Abstract
Despite having identified key physiological and behavioral risk factors, the prevalence of hypertension continues to rise, affecting two-thirds of American adults 60 years or older. An important condition in its own right, hypertension is also a leading risk factor for cardiovascular diseases; thus, identifying additional modifiable determinants remains a public health priority. Psychological states and negative emotions more specifically have been proposed as risk factors, but the research findings are inconsistent. Additional prospective studies have recently been published increasing the availability of longitudinal data. The aim of this literature review is to evaluate these findings focusing on those from the last three years. We synthesize current research on whether negative (e.g., depression, anxiety) or positive (e.g., optimism) emotion-related factors are associated with high blood pressure onset. We discuss discrepant findings and propose considering emotion regulation as a novel approach to explain inconsistencies. Finally, we provide thoughts on future research directions.
Keywords: hypertension, anxiety, depression, anger, emotion regulation, optimism
Introduction
Hypertension is a highly prevalent condition affecting one out of three American adults and explaining 41.5% of mortality rates [1]. This condition contributes to health disparities, being more prevalent in non-white than white individuals, and varies across gender and age groups [1]. Furthermore, hypertension is projected to increase by 8.4% with an associated estimated cost of $274 billion by 2030 [1]. Both non-modifiable (e.g., age, ethnicity, genetics) and modifiable (e.g., physical activity, tobacco use, diet) risk factors for hypertension have been identified [1,2]. However, strategies to reduce risk have had limited success so far, suggesting additional determinants may be at play or more targeted interventions are needed. Psychosocial factors, including anxiety, anger and social support, have been identified as potential risk or protective factors, which may provide novel modifiable targets for intervention. However, much of the research to date is based on cross-sectional studies, which impedes interpretation regarding causality.
Notwithstanding, a quantitative review of 15 prospective studies published between 1972 and 2000 demonstrated that, compared to individuals reporting few psychological symptoms (i.e., anxiety, depression and anger), those with high levels had an 8% higher risk of hypertension, with a stronger association among black compared to white participants [3]. However, many of these studies included only male participants and short follow-up periods (mode: 3 years). As methods of assessing psychological factors have increasingly been refined (e.g., single-item vs. validated scale) and longer follow-up periods are available, considering recent research may further inform our understanding. Moreover, recent research has also considered protective psychological factors, contributing to a more comprehensive insight.
Thus, the aim of the current review is to summarize recent research examining known (i.e., anxiety, depression, anger) and more novel (i.e., well-being) psychological factors that may influence hypertension incidence. Some integrative reviews on the role of psychological determinants on hypertension have been published [4-7], but those considering the role of emotion-related factors comprehensively are outdated [3,8]. We did not conduct a formal systematic review but rather identified and discussed key studies from the last three years to assess our current state of understanding and to develop new directions for future research.
Methodological approach
Literature searches within PubMed and PsycInfo databases targeted individual studies, prior systematic reviews, and meta-analyses, written in English or French. Additional studies were obtained through bibliographies of eligible articles. Individual studies published between January 2012 and September 2015 were included if: 1) the study design was longitudinal; 2) the sample consisted of human adults; 3) the main exposure was psychological distress (i.e., symptoms of anxiety, depression, anger/hostility) or positive psychological well-being (PPWB; i.e., optimism, emotional vitality, life satisfaction, happiness, positive affect); and 4) the primary outcome was incident hypertension (i.e., directly assessed blood pressure (BP), report of antihypertensive medication, report of physician-diagnosed hypertension).
Due to space constraints, other relevant psychosocial factors such as discrimination and social support/isolation [2,5,6,9,10] were not considered. Articles were not included if they: 1) tested experimental tasks or psychosocial interventions; 2) considered hypertension as a risk factor for psychological distress; 3) were based on clinical/medical samples; or 4) monitored BP with a 24-hour ambulatory assessment, which does not provide information on hypertension onset specifically. Consequently, most of the retained epidemiologic studies used the strongest methods available for assessing associations: sample of normotensive individuals, longitudinal design with up to 25 years of follow-up time, and adjustment for conventional potential confounders including demographic characteristics (e.g., age, education) and health behaviors (e.g., smoking, physical activity).
