ABSTRACT
Objective:
To evaluate the applicability of modified formulae based on plasma creatinine levels in Chinese diabetic patients with chronic kidney diseases (CKD).
Methods:
A total of 294 diabetic patients were investigated. Glomerular filtration rate (GFR) was estimated with the Ruijin equation, Cockcroft-Gault (CG) and Modification of Diet in Renal Disease (MDRD) formulae. The accuracy of estimated GFR was compared with technetium-99m diethylene triamine pentaacetic acid (99mTc-DTPA)-GFR (sGFR).
Results:
Bland-Altman analysis demonstrated that the Ruijin equation was more consistent with sGFR than the other equations. However, all the equations were not very consistent with sGFR. The analysis showed that the slope of the Ruijin equation was closer to the identical line and indicated that the bias of Ruijin equation was lowest. The 15%, 30% and 50% accuracies of the Ruijin equation were higher than those of the other equations; the 30% accuracy of Ruijin equation was more than 70%.
Conclusions:
Ruijin equation is more applicable in Chinese diabetic and CKD patients.
Keywords: Chronic kidney disease, glomerular filtration rate, diabetes
RESUMEN
Objetivo:
Evaluar la aplicabilidad de las fórmulas modificados basadas en los niveles de creatinina del plasma en pacientes diabéticos chinos con enfermedades renales crónicas (ERC).
Métodos:
Se investigaron un total de 294 pacientes diabéticos. La tasa de filtración glomerular (TFG) se estimó usando las fórmulas de Ruijin, Cockcroft-Gault (CG) y MDRD (Modification of Diet in Renal Disease). La exactitud de la TFG estimada se comparó con ácido dietileno-triamino-pentaacético con tecnecio-99m (DTPA-99mTc)-TFG (sTFG).
Resultados:
El análisis de Bland-Altman demostró que la ecuación de Ruijin fue más coherente con sTFG que las otras ecuaciones. Sin embargo, no todas las ecuaciones fueron coherentes con sTFG. El análisis mostró que la pendiente de la ecuación de Ruijin estaba más cercana a la línea idéntica e in-dicó que el sesgo de la ecuación de Ruijin fue menor. Las precisiones de 15%, 30% y 50% de la ecua-ción de Ruijin fueron superiores a las de las otras ecuaciones. La precisión de 30% de la ecuación de Ruijin fue más del 70%.
Conclusiones:
La ecuación de Ruijin es más aplicable en los pacientes chinos con diabetes y ERC.
INTRODUCTION
The glomerular filtration rate (GFR) is an important indicator for clinical evaluation of renal function. American Diabetes Association and other guidelines recommend the Cockcroft-Gault (CG) formula and Modification of Diet in Renal Disease (MDRD) formula to estimate GFR. Recently, the estimated GFR (eGFR) project collaborative group (1, 2) and Ruijin hospital (3) developed a new GFR assessment equation based on the Chinese population. In this study, we compared the eGFR and standard GFR (sGFR) measured by technetium-99m diethylene triamine pentaacetic acid (99mTc-DTPA) and evaluated the applicability of the above equation in our diabetic patients.
SUBJECTS AND METHODS
This work was approved by the Ethics Committee of Provincial Hospital Affiliated to Anhui Medical University. Two hundred and ninety-four cases of diabetes were chosen from March 2008 to November 2009 in our hospital. Study participants included 199 males and 95 females, with a mean age of 57.28 ± 13.95 years. There were 16 cases with Type 1 diabetes and 278 cases with Type 2 diabetes. The diagnosis of diabetes was in agreement with the World Health Organization (WHO) standard proposed in 1998. All patients with diabetic ketoaci-dosis, hyperosmolar nonketotic coma, urinary tract infections, serious heart and liver dysfunction, malignant tumours and rheumatic diseases were excluded.
All patients underwent radionuclide renal dynamic imaging through projectile intravenous injection of 99mTc-DTPA (Siemens Signature e.Cam SPECT, Germany). We inputted the height and body mass of patients, calculated the sGFR with Gates method, and corrected the sGFR with body surface area (BSA).
We also analysed the biochemical parameters in venous blood after patient-fast of 12 hours: fasting plasma glucose (FPG), two hours postprandial glucose (2hPG), serum creatinine (Scr), triglyceride (TG) and total cholesterol (TC). The haemoglobin was also done. All the indices were measured with Hitachi 7600 automatic biochemistry analyser. Serum creatinine was measured by the creatine oxidase method, and the haemoglobin Alc (HbAlc) was measured with high-pressure liquid chromatography. The albumin:creatinine ratio (ACR) was analysed from the first urine in the morning by immunoturbidimetric assay.
