Abstract
Background
Efforts to improve diabetes care in residency programs are ongoing and in the midst of continuity clinic redesign at many institutions. While there appears to be a link between resident continuity and improvement in glycemic control for diabetic patients, it is uncertain whether clinic structure affects quality measures and patient outcomes.
Methods
This multi-institutional, cross-sectional study included 12 internal medicine programs. Three outcomes (glycemic control, blood pressure control, and achievement of target low-density lipoprotein [LDL]) and 2 process measures (A1C and LDL measurement) were reported for diabetic patients. Traditional, block, and combination clinic models were compared using analysis of covariance (ANCOVA). Analysis was adjusted for continuity, utilization, workload, and panel size.
Results
No significant differences were found in glycemic control across clinic models (P = .06). The percentage of diabetic patients with LDL < 100 mg/dL was 60% in block, compared to 54.9% and 55% in traditional and combination models (P = .006). The percentage of diabetic patients with blood pressure < 130/80 mmHg was 48.4% in block, compared to 36.7% and 36.9% in other models (P < .001). The percentage of diabetic patients with HbA1C measured was 92.1% in block compared to 75.2% and 82.1% in other models (P < .001). Also, the percentage of diabetic patients with LDL measured was significantly different across all groups, with 91.2% in traditional, 70.4% in combination, and 83.3% in block model programs (P < .001).
Conclusions
While high scores on diabetic quality measures are achievable in any clinic model, the block model design was associated with better performance.
What was known and gap
There appears to be a link between resident continuity and improved glycemic control for diabetic patients, but the mechanism is not clear.
What is new
A multi-institution study tested the impact of 3 models for continuity clinics on glycemic control.
Limitations
Lack of randomization and self-selection of clinic model may introduce selection bias.
Bottom line
All clinical models produced good diabetic quality outcomes, but the block model design was associated with improved performance.
Introduction
Some medical schools are introducing longitudinal patient care experiences for students. Yet it is during residency that most internal medicine residents first provide primary care for chronically ill patients in a long-term therapeutic relationship. For this reason, several professional organizations have recommended that internal medicine residents practice in high-functioning clinics in order to learn best practices and quality processes of care for continuity patients.1–3 The residency program features that best facilitate delivery of high-quality primary care for patients still need to be determined. Some evidence suggests that practicing physicians provide significantly better care for diabetic patients than resident physicians; this raises the possibility that provider experience level is linked to quality, or that there are inherent deficiencies in resident continuity clinic that affect care.2 Patients in resident clinics tend to be sicker and more likely to report barriers to self care.2,3
Efforts to improve the quality of diabetes care in residency training programs have been made. Studies have demonstrated that implementing the chronic care model in primary care residency clinics improved diabetic patients' metabolic and process measures.4–7 A regional quality improvement collaborative aimed at improving care for diabetes in 10 primary care residency programs also resulted in better process measures with improved frequency of hemoglobin A1C testing and monofilament foot examinations.8 In addition, there appears to be a positive link between resident continuity and improvement in glycemic control in diabetic patients.9 However, it is uncertain whether the continuity clinic structure itself impacts quality measures and patient outcomes for diabetic patients. Therefore, in this study we evaluated correlations between continuity clinic design, resident experience level, and diabetes quality measures at the 12 institutions that are participating in the Educational Innovations Project Ambulatory Collaborative (EPAC).
Methods
Study Population and Design
Twelve programs participated in EPAC, and 98% of the 730 residents from these programs consented to participate (table 1).10–12 This was a multiinstitutional, cross-sectional study. The primary aim of this analysis was to assess the effect of clinic structure on quality measures for patients with diabetes mellitus in internal medicine (IM) residency continuity clinics. Additionally, we assessed the effect of level of resident training on diabetic outcomes. The data collection period was September 1, 2010, to May 31, 2011. One institution implemented a long block ambulatory experience that was off cycle from the traditional academic year, so the time frame at that institution was shifted to align with the residents' ambulatory experience.
TABLE 1.
