Abstract
Background:
Glomus tumor is a common lesion of the subungual area of the hand fingers. However, glomus tumors located outside the hand region are rare and the diagnosis is often difficult due to their low incidence and lack of distinct clinical features in the physical examination. The presented article contains five cases of extradigital glomus tumors with a short review of the literature.
Patients and Methods:
Five cases of extradigital glomus tumor were included in the study. All lesions were purple colored subcutaneous nodules with sharp pain by digital palpation. All lesions were examined with ultrasound imaging were operated under local anesthesia using loupe magnification.
Results:
Among five patients, only one patient was female with a mean age of 35. Two lesions were located at the arm region, two at the crural region and one at the sternal area. The smallest nodule was 0.5 cm and the biggest lesion was 2 cm in diameter. In all the cases, the early postoperative period was uneventful without any surgical complication or acute recurrence. The postoperative 1st year examination of all patients revealed complete resolution of the pain and no recurrence was encountered.
Conclusions:
Glomus tumor should be kept in mind in the differential diagnosis of all painful subcutaneous lesions especially for those with purple reflection on the skin surface. In this manner, patients with extradigital glomus tumors may be diagnosed earlier and unnecessary and wrong treatments may be prevented.
Keywords: Extradigital glomus tumor, glomus tumor, painful nodule, purple skin reflection, subcutaneous nodule
Introduction
What was known?
Glomus tumor is common lesion arising from the perivascular structures
The most common location of the lesion is the subungual area of the hand fingers
Extradigital presentation of the gloms tumors is rare and frequently misdiagnosed.
Subcutaneous tissue is a common location for several benign and malignant solid lesions with different clinical presentations.[1] Glomus tumors are benign neoplasms containing cells from the glomus apparatus which is responsible for thermoregulatory control, accounting 1–2% of all soft tissue tumors.[2,3] Histologically, glomus tumors and their variants are benign neoplasms requiring only a simple excision.[4] Painful subcutaneous nodule formation located on the subungual area of the digits is the usual presentation of glomus tumors.[3] Extradigital glomus tumors are rare lesions and their diagnosis are often delayed due to the physicians lack of awareness and low level of suspicion.[5] In this article, five cases of subcutaneous extradigital glomus tumors with sharp pain by digital palpation are presented in conjunction with a short literature review about this commonly misdiagnosed lesion.
Patients and Methods
A retrospective analysis of tumors diagnosed as glomus tumor in histopathological evaluation and located outside the digital area is performed between October 2012 and November 2013 and five patients fitting these criteria are determined.
All lesions were purple-colored, hard subcutaneous nodules which are painful by palpation [Figure 1]. The examination of the lesions with ultrasound imaging demonstrated hypoechoic solid masses with regular borders located in the subcutaneous tissue.
Figure 1.

The purple reflection seen on the skin surface of a subcutaneous nodule with 2 cm diameter on medial arm
All lesions were operated under local anesthesia using ×4 loupe magnification. The exposure was achieved through a linear incision performed over the lesions surface. The tumors had clear borders without any adhesion to surrounding tissues and no capsule formation was encountered. All lesions had a rich venous network at their base and a thin cutaneous nerve was detected during the dissection and protected. Wounds were closed with subcutaneous and cutaneous sutures after the removal of the tumor [Figure 2].
Figure 2.

The intraoperative appearance of the resected glomus tumor on the operation table
Results
Among five patients, only one patient was female and the remaining four patients were male. The mean age of the patients was 35 in a range of 14–65. Two lesions were located at the arm region, two lesions at the crural region and one lesion at the sternal area. The smallest nodule was 0.5 cm and the biggest lesion was 2 cm in diameter.
All lesions were reported as glomus tumor located outside the fingers called as “slledsdivesn glomus tumors [Figure 3]. The early postoperative period was uneventful in all patients with complete resolution of the pain and without any wound healing problems. A close follow-up carried out for the postoperative 1st year demonstrated that the complete resolution of the pain was permanent and no recurrence was encountered.
Figure 3.
