INTRODUCTION
The recurrent laryngeal nerve (RLN) innervates all the important laryngeal muscles except the cricothyroid. Careful dissection of the RLN during surgery reduces the risk of damage. The non-RLN (NRLN) is a rare anatomical anomaly of the RLN, with an incidence of 0.5 to 0.7% in thyroid surgery (1). It is difficult to identify this anomaly preoperatively unless an associated vascular anomaly is suspected. This study aims to emphasize the awareness of the possibility of a NRLN to prevent iatrogenic injury.
CASE REPORT
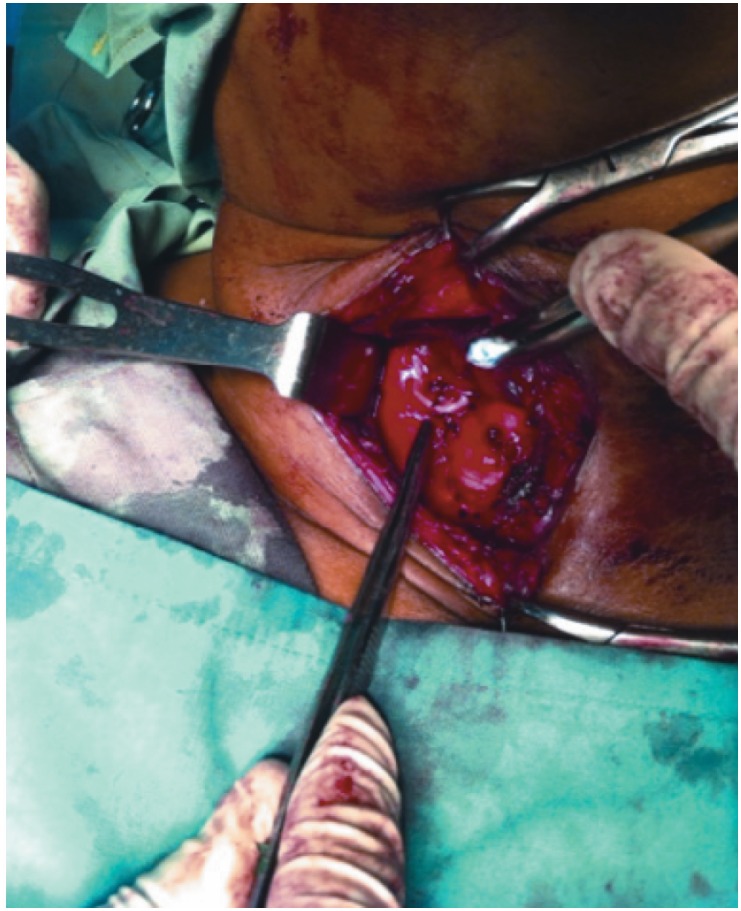
A 49-year old woman with no known chronic illnesses presented to a private medical facility with a left-sided thyroid nodule for one year. She had no complaints of hoarseness or compressive symptoms. On examination, the left lobe of the thyroid was found to be enlarged. An indirect laryngoscopic examination showed normal vocal cord function. Ultrasound revealed a solitary, solid 3.1 × 2.5 cm nodule in the left lobe. There were no cervical nodes seen on ultrasound. She was confirmed to be euthyroid. The patient declined fine needle aspiration and opted instead for a left hemithyroidectomy. The nerve on the left side was found in the left tracheoesophageal groove in a recurrent fashion. Histopathological evaluation of the left hemithyroid revealed papillary carcinoma. It was decided that the patient should undergo a completion thyroidectomy. During surgery, the right thyroid lobe was rotated medially and the right RLN was not found as expected in or near the tracheoesophageal groove. However, careful exploration revealed a transverse nerve running medially to the cricothyroid joint (Figure). The nerve was preserved without damage. The postoperative period was uneventful and the patient had no change in her voice. She was treated postoperatively with whole body ablation and thyroid suppression therapy. Follow-up whole body scans have been normal.
Figure. Right lateral view of the neck of a patient undergoing thyroidectomy. The right thyroid lobe is retracted and the non-recurrent laryngeal nerve is seen following a transverse path.
