Sir,
Fixed drug eruption (FDE) is a special type of cutaneous adverse drug reaction, which characteristically recurs in the same site on skin/mucosa each time the offending drug is administered (hence called “fixed”).[1] FDEs comprise about 10% of all adverse drug reactions (ADR), the main causative drugs being analgesics, sulfonamides, and tetracyclines, etc.[2] Usually it presents as a single, sharply marginated, and round to oval patch or plaque on a violaceous or dusky erythematous background, associated with pruritus or burning. Occasionally, localized vesicles or bullae may be formed when it is referred to as localized bullous FDE. Multifocal or generalized bullous FDE (GBFDE) is an extremely uncommon variant, which may be clinically confused with the more sinister Stevens–Johnson syndrome (SJS) or toxic epidermal necrolysis (TEN).
A 30-year-old man presented to us with a 4 days history of multiple itchy and painful erythematous patches with vesicles and bullae of varying sizes scattered all over the body along with oral and genital ulcerations. The patient stated that these lesions developed suddenly after about 3 h following the ingestion of a single dose of doxycycline (100 mg) which was prescribed by a physician for some skin infection. On further probing, the patient revealed the appearance of similar lesions at the same sites 2 years ago following same drug intake, though the lesions were fewer and much less extensive; which had healed forming residual hyperpigmented macules. There was no history of any other drug intake.
Physical examination revealed multiple, well-defined, 3–5 mm diameter, round or oval violaceous to erythematous patches with overlying tense bullae. The lesions were predominantly located over the forearm, hand, and chest; with sparing of the face, scalp, palms, and soles [Figure 1]. Multiple erosions were present over lips and buccal mucosa [Figure 2]. The examination of genitalia revealed the swelling of the glans penis, and crusted lesions with a few vesicles over the scrotum [Figure 3]. He was afebrile, and other vital signs and the systemic examination did not reveal any abnormality.
Figure 1.

Multiple well-defined erythematous patches with overlying tense bullae distributed over the chest and upper limb
Figure 2.

Multiple erosions over the lips
Figure 3.

Swollen glans penis crusted lesions with a few vesicles over the scrotum. Note the purulent discharge from the ruptured bullae
Histopathological examination showed subepidermal bulla, inflammatory infiltrate, and necrotic keratinocytes [Figures 4 and 5]. This was consistent with a diagnosis of generalized bullous FDE (GBFDE). Causality assessment by Naranjo Scale and WHO Uppsala Monitoring Center Scale categorized the reaction as “probable” (Naranjo's Score = 8) adverse effect induced by doxycycline. Severity assessment using modified Hartwig and Siegel's ADR Severity Assessment Scale labeled the reaction as “moderate” (level = 3).
Figure 4.
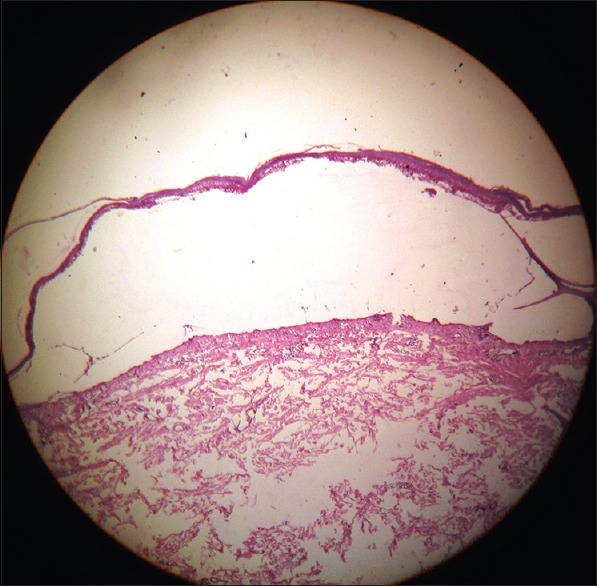
Photomicrograph showing subepidermal bulla (H and E, ×10)
Figure 5.
