Abstract
Background
Mastery in performing carpal tunnel release (CTR) and hand fracture procedures is an essential component of orthopaedic residency training.
Objective
To assess orthopaedic resident case log data for temporal trends in CTR and hand fracture cases and to determine the degree of variability in case volume among residents.
Methods
Accreditation Council for Graduate Medical Education orthopaedic surgery resident case logs were reviewed for graduation years 2007 through 2014. Annual data regarding the mean number of CTR and hand fracture/dislocation procedures were recorded, as well as the median number of procedures reported by the top and bottom 10% of residents (by case volume). Temporal trends were assessed using linear regression modeling.
Results
There was no change in the mean number of CTRs performed per resident. Over the 8-year period, the top 10% of residents performed a significantly greater number of CTRs than the bottom 10% (62.1 versus 9.3, P < .001). Similarly, no change was noted in the mean number of total hand fracture/dislocation cases performed, with the top 10% of residents performing significantly more hand fracture cases than the bottom 10% (47.1 versus 9.3, P < .001).
Conclusions
Our results indicate no change in CTR and hand fracture caseload for orthopaedic residents. However, as resident experience performing both procedures varies significantly, this variability likely has important educational implications.
What was known and gap
All orthopaedic surgery residents must gain competence in carpal tunnel release (CTR) and hand fracture procedures.
What is new
Over the past 8 years, average CTR and hand fracture surgery experience has been stable.
Limitations
Reliance on resident self-reporting of case logs; inability to differentiate among levels of case involvement and different CTR procedures.
Bottom line
Despite stable average case volume, resident experience in both procedures is variable, which likely has educational implications.
Introduction
Carpal tunnel release (CTR) is the most common upper-extremity procedure submitted for Part II of the American Board of Orthopaedic Surgery (ABOS) certification examination.1 CTR is also 1 of 15 procedures with a minimum caseload required by the Accreditation Council for Graduate Medical Education (ACGME) for graduating orthopaedic surgery residents.2 Furthermore, CTR is a required educational topic in the Orthopaedic Surgery Milestone Project, a joint venture between the ACGME and ABOS for the evaluation of educational progress in orthopaedic surgery residents.3
Similarly, hand fracture cases have been identified as important components of orthopaedic surgery residents' education in trauma care.4 Management of these injuries, which account for up to 10% of axial skeleton fractures, is a key component of hand surgery education during orthopaedic residency.5,6 Despite both being educational foci of orthopaedic training, no analyses of CTR or hand fracture case volume have been published.
The objective of this study was to assess orthopaedic resident case log data for temporal trends in performing CTR and hand fracture cases, and to assess case volumes for variability among residents. This study is of interest because procedural case volume is a topic of importance for resident education in several specialties.7–9 Additionally, the methodology of our study may serve as a blueprint for assessments of resident caseload in other surgical specialties.
Methods
We reviewed national orthopaedic surgery resident ACGME case logs for graduation years 2007 through 2014. ACGME case logs are based on primary role procedures logged via current procedural terminology codes by residents.10 Primary role procedures were defined by the ACGME as Level I (primary or supervising resident surgeon) or Level II (assisting resident surgeon).11 The ACGME publishes annual reports of orthopaedic surgery resident case log data from the graduating residents, representing the number of cases performed during a trainee's entire residency. These reports are publicly available and provide information regarding the numbers and types of orthopaedic cases performed by residents during training.
Hand fracture and CTR cases were examined because they are essential hand surgery procedures that should be mastered by all graduating orthopaedic surgery residents,5 and the ACGME requires that orthopaedic residents perform at least 10 CTRs during residency.2 For this study, we reviewed annual data on the mean numbers of adult and pediatric cases involving CTR and hand fracture and dislocation procedures. The ACGME case logs classified carpometacarpal joint, metacarpal, metacarpophalangeal joint, phalangeal, and interphalangeal joint fracture cases as hand fracture procedures, and they also reported the total annual number of graduating orthopaedic residents and the total annual number of orthopaedic residency programs. The median number of procedures reported by the top 10% and bottom 10% of residents (by case volume) was also noted.
Statistical analysis was performed with JMP Pro 10 software (SAS Institute Inc, Cary, NC). Temporal trends were assessed using linear regression modeling. The median number of procedures reported by the top 10% and bottom 10% of residents from 2007 through 2014 was compared using Student t tests. The level of significance for all tests was P < .05.