Psychological risk factors for incident hypertension
The notion that psychological distress affects BP has drawn scientific attention since the early 1900s [11-13]. Initial empirical investigations mainly focused on anger, though anxiety and depression were also considered [3,14]. More recently, PPWB has been of interest [15-17]. A related body of research has also studied how stress influences BP [18,19] and although sometimes used interchangeably, it is important to distinguish emotions from stress. Stress is experienced when individuals judge external demands to surpass their capacity to cope [20]. Because it remains difficult to operationalize this phenomenon consistently [21], some investigators have suggested that emotions, defined as positive or negative responses rising from a specific situation [22], may provide a more accurate assessment of one’s interaction with the environment [21,23,24]. Emotions can be categorized as states, when they are transitory responses to particular situations, or traits, reflecting a more stable disposition to experience specific emotions [25]. By adulthood, individuals have developed attributes and cognitions (traits) that affect the frequency with which they experience particular emotional states (e.g., hostile individuals experience anger more frequently than less hostile counterparts).
Clinical disorders (e.g., major depression), reflecting persistent and debilitating emotions, are usually diagnosed by a trained clinician with a psychiatric interview. Self-report questionnaires, either assessing state or trait emotion-related constructs, cover a wide range of symptoms severity and require less time to complete. However, they generally cannot be used to diagnose a psychiatric condition. Questionnaires assessing PPWB constructs (e.g., optimism) often have no validated clinical cutpoints.
Several pathways have been identified to explain how emotions affect BP and thereafter, hypertension onset. Both clinical and sub-clinical levels of emotion-related factors directly impact biological pathways like the sympathetic nervous system and the hypothalamic-pituitary-adrenal axis (HPA), which influence a cascade of processes involved in regulating BP [26-32]. Emotions can also alter behaviors, subsequently altering risk of hypertension. For instance, higher levels of anxiety and depression are related to greater alcohol and tobacco consumption [26,33,34], whereas PPWB is associated with higher likelihood of being physically active and eating a healthy diet [32]. Indeed, health behaviors could either be confounders or mediators of the associations of interest, although both possibilities have not been tested separately.
Anxiety
Clinical disorders like phobia and generalized anxiety disorder affect nearly 30% of Americans [35], while sub-clinical manifestations, such as feeling nervous and worried, are experienced by even more individuals. Since 2012, empirical findings have generally shown consistent associations between anxiety symptoms (clinical and sub-clinical) and higher risk of high BP or hypertension [36-39], but some null [37,40,41] and even protective [41] relationships have been observed too.
For instance, in one study following 1,638 individuals over 25 years, a trained nurse obtained two measures of resting BP and data about medication usage at four time points, where participants also completed measures of state anxiety and depression symptoms [41]. After adjusting for potential confounders and antidepressant use, individuals reporting lifetime anxiety or depression (i.e., symptoms above clinical cut-points at ≥3 out of 4 time points) had significantly lower systolic blood pressure (SBP) levels at the last time assessment, compared to those never meeting case-criteria. No associations with diastolic blood pressure (DBP) or hypertension case status (i.e., SBP≥140mmHg, DBP≥90mmHg or antihypertensive use) were evident. While results remained similar when excluding participants using antihypertensive medication, differential participation is hypothesized as the analytic sample only comprised individuals with complete data on psychological symptoms and covariates.
A recent meta-analysis (8 prospective studies; N=80,146) reported a 55% higher risk of incident hypertension for anxious versus non-anxious individuals [4]. For example, among 455 Dutch older adults, more versus less anxious individuals at baseline had 10% higher odds of reporting hypertension five years later, even after adjusting for potential confounders at baseline including SBP and antihypertensive medication [39]. Because hypertension was defined by a self-report of lifetime diagnosis, reverse causation cannot be ruled out – having hypertension could engender higher anxiety. When participants taking antihypertensive were excluded, similar findings were noted, hence reducing concerns about reverse causation.
In another study in the meta-analysis, researchers completed an psychiatric interview among 190 middle-aged Canadian adults (MOMSI study) and considered risk of developing hypertension (ncases=16) over the following year [38]. Individuals with anxiety disorders had 7.25 higher odds (95%CI=1.90-27.74) of having physician-diagnosed hypertension or antihypertensive medication at follow-up, after adjusting for standard covariates, psychotropic medication, and comorbid mood disorder. Consistent and more stable estimates were obtained in a larger study published after the release of the meta-analysis, which included 52,095 normotensive adults with 8,422 incident cases occurring over 12 to 34 years after onset of mental health disorder. These retrospective results from the World Mental Health Surveys (WMSH) showed that various anxiety disorders were associated with a 10-30% higher odds of incident hypertension, after adjusting for confounders including psychiatric comorbidities [37].
