Abstract
The current method of transporting self-collected cervicovaginal specimen for HPV DNA testing relies on liquid based medium, which is challenging and expensive to transport. A novel, dry storage and transportation device, Whatman indicating FTA™ Elute Cartridge, avoids some of the pitfalls of liquid-based medium. This method has been shown to be comparable to liquid-based collection medium, but relative performance of self-collected (SC) and clinician-collected (CC) samples onto FTA cards has not been reported. The objective of this study is to compare the analytic performance of self- and clinician-collected samples onto FTA cartridges for the detection of carcinogenic HPV using Linear Array. There was a 91% agreement, 69% positive agreement, and kappa of 0.75 between the clinician-collected and self-collected specimens for detection of any carcinogenic HPV genotype. When the HPV results were categorized hierarchically according to cervical cancer risk, there was no difference in the distribution of the HPV results for the clinician- and self-collected specimens (p = 0.7). This study concludes that FTA elute cartridge is a promising method of specimen transport for cervical cancer screening programs considering using self-collected specimen and HPV testing. Larger studies with clinical endpoints are now needed to assess the clinical performance.
Keywords: FTA cartridge, Self-collection, Cervical cancer, Human papillomavirus (HPV)
1. Introduction
It has been well established that persisting cervical infection with human papillomavirus (HPV) is the necessary cause of cervical cancer. HPV DNA testing has proven clinical value as a primary screening method as it is a much more effective (more sensitive and equally specific) screening method compared to Pap smear (Bais et al., 2005; Arbyn et al., 2005; Cuzick et al., 2003; Schiffman et al., 2011; Bandyopadhyay et al., 2008; Katki et al., 2011). It has been shown that in low-resource settings, a single round of HPV testing is associated with significant decrease in cervical cancer-related mortality (Sankaranarayana et al., 2009).
Self-collected cervicovaginal specimens tested for carcinogenic human papillomavirus (HPV) DNA may be used to complement current screening programs to reach underserved populations (Gravitt et al., 2011; Sowjanya et al., 2009). Self-collected specimens with HPV DNA testing may be less sensitive and specific than clinician-collected specimens for identifying women with cervical precancer and cancer but has comparably sensitivity as cytology-based screening. The advantage of using self-collection are that it does not require a clinic-based pelvic exam with speculum, thereby needed fewer resources and is less dependent on the healthcare infrastructure.
However, current methods of transporting self-collected specimens to the testing laboratory rely on liquid buffers, which can be flammable, toxic, bulky, and challenging and expensive to transport. This limits the feasibility of using self-collection in screening programs. Therefore this study evaluated the acceptability and analytic performance of a novel, dry storage and transportation device, FTA elute cartridge (GE Healthcare, Buckinghamshire, UK), which avoids some of the pitfalls of liquid-based medium. Previous studies have shown good agreement for HPV DNA detection using the liquid based medium and the FTA cartridge (Lenselink et al., 2009; Gustavsson et al., 2009, 2011). As part of the overall study, here the agreement of self-versus clinician-collection specimens onto FTA cartridges for the detection of carcinogenic HPV are reported.
2. Materials and methods
The institutional review boards of the Cancer Institute/Hospital of the Chinese Academy of Medical Sciences (CICAMS) in Beijing, China approved the study, and the Institutional Review Board of Johns Hopkins University School of Medicine and National Cancer Institute granted Institutional Review Board exception for the study because all identifying information was removed.
2.1. Study subjects
Two thousand and five hundred women between the ages of 30 and 59 were recruited from the general population in Xiangyuan County, Shanxi Province, China. The participants were also offered to participate in the Chinese National Screening program for Cervical Cancer sponsored by the Chinese government. Eligible women were not pregnant and have not had a hysterectomy. Informed, written consent was obtained from all participants.