DISCUSSION
The recurrent laryngeal nerve receives its name simply because, after branching off the vagus nerve in the root of the neck, its path describes a loop as it turns upwards (recur) under the subclavian artery on the right side and under the ligamentum arteriosum on the left. It provides innervations to all the important intrinsic muscles of the larynx, with the exception of the cricothyroid which is supplied by the external laryngeal nerve (2). The non-recurrent laryngeal nerve is an anomaly of the RLN because its origin is cervical and it runs a direct course from the vagus nerve to the larynx without looping around any of the above named structures (3). The origin of the NRLN is cervical and there are three types (4). Type 1 occurs where the NRLN arises directly from the vagus and travels with the superior thyroid pedicle vessels. In Type 2A, the NRLN travels transversely, parallel and superficial to the trunk of the inferior thyroid artery and Type 2B occurs where the nerve travels in a transverse path parallel, but deep to or between the branches of the inferior thyroid artery. Our case involved a Type 2A NRLN.
The NRLN anomaly was first observed by Steadman in 1823 when he noticed it during a cadaveric dissection, along with an anomaly of the origin and course of the right subclavian artery (4). The NRLN is rare; its prevalence has been reported as 0.3–1% on the right side and 0.004% on the left side (4).
The embryological explanation for the right-sided NRLN appears to be secondary to a vascular disorder called arteria lusoria in which the fourth arch on the right involutes instead of persisting on the right as the subclavian artery. When this happens, the right RLN is not pulled inferiorly when the heart descend and the neck elongates during embryogenesis (5). The RLN will now arise higher in the neck instead of at the root and will then run a course directly to the larynx as the NRLN. The right subclavian artery will then arise on the left side from the aortic arch and will take a course posterior to the oesophagus. Five per cent of patients with this vascular malformation will experience dysphagia (dysphagia lusoria) due to compression of the oesophagus by this retro-oesophageal artery. The patient in our case report denied any symptoms of dysphagia. The NRLN on the left is associated with situs in-versus and dextrocardia, where the aortic arch and ligamentum arteriosum are now on the right (3).
A NRLN may be suspected preoperatively if there was a barium swallow done for a patient experiencing dysphagia which might show indentation of the oesophagus by an anomalous vessel (bayonet sign), or by an abnormal chest X-ray with superior mediastinal widening or vascular anomalies detected on digital subtraction angiography. In the majority of cases, these test are not done routinely, and so the surgeon will have to identify the NRLN at the time of surgery.
During thyroid surgery, the thyroid surgeon should search diligently for the right RLN as a white vertical structure close to or in the tracheoesophageal groove. As the right RLN is less likely to be in the tracheoesophageal groove than the left due to its relation to the inferior thyroid artery and oesophagus, one has to undergo a meticulous dissection in the fascial space between the carotid artery and the tracheoesophageal groove after the thyroid gland is mobilized. If the familiar vertical white structure resembling the RLN is not seen after careful blunt dissection, the surgeon should consider a NRLN and search for any transverse white structures which course into the larynx close to the inferior cornu of the thyroid cartilage. Our meticulous practice of searching for the right RLN in this fascial space and not ligating any transverse structures except the middle thyroid vein until we have found the RLN, allowed us to identify a rare right RLN and preserve it.
CONCLUSIONS
The incidence of NRLN is rare, but lack of knowledge and vigilance of this rare phenomenon can result in iatrogenic ligation and its attendant complications. If there is a preoperative diagnosis of dysphagia lusoria or situs inversus in a patient undergoing thyroidectomy, this should be a red flag for the existence of a NRLN. Systematic and meticulous dissection of the RLN longitudinally in the region of the tracheoesophageal groove, and if not found, dissecting transversely in the fascial space between the carotid sheath and the larynx, will allow identification of the nerve and preservation of this very important structure.
REFERENCES
- 1.Raj S, Deo RP, Mohiyuddin A. Nonrecurrent laryngeal nerve: an Indian documentation. Int J Head Neck Surg. 2012;3:28–29. [Google Scholar]
- 2.Casal D, Pecas A, Sousa D. A non-recurrent inferior laryngeal nerve in a man undergoing thyroidectomy: a case report. J Med Case Rep. 2010;4:386–386. doi: 10.1186/1752-1947-4-386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cannon C. The anomaly of nonrecurrent laryngeal nerve: identification and management. Otolaryngol Head Neck Surg. 1999;120:769–771. doi: 10.1053/hn.1999.v120.a84675. [DOI] [PubMed] [Google Scholar]
- 4.Kamath S, Rathnakar P, Shetty K. Nonrecurrent laryngeal nerve: a rare entity. NUJHS. 2012;2:42–44. [Google Scholar]
- 5.Sarkar A. A case report on abnormal origin of right recurrent laryngeal nerve from right vagus in thorax. Int J Case Rep Images. 2012;3:4–7. [Google Scholar]