Abstract
Aims:
To assess the coping strategies and the relationship of coping with subjective burden and positive caregiving consequences as perceived by the caregivers of children and adolescents with Type-1 diabetes.
Design:
Cross-sectional assessment.
Setting:
Outpatient of Endocrinology Department.
Participants:
Forty-one parents of children and adolescents with Type-1 diabetes
Main Outcome Measure:
Ways of coping checklist (WCC), involvement evaluation questionnaire (IEQ) and scale for assessment of positive aspects of caregiving experience (scale for positive aspects of caregiving experience) to study the coping, burden and positive aspects of caregiving respectively.
Results:
On WCC, the highest score was obtained for seeking social support, followed by planful problem-solving. More frequent use of coping strategies of confrontation and escape-avoidance was associated with significantly higher score on the tension domain of IEQ. Those who more frequently used problem-solving and distancing had significantly higher scores on worrying-urging-I domain of IEQ. supervision domain of IEQ was associated with more frequent use of confrontation, self-control, social support, escape-avoidance and positive reappraisal. More frequent use of distancing and problem-solving were associated with lower caregiving personal gains. More frequent use of problem-solving was associated with higher caregiver satisfaction and lower scores in the domain of self-esteem and social aspects of caring.
Conclusion:
Caregivers of patients with Type-1 diabetes predominantly use adaptive coping strategies. Higher use of certain coping strategies is associated with negative and positive caregiving consequences.
Key words: Burden, caregiving, coping, positive caregiving experience, Type-1 diabetes
INTRODUCTION
Type-1 diabetes is a chronic disease, which usually starts early in life, impacting the individual in the growing years of his/her life, a time period that is treasured not only by the individual but also his/her parents. Due to early onset of the disease, the responsibility of care for the disorder falls on the family members, especially parents, who bring the children and adolescents to the hospital for consultation and are also involved in administration of insulin and overall management. Such close involvement leads to major disruption in the life of the parents, daily family functioning and management of the illness.[1,2,3,4,5,6,7] Parents experience a substantial shame, grief, guilt,[8] distress,[9] anxiety, depression[7,10,11,12,13] and poor quality of life.[7,10,13,14] Studies also suggest that use of disengagement coping strategies (avoidance, denial and wishful thinking) by mothers’ is related to maternal symptoms of anxiety and depression. Further, it is seen that use of coping strategies, like acceptance and distraction, influences the relationship of diabetes-related stress and psychological distress and that between diabetes-related stress and family conflict.[15] A previous study from our center showed that nearly two-third of parents (64%) of patients with Type-1 diabetes have psychological morbidity, and about one-third were diagnosed to have a psychiatric disorder.[16] Parents who more frequently used internalization and externalization as a coping mechanism to overcome the stress of chronic illness suffered from psychological morbidity. Parents with psychological morbidity had more dysfunction in social, personal and cognitive domains and also had significantly poorer quality of life in the domains of physical health, psychological health and general well-being domains.[16] Taken together, all these observations suggest that the parents of children and adolescent with diabetes are vulnerable to psychological stress and morbidity. Studies have shown that maternal psychological adjustment problems (i.e. distress) are associated with maladjustment in children with chronic health conditions.[17] Hence, it is important to understand how parents of children and adolescent with Type-1 diabetes appraise and cope with the stress of chronic illness.
Earlier caregiving was understood only as a stressful situation with only negative outcome on the parents in the form of burden, poor quality of life or psychological morbidity. In recent times, caregiving is understood in the “stress-appraisal-coping” framework as “caregiver's appraisal,” according to which the final perception of caregiving depends on the transaction between the person and the environment.[18] Accordingly, caregiver appraisal refers to the process by which a caregiver estimates the amount or significance of caregiving, in which she/he takes into consideration both the nature of the stressor and his or her resources to cope with the same. Therefore, the caregiving appraisal may be positive, negative, or neutral[19] and it consists of subjective cognitive and affective appraisals of the potential stressor and the efficacy of one's coping efforts.[20] Interventions that focus on improving the adaptive coping can thus improve the overall outcome of the caregiving and possibly have a positive impact on the care recipient.
