Abstract
Background
Mentors influence medical trainees' experiences through career enhancement and psychosocial support, yet some trainees never receive benefits from involved mentors.
Objective
Our goals were to examine the effectiveness of 2 interventions aimed at increasing the number of mentors in training programs, and to assess group differences in mentor effectiveness, the relationship between trainees' satisfaction with their programs given the presence of mentors, and the relationship between the number of trainees with mentors and postgraduate year (PGY).
Methods
In group 1, a physician adviser funded by the graduate medical education department implemented mentorships in 6 residency programs, while group 2 involved a training program with funded physician mentoring time. The remaining 89 training programs served as controls. Chi-square tests were used to determine differences.
Results
Survey responses from group 1, group 2, and controls were 47 of 84 (56%), 34 of 78 (44%), and 471 of 981 (48%, P = .38), respectively. The percentages of trainees reporting a mentor in group 1, group 2, and the control group were 89%, 97%, and 79%, respectively (P = .01). There were no differences in mentor effectiveness between groups. Mentored trainees were more likely to be satisfied with their programs (P = .01) and to report that faculty supported their professional aspirations (P = .001). Across all programs, fewer first-year trainees (59%) identified a mentor compared to PGY-2 through PGY-8 trainees (84%, P < .001).
Conclusions
A supported mentorship program is an effective way to create an educational environment that maximizes trainees' perceptions of mentorship and satisfaction with their training programs.
What was known and gap
Mentors provide career enhancement and psychosocial support to trainees, yet few studies have assessed the effectiveness of different approaches to support mentor programs.
What is new
Two approaches to supported mentorship in selected residency programs were compared to a control group at a single institution.
Limitations
Single institution and lack of randomization reduce generalizability.
Bottom line
Supported mentorship programs maximized trainees' perceptions of mentorship and satisfaction with their training program.
Editor's Note: The online version of this article contains the survey questions used in the study.
Introduction
A mentor is defined as a supporting person who provides career enhancement and psychosocial support to another individual.1–3 Career enhancement refers to the mentor's ability to prepare the mentee for the “next step” by providing advocacy, offering challenging assignments, and transmitting ethics.1,3,4 Mentors provide psychosocial support by enhancing the mentee's sense of identity and work role effectiveness.1 The first postgraduate year (PGY-1) is a critical period for mentorship, given the unique stressors placed on residents, which include relocation, separation from friends, and long hours that contribute to an increased risk of depressive symptoms.5,6
Trainees and faculty mentors mutually benefit from mentorship. Trainees develop enhanced professional skills, greater confidence, and increased scholarly productivity.7–9 Faculty mentors gain increased academic productivity and accelerated professional recognition.1,10,11
The goal of this study was to examine the effectiveness of 2 interventions on increasing the number of mentor relationships in graduate medical education (GME) programs at Stanford University Medical Center and Lucile Packard Children's Hospital. Secondary goals included describing differences in mentor effectiveness, relationship between trainees' satisfaction with their programs given the presence of mentors, and distribution of trainees with mentors across training years.
Methods
Setting and Study Design
We conducted a prospective cohort study at Stanford University Medical Center and Lucile Packard Children's Hospital between January 2014 and January 2015. The institutions collectively have 1143 medical trainees in 96 Accreditation Council for Graduate Medical Education (ACGME)–accredited programs.
The 2 interventions were aimed at increasing the number of mentor relationships. In group 1, the GME department funded a physician faculty adviser (0.2 full-time equivalent [FTE]) to implement countermeasures against barriers to effective mentorship. The adviser had a master's degree in education for health professionals, with a focus on educational leadership and mentorship. In group 2, the intervention involved funded physician mentoring time for trainees. Faculty coaches were funded by the pediatrics department (0.2 FTE for the coaching director and 0.1 FTE each for the 8 coaches). Scholarly concentration leaders were funded by the department, Lucile Packard Children's Hospital, and Stanford University School of Medicine (0.2 FTE each for 5 leaders).