Results
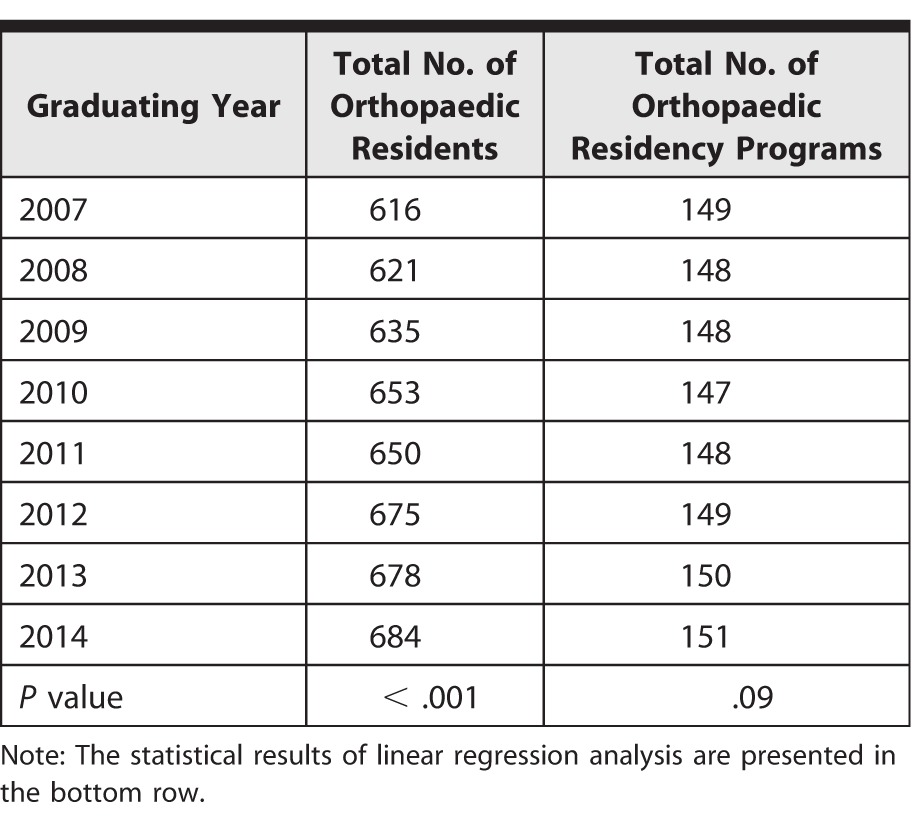
From 2007 through 2014, the total number of annual graduating orthopaedic residents significantly increased from 616 to 684 (P < .001). Concurrently, there was no change in the total number of orthopaedic residency programs during the study period (149 to 151, P = .09; table 1).
TABLE 1.
Total Annual Number of Graduating Orthopaedic Residents and Total Annual Number of Orthopaedic Residency Programs (2007–2014)
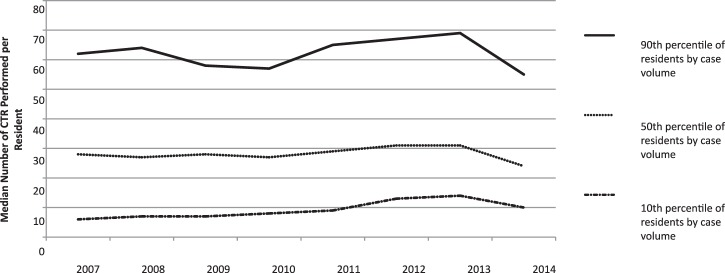
There was no significant change in the mean number of CTRs per resident between 2007 and 2014 (32.8 to 28.9, P = .79; table 2). The number of adult (32.4 to 28.7, P = .77) and pediatric (0.3 to 0.2, P = .80) CTR cases remained unchanged. The median number of CTRs performed by residents in the top 10% by case volume did not change (62 to 55, P = .88), although CTR case volumes for the bottom 10% of residents increased from 6 to 10 (P = .01; figure 1). Over the 8-year study period, the top 10% of residents performed a significantly greater number of CTRs than the bottom 10% (62.1 versus 9.3, P < .001).
TABLE 2.