In this background, this study aimed to assess the coping strategies used by the parents of children and adolescents with Type-1 diabetes. Additionally, an effort was made to study the relationship of coping with subjective burden and positive caregiving consequences as perceived by the parents of children and adolescents with Type-1 diabetes.
METHODOLOGY
The study was carried out at the outpatient services of the Department of Endocrinology of a tertiary care hospital. The study was approved by the Ethic Review Committee of the Institute. All the participants were recruited after obtaining written informed consent/assent. The inclusion criteria for the patients were diagnosis of Type-1 diabetes for at least 1-year, age ≤19 years and accompanied by a parent. To participate in the study, the parents/first-degree relatives were required to be able to read Hindi or English and to be involved in the care of the patient. Parents with a chronic physical illness in themselves were excluded. In case more than one caregiver was available, the one who spent the greatest time in the care of the patient was chosen.
INSTRUMENTS
Ways of coping checklist (revised)
Ways of coping checklist (WCC) (revised) was used to assess coping strategies used by the parents. WCC was developed by Folkman and Lazarus.,[21,22] and it consists of a checklist of problem-focused and emotional-focused responses. Problem-focused coping refers to activities through which problems are directly confronted, whereas emotional-focused coping refers to activities that reduce the degree of emotional distress induced by the stressful situation. This instrument consists of 66 items where each item has a brief description of a cognitive and behavioral strategy for coping with stressful events. Rating is done on a four-point scale with higher scores indicating more frequent use of that particular strategy by the individual while dealing with the specific stressful situation. The responder is asked to keep a specific stressful situation in mind that he/she may have experienced in the past week. The specific situation may have involved one's family, job, friends, or something else important to the person. The 66 items are grouped into eight coping subscales viz., confrontative coping, distancing, self-controlling, seeking social support, accepting responsibility, escape-avoidance, planful problem-solving, and positive reappraisal. The score on each subscale is obtained by the addition of the item scores. WCC has high reliability with Cronbach's alpha (a) score of 0.89. For this study, the total scores obtained in each domain were divided by number of items in the domain to get the mean scores in each domain that could be comparable.
Hindi version of involvement evaluation questionnaire
The involvement evaluation questionnaire (IEQ) consists of a series of interconnected domains that represent the possible consequences of caring for a family member with severe mental illness.[23,24] The instrument has been refined over several versions and has been translated into a number of languages. In a previous study from India, IEQ was adapted and translated into Hindi. Factor analysis of the Hindi IEQ yielded four subscales covering 29 items. These four factors were labeled as tension (10 items), worrying-urging-I (10 items), worrying-urging-II (6 items) and supervision (3 items). The Hindi-IEQ has been found to have significant Pearson's correlation coefficients (P < 0.05) and intra-class correlation coefficients for each item and subscales, indicating a satisfactory level of agreement between the Hindi and English versions. Test-retest reliability and split-half reliability of the Hindi-IEQ were found to be satisfactory.[25] The scale was modified for this study to assess the possible consequences of caring for a family member with diabetes.
Scale for positive aspects of caregiving experience
It consists of 44 items, which assess various aspects of positive caregiving experience covering four domains of positive caregiving that is, caregiving personal gains, motivation for caregiving role, caregiver satisfaction and self-esteem and social aspect of caring. Each item is rated on a five point rating scale (0–4). The scale has good internal consistency (Cronbach's alpha = 0.923), test-retest reliability (intra-class correlation coefficient = 0.81–0.99 for different items), cross-language reliability (intra-class correlation coefficient = 0.47–0.97 for different items), split half reliability (Guttmann split half coefficient was 0.834) and face validity (>90%). The mean score for each domain can be obtained by dividing the total score of the domain by the number of items included in the domain.[26]
Procedure
Patients fulfilling the inclusion and exclusion criteria for the study were approached for inclusion into the study. Those providing the assent (i.e. children and adolescents <12 years of age) or written informed consent were recruited. Informed consent was also obtained from the parents on behalf of the patients when the patient was <18 years of age. Additionally informed consent was obtained from the parents for their willingness to participate in the study. For the purpose of the study, the caregiver was defined as “a person who has been living with the patient and has been intimately involved in the care of the patient for at least 1-year that is, looking after her/his daily needs, supervising the medications, bringing the patient to the hospital, staying with the patient during inpatient stay and maintaining liaison with the hospital staff.” Socio-demographic and clinical profile of the consenting patients was recorded. The sociodemographic profile of the parents was noted. The parents were requested to complete the IEQ, scale for positive aspects of caregiving experience, and WCC-revised version. Parents who were not able to complete the questionnaires on their own were provided assistance by one of the researchers.