Study Population
Group 1 consisted of 6 residency programs: medical genetics (n = 5), neurological surgery (n = 20), ophthalmology (n = 10), pediatric anesthesiology (n = 6), pediatric cardiology (n = 21), and radiation oncology (n = 15). The designated institutional official chose these programs as a cross-section of residency and fellowship programs. Group 2 consisted of the pediatrics residency (n = 78), the control group, and the remaining 89 accredited programs, which had variable mentorship requirements. Non–ACGME-approved programs were excluded.
Intervention
In group 1, the GME faculty adviser used a 5-step, evidence-based strategy to improve mentoring.
Step 1: Identified Program Rationale
The GME adviser met with the program director to highlight the rationale and to provide a 1-hour interactive session on the attributes of successful mentors and the benefits of effective mentorship to faculty.12 The session emphasized the role of emotional intelligence and traits, such as empathy, humor, and patience, in successful mentoring,1,8,13 and, given the potential for apathy or incompatibility, also highlighted that not all faculty members make suitable mentors.1
Step 2: Provided Trainee Educational Session
The GME adviser provided a 1-hour interactive session to trainees, outlining strategies for successful mentorship.14 It included a discussion regarding mentee roles and relationship engagement, with active follow-through on tasks and solicitation of feedback.14 These responsibilities were shared with faculty at their session.
Step 3: Designed Structured Program
The GME adviser met with program directors to initiate a structured mentorship program and to address the fact that many mentorships fail due to forced relations, random assignment, and lack of trust.1,15 To address the issue of forced relations, program directors solicited faculty mentors who would volunteer their time outside of clinical commitments for mentorship.1 Trainees entered into mentor relationships voluntarily.
Step 4: Developed Mentor Profiles
To circumvent random assignment of mentors to mentees, volunteer mentor faculty developed profiles of their personal and academic interests, which were used to facilitate early matching of mentors.16 Trainees selected mentors based on shared interests identified through the profiles.11
Step 5: Fostered Mentor Relationships
As effective mentor relationships are built on trust, relationships were developed through meetings at least every 4 months.11 To provide structure for mentor-mentee meetings, a discussion guide was distributed, which highlighted 6 areas of effective mentorship1: clinical skill development, posttraining career planning, networking opportunities, sponsorship and advocacy during training, research pursuits, and mentoring on challenging or sensitive issues. The program director reviewed the mentee-mentor relationships annually to facilitate change as needed.
Group 2 was the pediatrics residency program, and it implemented a mandatory resident mentoring program that included funded and volunteer faculty mentors who volunteered time beyond clinical commitments. Each resident received mentorship in 4 areas:
Clinical skill development by funded faculty coaches.
Scholarship development by funded scholarly concentration leaders and individual volunteer research mentors.
Career development by volunteer faculty advisers.
Resident wellness taught by volunteer humanism leaders.
An associate program director oversaw mentorship in all domains. Faculty coaches promoted self-reflection, provided feedback, and helped residents strengthen clinical skills. The scholarly concentration leaders mentored residents in developing research skills. Humanism leaders met monthly with residents to discuss topics, such as coping with patient death, workplace conflict, and work-life integration.
Outcomes
The annual GME resident survey measured, among groups, differences in the number of mentors, mentor effectiveness, program satisfaction, and PGY distribution of mentors (provided as online supplemental material). The survey was electronically distributed to trainees between November 4, 2014, and December 15, 2014.
The Institutional Review Board approved this research.
Statistical Analysis
Data were electronically collected via Qualtrics (Qualtrics LLC, Provo, UT). SPSS version 22 (IBM Corp, Armonk, NY) was used to analyze the results. PGY-1 trainees were analyzed separately, given their unique stressors.5
Chi-square tests were used to determine group differences between trainees with a mentor and those without (P < .016 denoted statistical significance after Bonferroni correction as a conservative measure against multiple comparisons).
Median Likert scores were used to compare mentor effectiveness between groups. Chi-square tests measured the relationship between trainees' satisfaction with programs, resident perception of faculty support and presence of a mentor, and relationship between the presence of a mentor and PGY of training. An alpha level of < .05 indicated statistical significance.