Mean Number of Adult and Pediatric Carpal Tunnel Releases (CTRs) and Hand Fracture Cases Performed per Resident (2007–2014)
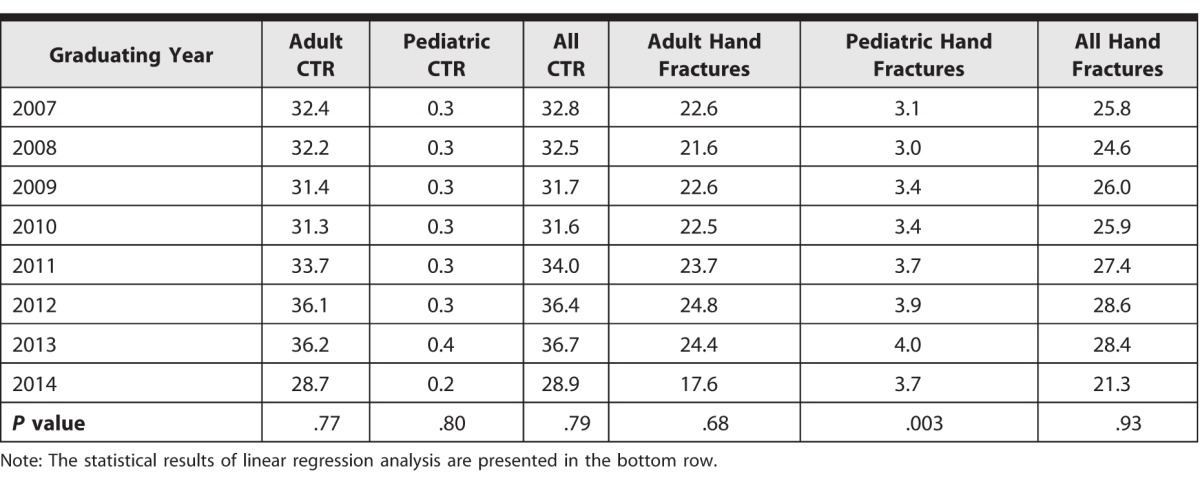
FIGURE 1.
Median Number of Carpal Tunnel Releases (CTRs) Performed per Resident in the 90th, 50th, and 10th Percentiles of Case Volume (2007–2014)
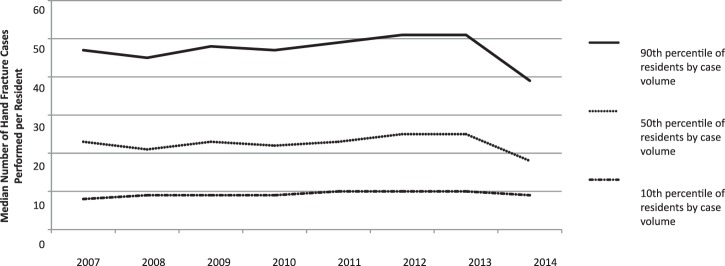
FIGURE 2.
Median Number of Hand Fracture Cases Performed per Resident in the 90th, 50th, and 10th Percentiles of Case Volume (2007–2014)
There was no change in the mean number of hand fracture cases per resident from 2007 through 2014 (25.8 to 21.3, P = .93), and the number of adult cases also remained unchanged (22.6 to 17.6, P = .68; table 2). The number of pediatric cases per resident increased significantly from 3.1 in 2007 to 3.7 in 2014 (P = .003). The median number of hand fracture procedures performed by the top 10% of residents did not change over this time period (47 to 39, P = .79), and the bottom 10% of residents also experienced no change in median case volume (8 to 9, P = .08; figure 2). The top 10% of residents performed significantly more hand fracture cases than the bottom 10% (47.1 versus 9.3, P < .001).
Discussion
Our study showed differences in case volume for the top 10% and the bottom 10% of residents for CTR (62.1 versus 9.3) and hand fracture procedures (47.1 versus 9.3). We also found no significant changes in the mean number of CTR and hand fracture cases for residents over the 8-year study period. The literature12–14 shows that the incidence of hand fractures is decreasing, while the rates of carpal tunnel syndrome and CTR are increasing. A recent study12 of the incidence of CTR in the United States found a decline in CTR in hospital-based surgical centers and a nearly 5-fold increase in CTR performed in freestanding ambulatory surgical centers. Stagnant resident CTR case volume in our study may be due to an increase in CTRs performed in surgical centers where resident training may not occur.15
In our study, orthopaedic residents performed an average of 3.5 pediatric hand fracture cases during their training, accounting for approximately 14% of all resident hand fracture cases. Children aged 5 to 14 have a hand fracture incidence of 546 per 100 000, and comprise a reported 2.3% of all emergency room visits.16,17 Although the high incidence of pediatric hand fractures does not necessarily translate to increased operative case volume, the minimal caseload revealed in our study (3.5 cases per graduating resident) suggests a relative paucity of operative pediatric hand fracture experience among residents. Nonetheless, our study did demonstrate a statistically significant increase in pediatric hand fracture case volume.