All 2500 women underwent initial screening in the local clinics, which consisted of gynecologic exam with visual inspection with acetic acid and Lugol’s iodine (VIA/VILI). The study was nested in this population by selecting and enrolling all 63 VIA/VILI-positive patients (2.5%) and a random sample of 111 VIA/VILI negative patients.
2.2. Study procedures
The 174 participants were offered transportation from their local villages to the Xiangyuan County Maternal and Child Health Hospital of Shanxi, where the study was conducted. Each participant had an initial one-on-one interview with a trained health worker, where basic demographic information (age, education, and income), past medical/gynecological history, family history, HPV knowledge assessment, and other behavioral factors (transportation method, access to medical care, distance to closest clinic, and attitude toward regular gynecological checkups) were collected.
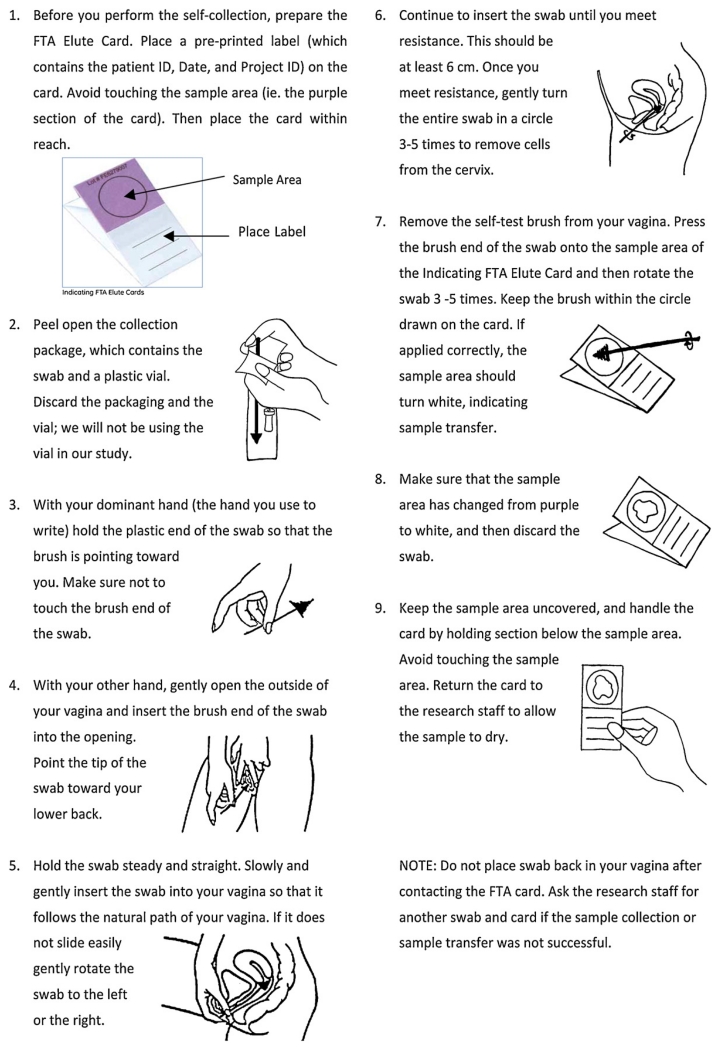
After the initial interview, the participants were given written and verbal instructions for self-collection. The instructions were given in Chinese and each step was also supplemented with descriptive figures (Fig. 1). Instructions were also posted in the self-collection room for reference. Each participant obtained a Qiagen cervical sampler brush (Qiagen, Gaithersburg, MD, USA) and a Whatman indicating FTA elute cartridge (GE Healthcare, Buckinghamshire, UK) and was sent to a private room for self-collection. The Whatman Indicating FTA elute cartridge (FTA cartridge) uses a paper matrix chemically treated to denature and stabilize the DNA in the biospecimen and renders the specimen biohazard free. The paper is also infused with an indicator dye that changes color, from purple to white, when the specimen is applied, thereby confirming that women performed the procedure properly.
Fig. 1.