The data were analyzed using the SPSS-14 (Chicago, Illinois: SPSS Inc). Descriptive analysis involved calculation of frequency–percentages and mean-standard deviation (SD) for the discrete and continuous variables respectively. Comparisons were done using the Student's t-test and Chi-square test. Relationship between different variables was studied using Pearson's product moment correlation or Spearman's correlation test. In view of the multiple correlations and the small sample size, for the correlation analysis, P < 0.01 was considered as statistically significant.
RESULTS
Socio-demographic and clinical profile
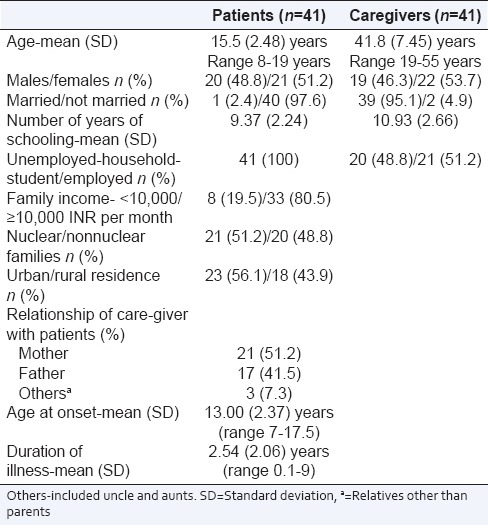
The study sample comprised of 41 children and adolescents and one of their parents. The mean age of the patients was 15.5 (SD 2.48; range 8–19) years and that of parents was 41.8 (SD 7.45; range 19–55) years. All the patients were single, whereas, most of the caregivers (95.1%) were currently married. There were more patients from urban background (56.1%). Nearly equal representation of patients from nuclear (51.2%) and nonnuclear families (48.8%) was found. Most of the patients (80.5%) came from families with monthly income in excess of Rupees 10,000. More commonly mothers (51.2%) were closely associated with care of the child though fathers (41.5%) were also closely involved in the care of the child and participated in the study. The mean age of onset of Type-1 diabetes in the study participants varied from 7 to 17.5 years with a mean of 13.00 (SD-2.37) years. The mean duration of illness at the time of assessment for the study was 2.54 (SD-2.06) years [Table 1].
Table 1.
Demographic and clinical profile of participants
Coping, caregiving burden and positive aspects of caregiving as perceived by the caregivers
As shown in Table 2, highest score on the WCC was obtained for seeking social support, followed by planful problem-solving, self-controlling, positive reappraisal, accepting responsibility, escape-avoidance, and distancing. The least score was obtained for the domain of using confrontative coping.
Table 2.
Coping, burden, positive aspects of caregiving, quality of life and social support as perceived by the caregivers
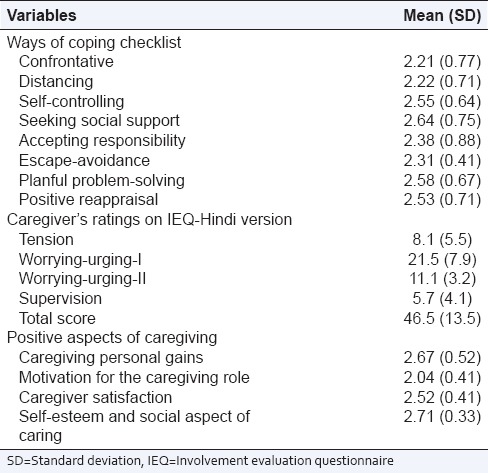
The mean Hindi IEQ score, indicating the caregivers own perception of the burden, was 46.5 (SD-13.5) with the highest score for worrying-urging-I domain followed by the domains of worrying-urging-II, tension and least for the supervision domain [Table 2].