The evaluations used were:
Cockcroft-Gault formula: GFR = [(140-age) × weight (kg)]/ [(72 × Scr (mg/dL)], correction with BSA
MDRD formula: 186 × Scr (mg/dL)-1.154 × age-0.203 × 0.742 (female)
Ruijin equation: 234.96 × (Scr)-0.926 × (age)-0.280 × 0.828 (female)
Scr conversion formula: 1 μmol/L = 0.0113 mg/dL
Statistical analysis
Data are expressed as mean ± standard deviation. The relationship between eGFR and sGFR is analysed by Spearman correlation coefficient. The consistency limits of eGFR and sGFR is calculated with Bland-Altman plotting method. Consistency limits = 95% × (eGFR – sGFR). Deviation from the measured values = IeGFR – sGFRI/sGFR×100%. We did regression analysis of the deviation and average of eGFR and sGFR. The regression line and x-axis slope indicates the degree of equation deviation from sGFR; the greater the slope, the greater the deviation. The regression line and y-axis intercept indicates the accuracy of the equation; the wider the intercept, the worse the accuracy of the equation. Compliance rates of 15%, 30% and 50% are the estimated values of the equation that fall in the range of sGFR ± 15%, ± 30% and ± 50%. The accuracy of the equations was analysed by Chi-squared test. All data were analysed with SPSS 13.0 and MedCal software.
RESULTS
The GFR and sGFR estimated by all equations showed a significant correlation. Bland-Altman analysis showed that the GFR and sGFR estimated by Ruijin equation were the best; linear regression analysis showed that the slope of GFR and x-axis calculated with Ruijin equation was smaller than that estimated with other equations. The intercept of regression line on the y-axis was also smaller with Ruijin equation; compared with MDRD equation, the Ruijin and CG equations had smaller deviation. The percentage of deviation from measurement was also the smallest in the Ruijin equation; the GFR 15%, 30% and 50% compliance rates were the highest in the Ruijin equation, and the GFR 30% compliance rate was higher than 70% only in the Ruijin equation (Table).
Table. Overall performance of agreement, differences and accuracy between eGFR and sGFR.
| CG equation | MDRD equation | Ruijin equation | |
|---|---|---|---|
| Correlation coefficient | 0.70 | 0.70 | 0.72 |
| Consistency limits | -45.1~65.5 | -39.6~72.8 | -37.2~50.2 |
| Slope between regression line and x-axis (95% CL) | 0.42 (0.32, 0.51) | 0.44 (0.34, 0.52) | 0.15 (0.06, 0.24) |
| Intercept between regression line and y-axis (95% CL) | -26.55 (-35.33, −17.76) | -23.24 (-32.25, −14.23) | 6.52 (-14.91, 1.87) |
| Deviation value (25%, 75%) | 5.23 (-6.76, 26.15) | 14.51 (-3.14, 34.09) | 5.84 (-5.83, 20.72) |
| Deviation measured value% (25%, 75%) | 21.87 (8.53, 38.42) | 25.76 (10.90, 47.15) | 17.42 (16.83, 32.29) |
| 15% coincidence rate | 0.377551 | 0.363946 | 0.44898 |
| 30% coincidence rate | 0.64966 | 0.598639 | 0.710884 |
| 50% coincidence rate | 0.823129 | 0.785714 | 0.901361 |
eGFR: estimated glomerular filtration rate; sGFR: standard glomerular filtration rate;
CG: Cockcroft-Gault; MDRD: Modification of Diet in Renal Disease
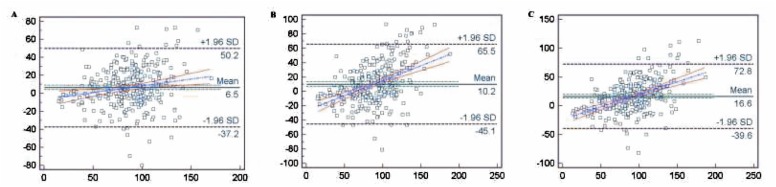
In our study, CKD stage 1 was 123 cases, CKD stage 2 was 113 cases, CKD stage 3 was 48 cases and CKD stage 4–5 was 10 cases. There was a small deviation between the Ruijin equation and CG equation in CKD stage 1; the percentage of deviation from measurement was smaller in the Ruijin equation. All the GFR 15%, 30% and 50% compliance rates were higher in the Ruijin and CG formula. In CKD stage 2, there also was a small deviation between the Ruijin and CG equation, and the percentage of deviation from the measurement was smaller in the Ruijin and CG equations; the GFR compliance rate was higher in the Ruijin and CG equations. In CKD stage 3, the CG formula had smaller deviation compared to other equations; the percentage of deviation from measurement was smaller in the Ruijin and CG equations, and the GFR compliance rate was higher in the Ruijin and GC equations. In CKD stage 4–5, there was lower deviation and the percentage of deviation from the measurement was smaller in Ruijin equation than in other equations; the GFR compliance rate was also higher in the Ruijin equation. The Bland-Altman plot shows the disagreement between eGFR and sGFR (Figure).
