Abstract
Immune reconstitution inflammatory syndrome is characterized by a paradoxical worsening of an existing infection or disease process, soon after initiation of highly active antiretroviral therapy. The first case of leprosy presenting as immune reconstitution inflammatory syndrome was published in 2003. Here we report a case of Hansen's disease borderline tuberculoid presenting with type 1 lepra reaction 5 months after initiation of highly active antiretroviral therapy.
Key words: Borderline tuberculoid Hansen's disease, HIV infection, immune reconstitution inflammatory syndrome, type 1 lepra reaction
INTRODUCTION
The cutaneous manifestations of leprosy in patients who are coinfected with leprosy and HIV are not different from those in conventional leprosy.[1] After the introduction of highly active antiretroviral therapy (HAART), the leprosy HIV coinfection has manifested itself as an immune reconstitution inflammatory syndrome (IRIS) or immune restoration disease or immune reconstitution disease. Some persons with HIV infection experience a clinical deterioration following initiation of antiretroviral therapy that is believed to be a consequence of the restored ability to mount an inflammatory response.[2] This has been described among HIV infected individuals coinfected with Mycobacterium tuberculosis, nontuberculous mycobacteria, cytomegalovirus, and hepatitis B and C viruses. The first report of leprosy presenting as IRIS was published by Lawn et al. in 2003.[3]
Here we report a case of Hansen's disease borderline tuberculoid presenting with manifestations of type 1 lepra reaction, one among the myriad manifestations of IRIS.
CASE REPORT
A 38-year-old male patient, diagnosed with retroviral infection and disseminated tuberculosis presented with weakness and numbness of the right hand of 2 weeks duration. He also noticed an edematous reddish raised lesion on the inner aspect of right hand, which he attributed to the topical agent he used for relieving the numbness. Pain was present on the right elbow and forearm. The patient had been on antitubercular therapy (ATT) followed by antiretroviral therapy (ART), 5 months prior to presentation at our department. The CD4 count was 67 cells/μL during initiation of HAART.
Dermatological examination showed a single well-defined erythematous plaque, 20 × 5 cm with raised borders on the ulnar aspect of right hand and distal forearm, extending to the palm [Figures 1 and 2]. A satellite lesion was present on the upper part of forearm, which also showed erythema and edema. All modalities of sensations were lost in these lesions. Both ulnar nerves were thickened with tenderness on the right side. Slit skin smears from the earlobe, lesional, and normal skin were negative. Histopathological examination showed dermal edema, diffuse granulomas composed of Langhans type giant cells, surrounded by epithelioid cells, lymphocytes, multinucleated giant cells, and fibroblasts with perivascular lymphocytic infiltrate, consistent with Hansen's disease borderline tuberculoid type, with features suggesting type 1 lepra reaction [Figures 3-6]. AFB stain was negative. CD4 count after 5 months showed a rise to 160 cells/μL. The viral RNA load was not measured due to lack of facilities.
Figure 1.

Erythematous plaque on the ulnar aspect of right hand
Figure 2.

Erythematous plaque extending to the palm
Figure 3.
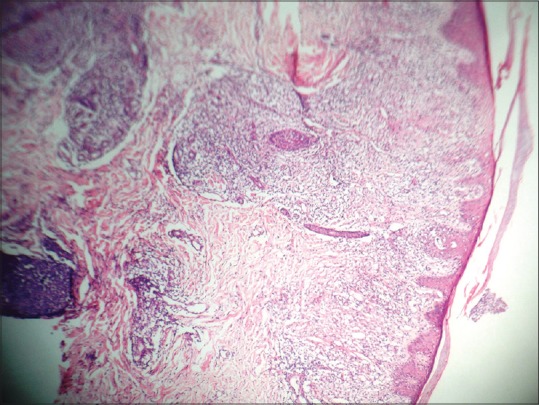
Diffuse granulomas in the dermis (H and E, ×40)
Figure 6.