HPV self-collection instructions. This instruction was translated to Chinese and used during the study.
Women were instructed to hold the plastic end of the swab without touching the brush end, insert the brush until they meet resistance, which is about 6 cm, and then rotate the brush 3–5 times. After the brush was removed, the participants were asked to apply the sample onto the FTA card by pressing the brush onto the sample area and then rotate it 3–5 times, keeping the brush within the circle drawn on the card. Upon completion, subjects underwent the clinician-collection using a speculum and the same type of collection materials. After clinician-collection, a colposcopy exam was done and biopsy was taken if indicated by the exam. Biopsies were formalin fixed, paraffin embedded, sectioned into 4 μm thick slides, and stained with haematoxyin-eosin for diagnosis by a licensed pathologist.
2.3. HPV testing
Small pieces were cut from a 1-mm2 center section of the FTA card with a disposable razor blade and placed into a 1.5 ml microcentrifuge tube. A fresh razor blade was used for each card. The sections were vortexed in 1.5 mL DEPC water for 30 s and the water decanted. Fifty microliters of DEPC water were added to the sections and heated for 30 min at 95 °C to release the DNA After incubation, each sample was vortexed about 60s and then centrifuged for 30 s. A10-μL aliquot was removed for PCR and genotyping using the Roche HPV Linear Array (LA) test per the manufacturer’s instructions. LA detects 37 HPV genotypes (HPV 6, 11, 16, 18, 26, 31, 33, 35, 39, 40, 42, 45, 51–56, 58, 59, 61, 62, 64, 66–73, 81–84, 82v, and 89); HPV 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, and 68 were considered carcinogenic HPV genotypes. Results were also classified hierarchically according to a priori cancer risk (Tornesello et al., 2011): HPV 16 positive, else HPV 16 negative and HPV 18 positive, else HPV 16 and HPV 18 negative and positive for any other carcinogenic HPV genotype, else negative for all carcinogenic HPV genotypes and positive for a non-carcinogenic HPV genotype, else negative for all HPV genotypes.
2.4. Statistical analysis
Percent total and positive agreement with binomial 95% confidence intervals (95%CI) and kappa values with 95%CI were calculated as measures of agreement for detection of any HPV and any carcinogenic HPV between the clinician-collected and self-collected specimens. An exact version of the McNemar or symmetry chi-square test was used to test for differences in detection between the two specimen types. Paired results were stratified by median age or by VIA/VILI results.
3. Results
There was no difference in the prevalence of any HPV using the clinician-collected and self-collected specimens (32% vs. 30%, respectively, p = 0.6) (Table 1). There was 91% (95%CI = 86–95%) agreement, 76% (95%CI = 63–86%) positive agreement, and a kappa of 0.80 (95%CI = 0.70–0.90) between two specimens for detection of any HPV. There was no difference in the prevalence of any carcinogenic HPV using the clinician-collected and self-collected specimens (25% vs. 24%, respectively, p = 0.8). There was a 91% (95%CI = 86–95%) agreement, 69% (95%CI = 54–81%) positive agreement, and kappa of 0.75 (95%CI = 0.64–0.87) between two specimens for detection of any carcinogenic HPV. The agreement for the detection of any HPV or any carcinogenic HPV between specimens was similar in strata defined in median age (<41 or 41 and older) or whether women were positive or negative for VIA/VILI.
Table 1.