Results
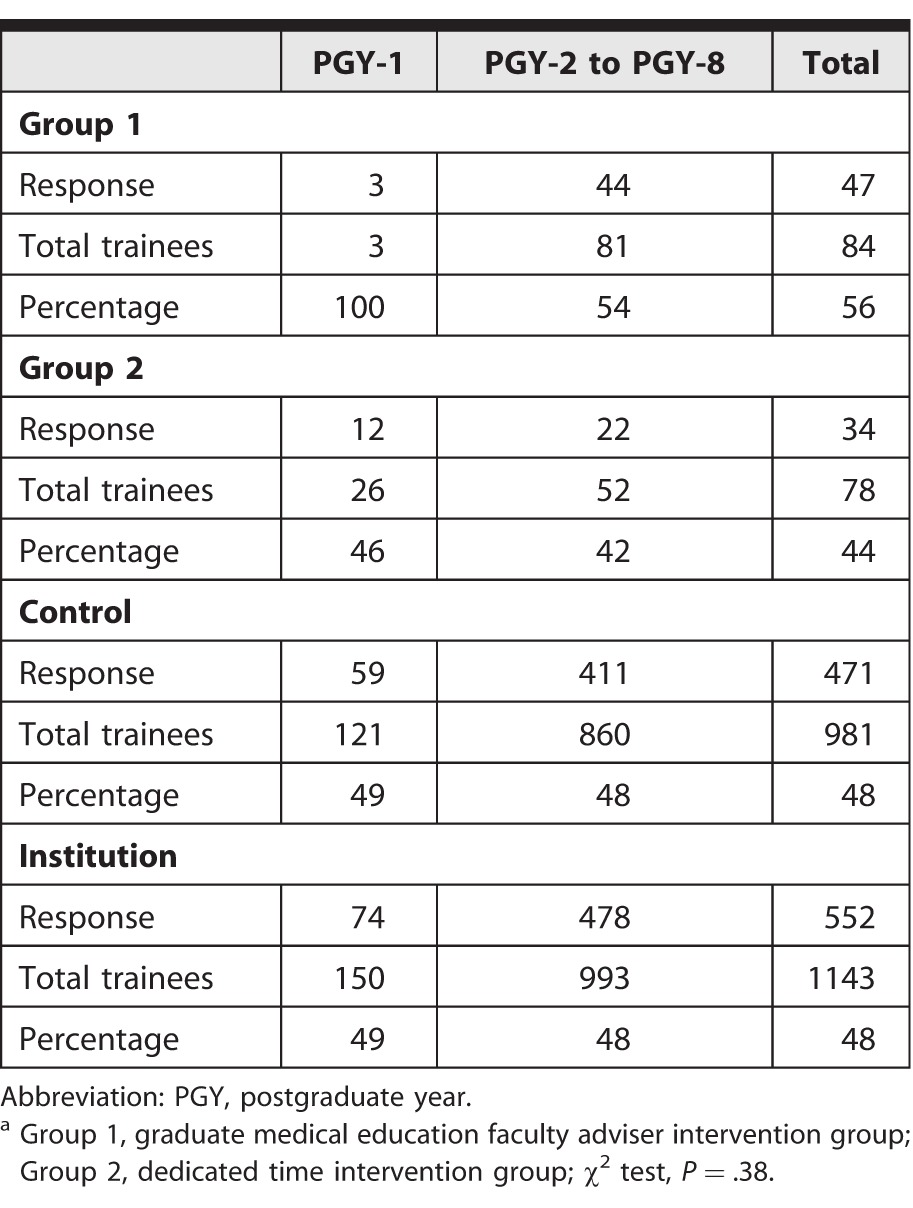
The survey was distributed to 1143 trainees, and 552 responses (48%) were received (table 1). In group 1, the response rate was 56% (47 of 84); in group 2, the rate was 44% (34 of 78 trainees); and in the control group, 471 of 981 trainees (48%) responded. There were no significant differences in response rates between group 1, group 2, and the controls (P = .38).
TABLE 1.