With regard to the positive aspects of caregiving, the highest score was obtained for the domain of self-esteem and social aspect of caring followed by caregiving personal gains. Least score was obtained for the domain of motivation for the caregiving role [Table 2].
Relationship of coping with sociodemographic and clinical variables
No relationship was found between coping strategies used by parents and the age of patients, gender of patients, age of caregivers, education level of caregivers, family income, family type, duration of illness and age of onset, urban or rural background. No significant differences were found in the coping between the two parents.
Relationship between subjective burden and coping in caregivers
Caregivers who more frequently used coping strategies of confrontation and escape-avoidance had significantly higher score on the tension domain of IEQ [Table 3]. Those who more frequently used problem-solving had significantly higher scores on the worrying-urging-I and II domains of IEQ while those who used distancing coping had higher scores on worrying-urging-I domain only. Supervision was associated with more frequent use of confrontation, self-control, social support, escape and positive reappraisal [Table 3].
Table 3.
Relationship of coping with sociodemographic and clinical variables, burden, positive aspects of caregiving, quality of life and social support as perceived by the caregivers
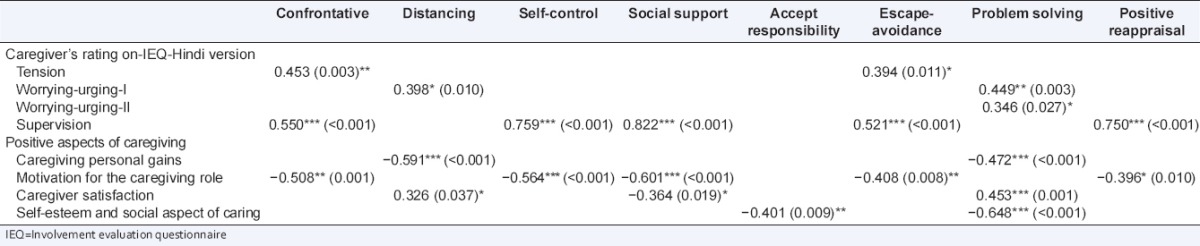
Relationship between positive aspects of caregiving and coping in caregivers
More frequent use of distancing and problem-solving were associated with lower caregiving personal gains. Lower use of confrontation, self-control, seeking social support, escape-avoidance and positive reappraisal were associated with better motivation for being in the caregiver's role. Higher caregiver satisfaction was associated with higher use of distancing and problem-solving and lower use of social support. Lower use of accepting responsibility and problem-solving was associated with higher self-esteem and social aspect of caring [Table 3].
DISCUSSION
In recent times, stress-appraisal-coping paradigm has been used to understand the evaluation of the caregiving experience by an individual. As per this paradigm, the experience of a stressful situation is modified by an individual's coping skills. It can be hoped that by promoting adaptive coping, appraisal of the caregiving experience can be tilted toward a more positive caregiving experience, which can help in preventing burnout in the caregivers and enhance their motivation. This may possibly improve the care provided to the diabetic children and adolescents.
This was an exploratory study to understand the coping strategies used by the caregivers of children and adolescents when faced with stress of managing Type-1 diabetes mellitus. Findings suggest that caregivers use adaptive coping strategies like seeking social support and planful problem-solving quite frequently while dealing with this kind of stress. The questions used to assess coping strategy of seeking social support include “talked to someone to find out more about the situation,” “talked to someone who could do something concrete about the problem,” “I asked a relative or friend I respected for advice” etc., Higher use of the coping strategy of “using social support” by the parents, possibly reflects the cultural influence on the commonly used coping when faced with stress and reflects the typical Indian personality characteristic of interdependence. According to Varma,[27] Indians are more dependent on each other than their Western counterparts, and this creates a system of interdependence in which everyone leans on the other. The higher use of seeking social support also possibly reflects the family structure and family values of Indian tradition in which individualism is given much less importance than cohesion and togetherness. Higher use of planful problem-solving also indicates higher use of adaptive coping strategies in dealing with the stressors.