Depression
Sadness, hopelessness, and lack of interest/pleasure are examples of depressive symptoms, which can reach the threshold of a major depression if they persist for at least two weeks and impair functioning [42]. Among U.S. adults, 7% report having major depressive disorder in the past 12-months [43] and 21% report a lifetime prevalence of any mood disorders, including major depressive disorder, dysthymia (a milder depressive disorder), and bipolar depressive disorders [35].
Overall, despite some mixed results [38,41], recent findings suggest a positive association between depressive symptoms or disorder and high BP [7,37,39,44]. A meta-analysis published in 2012 (9 prospective studies; N=22,367) found that depression or depressive symptoms was associated with a 42% higher risk of incident hypertension [7]. While most studies adjusted for demographic characteristics and some health-related behaviors, the extent to which additional confounders were considered varied. An elevated risk of depression-related incident hypertension was evident among cohorts with follow-up periods longer than 9.6 years and in samples with, surprisingly, lower baseline prevalence of depression. White participants with depression had a non-significantly lower risk than non-Whites, although this difference is inconclusive because of the limited number of non-white participants in the available studies.
Since the meta-analysis, the study using data from the WMSH (described above) also found an association between depression status and incident hypertension [37]. Major depressive episode or dysthymia were associated with 20% greater odds of hypertension in the following year after adjusting for confounders including other psychiatric disorders. In the MOMSI study (described above), no association was found between mood disorders and incident hypertension [38]. Though inconsistent with previous findings, this may be due to the limited power (ncases=16) or to the heterogeneity of mood disorders category, which unlike other studies included bipolar disorder. Bipolar disorders were unrelated to incident hypertension in the WMSH study [37], but it is not yet clear if different mood disorders have divergent effects.
Anger
Anger is characterized has having affective, behavioral, and cognitive dimensions [45,46], each studied in relation to BP. The affective dimension of anger arises out of feelings of injustice and can vary in intensity, but is considered a stable disposition. Regarding the behavioral dimension, anger may be expressed outwardly (e.g., aggression toward others) or not expressed (e.g., suppression, withholding). Hostility, the cognitive dimension, refers to the tendency to make hostile attributions or have a cynical attitude. While these dimensions are often used interchangeably, they may affect BP differently [47]. Accordingly, in the 2002 quantitative review discussed above, a higher risk of hypertension was associated with higher levels of anger experience and expression but not higher levels of hostility, among mostly male samples. In parallel, a 2003 meta-analysis (15 cross-sectional studies; N=2,213) showed that experiencing anger was associated with higher SBP, but not DBP, whereas expressing anger was related to lower DBP only in mostly Caucasian participants [48].
Given earlier research more frequently investigated anger constructs than anxiety and depressive manifestations [3,14], it is surprising that few prospective studies with up-to-date methodology considering anger have been conducted in the last decade, with none since 2012. Although recent cross-sectional research is available [49,50], this design remains less informative with regard to establishing if anger truly influences hypertension onset. Hence, prospective studies targeting diverse anger constructs among varied samples (e.g., women, non-white individuals) are needed.
Positive Psychological Well-being
Most recently, investigators have posited PPWB might be worth investigating, as it represents more than the simple absence of psychological distress [51-53]. Life satisfaction, positive affect, purpose in life, optimism and emotional vitality (i.e., an active engagement with the world and sense of enthusiasm) are amongst the most studied indicators of PPWB [32,51,52]. A recent review of the literature on PPWB in relation to cardiovascular function [32] reported heterogeneous results among mostly cross-sectional studies. This heterogeneity might arise from state vs. trait measures having different associations with BP. Indeed, while state well-being is generally associated with higher BP in experimental settings, trait well-being is more often associated with lower resting BP over time [32].
