Abstract
The Accreditation Council for Graduate Medical Education (ACGME) has launched a new shared learning collaborative as part of its larger Clinical Learning Environment Review (CLER) initiative. The collaboration, called Pursuing Excellence in Clinical Learning Environments, aims to improve teaching practices and patient care in the hospitals, medical centers, and ambulatory care sites where residents and fellows pursue their formal clinical training in a specialty or subspecialty. The Pursuing Excellence Initiative (PEI) builds on the 2015 report of findings of the CLER program. These findings demonstrate variability across the nation's teaching hospitals in addressing 6 key focus areas.
PEI sets up a shared system of collaborative learning among participating sites of ACGME-accredited institutions, in which early participants share advances that will be disseminated through an expanding circle of other participants. The ACGME will award funding to encourage participation in the first major component of PEI. The goal is to stimulate high-leverage changes that will broadly improve patient care and clinical learning environments across the nation.
Editor's Note: The ACGME News and Views section of JGME includes data reports, updates, and perspectives from the ACGME and its review committees. The decision to publish the article is made by the ACGME.
Introduction
Over the past decade, health care organizations have increasingly focused on developing and implementing systems-based approaches to improving patient care. The specific areas for these innovations have varied, but the approach has typically involved interdisciplinary teams of professionals working together to standardize on evidence-based practices, reduce errors, and achieve continuous quality improvement.
Concurrent with these changes, the Accreditation Council for Graduate Medical Education (ACGME) and other national organizations have been reexamining the nation's graduate medical education (GME) system to address evolving needs in the area of the quality and safety of patient care.1–3 Studies have demonstrated that residents' clinical learning environments can influence their practice patterns over their clinical careers.4–6 One study showed, for example, that residents who train in areas where aggressive medical management is the norm tend to choose more aggressive measures later in life, even in cases where conservative care may be as or more appropriate.5 Another study found that physicians who trained in regions with relatively high per-capita health costs continue to practice in a higher-cost manner for up to 2 decades later, even if they have moved to a lower-cost region during the interim.5,6
In 2012, the ACGME launched the Clinical Learning Environment Review (CLER) to provide feedback to the nation's teaching hospitals and medical centers on how successful they are at engaging residents to improve quality and safety in the systems of patient care in which they learn and participate.7 Over the 3 intervening years, CLER representatives have site visited hospitals, medical centers, and ambulatory sites of 297 sponsoring institutions. At each site, they have conducted group meetings and in-person visits to individual clinical units. Their observations have focused on the 6 areas defined by the CLER Evaluation Committee in its Pathways to Excellence document,8 which encompass patient safety, health care quality (including health disparities), care transitions, supervision, fatigue management and mitigation, and professionalism. At the conclusion of each visit, the site visitors have shared their feedback at a meeting with the administrative, clinical, and educational leaders of the institution, highlighting areas of strength and opportunities for improvement.
The CLER program will publish a detailed report of findings from this first cycle of site visits in a supplement to the Journal of Graduate Medical Education later this spring. Four overarching key findings will be presented as part of the larger body of findings in that report. They include:
Clinical learning environments vary in their approaches to and capacity for addressing patient safety and health care quality, as well as the degree to which they engage resident and fellow physicians in addressing these areas.
Clinical learning environments vary in their approach to implementing GME. In many clinical learning environments, the approach to GME is largely developed and implemented independent of the organization's other areas of strategic planning and focus.
Clinical learning environments vary in the degree to which they coordinate and implement educational resources across the health care professions.
Clinical learning environments vary in the extent to which they invest in continually educating, training, and integrating faculty members and program directors in the areas of health care quality, patient safety, and other systems-based initiatives.
The CLER program found a high degree of variability both between and within institutions with regard to practices in all 6 focus areas. Currently, little is known about what underlies this variability, either for patient care or for the training of residents and fellows. We believe it is essential that this variability be studied so that innovations and successful practices can emerge to characterize high performance in clinical learning environments. The first component of the Pursuing Excellence Initiative (PEI) will focus on improvements in clinical learning environments related to these 4 overarching findings.
The Pursuing Excellence Initiative
The ACGME's new Pursuing Excellence in Clinical Learning Environments initiative offers a structured program to identify and promulgate advances across all 6 CLER focus areas. PEI sets up a shared collaborative learning program, in which early participants develop innovations that are passed along to an ever-expanding circle of participants at other clinical learning environments. The ACGME will provide funding to stimulate the first round of innovation, with a Request for Proposals to be released at the 2016 ACGME Annual Educational Conference later this month. (Proposals will be due by May 4, and awards will be announced in July.) The ACGME will also provide additional resources to support the learning collaborative throughout the 4-year program, such as sponsoring meetings, webinars, and online resources to facilitate collaboration and disseminate knowledge developed during the process.