There was a 6.7-fold difference in the median number of CTRs performed between residents in the 90th and 10th percentiles by case volume. Similarly, residents in the 90th percentile of hand fracture caseloads performed nearly twice the number of procedures as residents in the 10th percentile. These findings highlight significant disparities in case volume among trainees, which likely has important educational implications.
A forum of orthopaedic surgery program directors noted the importance of case volume in building core orthopaedic knowledge,18 and the literature19 also indicated that case volume is used as a proxy to assess competency. If this is the case, residents with lower case volumes may be at a substantial disadvantage to acquire the necessary procedural proficiency compared to colleagues who have higher case numbers.
Causes of resident caseload disparity are likely multifactorial. Local disease/injury prevalence, the number of orthopaedic residents in the program, seasonality, and duration of the hand surgery rotation all may affect residents' case volumes. Additionally, the postgraduate level in which the hand surgery rotation occurs also may influence opportunities to perform primary role procedures.1 Finally, subspecialty interests may strongly dictate procedural experience during senior resident years.
We found that only in 2012 did the bottom 10% of graduating residents begin to perform more than 10 CTR procedures during training. This increase may have been due to residency program efforts to meet the ACGME-required minimum20 of 10 CTR procedures set in 2013. A survey21 found that this minimum is seen as appropriate by residents, with 78% of orthopaedic resident responders indicating that a minimum of 10 CTRs was “on target.” We found a significant increase in the number of CTR procedures performed by residents in the lower percentiles over the last 8 years. Our findings demonstrate that implementation of minimum case requirements can result in increased resident caseload.
Our study has limitations. ACGME case logs do not fully show the actual procedural experience of orthopaedic residents, as residents may overreport or underreport procedures due to poor recall and inappropriate procedure unbundling. Additionally, the ACGME case log reports do not differentiate between Level I (primary or supervising resident surgeon) or Level II (assisting resident surgeon) procedures, open and endoscopic CTR, or the anatomic locations of hand fracture fixation.
Future studies are needed to assess potential causes of CTR and hand fracture caseload variability among residents. Correlation of resident case volume with other measures of performance may be needed to quantitatively determine the educational impact of caseload variability.
Conclusion
Our results indicate no significant change in average per-resident CTR and hand fracture caseload during the study period. Resident experience performing both procedures shows significant variability; this likely has important educational implications.
Footnotes
Richard M. Hinds, MD, is Research Fellow, Department of Orthopaedic Surgery, New York University Hospital for Joint Diseases; Michael B. Gottschalk, MD, is Assistant Professor, Department of Orthopaedics, Emory University School of Medicine; and John T. Capo, MD, is Professor, Department of Orthopaedic Surgery, New York University Hospital for Joint Diseases.
Funding: The authors report no external funding source for this study.
Conflict of interest: The authors declare they have no competing interests.
References
- 1.VanHeest A, Kuzel B, Agel J, Putnam M, Kalliainen L, Fletcher J. Objective structured assessment of technical skill in upper extremity surgery. J Hand Surg Am. 2012;37(2):332–337.e1. doi: 10.1016/j.jhsa.2011.10.050. –e4. [DOI] [PubMed] [Google Scholar]
- 2.Accreditation Council for Graduate Medical Education. ACGME orthopaedic surgery minimum numbers. 2015 https://www.acgme.org/acgmeweb/Portals/0/PFAssets/ProgramResources/260_ORS_Case_Log_Minimum_Numbers.pdf. Accessed September 25. [Google Scholar]
- 3.Stern PJ, Albanese S, Bostrom M, Day CS, Frick SL, Hopkinson W, et al. Orthopaedic surgery milestones. J Grad Med Educ. 2013;5(1 suppl 1):36–58. doi: 10.4300/JGME-05-01s1-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Born CT. Orthopaedic Trauma Association, Fellowship and Career Choices Committee. Resident education curriculum for orthopaedic trauma. J Orthop Trauma. 1999;13(6):441–455. doi: 10.1097/00005131-199908000-00010. [DOI] [PubMed] [Google Scholar]