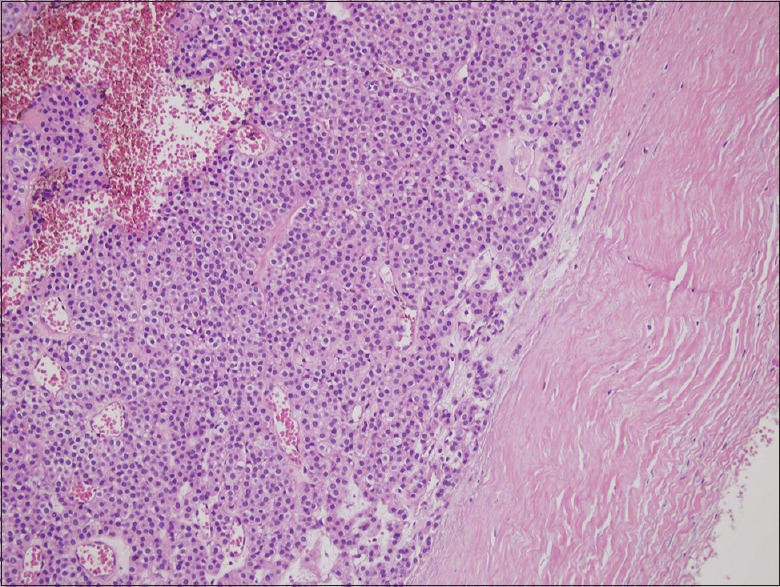
The histopathological appearance of the tumor showing clear blood vessels (H and E, ×40)
Discussion
Glomus tumor is the benign neoplasm of the glomus body which is a myoarterial unit acting like an arteriovenous anastomosis.[6] It basically regulates the blood flow to the skin according to the changes occurring in the body temperature.[7] Hoyer was the first researcher presenting the glomus body in 1877, however, the first clinical description of the tumor was performed by Masson in 1924.[8,9] Glomus tumors accounts for 1–2% of all soft tissue tumors and malignant transformation is very rare.[8,9] The glomus bodies are mainly concentrated on the fingers, palm and sole and the most common location of glomus tumors is the subungual area of the hand fingers.[10] Extradigital glomus tumor is a rare presentation commonly encountered in the lower extremity.[11] In our case series of five extradigital glomus tumors, two of them were located at the arm, two at the cruris and one at the sternal area.
The common presentation of the tumor is painful and purple colored subcutaneous nodules with hard consistency.[6,12] The pain caused by the tumor may occasionally be very severe causing fear by using the effected extremity causing muscle atrophy.[13] Glomus tumors are mainly reported as small nodules which rarely exceeds a diameter of 1 cm.[14,15] Despite that glomus tumors located at the lower extremity are usually encountered larger than 2 cm.[5] All lesions in the presented article were purple subcutaneous nodules with severe pain by palpation. Furthermore, the largest tumor with 2 cm diameter was located at the cruris and the other four tumors were between 0.5 cm and 1 cm supporting the literature. In our opinion, the purple color reflection encountered on the skin surface of the lesion [Figure 1] is an important finding for the diagnosis of the extradigital glomus tumors. In small subcutaneous nodules with pain by palpation and purple reflection on their surface, the extradigital glomus tumor should be considered as one of the forecoming lesions in the differential diagnosis.
The extradigital glomus tumor is an uncommon condition rarely coming into consideration in routine practice and, therefore, it commonly creates a confusion by the physician causing misdiagnosis.[16] Many examples may be given for this situation such as the facial glomus tumors usually reported as arteriovenous malformation in radiological evaluation,[17] lesions located at the elbow region especially causing pain are commonly diagnosed as neuroma,[18] abdominal glomus tumor may be the etiological reason of a chronic abdominal pain[19] or lesions located over the tendons may mimic tenosynovitis.[4] Our series also includes similar misdiagnosed cases such as the lesion at the sternal area which was initially diagnosed as an infected cyst and treated 3 weeks with oral antibiotics.