Figure. Bland-Altman plot of estimated and standard glomerular filtration rate (eGFR and sGFR). The solid lines represent the mean of difference between methods; dashed lines represent 95% CI for the regression line and dotted lines represent 95% limits of agreement. The horizontal coordinates indicate the average of eGFR and sGFR. The longitudinal coordinates indicate the deviation of them. A) sGFR and eGFR – Ruijin equation; B) sGFR and eGFR – Cockcroft-Gault (CG) equation; C) sGFR and eGFR – Modification of Diet in Renal Disease (MDRD) equation.
DISCUSSION
In this study, we used Bland-Altman analysis for conformance assessment. The results showed that the consistency of GFR and sGFR estimated by all equations was poor. The consistency limits of GFR and sGFR estimated by all equations exceeded the value of 60 ml·min-1 (1.73 m2)-1, in which the consistency of GFR and sGFR estimated by the Ruijin equation was the best one. The slope of GFR and x-axis, and the intercept of regression line on y-axis estimated by Ruijin equation were smaller than those estimated with other equations. In all equations, the GFR 15%, 30% and 50% compliance rates were the highest in the Ruijin equation, and the GFR 30% compliance rate was more than 70% only in the Ruijin equation, according to the estimation of the Kidney Disease Outcomes Quality Initiative (K/DOQI) professional group (4). Therefore, evaluation of GFR with the Ruijin equation, which was developed based on the Chinese population, is more suitable for our diabetic patients with CKD.
Technetium-99m (99mTc) has features of a shorter halflife, is economical, practical and simple to prepare; it has been widely applied in clinical practice (5). The correlation of GFR and insulin clearance rate is good with 99mTc-DTPA; it is an accurate marker for GFR. The American Society of Nuclear Medicine recommends a two-sample method as the reference standard to measure GFR; however, the blood needs to be collected two hours and four hours after injection with the two-sample method, so the patients need to wait a long time in the hospital; therefore, it is not convenient. There was a good correlation between 99mTc-DTPA method and the two-sample method [p < 0.01] (6).
It should be noted that some factors might affect our results. The picric acid and enzymatic methods are the most common methods for determination of Scr; however, it has been proven that there was not a linear relationship between the measured values of the two methods. In the Ruijin equation, the Scr was determined by the picric acid method, while the Scr was measured by the enzymatic method in our study. There was deviation of Scr detected by different methods; therefore, it caused greater degree of deviation of GFR assessment based on Scr (7). Moreover, different population and race also lead to deviation. Therefore, there needs to be further evaluation and validation of the applicability of the above equation in our diabetic population, and positive development of the assessment equation using the enzymatic method to detect Scr.
Footnotes
This manuscript was previously published in New York Science Journal 2013; 6 (9): 29–31 and Chinese Journal of Diabetes 2013; (5): 422–5. Permission was obtained for it to be republished in West Indian Medical Journal.
REFERENCES
- 1.Chinese eGFR Investigation Collaboration Modification and evaluation of MDRD estimating equation for Chinese patients with chronic kidney disease. Chin J Nephrol. 2006;22:589–595. [Google Scholar]
- 2.Ma YC, Zuo L, Chen JH, Luo Q, Yu XQ, Li Y, et al. Modified glomerular filtration rate estimating equation for Chinese patients with chronic kidney disease. J Am Soc Nephrol. 2006;17:2937–2944. doi: 10.1681/ASN.2006040368. [DOI] [PubMed] [Google Scholar]
- 3.Shi H, Chen N, Zhang W. Evaluating and refitting the simplified equation of MDRD to predict glomerular filtration rate in Chinese patients with chronic kidney disease. Chin J Pract Int Med. 2006;36:665–669. [Google Scholar]
- 4.Wang HY, Wang MY. American NKF-K/DOQI Collaboration – clinical practice guidelines for chronic kidney disease and dialysis. Beijing: People's Medical Publishing House; 2003. [Google Scholar]
- 5.Schwartz GJ, Furth SL. Glomerular filtration rate measurement and estimation in chronic kidney disease. Ped Nephrol. 2007;22:1839–1848. doi: 10.1007/s00467-006-0358-1. [DOI] [PubMed] [Google Scholar]
- 6.Fleming JS, Zivanovic MA, Blake GM, Burniston M, Cosgriff PS, British Nuclear Medicine Society Guidelines for the measurement of glomerular filtration rate using plasma sampling. Nucl Med Commun. 2004;25:759–769. doi: 10.1097/01.mnm.0000136715.71820.4a. [DOI] [PubMed] [Google Scholar]
- 7.Vickery S, Stevens PE, Dalton RN, van Lente F, Lamb EJ. Does the ID-MS traceable MDRD equation work and is it suitable for use with compensated Jaffe and enzymatic creatinine assays? Nephrol Dial Transplant. 2006;21:2439–2445. doi: 10.1093/ndt/gfl249. [DOI] [PubMed] [Google Scholar]