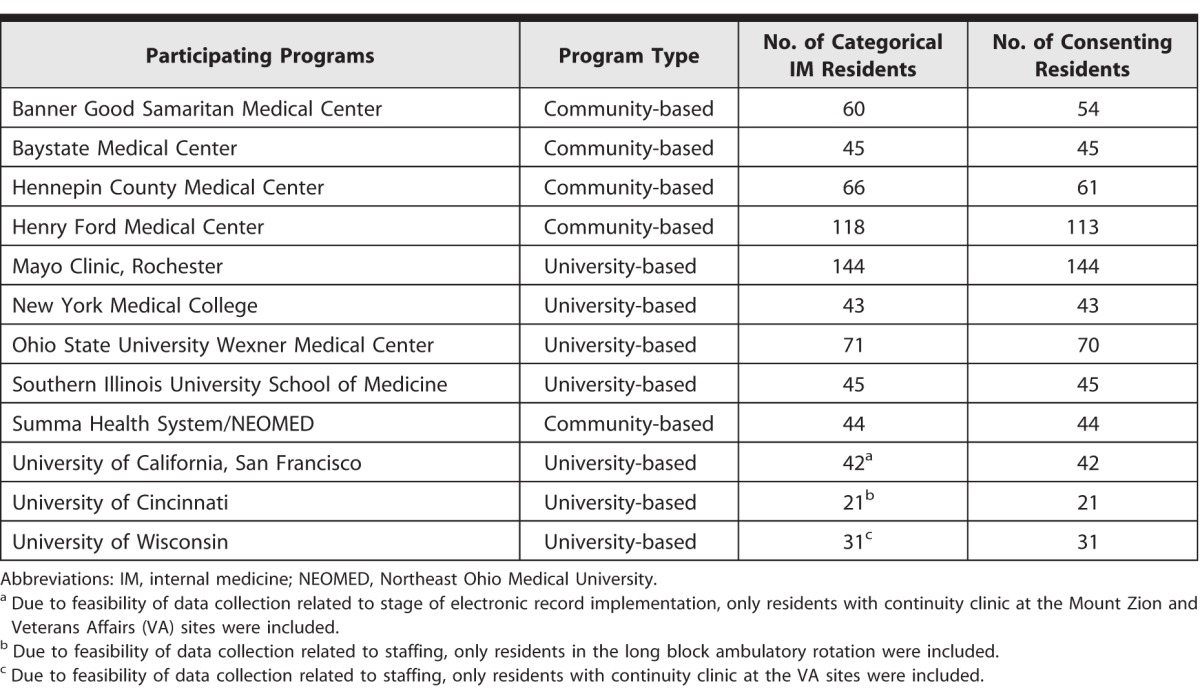
Clinic Model
As previously described, program leadership from each institution described their continuity clinic model as 1 of 3 groups: (1) traditional weekly experience; (2) combination with some weekly experience plus additional ambulatory block rotations; and (3) block structure with discrete inpatient and ambulatory rotations.10,11
Quality Measures for Patients With Diabetes Mellitus
Three outcome and 2 process measures were reported for diabetic patients. Outcome measures were in keeping with standards of care at the time of data collection and included the percentage of patients with HbA1c < 8%, the percentage of patients with blood pressure < 130/80 mmHg, and the percentage of patients with low-density lipoprotein (LDL) < 100 mg/dL.13 Process measures that were reported were the percentage of patients with recorded measurement of HbA1c and LDL within the last 12 months.
Practice Metrics
Practice metrics were used as control variables in the analyses. Continuity was measured using 2 methods: the usual provider of care method (UPC),14,15 and the continuity for physician method (PHY).16,17 The UPC is defined as the percentage of visits in which patients see their primary resident, whereas the PHY is defined as the percentage of visits for residents in which they see their own patients. Ambulatory workload was defined based on volume as the total number of patient visits provided by each resident during the study period divided by the number of clinics attended. Utilization was defined as the average number of visits for patients during the study period, and panel size was the number of patients followed by each resident in their continuity clinic at the end of the data collection period.
Texas Tech University Health Sciences Center El Paso provided oversight of the project as an unbiased, independent entity. All participating sites received approval from their local Institutional Review Boards.