Ultrasound imaging is considered as the initial and usually the most useful method for the evaluation of the glomus tumor.[20] Magnetic resonance imaging may be useful for the detection of the tumor but its sensitivity was found to be lower than the ultrasound imaging.[21] All cases presented in this report was examined with ultrasound imaging and satisfactory radiological evaluation was achieved. In one case, Doppler ultrasound imaging was performed for the differential diagnosis of the lesion from a vascular lesion due its dense vascular nature.
The preferred treatment for isolated glomus tumor is surgical excision.[15] Small lesions may also be treated with laser ablation using argon or carbondioxide lasers.[22] In multiple cases located in the extremities, sclerotherapy using sodium tetradesyl or hypertonic saline solution is considered as an alternative.[5] The results obtained by surgical excision are found to be very successful with low recurrence rates between 12% and 33% in different publications.[23,24] Recurrences occurring in the 1st day or week are commonly a result of inadequate surgical excision[25] and recurrences occurring at the postoperative second or 3rd year are usually caused by multiple primary tumors.[11,22] In the presented study, all cases were solitary lesions and, therefore, treated with surgical excision. No recurrences were encountered in a follow-up period of 1 year which means that all lesions were totally excised without leaving any residual mass. However, our follow-up period is not enough to discuss the problem about the late recurrence which is directly related to undiagnosed multiple primary lesions. All lesions presented in this study were examined with ultrasound imaging preoperatively and were reported as solitary masses which fairly reduced the possible risk of late term recurrence.
Conclusion
Extradigital glomus tumor is a rare presentation and, therefore, the diagnosis is complicated for the physician resulting delayed diagnosis of the tumor. Early diagnosis of this condition is essential for protecting the patient from unnecessary and wrong treatments. Glomus tumor should be kept in mind for the differential diagnosis of all painful subcutaneous lesions especially for those with purple reflection on the skin surface.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
What is new?
Glomus tumor should be kept in mind in the differential diagnosis of all painful subcutaneous lesions
A slightly visible purple reflection on the skin surface is a very important feature of extra digital gloms tumor
Extradigital glomus tumor may be diagnosed earlier with a better knowledge about the clinical features and appearance of the tumor and in this way, unnecessary and wrong treatments may be prevented.
References
- 1.Gombos Z, Zhang PJ. Glomus tumor. Arch Pathol Lab Med. 2008;132:1448–52. doi: 10.5858/2008-132-1448-GT. [DOI] [PubMed] [Google Scholar]
- 2.Enzinger SW, Weiss FM. Soft Tissue Tumors. 5th ed. St. Louis: Mosby Elsevier; 2008. Perivascular tumors; pp. 751–65. [Google Scholar]
- 3.Veros K, Markou K, Filitatzi C, Kyrmizakis DE. Glomus tumor of the cheek: A case report. Case Rep Med 2012. 2012:307294. doi: 10.1155/2012/307294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nigam JS, Misra V, Singh A, Karuna V, Chauhan S. A glomus tumour arising from the flexor aspect of the forearm: A case report with review of the literature. J Clin Diagn Res. 2012;6:1559–61. doi: 10.7860/JCDR/2012/4233.2561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Frumuseanu B, Balanescu R, Ulici A, Golumbeanu M, Barbu M, Orita V, et al. A new case of lower extremity glomus tumor up-to date review and case report. J Med Life. 2012;5:211–4. [PMC free article] [PubMed] [Google Scholar]
