Sir,
Subcutaneous emphysema is an uncommon entity that may be associated with an underlying pneumothorax. Timely intervention in the form of early diagnosis and treatment is important to avoid a fatal outcome.[1,2] It may mimic angioedema, a common and often a relatively benign disorder thereby leading to inappropriate management.[3] We report a case of a 65-year-old man who was referred to the dermatology outpatient department for evaluation of progressively increasing facial swelling of two days duration associated with difficulty in breathing. There was no preceding history of drug intake. There was no history of any food allergy, drug allergy, or similar such episodes in the past. He was a chronic smoker and a known case of chronic obstructive pulmonary disease (COPD). He developed acute respiratory distress three days ago and was subsequently diagnosed as a case of angioedema by a dermatologist and was prescribed tablet prednisolone 40 mg daily and tablet hydroxyzine 25 mg thrice daily with no symptomatic improvement over the next two days. Physical examination revealed the presence of a diffuse facial swelling predominantly involving periorbital region and both cheeks extending down to the supraclavicular region and upper chest. However, there was distinct sparing of the lips, which prompted us to look for other clues and to consider other differentials. Crepitus could be elicited on palpation of the swollen areas., Chest radiograph (posteroanterior view), showed presence of opaque striations/shadows in the scapular region suggesting subcutaneous emphysema without any evidence of pneumothorax [Figure 1]. Therefore, a final diagnosis of subcutaneous emphysema, resulting probably from the rupture of an apical lung bulla in a patient with pre-existing COPD was made. The patient was referred to medical emergency where he was treated with anxiolytics, bronchodilators, and administered ventilation with 100% oxygen leading to remarkable improvement in respiratory distress and satisfactory reduction in facial swelling over next three days.
Figure 1.
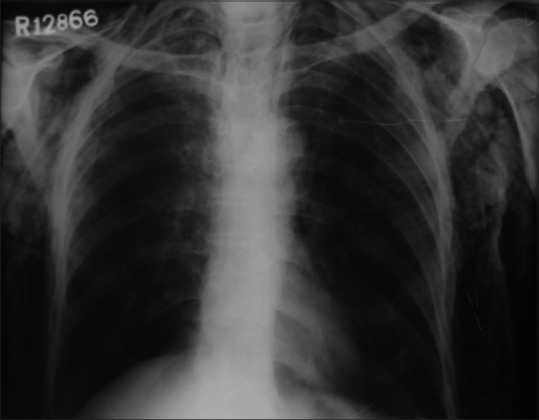
Chest radiograph posteroanterior view showing radiolucent shadows in scapular and subcutaneous region of upper chest
Subcutaneous emphysema results from entrapment of air into the subcutaneous tissues.[1,2] It can result from various causes including blunt or penetrating trauma to the chest or neck, following gastrointestinal perforation (corrosives burns of the esophagus, Boerhaave's syndrome, gas gangrene), diving injuries, endoscopy, tracheostomy, cryosurgery, dental surgery, or skin biopsy.[1,2,3,4,5,6,7] While reviewing the literature we came across only four reports of subcutaneous emphysema mimicking angioedema[3,4,5,7] where subcutaneous emphysema resulted from dental surgery in majority.[3,4] Subcutaneous emphysema may occur spontaneously as a result of increased pressure in the lungs due to rupture of alveoli, as might have happened in our patient. Subsequent to an injury or otherwise, air from the mediastinum and retroperitoneal spaces travels along the fascial planes to reach the subcutaneous region where it gets trapped, resulting in subcutaneous emphysema. Spontaneous subcutaneous emphysema may have varied clinical presentations depending on the cause, but is often associated with sudden onset dramatic swelling of the neck associated with chest pain, wheezing, dyspnea, and dysphagia.[2,7] Similarity of most of these symptoms to angioedema can lead to a misdiagnoses by the dermatologists. History of COPD along with characteristic sparing of lips and presence of crepitus on palpation prompted us to diagnose subcutaneous emphysema in our patient. Imaging techniques such as radiographs of the chest and neck regions have been used to visualize air in the subcutaneous spaces. Radiolucent striations in the subcutaneous tissues are seen in radiographs, whereas computed topography shows air as dark pockets along with the entry point of the air.[2,7] Subcutaneous emphysema usually has a benign course. Mild-to-moderate cases of subcutaneous emphysema may be dealt with by treatment of the predisposing factors, bed rest, anxiolytics, supplemental oxygen, and reassurance. Severe cases might require chest tube or insertion of catheter and positive pressure ventilation.[1,2] This report highlights the fact that subcutaneous emphysema is an uncommon but an important cause of facial swelling with respiratory distress that is likely to be misdiagnosed as angioedema, a commonly encountered dermatological condition.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Maunder RJ, Pierson DJ, Hudson LD. Subcutaneous and mediastinal emphysema. Pathophysiology, diagnosis, and management. Arch Intern Med. 1984;144:1447–53. [PubMed] [Google Scholar]
- 2.Pan PH. Perioperative subcutaneous emphysema: Review of differential diagnosis, complications, management, and anesthetic implications. J Clin Anesth. 1989;1:457–9. doi: 10.1016/0952-8180(89)90011-1. [DOI] [PubMed] [Google Scholar]
- 3.Frühauf J, Weinke R, Pilger U, Kerl H, Müllegger RR. Soft tissue cervicofacial emphysema after dental treatment: Report of 2 cases with emphasis on the differential diagnosis of angioedema. Arch Dermatol. 2005;141:1437–40. doi: 10.1001/archderm.141.11.1437. [DOI] [PubMed] [Google Scholar]
- 4.Haitz KA, Patel AJ, Baughman RD. Periorbital subcutaneous emphysema mistaken for unilateral angioedema during dental crown preparation. JAMA Dermatol. 2014;150:907–9. doi: 10.1001/jamadermatol.2014.478. [DOI] [PubMed] [Google Scholar]
- 5.Jensen P, Johansen UB, Thyssen JP. Cryotherapy caused widespread subcutaneous emphysema mimicking angiooedema. Acta Derm Venereol. 2014;94:241. doi: 10.2340/00015555-1663. [DOI] [PubMed] [Google Scholar]
- 6.Yadav P, Pandhi D, Singal A. Benign subcutaneous emphysema following punch skin biopsy. J Cutan Aesthet Surg. 2013;6:171–2. doi: 10.4103/0974-2077.118441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cakmak SK, Gönül M, Gül U, Kiliç A, Demirel O. Subcutaneous emphysema mimicking angioedema. J Dermatol. 2006;33:902–3. doi: 10.1111/j.1346-8138.2006.00207.x. [DOI] [PubMed] [Google Scholar]