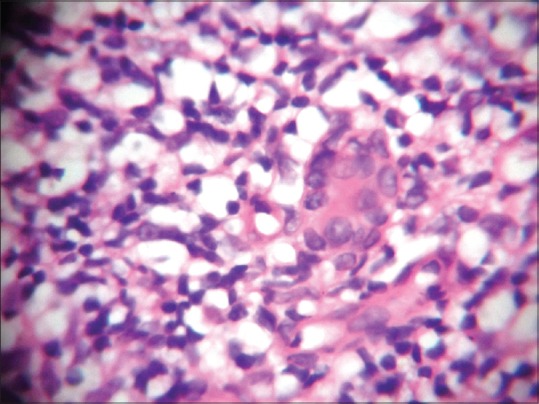
Granuloma surrounded by lymphocytes and epithelioid giant cells (H and E, ×100)
Figure 4.
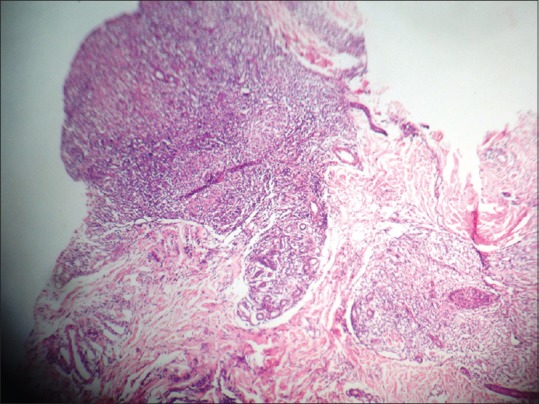
Dermal edema with Langhans giant cells, epithelioid cells and lymphocytes (H and E, ×40)
Figure 5.
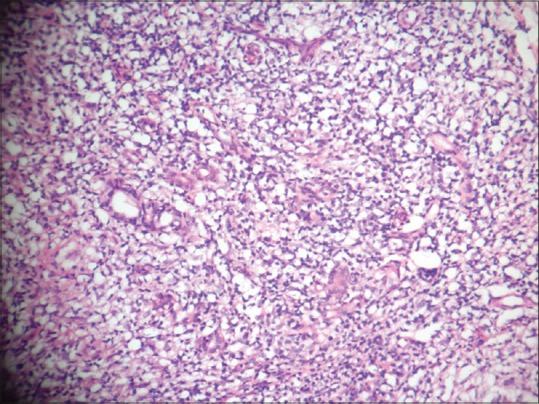
Section under high-power showing diffuse dermal edema and granulomas (H and E, ×40)
Thus correlating the clinical, bacteriological, and histopathological features, a diagnosis of Hansen's disease borderline tuberculoid with type 1 lepra reaction presenting as IRIS was made. MB-MDT was started, avoiding rifampicin from the regimen, as patient was also on ATT. HAART was continued and systemic steroids were also given in tapering doses. On follow up there was marked alleviation of his symptoms. However, the patient succumbed within 3 months to a brain tuberculoma.
DISCUSSION
IRIS is characterized by a paradoxical worsening of an existing infection or disease process, soon after initiation of HAART. The immunopathogenesis of the syndrome is unclear and appears to be the result of unbalanced reconstitution of effector cells and regulatory T cells, leading to exuberant inflammatory response in patients receiving ART. Biomarkers including INF-γ, TNFα, CRP, and IL-2, 6 and 7 are the subject of intense investigation at present. The most common forms of IRIS are associated with mycobacterial infections, fungi, and herpes viruses.