The Pursuing Excellence Initiative was launched on November 3, 2015, at a special kick-off event in Washington, DC. It was attended by more than 70 leaders in health care quality and education. This initiative will serve to bring together participating sites from ACGME-accredited sponsoring institutions. The collaborative learning model approach for participating sites was chosen because of ACGME's recognition that the best solutions often come from collective exploration. PEI is being undertaken with 21 partners that are comprised of national organizations focused on health care and health care education (box).
box: The 21 Pursuing Excellence Partners
These organizations are providing important support as key partners in the Pursuing Excellence Initiative (in alphabetical order).
Accreditation Council for Continuing Medical Education
Alliance of Independent Academic Medical Centers
American Association for Physician Leadership
American Association of Colleges of Osteopathic Medicine
American Board of Medical Specialties
American Hospital Association
American Medical Association
American Nurses Credentialing Center
American Osteopathic Association
American Society of Health-System Pharmacists
Association for Hospital Medical Education
Association of American Medical Colleges
Association of Osteopathic Directors and Medical Educators
Council of Medical Specialty Societies
Health Resources and Services Administration
Institute for Healthcare Improvement
Liaison Committee on Medical Education
National Patient Safety Foundation
Organization of Program Director Associations
The Joint Commission
VHA-UHC Alliance NewCo Inc.
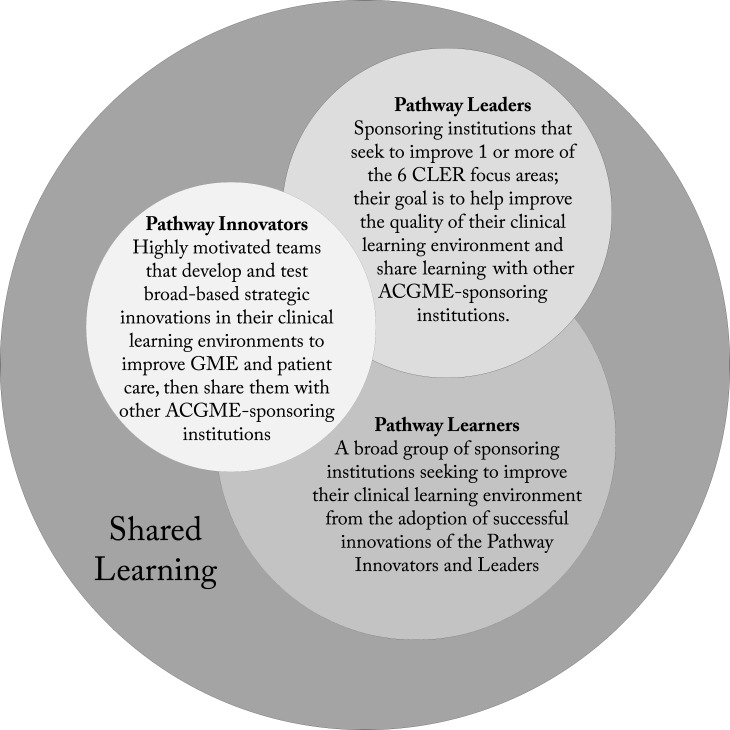
Institutions will participate in PEI through 1, 2, or 3 components (figure): Pathway Innovators, Pathway Leaders, and Pathway Learners, each with a slightly different yet interconnected role and aim. Their respective roles are discussed below.
FIGURE.
How Pursuing Excellence Will Work
Note: The conceptual diagram shows how early participants in the Pursuing Excellence Initiative will develop and share learning across an ever-expanding circle of others over a 4-year period. Institutions can take part by joining 1 of the 3 component groups described WHERE.
Pathway Innovators
The Pathways Innovators will be a select group of highly motivated teams of hospital and medical center executives and GME leaders who commit significant time and resources to enhance the vision and culture of clinical learning at their organizations. The ACGME will provide external funding to support these efforts through a competitive award process, and will provide access to a range of consultants and experts to assist with implementing new models for clinical learning environments. Organizations selected as Pathway Innovators will meet several times per year over a 4-year period to share progress and learn from one another.
Pathway Leaders
This component is designed to help support sponsoring institutions that seek to improve the quality of their clinical learning environments by focusing selectively on 1 of the 6 CLER focus areas. Although narrower in scope and shorter in duration than the Pathway Innovators component, the Pathway Leaders component will similarly bring together groups of key individuals from the participating sites of ACGME-accredited sponsoring institutions to identify new structures and processes for optimizing the learning environment in the chosen focus area.
Pathway Learners
This component aims to reach a broad audience of sponsoring institutions seeking to improve their clinical learning environments. Over the 4 years of PEI, the ACGME will identify numerous opportunities for the Innovators and Leaders to share their successes with the Pathway Learners. The Pathway Learners will help to accelerate adoption of the efforts while providing important feedback that helps shape innovations so they can be integrated across a large and variable set of institutions.