Statistical Analysis
The quality measures for diabetic patients were the dependent variables. Clinic model was the independent variable included in the primary analysis. Control variables were UPC, PHY, utilization, ambulatory workload, and panel size. We compared the 3 clinic models using analysis of covariance (ANCOVA) with a subsequent Fisher least significant difference test for those means found to be statistically significant. A P value of < .05 was considered statistically significant. The Tukey studentized range (honest significant difference) test was used to assess significance among groups. The same analysis was conducted in the comparison of postgraduate year (PGY) levels with PGY level as the independent variable. We used SAS version 9.3 (SAS Institute Inc, Cary, NC) for statistical analysis. Missing values were eliminated.
Results
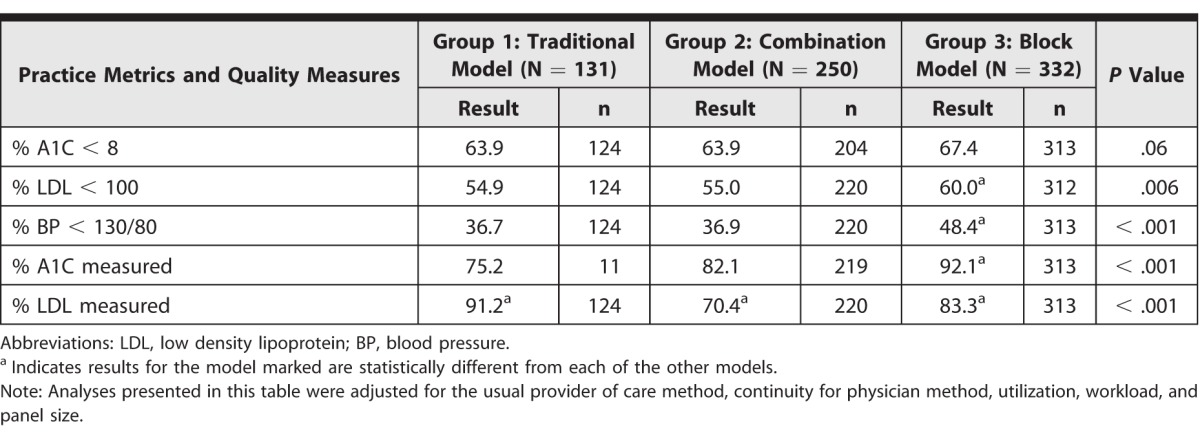
Data on quality measures for diabetic patients followed in continuity clinics were available for 77% to 97% of the participating residents, varying with the particular measure. The percentage of patients who had their HbA1C measured in the preceding year was available for 77%, while all other measures were available for at least 90% of participating residents overall. Results by clinic model are displayed in table 2. The percentages of diabetic patients with HbA1C < 8% were 63.9%, 63.9%, and 67.4% in the traditional, combination, and block models respectively (P = .06). The percentage of diabetic patients with LDL < 100 mg/dL was 60% in the block model, which was significantly different from 54.9% and 55% in the traditional and combination models (P = .006). The percentage of diabetic patients with blood pressure < 130/80 mmHg was 48.4% in the block model, compared to 36.7% and 36.9% in the traditional and combination models (P < .001). The percentage of diabetic patients with HbA1C measured in the preceding year was 92.1% in block model programs compared to 75.2% and 82.1% in the other models (P < .001). This measure was only available for a small number of the residents in the traditional model programs. The percentage of diabetic patients with LDL measured was significantly different across all 3 groups, with 91.2% in the traditional model, 70.4% in the combination group, and 83.3% in the block model programs (P < .001).
TABLE 2.