In this study, the negative caregiving consequences were assessed using Hindi version of IEQ, which is based on the stress-appraisal-coping model for assessment of caregiver burden.[20] The Hindi-IEQ was adapted to suit the assessment of caregiver burden in patients with Type-1 diabetes. In the present study, the rank order of scores obtained in the various domains (worrying-urging-I > worrying-urging-II > tension > supervision) was very similar to that seen in previous studies from our center evaluating the caregiving experience in patients with schizophrenia and affective disorders.[25,28,29] The mean IEQ score obtained in the present study is slightly less than the previous study evaluating the caregivers of patients with severe mental disorders,[25,28] but is very similar to that seen in a previous study from our center[29] evaluating the caregivers of schizophrenia. Notwithstanding the patient profile, the comparative findings suggest that caregivers of patients with chronic mental as well as physical illness possibly appraise the caregiver's role in the similar manner.
In the present study, on the scale of positive aspects of caregiving experience, highest score was obtained for the domain of “self-esteem and social aspect of caring” followed by the domains of “caregivers personal gains,” “caregiver satisfaction” and the least score was obtained for the domain of “motivation for the caregiving role.” A previous study from our center, which evaluated the positive aspect of caregiving experience of caregivers of schizophrenia showed highest mean scores for the domain of “motivation for the caregiving role,” followed by caregiver satisfaction, caregiver personal gains and the least score for the domain of self-esteem and social aspect of caring.[29] These differences could possibly be due to the differences in the caregiver profile and the personality of caregivers who took up the caregiver's role in different illnesses.
There are occasional studies[30] that focus on the burden of caregivers of Type-1 diabetes, but there is a paucity of national or international literature that focuses on the positive caregiving experience in this group of patients. The findings of burden obtained in the present study could not be compared with the existing literature because of the significant difference in the conceptual understanding of the burden as assessed in the present study. Therefore, we do not have any comparative data that would help to put our findings in better perspective. Keeping this in mind, we have tried to understand the findings of the relationship of coping and caregiving experience in the socio-cultural milieu.
Relationship of coping with burden as assessed by involvement evaluation questionnaire-Hindi
Negative appraisal of caregiving as “tension” was associated with significantly more frequent use of coping strategies of confrontation and escape-avoidance. The confrontation domain of coping strategies include questions like “tried to get the person responsible to change his or her mind,” “I expressed anger to the person(s) who caused the problem,” “I let my feelings out somehow” and “took a big chance or did something very risky,” etc., Using the confrontation coping strategies, the caregivers actually indulge in risky behavior and indulge in interpersonal problems, which ultimately lead to higher perception of “tension.” Keeping this in mind, physicians dealing with the caregivers of patients with Type-1 diabetes should be supportive and try to listen to them rather than blaming the caregivers or confronting them. Similarly, those caregivers who are less involved, suggesting higher use of “escape-avoidance,” should be encouraged to get involved in the care of patients in such a way that the caregivers feel that they can contribute to the care of their children. This could be achieved by educating them as to how to deal with day to-day problems associated with the illness and how to use problem-solving skills more often to avoid distress.
The relationship between problem-solving and the two worrying-urging domains of IEQ suggest that the problem solving as a coping has a reciprocal relationship with worrying-urging. Parents who worry more about their children with diabetes and those who urge their children more frequently, make efforts to resolve the issues related to the disease and hence tend to look for amicable solutions for the same. This also possibly reflects higher involvement of the caregivers in taking care of their patients. In the present study, it was also evident that those caregivers who used distancing more frequently had higher scores in the domain of worrying-urging. The distancing domain of WCC has statements like “didn’t let it get to me; refused to think too much about it; looked for the silver lining, so to speak; tried to look on the bright side of things”. It can be hypothesized that higher level of involvement leads to higher level of experience of worrying-urging, therefore, to overcome the same, parents use distancing as an adaptive coping strategy.
Higher level of supervision of the sick relative is associated with more frequent use of confrontation, self-control, seeking social support, escape-avoidance and positive reappraisal. An individual who attempts to supervise someone (and in this case, a growing adolescent), would need these coping skills of confrontation and self-control to deal with the situation. The ability to maintain the parental role of supervision possibly enhances the positive reappraisal as demonstrated by the items in this domain which include statements like, “I changed something about myself” or “rediscovered what is important in life.” The correlation of escape-avoidance is also understandable as the constant need for injectable insulin, frequent blood glucose level monitoring (and the everyday needle pricks associated with the same) can make any caregiver who supervises such tasks to “hope a miracle would happen” or “wish that the situation would go away or somehow be over with.”