In seeking PEI participants, the ACGME will focus on institutions that are willing to explore innovative and strategic systems-based approaches to improving the clinical learning environment. It will also aim to assemble a cross-section of organizations that vary in size, geographic location, and mission within each component.
In keeping with the continuous quality improvement model, the ACGME also anticipates that PEI may evolve over time. Thus, the specifics of the program may be modified in future years depending on what new knowledge emerges from the process or from the ongoing program of CLER site visits.
Conclusions
In an effort to accelerate positive change, the ACGME has undertaken a number of initiatives focused on its mission to improve health care and population health by assessing and advancing the quality of resident physicians' education through accreditation. The Pursuing Excellence Initiative is the most recent effort to advance the mission—to emphasize the outcomes, not just the process, of GME.
The fundamental goal of PEI is to bring about high-leverage changes that broadly affect the quality of the clinical learning environments of ACGME-accredited sponsoring institutions. As with the CLER program, the PEI initiative is formative—meaning that it is designed to generate knowledge to help individual institutions make their own improvements. By using a shared learning collaborative approach, PEI also will help organizations that may lack the structure or resources to be on the leading edge of change join in the process by refining and spreading the learnings of others.
The ultimate goal—for ACGME and for its partners in PEI—is to improve GME as well as the patient care delivered in clinical learning environments, and to do so in a humanistic environment that promotes quality, safety, and professionalism.
Footnotes
Robin Wagner, RN, MHSA, is Vice President, Clinical Learning Environment Review (CLER), Accreditation Council for Graduate Medical Education (ACGME); Kevin B. Weiss, MD, MPH, is Senior Vice President, Institutional Accreditation, and Co-Chair, CLER Evaluation Committee, ACGME, and Professor of Medicine, Northwestern University Feinberg School of Medicine; Morgan L. Passiment, MS, is Director of Institutional Outreach and Collaboration, ACGME; and Thomas J. Nasca, MD, MACP, is Chief Executive Officer, ACGME and ACGME International, and Professor of Medicine (vol), Sidney Kimmel Medical College, Thomas Jefferson University.
The authors would like to thank Kevin McKean and Paige Amidon for their editorial assistance in preparing this article.
References
- 1.Institute of Medicine. Graduate Medical Education That Meets the Nation's Health Needs. Washington, DC: The National Academies Press;; 2014. [PubMed] [Google Scholar]
- 2.Josiah Macy Jr Foundation. Conclusion V. Ensuring an Effective Physician Workforce for the United States: Recommendations for Reforming Graduate Medical Education to Meet the Needs of the Public. The Second of Two Conferences—The Content and Format of GME. Conference Summary. 2011;10 http://macyfoundation.org/docs/macy_pubs/Macy_GME_Report,_Aug_2011.pdf. Accessed November 24, 2015. [Google Scholar]
- 3.Nasca TJ, Philibert I, Brigham T, Flynn TC. The next GME accreditation system—rationale and benefits. N Engl J Med. 2012;366(11):1051–1056. doi: 10.1056/NEJMsr1200117. [DOI] [PubMed] [Google Scholar]
- 4.Asch DA, Nicholson S, Srinivas S, Herrin J, Epstein AJ. Evaluating obstetrical residency programs using patient outcomes. JAMA. 2009;302(12):1277–1283. doi: 10.1001/jama.2009.1356. [DOI] [PubMed] [Google Scholar]
- 5.Sirovich BE, Lipner RS, Johnston M, Holmboe ES. The association between residency training and internists' ability to practice conservatively. JAMA Intern Med. 2014;174(10):1640–1648. doi: 10.1001/jamainternmed.2014.3337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen C, Petterson S, Phillips R, Bazemore A, Mullan F. Spending patterns in region of residency training and subsequent expenditures for care provided by practicing physicians for Medicare beneficiaries. JAMA. 2014;312(22):2385–2393. doi: 10.1001/jama.2014.15973. [DOI] [PubMed] [Google Scholar]
- 7.Weiss KB, Bagian JP, Nasca TJ. The clinical learning environment: the foundation of graduate medical education. JAMA. 2013;309(16):1687–1688. doi: 10.1001/jama.2013.1931. [DOI] [PubMed] [Google Scholar]
- 8.Weiss KB, Bagian JP, Wagner R, Nasca TJ. Introducing the CLER Pathways to Excellence: a new way of viewing clinical learning environments. J Grad Med Educ. 2014;6(3):608–609. doi: 10.4300/JGME-D-14-00347.1. [DOI] [PMC free article] [PubMed] [Google Scholar]