The percent agreement, positive agreement, and Kappa values for detection of any of 37 human papillomavirus (HPV) genotype or any of 13 carcinogenic HPV genotypes between clinician-collected cervical specimens and self-collected cervicovaginal specimens smeared on a FTA transport device collected from the same woman (n = 174). The results are present for all women, and stratified on whether women were visual inspection with acetic acid positive or negative and on the median age (41 years old). An exact version of the McNemar chi-square test was used to test for differences in testing positive.
| Clinician/self |
% agreement |
% positive agreement |
Kappa |
P | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Neg/neg | Pos/neg | Neg/pos | Pos/pos | % | 95% CI | % | 95% CI | Value | 95% CI | |||
| All women (n = 174) | ||||||||||||
| Any HPV |
n %row |
112 64% |
9 5% |
6 3% |
47a 27% |
91% | 86–95% | 76% | 63–86% | 0.80 | 0.70–0.90 | 0.6 |
| Carcinogenic HPV |
n %row |
123 71% |
9 5% |
7 4% |
35b 20% |
91% | 86–95% | 69% | 54–81% | 0.75 | 0.64–0.87 | 0.8 |
| VIA+ (n = 63) | ||||||||||||
| Any HPV |
n %row |
37 59% |
4 6% |
4 6% |
18 29% |
87% | 77–94% | 64% | 44–81% | 0.72 | 0.54–0.90 | 1 |
| Carcinogenic HPV |
n % row |
40 63% |
4 6% |
5 8% |
14 22% |
86% | 75–93% | 61% | 39–80% | 0.66 | 0.45–0.86 | 0.7 |
| VAI− (n = 111) | ||||||||||||
| Any HPV |
n % row |
75 68% |
5 5% |
4 4% |
29 26% |
94% | 87–97% | 76% | 60–89% | 0.81 | 0.69–0.93 | 0.3 |
| Carcinogenic HPV |
n %row |
83 75% |
5 5% |
2 2% |
21 19% |
94% | 87–97% | 75% | 55–89% | 0.82 | 0.69–0.95 | 0.3 |
Abbreviation: 95%CI, 95% confidence interval.
29 (61.7%) had perfect concordance, 16 (34.0%) had partial concordance, and 2 (4.3%) had no concordance for any HPV genotypes detected.
30 (85.7%) had perfect concordance and 5 (14.3%) had partial concordance for carcinogenic HPV genotypes detected.
When the HPV results were categorized hierarchically according to cervical cancer risk (Table 2), there was no difference in the distribution of the HPV results for the clinician- and self-collected specimens (p = 0.7). There was 88% (95%CI = 82–92%) agreement and a kappa of 0.76 (95%CI = 0.66–0.85) for the categories of HPV. The agreement within categories was 67% for HPV 16, 100% for HPV 18, 77% for other carcinogenic HPV genotypes, 67% for non-carcinogenic HPV genotypes, and 95% for HPV negative.
Table 2.
A comparison of detection of human papillomavirus (HPV) DNA, categorized according to cancer risk (HPV16>HPV18>other carcinogenic HPV>non-carcinogenic HPV > negative), between clinician-collected cervical specimens and self-collected cervicovaginal specimens smeared on a FTA transport device collected from the same wnman (n = 174) Highlighted in gray are the concordant results
| Self-Collection | Total | |||||||
|---|---|---|---|---|---|---|---|---|
| Negative | Non-Carcinogenic | Carcinogenic | HPV 18 | HPV 16 | ||||
| Clinician Collection | Negative | n % row |
112 95% |
1 1% |
4 3% |
0 0% |
1 1% |
118 100% |
| Non-Carcinogenic | n % row |
2 17% |
8 67% |
1 8% |
0 0% |
1 8% |
12 100% |
|
| Carcinogenic | n % row |
3 12% |
2 8% |
20 77% |
1 4% |
0 0% |
26 100% |
|
| HPV 18 | n % row |
0 0% |
0 0% |
0 0% |
3 100% |
0 0% |
3 100% |
|
| HPV 16 | n % row |
4 27% |
0 0% |
1 7% |
0 0% |
10 67% |
15 100% |
|
|
| ||||||||
| Total | n % row |
121 70% |
11 6% |
26 15% |
4 2% |
12 7% |
174 100% |
|
Biopsy was taken from 62 (36%) patients: 1 (2%) had cervical cancer, 8 (13%) had cervical intraepithelial neoplasia grade 2 (CIN2) or grade 3 (CIN3), 2 (3%) had CIN 1, and the other 49 (79%) had no CIN. Among women with CIN2, CIN3, or cervical cancer, 9 of 9 (100%) tested positive for carcinogenic HPV on the clinician-collected specimens and 7 of 9 (78%) tested positive for carcinogenic HPV on the self–collected specimens.