Relationship between positive aspects of caregiving and coping in caregivers
It was seen that more frequent use of problem-solving was associated with higher caregiver satisfaction and lower scores in the domains of caregiving personal gains, self-esteem and social aspects of caring. While the relationship of this coping skill with caregiver satisfaction is understandable, it is the negative correlation with the other two domains that is concerning. The traditionally adaptive coping skill of problem-solving possibly fails in our caregivers because of the dearth of information and facilities available to the patients and their parents. Hence, it is possible that those caregivers who attempt to use problem-solving to deal with their problems often end up feeling frustrated and dejected. Additionally, it was seen that more frequent use of distancing was also associated with lower caregiving personal gains. As discussed earlier, distancing basically involves efforts to take away oneself from the stressful situation. It is quite possible that those caregivers who are effectively able to use distancing don’t perceive their caregiver role as very stressful, and hence also do not perceive any caregiving gains.
Higher use of confrontation, self-control, seeking social support, escape-avoidance and positive reappraisal are associated with lower motivation for being in the caregiver's role. The relationship of higher use of self-control and lower motivation is quite understandable considering the fact that self-control as a means of coping may not be a very adaptive way of dealing with stress and may be a demotivating factor to be in the caregiver role. The same is supported by the observation discussed earlier of positive correlation between self-control coping and IEQ domain of tension. Motivation for caregiving also decreases with more use of confrontative coping. Confrontation is often associated with negative emotions, thus, leading to a dip in the motivation for the caregiving role. Seeking social support is also negatively correlated with poor motivation for taking up caregiving role. One can hypothesize that those individuals who have an inherent motivation for the caregiving role would not need social encouragement and support for the same. Another possible explanation could be that although the parents seek social support, they often do not receive the required amount of the same, and this in turn possibly demotivates them from being in the caregivers’ role. Lower use of accepting-responsibility and problem-solving is associated with higher self-esteem and social aspect of caring. Problem-solving as a coping strategy leads to resolution of the problem with a sense of accomplishment and increased self-esteem. Lower use of accepting-responsibility could lead to lower level of perceived stress and possibly lower level of frustration. Resultantly, such caregiving may maintain higher self-esteem.
Certain limitations must be taken into consideration while interpreting the results of this study. Only 41 patients and their caregivers attending the outpatient services of the Department of Endocrinology were included, hence, the findings cannot be generalized to the caregivers in the community. The instruments used for assessment of positive aspects of caregiving and burden have been validated for the caregivers of patients with psychiatric disorders. There is a need to validate these instruments in the caregivers of patients with chronic physical disorders. We also did not evaluate the level of involvement of the caregivers (i.e. time spent in caregiving) and the personality of the caregivers, which can influence the level of coping and the caregiving experience. Future studies must attempt to overcome these limitations.