Resident Survey Completion Rate by Interventiona
Establishment of Mentor Relationships
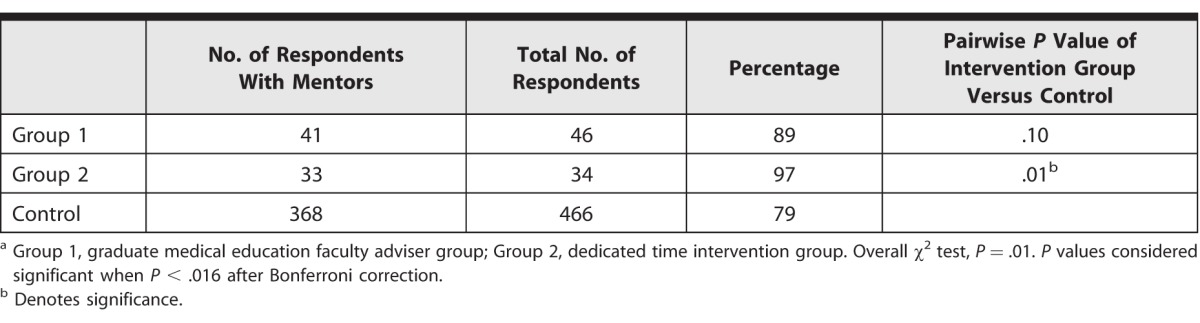
The percentages of trainees reporting a mentor in group 1, group 2, and the control group were 89%, 97%, and 79%, respectively (P = .01). A subgroup pairwise analysis using χ2 indicated a statistically significant difference between the intervention groups and the control group (table 2).
TABLE 2.
Incidence of Trainees With Mentorsa
Description of Mentor Effectiveness
For trainees who reported mentors, there were no differences in mentor effectiveness between group 1, group 2, and the control group. The median Likert score was 5 out of 6 in each category, indicating that faculty mentors were viewed as effective.
Description of Trainee Satisfaction With Program and Faculty
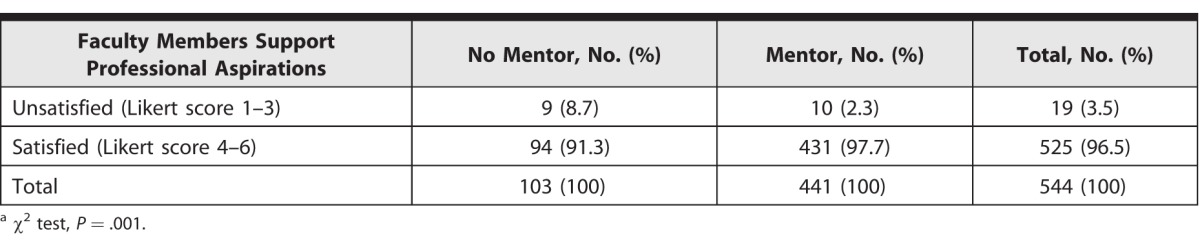
In the analysis of all groups, trainees with mentors were more satisfied with their programs compared to trainees without mentors (χ2, P = .01; table 3) and were more likely to report that faculty supported their professional aspirations (χ2, P = .001; table 4).
TABLE 3.
Institutional Comparison of Mentorship Status and Trainees' Program Satisfactiona
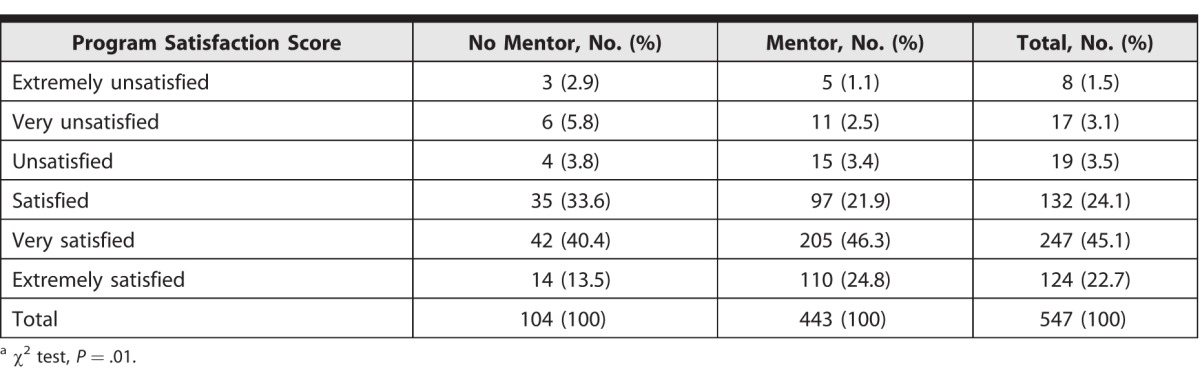
TABLE 4.