Continuity Clinic Model, Practice Metrics, and Quality Measures
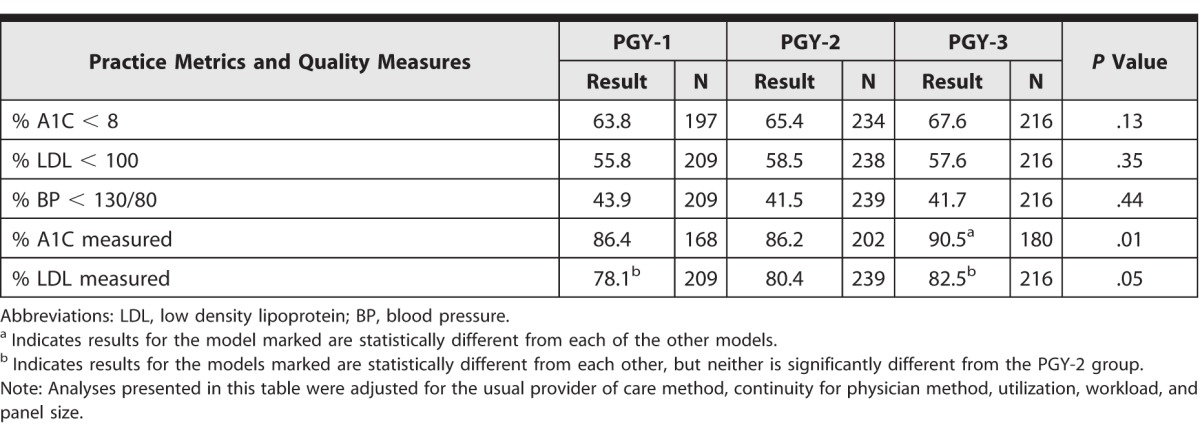
Results by level of training are shown in table 3. There were no significant differences in the 3 outcome measures for diabetic patients, the percentage of patients with HbA1c < 8%, LDL < 100mg/dL, and blood pressure < 130/80 mmHg. However, the 2 process measures did show significant differences based on PGY level. The percentage of diabetic patients with HbA1c measured in the preceding year was 90.5% for PGY-3 compared to 86.2% and 86.4% for PGY-2 and PGY-1 residents (P = .01). Also, the percentage of patients with LDL measured in the preceding year was significantly higher at 82.5% for PGY-3, compared to 78.1% for PGY-1 residents (P = .05).
TABLE 3.
Postgraduate Year (PGY), Practice Metrics, and Quality Measures
Discussion
Our findings indicate that the clinic model may indeed affect the outcome and process quality measures for diabetic patients. Two of the diabetic outcome measures and 1 of the diabetic process measures were more favorable in block model programs, even though as previously reported, this group had the highest ambulatory workload and panel size.12 However, measurement of LDL in the preceding year was highest in the traditional group. Thus, it is clearly possible to reach high targets for quality measures in various other clinic models, and clinic structure by itself is not the only contributing factor.
Practice redesign with implementation of the chronic care model with subsequent improvement in clinical outcomes was achievable in the multi-institutional Academic Chronic Care Collaborative.6 Studies have shown that total contact time with a practice team, regardless of the team, can be associated with an improvement in HbA1c concentration.7 It is possible that dedicated time in the ambulatory setting and increased clinic time during block rotations may explain some of the differences seen in our study. Identifying contributory factors within the various models will be critical for residencies to establish program structures that facilitate continuity of care and learning as recommended by Bowen and colleagues.18
Experience level has been linked to quality of care.2 PGY level is a marker for experience during residency, and PGY-3 status was associated with improved performance in diabetic process measures in keeping with prior literature. Variation related to experience level may be an interesting and useful marker of overall system performance. Indeed, in the future, as medical care systems become more reliable, this quality gap related to experience level should be expected to close.
Our study has a few limitations. One limitation is that it is not randomized. The participating institutions chose the model for their continuity clinic. In addition, the 12 residency programs that participated represent a small segment of the total number of internal medicine programs in the United States. The general focus of the Educational Innovations Project programs on performance enhancement may bias the results. There are inherent variations within the general categories that were labeled block and combination models. Data on 1 of the measures (percentage of A1C measured) was not available for more than 30% of the participants in the traditional model and we do not know whether this missing data affected the results. Finally, in the ambulatory environment there are many challenges that could not be controlled that may affect quality of care, such as level of staffing, staff training, stage of implementation of electronic health records, quality improvement techniques in use, and patient factors such as case mix, team relationships, and patient-centered medical home status. Future studies will be needed to clarify the role of clinic structure amid the many variables that can affect patient outcomes and resident learning.
Conclusion
High scores on diabetic quality measures are achievable in any clinic model. While the block model design was associated with better performance, clinic structure does not appear to be the key factor in determining results of diabetic process and outcome measures.