- 6.Fletcher C. Diagnostic Histopathology of Tumors. Edinburgh: Churchill Livingstone; 2000. Tumours of blood vessels and lymphatics; pp. 75–6. [Google Scholar]
- 7.Venkatachalam MA, Greally JG. Fine structure of glomus tumor: Similarity of glomus cells to smooth muscle. Cancer. 1969;23:1176–84. doi: 10.1002/1097-0142(196905)23:5<1176::aid-cncr2820230525>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 8.Chatterjee JS, Youssef AH, Brown RM, Nishikawa H. Congenital nodular multiple glomangioma: A case report. J Clin Pathol. 2005;58:102–3. doi: 10.1136/jcp.2003.014324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carvalho VO, Taniguchi K, Giraldi S, Bertogna J, Marinoni LP, Fillus JN, et al. Congenital plaquelike glomus tumor in a child. Pediatr Dermatol. 2001;18:223–6. doi: 10.1046/j.1525-1470.2001.018003223.x. [DOI] [PubMed] [Google Scholar]
- 10.Tang CY, Tipoe T, Fung B. Where is the lesion?. Glomus tumours of the hand. Arch Plast Surg. 2013;40:492–5. doi: 10.5999/aps.2013.40.5.492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Folpe AL, Fanburg-Smith JC, Miettinen M, Weiss SW. Atypical and malignant glomus tumors: Analysis of 52 cases, with a proposal for the reclassification of glomus tumors. Am J Surg Pathol. 2001;25:1–12. doi: 10.1097/00000478-200101000-00001. [DOI] [PubMed] [Google Scholar]
- 12.Heje M, Bang C, Jensen SS. Glomus tumours causing limb hypoplasia? J Bone Joint Surg Br. 1992;74:779–80. doi: 10.1302/0301-620X.74B5.1326563. [DOI] [PubMed] [Google Scholar]
- 13.Kuru I, Oktar SO, Maralcan G, Yaycioglu S, Bozan ME. Familial glomus tumor encountered in the same finger and localization in four family members. Acta Orthop Traumatol Turc. 2005;39:365–8. [PubMed] [Google Scholar]
- 14.Caughey DE, Highton TC. Glomus tumour of the knee. Report of a case. J Bone Joint Surg Br. 1966;48:134–7. [PubMed] [Google Scholar]
- 15.Mullis WF, Rosato FE, Rosato EF, Butler CJ, Mayer LJ. The glomus tumor. Surg Gynecol Obstet. 1972;135:705–7. [PubMed] [Google Scholar]
- 16.Anagnostou GD, Papadementriou DG, Toumazani MN. Subcutaneous glomus tumors. Surg Gynecol Obstet. 1973;136:945–50. [PubMed] [Google Scholar]
- 17.Lee S, Le H, Munk P, Malfair D, Lee ChH, Clarkson P. Glomus tumour in the forearm: A case report and review of MRI findings. JBR-BTR. 2010;93:292–5. doi: 10.5334/jbr-btr.342. [DOI] [PubMed] [Google Scholar]
- 18.White CP, Jewer DD. Atypical presentation of a glomus tumour: A case report. Can J Plast Surg. 2006;14:237–8. doi: 10.1177/229255030601400402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kim YD, Son JS, Lee JW, Han YJ, Choi H, Jeong YJ. Extradigit glomus tumor causing abdominal pain – A case report. Korean J Pain. 2012;25:108–11. doi: 10.3344/kjp.2012.25.2.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Höglund M, Muren C, Brattstr M G. A statistical model for ultrasound diagnosis of soft-tissue tumours in the hand and forearm. Acta Radiol. 1997;38:355–8. doi: 10.1080/02841859709172082. [DOI] [PubMed] [Google Scholar]
- 21.Takei TR, Nalebuff EA. Extradigital glomus tumour. J Hand Surg Br. 1995;20:409–12. doi: 10.1016/s0266-7681(05)80105-6. [DOI] [PubMed] [Google Scholar]
- 22.Rao AG, Indira D, Kamal J. Extra digital glomangioma. Indian J Dermatol. 2010;55:397–8. doi: 10.4103/0019-5154.74570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Carroll RE, Berman AT. Glomus tumors of the hand: Review of the literature and report on twenty-eight cases. J Bone Joint Surg Am. 1972;54:691–703. [PubMed] [Google Scholar]
- 24.Strahan J, Bailie HW. Glomus tumour. A review of 15 clinical cases. Br J Surg. 1972;59:91–3. doi: 10.1002/bjs.1800590204. [DOI] [PubMed] [Google Scholar]
- 25.Rettig AC, Strickland JW. Glomus tumor of the digits. J Hand Surg Am. 1977;2:261–5. doi: 10.1016/s0363-5023(77)80121-4. [DOI] [PubMed] [Google Scholar]