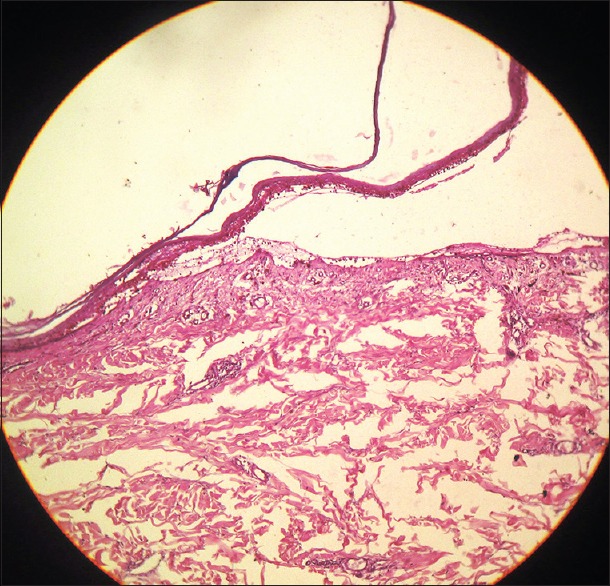
Photomicrograph showing subepidermal bulla, inflammatory infiltrate. The roof the blister showing necrotic keratinocytes (H and E, ×40)
A diagnosis of generalized bullous FDE was made based on clinical and histopathological evidence. However, considering the severity of reaction, oral provocation test and patch test with doxycycline were not performed, as we considered them unethical in view of the perceived risks. Doxycycline was stopped, and the patient was managed conservatively along with a short course of oral corticosteroid (prednisolone – 1 mg/kg/day) for 10 days. The lesions resolved with residual post inflammatory hyperpigmentation. The patient was advised to strictly avoid doxycycline and other related drugs in the future.
GBFDE is an extremely uncommon variant of FDE, which has been defined as the presence of typical FDE lesions (patch or plaque) with blisters involving at least 10% of body surface area or at least 3 of 6 different anatomic sites.[3] In our case, widespread distribution of bulla of different sizes was observed primarily involving the trunk and extremities; thus satisfying the definition of GBFDE. Usually in this variety, the mucosal surfaces are spared;[2] however, both oral and genital mucosal involvement was observed in our case. Other uncommon varieties of FDE, which have been reported includes morbilliform, scarlatiniform, erythema multiforme-like, urticarial, nodular, eczematous, and nonpigmenting type.[1] FDEs occur as a result of antibody-dependent, cell mediated cytotoxicity. The CD8+ effector/memory T-cells, which release interferon-gamma, are mainly responsible. Interleukin-20 is responsible for the remarkable site-specificity of the lesions. Generally, the lesions of FDE heal with the residual pigmentation, thus being of cosmetic concern to the patient. The time interval between the ingestion of the offending drug and appearance of symptoms varies from 30 min to 8 h, the mean being about 2 h.[4] In our case, the lesions developed about 3 h after ingestion of doxycycline.
Although, GBFDE is a relatively rare phenomenon, there are sporadic reports of its association with certain drugs viz. Mefenamic acid,[1] naproxen,[5] cetrizine,[6] ciprofloxacin,[7] and nicotinic acid/laropripant.[8] Fluoroquinolone has been reported to cause generalized FDE.[9] Localized bullous FDE has been reported with paracetamol.[10] Doxycycline is an antibiotic, belonging to the tetracycline group which is one of the common causes of classical FDE (macule/patch); however, rarely it may cause nongeneralized/localized bullous FDE[11] or generalized/multifocal bullous FDE.[12] In our case also, doxycycline has been implicated to cause GBFDE, along with mucosal involvement.
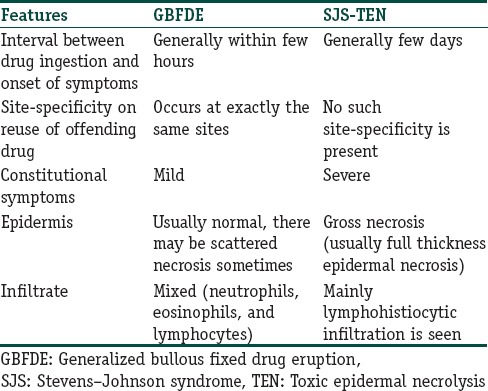
Although, the diagnosis is primarily clinical; sometimes it may be confused with SJS and TEN. A skin biopsy is diagnostic. These conditions can also be differentiated by immunohistopathological features.[3] The principle differentiating features between FDE and SJS-TEN are tabulated below [Table 1]. Recently, some workers have advocated the use of oral provocation tests and patch tests to confirm the diagnosis of FDE, however, concrete evidence of their efficacy is still lacking. These tests were not performed in our case due to the severity of the present episode. The temporal association with doxycycline, previous history of a milder reaction with the same drug at same sites which healed with subsequent hyperpigmentation and a consistent skin biopsy clinched our diagnosis as GBFDE due to doxycycline.