Certain minimum criteria should be fulfilled in order to diagnose IRIS. There must be temporal association between initiation of ART and subsequent development of symptoms (usually within 3 months), with evidence of immune restoration (viral and immunological response demonstrated by a decrease in plasma HIV RNA level by more than 1log10 copies/mL and an increase in CD4 T-cell count from baseline), and must exhibit clinical symptoms and signs consistent with an inflammatory process. The clinical course should neither be consistent with the usual course of a previously diagnosed opportunistic infection or a new infectious process, nor should the symptoms and signs be explained by drug toxicity.[4]
The first case of Hansen's disease presenting as IRIS was reported in 2003 by Lawn et al. in a previously healthy 37-year-old man from Uganda, who also had pulmonary tuberculosis.[3] Furthermore, there have been several reports of HIV and leprosy coinfections in which IRIS occurred after initiation of HAART. In the study by Pereira, et al., a significant percentage of co-infected patients were classified as the borderline tuberculoid leprosy.[5]
A review of the Indian scenario revealed only five cases of Hansen's disease presenting as IRIS. All were of the borderline tuberculoid type and were asspciated with type 1 lepra reaction.[6,7,8,9] Thus our case adds to the Indian scenario.
CONCLUSION
Our patient had pre-existing immunosuppression; features of lepra reaction occurred within 5 months of initiation of HAART. The diagnosis of Hansen disease borderline tuberculoid with type 1 lepra reaction in this patient indicates an improvement in the cell-mediated immunity, specifically the low CD4 count at initiation of HAART.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Massone C, Talhari C, Ribeiro-Rodrigues R, Sindeaux RH, Mira MT, Talhari S, et al. Leprosy and HIV coinfection: A critical approach. Expert Rev Anti Infect Ther. 2011;9:701–10. doi: 10.1586/eri.11.44. [DOI] [PubMed] [Google Scholar]
- 2.Robertson J, Meier M, Wall J, Ying J, Fichtenbaum CJ. Immune reconstitution syndrome in HIV: Validating a case definition and identifying clinical predictors in persons initiating antiretroviral therapy. Clin Infect Dis. 2006;42:1639–46. doi: 10.1086/503903. [DOI] [PubMed] [Google Scholar]
- 3.Lawn SD, Wood C, Lockwood DN. Borderline tuberculoid leprosy: An immune reconstitution phenomenon in a human immunodeficiency virus-infected person. Clin Infect Dis. 2003;36:e5–6. doi: 10.1086/344446. [DOI] [PubMed] [Google Scholar]
- 4.Sharma SK, Soneja M. HIV and immune reconstitution inflammatory syndrome (IRIS) Indian J Med Res. 2011;134:866–77. doi: 10.4103/0971-5916.92632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pereira GA, Stefani MM, Araújo Filho JA, Souza LC, Stefani GP, Martelli CM. Human immunodeficiency virus type 1 (HIV-1) and Mycobacterium leprae co-infection: HIV-1 subtypes and clinical, immunologic and histopathologic profiles in a Brazilian cohort. Am J Trop Med Hyg. 2004;71:679–84. [PubMed] [Google Scholar]
- 6.Kharkar V, Bhor UH, Mahajan S, Khopkar U. Type 1 lepra reaction presenting as immune reconstitution inflammatory syndrome. Indian J Dermatol Venereol Leprol. 2007;73:253–6. doi: 10.4103/0378-6323.33637. [DOI] [PubMed] [Google Scholar]
- 7.Rao GR, Amareswar A, Sandhya S. Can highly active antiretroviral therapy unmask leprosy?. A case of type 1 lepra reaction in a HIV-seropositive patient. Indian J Dermatol Venereol Leprol. 2012;78:101–3. doi: 10.4103/0378-6323.90959. [DOI] [PubMed] [Google Scholar]
- 8.Mehta S, Padhiar B, Shah B. Leprosy presenting as immune reconstitution inflammatory syndrome. Indian J Sex Transm Dis. 2008;29:96–7. [Google Scholar]
- 9.Mukhopadhyay P, Pal S, Mallik S, Biswas S, Saha B. Borderline tuberculoid leprosy: A manifestation of immune reconstitution inflammatory syndrome in a human immunodeficiency virus infected person. Indian J Dermatol. 2006;51:278–80. [Google Scholar]