4. Discussion
Similar to previous studies using liquid based collection media (Petignat et al., 2007), this study also found reasonable concordance for HPV DNA detection between paired collections clinician-collected cervical specimen and a self-collection cervicovaginal specimen applied to the FTA membranes. The kappa observed in this study (0.75) was better than kappa from a large systematic review of self vs. clinician-collected specimens (0.66) (Petignat et al., 2007). Using the FTA cartridge for cervicovaginal self-collection for HPV DNA testing is a promising alterative to the traditional liquid based transport medium. In many aspects, the FTA cartridge is superior to liquid-based medium. For example, samples are kept dry at ambient temperature on the FTA card, thus avoiding high cost and logistical challenges associated with transporting flammable and bio-hazardous liquid material. These benefits plus the small size of the cards (7.3 cm × 3.8 cm) make the FTA cartridge suitable to be sent by regular mail, which is more difficult for liquid based medium. In addition, the FTA card contains an indicating dye, which changes the color of the filter paper once DNA is detected. This provides instant verification of sample capture that is easily visible to the women, which is not possible with liquid based medium. By providing direct feedback, FTA card may improve the women’s confidence in their own ability to collect the specimen.
The benefits of the FTA cartridge are appealing to both public health practitioners and clinicians. It offers public health practitioners a more feasible and cost-effects transport method for large scale population based HPV screening, and it allows clinicians to offer their patients an alternative to a speculum exam for the collection of cervical sample for HPV DNA testing. Self-sampling at home can be offered to patients who cannot or are unwilling to travel to clinic, which could increase screening coverage (Sowjanya et al., 2009; Tisci et al., 2003).
Given the acceptability of the sampling method to women (Guan et al., 2012), reasonable performance in a number of pilot studies (Gravitt et al., 2011; Sowjanya et al., 2009; Lenselink et al., 2009), and the potential utility of the FTA device, larger-scale studies with sufficient endpoints are warranted. Since in low-resource settings it may be unrealistic to use clinic-based screening due to the general lack of such facilities and the large number of unscreened population, it will be particularly important to validate that women can successfully use a kit that incorporates the FTA device for specimen transport in the privacy of their home and achieve reasonable clinical performance.
Finally, it will be important to pair the FTA device with realistic DNA testing protocols that can work in the most basic laboratory settings, such as those found in most non-urban low-resource settings. Although it was found that the PCR-based method used in this study worked well, the testing was done in a state-of-the-art laboratory that takes PCR contamination precautions that may not be achievable in those settings. And as used in this study, punching out the membrane from the FTA device is laborious and has significant potential for cross contamination if sufficient precautions are not taken. Of note, one non-PCR, signal amplification test, Hybrid Capture 2, performed poorly compared to a PCR-based method using FTA devices (De Bie et al., 2011). This suggests that further protocol development may be needed to use non-PCR DNA testing methods, such as HC2 and careHPV (Qiagen, Gaithersburg, MD, USA), for FTA-transported specimens. This study provides clues for the comparable characteristics of clinician-collected and self-collected specimens captured by the FTA cards. Based on this study, further comparison among HC2, CE-validated PCR testing method such as Roche Cobas 4800, and careHPV are needed for the clinical validation of FTA cards.
5. Conclusion
Self-collection using the FTA elute cartridge for HPV DNA testing is a promising method of transport to be used in screening programs. There was high concordance between self-collection and clinician collection in detecting carcinogenic HPV DNA The FTA card is small, easy to use, stores the sample dry at room temperature, and can be shipped by regular mail. These benefits of the FTA cartridge may make it superior to the liquid-based media. Additional, sufficiently powered studies are now needed to assess the clinical performance for detection of CIN2 or more severe cervical disease.
