Abstract
We present a case report of a patient with epidermal inclusion cyst as a late complication of female genital mutilation (FGM). We describe the management of the patient, and a review of the literature. We report the clinical and pathological findings in a 37-year-old female patient from Nigeria, with a clitoral mass of 1 year duration. She declared to have an FGM since she was 5 years. The lesion was excised successfully with good cosmetic results. Histological examination revealed epidermal cyst with the presence of granular layer. An epidermal inclusion cyst can develop as a long-term consequence of FGM.
Keywords: Female genital mutilation, inclusion cyst, vulvar
Introduction
What was known?
Short-term and long-term complications of FGM have been well documented. The development of inclusion cyst along the line of the scar has been reported.
Female genital mutilation has been in practice for centuries. There are many reasons for perpetuation of this practice; the most common are cultural and religious beliefs. This has made eradication difficult. Health consequences depend on the severity of the initial mutilation. Most of these complications are immediate, though a few may present several years later.
Case Report
A 39-year-old, Nigerian woman was referred to our dermatological clinic due to painful genital swelling. Her medical history included a female genital mutilation (FGM) at the age of 5 years and an appendectomy 10 years before. She was otherwise in excellent health.
She had begun to notice a genital swelling 1 year prior and gradually increasing in size. She denied any trauma in the area. The patient had no history of difficulty with urination or with her sexual relations, but she recognized psychological discomfort since the cyst had begun to increase in size.
The clinical examination showed a nodular lesion covered with preserved mucosa, 30 mm × 20 mm in diameter, smooth surface, and not attached to deeper layers. The lesion was located in the scar of the mutilation.
Under local anesthesia and in lithotomy position the cyst was excised. It was easily removed by making a vertical incision in the skin and making a dissection along the lines of cleavage. The redundant skin was trimmed, and the edges were approximated. The nodule was a well-encapsulated unilocular cyst containing serous gray material [Figure 1].
Figure 1.

(a) Nodular lesion covered with preserved mucosa, not attached to deeper layers. Located in the scar of female genital mutilation. (b) The cyst was surgically removed. (c) A well-encapsulated unilocular cyst containing serous gray material
The histological examination showed a cystic lesion containing abundant laminated keratin. Walls were formed by keratinizing epithelium with the presence of granular layer. Diagnosis of infundibular inclusion cyst secondary to genital mutilation was established [Figure 2].
Figure 2.
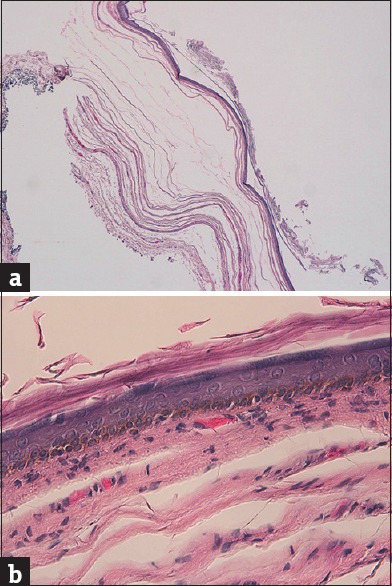
(a) Histological examination showed a cystic lesion containing abundant laminated keratin (H and E, ×2.5). (b) Walls were formed by keratinizing epithelium with the presence of granular layer (H and E, ×40)
The clinical follow-up of the patient after 6 months of the excision revealed no recurrence, with good appearance of the vulva and without pain.
Discussion
FGM is a very important event which is still taking place across the world, especially in Sub-Saharan Africa and in parts of the Middle East and Asia. Women with FGM are increasingly found in Europe, as a result of migration. The World Health Organization (WHO) defines this technique as any procedure that entails injury or removal of part or all of the external female genitalia, whether for cultural or nontherapeutic indications.