Comparison of Mentorship Status and Faculty Support of Professional Aspirationsa
Description of Mentor Distribution
Fewer PGY-1 trainees (44 of 74, 59%) identified a mentor compared with PGY-2 through PGY-8 trainees (399 of 473, 84%), and this difference was statistically significant (χ2, P < .001).
Discussion
Our findings demonstrate a significant increase in reported mentorship from trainees with funded faculty mentors. Faculty mentors received high effectiveness ratings. Mentored trainees were more likely to report greater satisfaction with their program and higher likelihood of feeling that faculty supported their professional aspirations. Finally, of the 21% of trainees without mentors, the majority were PGY-1s, highlighting the need for early mentor identification.
Although funding for mentorship has been examined, this study is the first known to the authors to directly compare 2 funded mentorship models.17–21 A survey in internal medicine showed that clinician investigators were more likely than noninvestigators to have mentorship funding, with the majority originating from federal grants.19 A study in surgery confirmed that federal funding for mentorship has increased over the last 20 years for clinician investigators.20 Although mentorship funding is available through external sources, there is little published on internally funded mentorships.19,21
The benefits of our group 1 intervention included the low cost (0.2 FTE) and deployment across multiple programs. Group 2, which was most effective, included a multifaceted approach, with several mentors per trainee at an expense of 2 FTE. The higher cost of the group 2 intervention should be weighed against its benefits. Previous studies report that trainees consider mentors influential to career growth, since those with mentors report an increased likelihood to enter academic medicine and achieve promotion.18,22,23 Several studies have established that trainees with mentors allocate more time to research and produce more publications.20,23–25 Given the competing demands of faculty physicians, our findings support the need for institutions to consider mentor compensation.
The analysis of secondary aims demonstrated a correlation between those with mentors and program satisfaction, aligning with a previous study that reported the presence of mentors to be associated with higher satisfaction.26 The majority of trainees without mentors were PGY-1s. PGY-1s have previously been shown to be at an increased risk of having depressive symptoms.5,27 A longitudinal study confirmed elevated depression and anxiety scores during training and recommended continuous support and counsel by a mentor.28 Close relationships with mentors have led to improved psychological well-being in young adults with depression.29 Given the psychological benefits of mentoring, PGY-1 trainees represent a population worthy of mentorship.
This study has several limitations. First, as with all self-reported surveys, data may be subject to recall bias. Because there was no measure of content validity, respondents may not have interpreted questions as intended. Second, data may not be representative of all trainees due to selection bias from some respondents. Selection bias may have also been present in relation to trainees who chose to pursue mentoring. Third, the intervention groups were not formally randomized to ensure a representative cross-section of different trainees in different settings. Group 2 consisted of 1 program due to financial constraints that limited support of a widespread mentoring program.
The results represent findings from a 1-year pilot intervention. Future studies should include pre-post data to better quantify effectiveness. Longitudinal studies to examine quantifiable benefits of mentorship are also needed as a balancing measure against the costs of funded mentorship programs.
Conclusion
Residency programs with a funded mentorship program reported a higher number of mentors compared with programs that were supported by a GME faculty adviser and programs serving as controls. Trainees with a mentor were more likely to report overall program satisfaction and faculty support of their aspirations.