Footnotes
Maureen D. Francis, MD, FACP, is Assistant Dean for Medical Education and Associate Professor, Texas Tech University Health Sciences Center El Paso; Katherine A. Julian, MD, is Professor of Clinical Medicine and Track Director, Primary Care General Internal Medicine Residency Program, University of California, San Francisco; David A. Wininger, MD, is Program Director, Internal Medicine Residency, and Associate Professor of Clinical Internal Medicine, Ohio State University Wexner Medical Center; Sean Drake, MD, FACP, is Program Director, Internal Medicine Residency, Henry Ford Hospital, and Clinical Associate Professor, Wayne State University; KeriLyn Bollman, MD, is Associate Program Director, University of Arizona College of Medicine Phoenix Internal Medicine Programs; Christopher Nabors, MD, is Assistant Professor and Associate Program Director, Internal Medicine Residency, New York Medical College at Westchester Medical Center; Anne Pereira, MD, MPH, FACP, is Assistant Dean for Clinical Education and Associate Professor of Medicine, University of Minnesota Medical School; Michael Rosenblum, MD, FACP, is Director, Baystate Internal Medicine Residency Programs, and Assistant Clinical Professor, Tufts University School of Medicine; Amy B. Zelenski, PhD, is Director of Education, Department of Medicine, University of Wisconsin-Madison; David Sweet, MD, FACP, is Program Director, Internal Medicine Residency, Summa Health System, and Professor, Internal Medicine, Northeast Ohio Medical University; Kris Thomas, MD, FACP, is Associate Professor of Medicine, Consultant in the Division of Primary Care Internal Medicine, and Associate Program Director, Internal Medicine Residency, Mayo Clinic; Andrew Varney, MD, is Professor of Clinical Medicine and Program Director, Internal Medicine Residency, Southern Illinois University School of Medicine; Eric Warm, MD, FACP, is Professor of Medicine and Program Director, Internal Medicine Residency, University of Cincinnati Academic Health Center; and Mark L. Francis, MD, MS, FACP, is Professor, Medical Education, Texas Tech University Health Sciences Center El Paso.
Funding: The authors report no external funding source for this study.
Conflict of interest: The authors declare they have no competing interests.
The authors would like to thank the following for their contributions to the design of the study and data management at the participating institutions: Jayne Peterson, MD, Banner Good Samaritan Medical Center; Reva Kleppel, MSW, MPH, Baystate Medical Center; Mark Wieland, MD, Mayo Clinic, Rochester; Michael Langan, MD, Ohio State University Wexner Medical Center; Lynn Clough, PhD, Summa Health System, NEOMED; Rebecca Shunk, MD, Maya Dulay, MD, and Pat O'Sullivan, PhD, University of California, San Francisco; and Bennett Vogelman, MD, and Robert Holland, MD, University of Wisconsin. The authors would also like to thank Melchor Ortiz, PhD, Texas Tech University Health Sciences Center El Paso, for his assistance with the initial management of the data, and the Alliance for Academic Internal Medicine for providing administrative support for the project and meeting space for the Educational Innovations Project Ambulatory Collaborative.