To conclude, this study demonstrates the coping strategies used by the caregivers of patients with Type-1 diabetes. Caregivers who use the adaptive coping skill of seeking social support are not found to have more positive caregiving experiences though they do experience caregiver burden. It seems that the caregivers who seek social support from various sources to overcome the stress of the caregiving possibly do not get the desired level of support, hence, end up perceiving the caregiving as a negative experience. Higher use of problem-solving is also associated with lower caregiver self-esteem, lesser caregiver gains and more caregiver burden. Taking these observations together, it is important for the treating agencies to provide adequate support to the caregivers and also encourage the caregivers to form mutual support groups. Further, the health care professionals involved in the care of patients with diabetes must teach effective coping skills like problem-solving to the caregivers to help them perceive the caregiving role as less stressful and more rewarding. The lack of scientific literature underlines our neglect toward the psychological aspects of children with such medical illnesses and their caregivers. Research should be directed to this area, for improving our understanding of such children and their parents. This would go a long way in providing holistic care to the children and adolescents with Type-1 diabetes.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Rubin R, Young-Hyman D, Peyrot M. Parent–child responsibility and conflict in diabetes care. Diabetes. 1989;38(Suppl 2):28. [Google Scholar]
- 2.Bobrow ES, AvRuskin TW, Siller J. Mother-daughter interaction and adherence to diabetes regimens. Diabetes Care. 1985;8:146–51. doi: 10.2337/diacare.8.2.146. [DOI] [PubMed] [Google Scholar]
- 3.Hanson CL, Henggeler SW, Burghen GA. Social competence and parental support as mediators of the link between stress and metabolic control in adolescents with insulin-dependent diabetes mellitus. J Consult Clin Psychol. 1987;55:529–33. doi: 10.1037/0022-006X.55.4.529. [DOI] [PubMed] [Google Scholar]
- 4.Hanson CL, Henggeler SW, Harris MA, Burghen GA, Moore M. Family system variables and the health status of adolescents with insulin-dependent diabetes mellitus. Health Psychol. 1989;8:239–53. doi: 10.1037//0278-6133.8.2.239. [DOI] [PubMed] [Google Scholar]
- 5.Schafer LC, McCaul KD, Glasgow RE. Supportive and nonsupportive family behaviors: relationships to adherence and metabolic control in persons with type I diabetes. Diabetes Care. 1986;9:179–85. doi: 10.2337/diacare.9.2.179. [DOI] [PubMed] [Google Scholar]
- 6.Wysocki T, Buckloh LM, Lochrie AS, Antal H. The psychologic context of pediatric diabetes. Pediatr Clin North Am. 2005;52:1755–78. doi: 10.1016/j.pcl.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 7.Malerbi FE, Negrato CA, Gomes MB. Brazilian Type Diabetes Study Group (BrazDiabSG). Assessment of psychosocial variables by parents of youth with type 1 diabetes mellitus. Diabetol Metab Syndr. 2012;22(4):48. doi: 10.1186/1758-5996-4-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Frank MR. Psychological issues in the care of children and adolescents with type 1 diabetes. Paediatr Child Health. 2005;10:18–20. [PMC free article] [PubMed] [Google Scholar]
- 9.Hilliard ME, Monaghan M, Cogen FR, Streisand R. Parent stress and child behaviour among young children with type 1 diabetes. Child Care Health Dev. 2011;37:224–32. doi: 10.1111/j.1365-2214.2010.01162.x. [DOI] [PubMed] [Google Scholar]
- 10.Aloulou J, Damak R, Ben Ammar H, Hachicha M, Amami O. Psychological impact of juvenile-onset diabetes on parents. Soins Pediatr Pueric. 2012;269:34–8. [PubMed] [Google Scholar]
- 11.Grey M. Coping and Psychosocial Adjustment in Mothers of Young Children with Type 1 Diabetes. Child Health Care. 2009;38:91–106. doi: 10.1080/02739610902813229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hansen JA, Weissbrod C, Schwartz DD, Taylor WP. Paternal involvement in pediatric Type 1 diabetes: fathers’ and mothers’ psychological functioning and disease management. Fam Syst Health. 2012;30:47–59. doi: 10.1037/a0027519. [DOI] [PubMed] [Google Scholar]