Supplementary Material
Footnotes
Thomas J. Caruso, MD, MEHP, is Graduate Medical Education Faculty Advisor, Departments of Graduate Medical Education and of Anesthesiology, Perioperative, and Pain Medicine, Stanford University; Diane H. Steinberg, PhD, is Program Manager and Education Specialist, Department of Graduate Medical Education, Stanford University; Nancy Piro, PhD, is Program Manager and Education Specialist, Department of Graduate Medical Education, Stanford University; Kimberly Walker, PhD, is Instructional Designer, Educational Technology, Stanford University School of Medicine; Rebecca Blankenburg, MD, MPH, is Clinical Associate Professor, Pediatric Hospital Medicine, and Associate Chair of Education, Pediatrics, Stanford University School of Medicine; Caroline Rassbach, MD, is Associate Program Director for Advising, Coaching, and Assessment, Department of Pediatrics, Stanford University School of Medicine; Juan L. Marquez, MD, is Resident Physician, Department of Anesthesiology, University of Michigan; Laurence Katznelson, MD, is Professor of Neurosurgery and Medicine and Associate Dean of Graduate Medical Education, Stanford University School of Medicine; and Ann Dohn, MA, is Designated Institutional Officer, Department of Graduate Medical Education, Stanford University Hospital and Clinics.
Funding: The authors report no external funding source for this study.
Conflict of interest: The authors declare they have no competing interests.
References
- 1.Johnson WB. The intentional mentor: strategies and guidelines for the practice of mentoring. Prof Psychol Res Pract. 2002;33(1):88–96. [Google Scholar]
- 2.Clapp E. 2011 Mentorship Conference. Albuquerque, NM: University of New Mexico; Oct 26 28, 2011. Omni-directional mentorship: redefining mentorship as a reciprocal process of teaching and learning. ed. [Google Scholar]
- 3.Arthur MB. Review of Mentoring at Work: Developmental Relationships in Organizational Life. Admin Sci Quart. 1985;30(3):454–456. [Google Scholar]
- 4.Kitchener KS. Psychologist as teacher and mentor: affirming ethical values throughout the curriculum. Prof Psychol Res Pract. 1992;23(3):190–195. [Google Scholar]
- 5.Reuben DB. Depressive symptoms in medical house officers: effects of level of training and work rotation. Arch Intern Med. 1985;145(2):286–288. [PubMed] [Google Scholar]
- 6.Kashiwagi DT, Varkey P, Cook DA. Mentoring programs for physicians in academic medicine: a systematic review. Acad Med. 2013;88(7):1029–1037. doi: 10.1097/ACM.0b013e318294f368. [DOI] [PubMed] [Google Scholar]
- 7.Hirsch AE, Agarwal A, Rand AE, DeNunzio NJ, Patel KR, Truong MT, et al. Medical student mentorship in radiation oncology at a single academic institution: a 10-year analysis. Pract Radiat Oncol. 2015;5(3):e163–e168. doi: 10.1016/j.prro.2014.08.005. [DOI] [PubMed] [Google Scholar]
- 8.Clark RA, Harden SL, Johnson WB. Mentor relationships in clinical psychology doctoral training: results of a national survey. Teach Psychol. 2000;27(4):262–268. [Google Scholar]
- 9.Johnson WB, Koch C, Fallow GO, Huwe JM. Prevalence of mentoring in clinical versus experimental doctoral programs: survey findings, implications, and recommendations. Psychother Theory Res Pract Train. 2000;37(4):325–334. [Google Scholar]
- 10.Ragins BR, Scandura TA. Gender differences in expected outcomes of mentoring relationships. Acad Manage J. 1994;37(4):957–971. [Google Scholar]
- 11.Russell JE, Adams DM. The changing nature of mentoring in organizations: an introduction to the special issue on mentoring in organizations. J Voc Behav. 1997;51(1):1–14. [Google Scholar]
- 12.Johnson WB. On Being a Mentor: A Guide for Higher Education Faculty. Mahwah, NJ: Lawrence Erlbaum Associates Inc;; 2007. [Google Scholar]