This procedure is classified by the WHO into four types: Type I, partial or total removal of the clitoris; Type II, partial or total removal of the clitoris and the labia minora; Type III (infibulation), excision of part or all of the external genitalia and narrowing of the vaginal orifice; Type IV, includes all other harmful procedures unclassified. Types I and II constitute about 80%.[1,2,3] Our patient had Type I circumcision.
Immediate complications as a complication of a female circumcision seen are infection, urinary retention, or hemorrhage. Late and long-term complications are urinary incontinence, recurrent urinary tract infections, adverse psychosexual sequelae, dyspareunia, obstetrical problems, and clitoral inclusion cysts. Delay from circumcision to the development of the cyst is variable, but a delay of more than 30 years, as in the present patient, is very infrequent.[4] It is thought that the formation of the cysts results from the embedding and invagination of squamous epithelium and sebaceous glands in the line of the scar which then desquamates and produce a cystic mass.[2,5] The cyst can be small from childhood without causing discomfort, although it may require excision because of inflammation, secondary infection, or malignant transformation.[6] In the puberty, the cyst can increase in size rapidly in response to estrogen. In a study of 37 patients with clitoral epidermoid inclusion cyst in a hospital of Nigeria, 59.5% were under 9 years, and 40.5% were between 14 and 21 years.[7]
To our knowledge, this is the first case reported in Europe that developed the cyst more than 30 years after FGM. Apart from FGM, trauma in female genitalia may also cause dermoid cyst.[8]
Conclusion
We recommend including inclusion cyst in the differential diagnosis of vulvar tumor. A high index of suspicion is required in a woman with vulvar swelling, especially in the case of history of FGM, trauma, or surgery in the genital area.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
What is new?
This is the first case reported in Europe that developed a vulvar inclusion cyst more than 30 years after FGM. This report aims to raise the awareness of the medical community to the dangers that arise from a remote complication of FGM.
References
- 1.Kelly E, Hillard PJ. Female genital mutilation. Curr Opin Obstet Gynecol. 2005;17:490–4. doi: 10.1097/01.gco.0000183528.18728.57. [DOI] [PubMed] [Google Scholar]
- 2.Yoong WC, Shakya R, Sanders BT, Lind J. Clitoral inclusion cyst: A complication of type I female genital mutilation. J Obstet Gynaecol. 2004;24:98–9. doi: 10.1080/01443610310001627254. [DOI] [PubMed] [Google Scholar]
- 3.Rouzi AA, Sindi O, Radhan B, Ba’aqeel H. Epidermal clitoral inclusion cyst after type I female genital mutilation. Am J Obstet Gynecol. 2001;185:569–71. doi: 10.1067/mob.2001.117660. [DOI] [PubMed] [Google Scholar]
- 4.Asante A, Omurtag K, Roberts C. Epidermal inclusion cyst of the clitoris 30 years after female genital mutilation. Fertil Steril. 2010;94:1097.e1–3. doi: 10.1016/j.fertnstert.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 5.Toubia N. Female circumcision as a public health issue. N Engl J Med. 1994;331:712–6. doi: 10.1056/NEJM199409153311106. [DOI] [PubMed] [Google Scholar]
- 6.Hamoudi A, Shier M. Late complications of childhood female genital mutilation. J Obstet Gynaecol Can. 2010;32:587–9. doi: 10.1016/S1701-2163(16)34528-5. [DOI] [PubMed] [Google Scholar]
- 7.Osifo OD. Post genital mutilation giant clitoral epidermoid inclusion cyst in Benin City, Nigeria. J Pediatr Adolesc Gynecol. 2010;23:336–40. doi: 10.1016/j.jpag.2010.02.006. [DOI] [PubMed] [Google Scholar]
- 8.Al-Ojaimi EH, Abdulla MM. Giant epidermoid inclusion cyst of the clitoris mimicking clitoromegaly. J Low Genit Tract Dis. 2013;17:58–60. doi: 10.1097/LGT.0b013e318259a410. [DOI] [PubMed] [Google Scholar]