- 5.Noland SS, Fischer LH, Lee GK, Hentz VR. Essential hand surgery procedures for mastery by graduating orthopedic surgery residents: a survey of program directors. J Hand Surg Am. 2013;38(4):760–765. doi: 10.1016/j.jhsa.2012.12.035. [DOI] [PubMed] [Google Scholar]
- 6.Baldwin PC, Wolf JM. Outcomes of hand fracture treatments. Hand Clin. 2013;29(4):621–630. doi: 10.1016/j.hcl.2013.08.013. [DOI] [PubMed] [Google Scholar]
- 7.Kane SM, Siddiqui NY, Bailit J, Blanchard MH. Duty hour restrictions, ambulatory experience, and surgical procedural volume in obstetrics and gynecology. J Grad Med Educ. 2010;2(4):530–535. doi: 10.4300/JGME-D-10-00076.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Curtis SH, Miller RH, Weng C, Gurgel RK. The effect of duty hour regulation on resident surgical case volume in otolaryngology. Otolaryngol Head Neck Surg. 2014;151(4):599–605. doi: 10.1177/0194599814546111. [DOI] [PubMed] [Google Scholar]
- 9.Nygaard RM, Daly SR, Van Camp JM. General surgery resident case logs: do they accurately reflect resident experience 2015] doi: 10.1016/j.jsurg.2015.04.022. ? [published online ahead of print June 11, J Surg Educ. doi: 10.1016/j.jsurg.2015.04.022. [DOI] [PubMed] [Google Scholar]
- 10.Accreditation Council for Graduate Medical Education. ACGME orthopaedic surgery case logs national data report. 2015 https://www.acgme.org/acgmeweb/Portals/0/OrthopaedicSurgery_National_Report_Program_Version.pdf. Accessed September 25. [Google Scholar]
- 11.Review Committee for Orthopaedic Surgery for the Accreditation Council for Graduate Medical Education. Case log guidelines. 2015 http://www.acgme.org/acgmeweb/portals/0/pfassets/programresources/260_case_log_guidelines.pdf. Accessed September 25. [Google Scholar]
- 12.Fajardo M, Kim SH, Szabo RM. Incidence of carpal tunnel release: trends and implications within the United States ambulatory care setting. J Hand Surg Am. 2012;37(8):1599–1605. doi: 10.1016/j.jhsa.2012.04.035. [DOI] [PubMed] [Google Scholar]
- 13.Feehan LM, Sheps SB. Incidence and demographics of hand fractures in British Columbia, Canada: a population-based study. J Hand Surg Am. 2006;31(7):1068–1074. doi: 10.1016/j.jhsa.2006.06.006. [DOI] [PubMed] [Google Scholar]
- 14.Dale AM, Harris-Adamson C, Rempel D, Gerr F, Hegmann K, Silverstein B, et al. Prevalence and incidence of carpal tunnel syndrome in US working populations: pooled analysis of six prospective studies. Scand J Work Environ Health. 2013;39(5):495–505. doi: 10.5271/sjweh.3351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dunning K, Liedtke E, Toedter L, Rohatgi C. Outpatient surgery centers draw cases away from hospitals, impact resident training volume. J Surg Educ. 2008;65(6):460–464. doi: 10.1016/j.jsurg.2008.07.011. [DOI] [PubMed] [Google Scholar]
- 16.Chung KC, Spilson SV. The frequency and epidemiology of hand and forearm fractures in the United States. J Hand Surg Am. 2001;26(5):908–915. doi: 10.1053/jhsu.2001.26322. [DOI] [PubMed] [Google Scholar]
- 17.Nellans KW, Chung KC. Pediatric hand fractures. Hand Clin. 2013;29(4):569–578. doi: 10.1016/j.hcl.2013.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Robbins L, Bostrom M, Craig E, Sculco TP. Proposals for change in orthopaedic education: recommendations from an orthopaedic residency directors' peer forum. J Bone Joint Surg Am. 2010;92(1):245–249. doi: 10.2106/JBJS.I.00210. [DOI] [PubMed] [Google Scholar]
- 19.Malangoni MA, Biester TW, Jones AT, Klingensmith ME, Lewis FR., Jr Operative experience of surgery residents: trends and challenges. J Surg Educ. 2013;70(6):783–788. doi: 10.1016/j.jsurg.2013.09.015. [DOI] [PubMed] [Google Scholar]
- 20.Salazar D, Schiff A, Mitchell E, Hopkinson W. Variability in Accreditation Council for Graduate Medical Education resident case log system practices among orthopaedic surgery residents. J Bone Joint Surg Am. 2014;96(3):e22. doi: 10.2106/JBJS.L.01689. [DOI] [PubMed] [Google Scholar]
- 21.Jeray KJ, Frick SL. A survey of resident perspectives on surgical case minimums and the impact on milestones, graduation, credentialing, and preparation for practice: AOA critical issues. J Bone Joint Surg Am. 2014;96(23):e195. doi: 10.2106/JBJS.N.00044. [DOI] [PubMed] [Google Scholar]