Acknowledgements
This study was funded by the Cancer Institute/Hospital, Chinese Academy of Medical Sciences Department of Epidemiology, the Johns Hopkins University Departments of Epidemiology and Molecular Microbiology and Immunology, and the Chinese National Cancer Screening Project for Cervical Cancer and Breast Cancer Among Rural Women. The FTA cards used in this study were donated by GE healthcare. Dr. Castle was previously supported by the Intramural Research Program of the NIH/NCI.
Footnotes
Conflict of interest
The authors have no conflicts of interest.
References
- Arbyn M, Paraskevaidis E, Martin-Hirsch P, Prendiville W, Dillner J. Clinical utility of HPV-DNA detection: triage of minor cervical lesions, follow-up of women treated for high-grade CIN: an update of pooled evidence. Gynecol. Oncol. 2005;99(Suppl. 3):S7–S11. doi: 10.1016/j.ygyno.2005.07.033. [DOI] [PubMed] [Google Scholar]
- Bais A, Rebolj M, Snijders PJ, Schipper F, Meulen D, Verheijen R, Voorhorst F, van Ballegooijen M, Meijer CJ, Helmerhorst TJ. Triage using HPV-testing in persistent borderline and mildly dyskaryotic smears: proposal for new guidelines. Int. J. Cancer. 2005;116:122–129. doi: 10.1002/ijc.20958. [DOI] [PubMed] [Google Scholar]
- Bandyopadhyay S, Austin RM, Dabbs D, Zhao C. Adjunctive human papillomavirus DNA testing is a useful option in some clinical settings for disease risk assessment and triage of females with ASC-H Papanicolaou test results. Arch. Pathol. Lab. Med. 2008;132:1874–1881. doi: 10.5858/132.12.1874. [DOI] [PubMed] [Google Scholar]
- Cuzick J, Szarewski A, Cubie H, Hulman G, Kitchener H, Luesley D, McGoogan E, Menon U, Terry G, Edwards R, Brooks C, Desai M, Gie C, Ho L, Jacobs I, Pickles C, Sasieni P. Management of women who test positive for high-risk types of human papillomavirus: the HART study. Lancet. 2003;362:1871–1876. doi: 10.1016/S0140-6736(03)14955-0. [DOI] [PubMed] [Google Scholar]
- De Bie RP, Schmeink CE, Bakkers JM, Snijders PJ, Quint WG, Massuger LF, Bekkers RL, Melchers WJ. The indicating FTA elute cartridge a solid sample carrier to detect high-risk HPV and high-grade cervical lesions. J. Mol. Diagn. 2011;13:371–376. doi: 10.1016/j.jmoldx.2011.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gravitt PE, Belinson JL, Salmeron J, Shah KV. Looking ahead: a case for human papillomavirus testing of self-sampled vaginal specimens as a cervical cancer screening strategy. Int. J. Cancer. 2011;129:517–527. doi: 10.1002/ijc.25974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guan Y, Castle PE, Wang S, Li B, Feng C, Ci P, Li X, Gravitt P, Qiao YL. A cross-sectional study on the acceptability of self-collection for HPV testing among women in rural China. Sex Transm. Infect. 2012 doi: 10.1136/sextrans-2012-050477. http://dx.doi.org/10.1136/sextrans-2012-050477 (Published Online First: 29 May 2012) [DOI] [PubMed]
- Gustavsson I, Lindell M, Wilander E, Strand A, Gyllensten U. Use of FTA card for dry collection, transportation and storage of cervical cell specimen to detect high-risk HPV. J. Clin. Virol. 2009;46:112–116. doi: 10.1016/j.jcv.2009.06.021. [DOI] [PubMed] [Google Scholar]