Table 1.
Differentiating features between GBFDE and SJS-TEN
Treatment of FDE is essentially symptomatic with systemic antihistamines and topical corticosteroids. When infection is suspected, suitable antibiotics are to be prescribed; severe cases of GBFDE warrant the attention and aggressive management of SJS or TEN.[13] However, most importantly we have to counsel the patient to avoid over the counter medications and the common offending drugs in the future; as there is a chance of cross-reaction with other drugs, especially other tetracycline antibiotics.[1]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Breathnach SM. Drug reactions. In: Burns T, Breathnach S, Cox N, et al., editors. Rook's Textbook of Dermatology. 8th ed. United Kingdom: Wiley-Blackwell Publisher (P) Ltd; 2010. pp. 75-28–75-29. [Google Scholar]
- 2.Patro N, Panda M, Jena M, Mishra S. Multifocal fixed drug eruptions: A Case Series. Int J Pharm Sci Rev Res. 2013;23:63–6. [Google Scholar]
- 3.Cho YT, Lin JW, Chen YC, Chang CY, Hsiao CH, Chung WH, et al. Generalized bullous fixed drug eruption is distinct from Stevens-Johnson syndrome/toxic epidermal necrolysis by immunohistopathological features. J Am Acad Dermatol. 2014;70:539–48. doi: 10.1016/j.jaad.2013.11.015. [DOI] [PubMed] [Google Scholar]
- 4.James WD, Elston DM, Berger TG. 11th ed. UK: Saunders Elsevier; 2011. Andrews’ Diseases of the Skin: Clinical Dermatology; pp. 117–8. [Google Scholar]
- 5.Bandino JP, Wohltmann WE, Bray DW, Hoover AZ. Naproxen-induced generalized bullous fixed drug eruption. Dermatol Online J. 2009;15:4. [PubMed] [Google Scholar]
- 6.Arslan Ş, Taçli L, Kaşar N, Ergin Ş. Generalized bullous fixed drug eruption associated with cetirizine and hydroxyzine demonstrated by patch test. Turkderm Deri Hastalik Frengi Arsivi. 2011;45:49–52. [Google Scholar]
- 7.Ada S, Yilmaz S. Ciprofloxacin-induced generalized bullous fixed drug eruption. Indian J Dermatol Venereol Leprol. 2008;74:511–2. doi: 10.4103/0378-6323.44324. [DOI] [PubMed] [Google Scholar]
- 8.Ho SA, Derrick CW. Bullous drug eruption. Ann Acad Med. 2012;41:134–5. [PubMed] [Google Scholar]
- 9.Hager JL, Mir MR, Hsu S. Fluoroquinolone-induced generalized fixed drug eruption. Dermatol Online J. 2009;15:8. [PubMed] [Google Scholar]
- 10.Nino M, Francia MG, Costa C, Scalvenzi M. Bullous fixed drug eruption induced by paracetamol: Report of a pediatric case. Case Rep Dermatol. 2009;1:56–9. doi: 10.1159/000243728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee CH, Chen YC, Cho YT, Chang CY, Chu CY. Fixed-drug eruption: A retrospective study in a single referral center in northern Taiwan. Dermatol Sin. 2012;30:11–5. [Google Scholar]
- 12.Nitya S, Deepa K, Mangaiarkkarasi A, Karthikeyan K. Doxycycline induced generalized bullous fixed drug eruption - A case report. J Young Pharm. 2013;5:195–6. doi: 10.1016/j.jyp.2013.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lipowicz S, Sekula P, Ingen-Housz-Oro S, Liss Y, Sassolas B, Dunant A, et al. Prognosis of generalized bullous fixed drug eruption: Comparison with Stevens-Johnson syndrome and toxic epidermal necrolysis. Br J Dermatol. 2013;168:726–32. doi: 10.1111/bjd.12133. [DOI] [PubMed] [Google Scholar]