- 13.Jaser SS, Whittemore R, Ambrosino JM, Lindemann E, Grey M. Mediators of depressive symptoms in children with type 1 diabetes and their mothers. J Pediatr Psychol. 2008;33:509–19. doi: 10.1093/jpepsy/jsm104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Farnik M, Brozek G, Pierzchala W, Zejda JE, Skrzypek M, Walczak L. Development, evaluation and validation of a new instrument for measurement quality of life in the parents of children with chronic disease. Health Qual Life Outcomes. 2010;23(8):151. doi: 10.1186/1477-7525-8-151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jaser SS, Linsky R, Grey M. Coping and psychological distress in mothers of adolescents with type 1 diabetes. Matern Child Health J. 2014;18:101–8. doi: 10.1007/s10995-013-1239-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bhadada S, Grover S, Kumar S, Bhansali A, Jaggi S. Psychological impact of type-1 diabetes on parents: an exploratory study from North India. Int J Diabetes Dev Ctries. 2011;31:174–9. [Google Scholar]
- 17.Drotor D. Relating parent and family functioning to the psychological adjustment of children with chronic health conditions: what have we learned? What do we need to know. J Pediatr Psychol. 1997;22:149–65. doi: 10.1093/jpepsy/22.2.149. [DOI] [PubMed] [Google Scholar]
- 18.Lazarus R, Folkman S. New York: Springer; 1984. Stress, Appraisal, and Coping. [Google Scholar]
- 19.Kinsella G, Cooper B, Picton C, Murtagh D. A review of the measurement of caregiver and family burden in palliative care. J Palliat Care. 1998;14:37–45. [PubMed] [Google Scholar]
- 20.Lawton MP, Kleban M, Moss M, Rovine M, Glicksman A. Measuring caregiving appraisal. J Gerontol Psychol Sci. 1989;44:61–71. doi: 10.1093/geronj/44.3.p61. [DOI] [PubMed] [Google Scholar]
- 21.Folkman S, Lazarus RS. An analysis of coping in a middle-aged community sample. J Health Social Behav. 1980;21:219–39. [PubMed] [Google Scholar]
- 22.Folkman S, Lazarus RS, Dunkel-Schetter C, DeLongis A, Gruen R. The dynamics of a stressful encounter: Cognitive appraisal, coping and encounter outcomes. J Personality Soc Psychol. 1986;50:992–1003. doi: 10.1037//0022-3514.50.5.992. [DOI] [PubMed] [Google Scholar]
- 23.Schene AH, van Wijngaarden B, Koeter MW. Family caregiving in schizophrenia: domains and distress. Schizophr Bull. 1998;24:609–18. doi: 10.1093/oxfordjournals.schbul.a033352. [DOI] [PubMed] [Google Scholar]
- 24.van Wijngaarden B, Schene AH, Koeter M, Vázquez-Barquero JL, Knudsen HC, Lasalvia A, et al. Caregiving in schizophrenia: development, internal consistency and reliability of the Involvement Evaluation Questionnaire – European Version. EPSILON Study 4. European Psychiatric Services: Inputs Linked to Outcome Domains and Needs. Br J Psychiatry Suppl. 2000;39:s21–7. doi: 10.1192/bjp.177.39.s21. [DOI] [PubMed] [Google Scholar]
- 25.Grover S, Chakrabarti S, Ghormode D, Dutt A, Kate N, Kulhara P. Psychometric properties and factor structure of Caregiver Involvement Evaluation Questionnaire (IEQ) in Indian setting. East Asian Arch Psychiatry. 2011;21:142–51. [PubMed] [Google Scholar]
- 26.Kate N, Grover S, Kulhara P, Nehra R. Scale for positive aspects of caregiving experience: development, reliability, and factor structure. East Asian Arch Psychiatry. 2012;22:62–9. [PubMed] [Google Scholar]
- 27.Varma VK. Transcultural psychiatry. In: Vyas JN, Ahuja N, editors. Texkbook of Postgraduate Psychiatry. 2nd ed. New Delhi: Jaypee Brothers Medical Publishers (P) Ltd; 1999. [Google Scholar]
- 28.Grover S, Chakrabarti S, Ghormode D, Dutt A, Kate N, Kulhara P. Clinicians’ versus caregivers’ ratings of burden in patients with schizophrenia and bipolar disorder. Int J Soc Psychiatry. 2013;60:330–336. doi: 10.1177/0020764013488708. [DOI] [PubMed] [Google Scholar]
- 29.Kate N, Grover S, Kulhara P, Nehra R. Relationship of caregiver burden with coping strategies, social support, psychological morbidity, and quality of life in the caregivers of schizophrenia. Asian J Psychiatr. 2013;6:380–8. doi: 10.1016/j.ajp.2013.03.014. [DOI] [PubMed] [Google Scholar]
- 30.Haugstvedt A, Wentzel-Larsen T, Rokne B, Graue M. Perceived family burden and emotional distress: Similarities and differences between mothers and fathers of children with type 1 diabetes in a population-based study. Pediatr Diabetes. 2011;12:107–14. doi: 10.1111/j.1399-5448.2010.00661.x. [DOI] [PubMed] [Google Scholar]