References
- 1.Holmboe ES, Bowen JL, Green M, Gregg J, DiFrancesco L, Reynolds E, et al. Reforming internal medicine residency training. A report from the Society of General Internal Medicine's task force for residency reform. J Gen Intern Med. 2005;20(12):1165–1172. doi: 10.1111/j.1525-1497.2005.0249.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lynn L, Hess BJ, Weng W, Lipner RS, Holmboe ES. Gaps in quality of diabetes care in internal medicine residency clinics suggest the need for better ambulatory care training. Health Aff (Millwood) 2012;31(1):150–158. doi: 10.1377/hlthaff.2011.0907. [DOI] [PubMed] [Google Scholar]
- 3.Mladenovic J, Shea JA, Duffy FD, Lynn LA, Holmboe ES, Lipner RS. Variation in internal medicine residency clinic practices: assessing practice environments and quality of care. J Gen Intern Med. 2008;23(7):914–920. doi: 10.1007/s11606-008-0511-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yu GC, Beresford R. Implementation of a chronic illness model for diabetes care in a family medicine residency program. J Gen Intern Med. 2010;25(suppl 4):615–619. doi: 10.1007/s11606-010-1431-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Coca A, Francis MD. Implementing the chronic care model in an academic setting: a resident's perspective. Semin Med Prac. 2007;10:1–8. [Google Scholar]
- 6.Stevens DP, Bowen JL, Johnson JK, Woods DM, Provost LP, Holman HR, et al. A multi-institutional quality improvement initiative to transform education for chronic illness care in resident continuity practices. J Gen Intern Med. 2010;25(suppl 4):574–580. doi: 10.1007/s11606-010-1392-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Siminerio LM, Piatt G, Zgibor JC. Implementing the chronic care model for improvements in diabetes care and education in a rural primary care practice. Diabetes Educator. 2005;31(2):225–234. doi: 10.1177/0145721705275325. [DOI] [PubMed] [Google Scholar]
- 8.Newton W, Baxley E, Reid A, Stanek M, Robinson M, Weir S. Improving chronic illness care in teaching practices: learnings from the I(3) collaborative. Fam Med. 2011;43(7):495–502. [PubMed] [Google Scholar]
- 9.Dearinger AT, Wilson JF, Griffith CH, Scutchfield FD. The effect of physician continuity on diabetic outcomes in a resident continuity clinic. J Gen Intern Med. 2008;23(7):937–941. doi: 10.1007/s11606-008-0654-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Francis MD, Thomas K, Langan M, Smith A, Drake S, Gwisdalla KL, et al. Clinic design, key practice metrics, and resident satisfaction in internal medicine continuity clinics: findings of the Educational Innovations Project Ambulatory Collaborative. J Grad Med Educ. 2014;6(2):249–255. doi: 10.4300/JGME-D-13-00159.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Francis MD, Warm EJ, Julian KA, Rosenblum M, Thomas K, Drake S, et al. Determinants of patient satisfaction in internal medicine resident clinics: findings of the Educational Innovations Project Ambulatory Collaborative. J Grad Med Educ. 2014;6(3):470–477. doi: 10.4300/JGME-D-13-00398.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Francis MD, Wieland ML, Drake S, Gwisdalla KL, Julian KA, Nabors C, et al. Clinic design and continuity in internal medicine resident clinics: findings of the Educational Innovations Project Ambulatory Collaborative. J Grad Med Educ. 2015;7(1):36–41. doi: 10.4300/JGME-D-14-00358.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.HEDIS 2009 Volume 2 Technical Update. 2008 http://www.ncqa.org/portals/0/PolicyUpdates/HEDIS%20Technical%20Updates/09_CDC_Spec.pdf. Accessed October 22, 2015. [Google Scholar]
- 14.Breslau N, Reeb KG. Continuity of care in a university-based practice. J Med Educ. 1975;50(10):965–969. doi: 10.1097/00001888-197510000-00006. [DOI] [PubMed] [Google Scholar]
- 15.Steinwachs DM. Measuring provider continuity in ambulatory care: an assessment of alternative approaches. Med Care. 1979;17(6):551–565. doi: 10.1097/00005650-197906000-00001. [DOI] [PubMed] [Google Scholar]
- 16.Darden PM, Ector W, Moran C, Quattlebaum TG. Comparison of continuity in a resident versus private practice. Pediatrics. 2001;108(6):1263–1268. doi: 10.1542/peds.108.6.1263. [DOI] [PubMed] [Google Scholar]
- 17.McBurney PG, Moran CM, Ector WL, Quattlebaum TG, Darden PM. Time in continuity clinic as a predictor of continuity of care for pediatric residents. Pediatrics. 2004;114(4):1023–1027. doi: 10.1542/peds.2003-0280-L. [DOI] [PubMed] [Google Scholar]
- 18.Bowen JL, Hirsh D, Aagaard E, Kaminetzky CP, Smith M, Hardman J, et al. Advancing educational continuity in primary care residencies: an opportunity for patient-centered medical homes. Acad Med. 2015;90(5):587–593. doi: 10.1097/ACM.0000000000000589. [DOI] [PubMed] [Google Scholar]