- 13.Pereg T. 2014 leadership program: emotional intelligence, mentoring are keys to effective performance. Bull Am Coll Surg. 2014;99(6):58–64. [PubMed] [Google Scholar]
- 14.Zerzan JT, Hess R, Schur E, Phillips RS, Rigotti N. Making the most of mentors: a guide for mentees. Acad Med. 2009;84(1):140–144. doi: 10.1097/ACM.0b013e3181906e8f. [DOI] [PubMed] [Google Scholar]
- 15.Fagenson-Eland EA, Marks MA, Amendola KL. Perceptions of mentoring relationships. J Voc Behav. 1997;51(1):29–42. [Google Scholar]
- 16.Cohee BM, Koplin SA, Shimeall WT, Quast TM, Hartzell JD. Results of a formal mentorship program for internal medicine residents: can we facilitate genuine mentorship? J Grad Med Educ. 2015;7(1):105–108. doi: 10.4300/JGME-D-14-00315.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sambunjak D, Straus SE, Marusić A. A systematic review of qualitative research on the meaning and characteristics of mentoring in academic medicine. J Gen Intern Med. 2010;25(1):72–78. doi: 10.1007/s11606-009-1165-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sambunjak D, Straus SE, Marusić A. Mentoring in academic medicine: a systematic review. JAMA. 2006;296(9):1103–1115. doi: 10.1001/jama.296.9.1103. [DOI] [PubMed] [Google Scholar]
- 19.Luckhaupt SE, Chin MH, Mangione CM, Phillips RS, Bell D, Leonard AC, et al. Mentorship in academic general internal medicine. J Gen Intern Med. 2005;20(11):1014–1018. doi: 10.1111/j.1525-1497.2005.215.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Orandi BJ, Blackburn S, Henke PK. Surgical mentors' and mentees' productivity from 1993 to 2006. Am J Surg. 2011;201(2):260–265. doi: 10.1016/j.amjsurg.2010.01.026. [DOI] [PubMed] [Google Scholar]
- 21.Donovan JC. Mentorship in dermatology residency training programs: charting the right course. Dermatol Online J. 2009;15(5):3. [PubMed] [Google Scholar]
- 22.Wise MR, Shapiro H, Bodley J, Pittini R, McKay D, Willan A, et al. Factors affecting academic promotion in obstetrics and gynaecology in Canada. J Obstet Gynaecol Can. 2004;26(2):127–136. doi: 10.1016/s1701-2163(16)30488-1. [DOI] [PubMed] [Google Scholar]
- 23.Pearlman SA, Leef KH, Sciscione AC. Factors that affect satisfaction with neonatal-perinatal fellowship training. Am J Perinatol. 2004;21(7):371–375. doi: 10.1055/s-2004-835308. [DOI] [PubMed] [Google Scholar]
- 24.Ramondetta LM, Bodurka DC, Tortolero-Luna G, Gordinier M, Wolf JK, Gershenson DM, et al. Mentorship and productivity among gynecologic oncology fellows. J Cancer Educ. 2003;18(1):15–19. doi: 10.1207/s15430154jce1801_9. [DOI] [PubMed] [Google Scholar]
- 25.Steiner JF, Curtis P, Lanphear BP, Vu KO, Main DS. Assessing the role of influential mentors in the research development of primary care fellows. Acad Med. 2004;79(9):865–872. doi: 10.1097/00001888-200409000-00012. [DOI] [PubMed] [Google Scholar]
- 26.Sciscione A, Colmorgen GC, D'Alton M. Factors affecting fellowship satisfaction, thesis completion, and career direction among maternal-fetal medicine fellows. Obstet Gynecol. 1998;91(6):1023–1026. doi: 10.1016/s0029-7844(98)00076-3. [DOI] [PubMed] [Google Scholar]
- 27.Ito M, Seo E, Ogawa R, Sanuki M, Maeno T, Maeno T. Can we predict future depression in residents before the start of clinical training? Med Educ. 2015;49(2):215–223. doi: 10.1111/medu.12620. [DOI] [PubMed] [Google Scholar]
- 28.Buddeberg-Fischer B, Stamm M, Buddeberg C, Klaghofer R. Anxiety and depression in residents—results of a Swiss longitudinal study [in German] Z Psychosom Med Psychother. 2009;55(1):37–50. doi: 10.13109/zptm.2009.55.1.37. [DOI] [PubMed] [Google Scholar]
- 29.Hurd NM, Zimmerman MA. An analysis of natural mentoring relationship profiles and associations with mentees' mental health: considering links via support from important others. Am J Community Psychol. 2014;53(1–2):25–36. doi: 10.1007/s10464-013-9598-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


