van Diest R, Höppner P, Mulder P, de Groen J. Are sleep complaints predictive of future myocardial infarction? Act Nerv Super (Praha) 1987;29:147–51. [PubMed] [Google Scholar]
- 25.Leineweber C, Kecklund G, Janszky I, Akerstedt T, Orth-Gomér K. Poor sleep increases the prospective risk for recurrent events in middle-aged women with coronary disease. The Stockholm Female Coronary Risk Study. J Psychosom Res. 2003;54:121–7. doi: 10.1016/s0022-3999(02)00475-0. [DOI] [PubMed] [Google Scholar]
- 26.Suzuki E, Yorifuji T, Ueshima K, et al. Sleep duration, sleep quality and cardiovascular disease mortality among the elderly: a population-based cohort study. Prev Med. 2009;49:135–41. doi: 10.1016/j.ypmed.2009.06.016. [DOI] [PubMed] [Google Scholar]
- 27.Chandola T, Ferrie JE, Perski A, Akbaraly T, Marmot MG. The effect of short sleep duration on coronary heart disease risk is greatest among those with sleep disturbance: a prospective study from the Whitehall II cohort. Sleep. 2010;33:739–44. doi: 10.1093/sleep/33.6.739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rod NH, Vahtera J, Westerlund H, et al. Sleep disturbances and cause-specific mortality: results from the GAZEL cohort study. Am J Epidemiol. 2011;173:300–9. doi: 10.1093/aje/kwq371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhan Y, Zhang F, Lu L, et al. Prevalence of dyslipidemia and its association with insomnia in a community based population in China. BMC Public Health. 2014;14:1050. doi: 10.1186/1471-2458-14-1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention. National Centre for Health Statistics. National Health and Nutrition Examination Survey: Sample Design: 2007-2010. [Accessed April 2015]. Available from: http://www.cdc.gov/nchs/data/series/sr_02/sr02_160.pdf.
- 31.American Psychiatric Association. 5th edition. Arlington, VA: American Psychiatric Publishing; 2013. Diagnostic and statistical manual of mental disorders. [Google Scholar]
- 32.Schutte-Rodin S, Broch L, Buysse D, Dorsey C, Sateia M. Clinical guideline for the evaluation and management of chronic insomnia in adults. J Clin Sleep Med. 2008;4:487–504. [PMC free article] [PubMed] [Google Scholar]
- 33.Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey. 2007 - 2008 Data Documentation, Codebook, and Frequencies. Triglycerides and LDL-Cholesterol. [Accessed April 2015]. Available at: http://wwwn.cdc.gov/nchs/nhanes/2007-2008/TRIGLY_E.htm.
- 34.Mora S, Rifai N, Buring JE, Ridker PM. Comparison of LDL cholesterol concentrations by Friedewald calculation and direct measurement in relation to cardiovascular events in 27,331 women. Clin Chem. 2009;55:888–94. doi: 10.1373/clinchem.2008.117929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nordestgaard BG, Benn M, Schnohr P, Tybjaerg-Hansen A. Nonfasting triglycerides and risk of myocardial infarction, ischemic heart disease, and death in men and women. JAMA. 2007;298:299–308. doi: 10.1001/jama.298.3.299. [DOI] [PubMed] [Google Scholar]
- 36.Doran B, Guo Y, Xu J, et al. Prognostic value of fasting versus nonfasting low-density lipoprotein cholesterol levels on long-term mortality: insight from the National Health and Nutrition Examination Survey III (NHANES-III) Circulation. 2014;130:546–53. doi: 10.1161/CIRCULATIONAHA.114.010001. [DOI] [PubMed] [Google Scholar]
- 37.National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–421. [PubMed] [Google Scholar]
- 38.Miller M, Stone NJ, Ballantyne C, et al. American Heart Association Clinical Lipidology, Thrombosis, and Prevention Committee of the Council on Nutrition, Physical Activity, and Metabolism; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Cardiovascular Nursing; Council on the Kidney in Cardiovascular Disease. Triglycerides and cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2011;123:2292–333. doi: 10.1161/CIR.0b013e3182160726. [DOI] [PubMed] [Google Scholar]
- 39.Vozoris NT. Sleep apnea-plus: prevalence, risk factors, and association with cardiovascular diseases using United States population-level data. Sleep Med. 2012;3:637–44. doi: 10.1016/j.sleep.2012.01.004. [DOI] [PubMed] [Google Scholar]
- 40.Gardner CD, Winkleby MA, Fortmann SP. Population frequency distribution of non-high-density lipoprotein cholesterol (Third National Health and Nutrition Examination Survey [NHANES III], 1988-1994) Am J Cardiol. 2000;86:299–304. doi: 10.1016/s0002-9149(00)00918-8. [DOI] [PubMed] [Google Scholar]
- 41.Gunnarsson SI, Peppard PE, Korcarz CE, et al. Obstructive sleep apnea is associated with future subclinical carotid artery disease: thirteen-year follow-up from the Wisconsin sleep cohort. Arterioscler Thromb Vasc Biol. 2014;34:2338–42. doi: 10.1161/ATVBAHA.114.303965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Canadian Institutes of Health Research, Natural Sciences and Engineering Research Council of Canada, and Social Sciences and Humanities Research Council of Canada, Tri-Council Policy Statement: Ethical Conduct for Research Involving Humans, December 2014. [Accessed April 2015]. Available at http://www.pre.ethics.gc.ca/pdf/eng/tcps2/TCPS_2_FINAL_Web.pdf.
- 43.Guilleminault C, Palombini L, Poyares D, Chowdhuri S. Chronic insomnia, post menopausal women, and sleep disordered breathing: part 1. Frequency of sleep disordered breathing in a cohort. J Psychosom Res. 2002;53:611–5. doi: 10.1016/s0022-3999(02)00445-2. [DOI] [PubMed] [Google Scholar]
- 44.Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP. Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med. 1999;131:485–91. doi: 10.7326/0003-4819-131-7-199910050-00002. [DOI] [PubMed] [Google Scholar]
- 45.Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry. 2002;59:131–6. doi: 10.1001/archpsyc.59.2.131. [DOI] [PubMed] [Google Scholar]
- 46.Kripke DF, Langer RD, Kline LE. Hypnotics' association with mortality or cancer: a matched cohort study. BMJ Open. 2012;2:e000850. doi: 10.1136/bmjopen-2012-000850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Riemann D. Nonrestorative sleep: a new perspective. Sleep. 2013;36:633–4. doi: 10.5665/sleep.2612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Roth T, Zammit G, Lankford A, et al. Nonrestorative sleep as a distinct component of insomnia. Sleep. 2010;33:49–58. doi: 10.1093/sleep/33.4.449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Phillips B, Buzkova P, Enright P on behalf of the Cardiovascular Health Study Research Group. Insomnia did not predict incident hypertension in older adults in the cardiovascular health study. Sleep. 2009;32:65–72. [PMC free article] [PubMed] [Google Scholar]
- 50.Vozoris NT, Leung RS. Sedative medication use: prevalence, risk factors, and associations with body mass index using population-level data. Sleep. 2011;34:869–74. doi: 10.5665/SLEEP.1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bertisch SM, Herzig SJ, Winkelman JW, Buettner C. National use of prescription medications for insomnia: NHANES 1999-2010. Sleep. 2014;37:343–9. doi: 10.5665/sleep.3410. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