- Gustavsson I, Sanner K, Lindell M, Strand A, Olovsson M, Wikstrom I, Wilander E, Gyllensten U. Type-specific detection of high-risk human papillomavirus (PV) in self-sampled cervicovaginal cells applied to FTA elute cartridge. J. Clin. Virol. 2011;51:255–258. doi: 10.1016/j.jcv.2011.05.006. [DOI] [PubMed] [Google Scholar]
- Katki HA, Kinney WK, Fetterman B, Lorey T, Poitras NE, Cheung L, Demuth F, Schiffman M, Wacholder S, Castle PE. Cervical cancer risk for women undergoing concurrent testing for human papillomavirus and cervical cytology: a population-based study in routine clinical practice. Lancet Oncol. 2011;12:663–672. doi: 10.1016/S1470-2045(11)70145-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenselink CH, de Bie RP, van Hamont D, Bakkers JM, Quint WG, Massuger LF, Bekkers RL, Melchers WJ. Detection and genotyping of human papillomavirus in self-obtained cervicovaginal samples by using the FTA cartridge: new possibilities for cervical cancer screening. J. Clin. Microbiol. 2009;47:2564–2570. doi: 10.1128/JCM.00285-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petignat P, Faltin DL, Bruchim I, Tramer MR, Franco EL, Coutlee F. Are self-collected samples comparable to physician-collected cervical specimens for human papillomavirus DNA testing? A systematic review and meta analysis. Gynecol. Oncol. 2007;105:530–535. doi: 10.1016/j.ygyno.2007.01.023. [DOI] [PubMed] [Google Scholar]
- Sankaranarayana R, Nene BM, Shastri SS, Jayant K, Muwonge R, Budukh AM, Hingmire S, Malvi SG, Thorat R, Kothari A, Chinoy R, Kelkar R, Kane S, Desai S, Keskar VR, Rajeshwarkar R, Panse N, Dinshaw KA. HPV screening for cervical cancer in rural India. N. Engl. J. Med. 2009;360:1385–1394. doi: 10.1056/NEJMoa0808516. [DOI] [PubMed] [Google Scholar]
- Schiffman M, Glass AG, Wentzensen N, Rush BB, Castle PE, Scott DR, Buckland J, Sherman ME, Rydzak G, Krik P, Lorincz AT, Wacholder S, Burk RD. A long-term prospective study of type-specific human papillomavirus infection and risk of cervical neoplasia among 20,000 women in the Portland Kaiser cohort study. Cancer Epidemiol. Biomarkers Prev. 2011;20:1398–1409. doi: 10.1158/1055-9965.EPI-11-0206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sowjanya AP, Paul P, Vedantham H, Ramakrishna G, Vidyadhari D, Vijayaraghavan K, Laksmi S, Sudula M, Ronnett BM, Das M, Shah KV, Gravitt PE, Community Access to Cervical Health Study Group Suitability of self-collected vaginal samples for cervical cancer screening in periurban villages in Andhra Pradesh, India. Cancer Epidemiol. Biomarkers Prev. 2009;18:1373–1378. doi: 10.1158/1055-9965.EPI-08-1171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tisci S, Shen YH, Fife D, Huang J, Goycoolea J, Ma CP, Belinson J, Huang RD, Qiao YL. Patient acceptance of self-sampling for human papillomavirus in rural China. J. Low. Genit. Tract. Dis. 2003;7:107–116. doi: 10.1097/00128360-200304000-00007. [DOI] [PubMed] [Google Scholar]
- Tornesello ML, Losito S, Benincasa G, Fulciniti F, Botti G, Greggi S, Buonaguro L, Buonaguro FM. Human papillomavirus (HPV) genotypes and HPV 16 variants and risk of adenocarcinoma and squamous cell carcinoma of the cervix. Gynecol. Oncol. 2011;121:32–42. doi: 10.1016/j.ygyno.2010.12.005. [DOI] [PubMed] [Google Scholar]