Within the last three years, only one longitudinal study has specifically examined PPWB and onset of hypertension [54]. Participants were 6,384 healthy middle-aged British adults, who completed self-reported measures on optimism and emotional vitality. Participants with high vitality at baseline had a 9-11% lower risk of incident hypertension over more than a decade of follow-up, compared to those with initially low levels. The relationship remained significant after adjusting for known cardiovascular risk factors and negative affect. Optimism’s association, measured with a single item, was not significant, calling for further research with multi-item measures. These findings are consistent with earlier longitudinal studies that revealed somewhat unstable results [15-17]. For instance, among 1,036 normotensive adults aged 55-70 years, baseline mental vitality (similar to emotional vitality) was significantly associated with 46% lower odds of developing hypertension two years later in demographics-adjusted models [16]. However, the association became non-significant and with wider confidence intervals after adjusting for health behaviors and negative affect, perhaps because of the small number of cases.
Given the preliminary findings, additional work on protective psychological factors is justified [52], particularly since PPWB is strongly linked to other aspects of cardiovascular health [32,52]. PPWB seems also related to health behaviors like physical activity and healthy diet [32]. If PPWB indeed reliably influences the risk of developing hypertension, then subsequent research should directly test whether a key mechanism is by improving lifestyle.
Summary of the recent findings in the context of prior mixed findings
Like prior reviews [4,5,7,10,26-29,55], research from the last three years suggests that anxiety and depression are associated with a higher risk of hypertension. Although the associations appear to be in expected directions, less firm conclusions can be drawn regarding the specific role of anger and PPWB, with fewer methodologically rigorous studies published recently. That said, the latest research provides a more consistent picture in contrast with earlier literature where more mixed results were obtained.
Methodological issues may explain the earlier inconsistent results. First, the relation between distress and hypertension may differ across subgroups [37,44,56], obscuring associations when groups are combined. For example, one study conducted prior to 2012 among 2,087 adults revealed that higher BP was associated with more depressive symptoms in women only [44]. Similarly, among 10,302 adults, increasing depressive symptoms were associated with lower hypertension odds among younger (35-39 years) but with higher odds among older participants (≥40 years) [56]. However, reverse causation can be suspected because timing of assessments of depression and hypertension overlapped in these longitudinal studies. Different lengths of follow-up could also lead to mixed findings as prior studies with follow-up period of less than 5 years were more likely to report null results [7]. Hypertension indeed develops more insidiously than other conditions (e.g., infectious disease), and emotion-related factors might influence BP through slower-acting pathways (e.g., behavioral changes, biological processes that accumulate over time).
Inconsistent results may also be due to the variety of instruments used to measure emotion-related factors (e.g., self-reported questionnaires vs. clinical interviews; assessing state vs. trait). Heterogeneity in definitions and measurements could also translate into differences in the estimated prevalence of distress at baseline, making it appear that lower levels of exposure are associated with a higher risk of developing hypertension [7]. If the higher prevalence of anxiety/depression results from including individuals with milder symptoms, and if those less distressed individuals are less likely to develop hypertension, they thereby dilute the apparent risk associated with distress. Furthermore, participants with lower-to-moderate levels of psychological distress may be less likely to consult a physician for their overall well-being, and therefore less likely to have their BP checked [38,39], hence possibly driving results towards the null. Comparably, definitions/measurements of hypertension are highly heterogeneous (e.g., self-reported diagnosis, antihypertensive medication, SBP or DBP thresholds either jointly or separately). Moreover, misclassification may occur, such as in “white-coat” hypertension where someone who only has high BP in the doctor’s office is characterized as hypertensive [40].
The inverse associations observed in some studies remain puzzling. Of note, individuals from highly developed countries, who are well represented in the cited studies, tend to become less anxious/depressed and more satisfied/happy as they age [52]. Interestingly, there is a parallel secular trend of increasing hypertension with age. If residual confounding exists, it could appear that decreased distress levels are accompanied by elevated BP. Besides, the relationship between psychological determinants and hypertension may not be linear, as found in a prior cross-sectional study where frequent panic attacks were related to higher and lower levels of SBP [57]. Inverse associations could rise from the “depletion of susceptibles” phenomenon too [58], whereby if hypertension onset happens at a specific time point after the emotion-related construct being measured for the majority of the exposed group, the likelihood of hypertension onset calculated afterwards amongst the remaining exposed subgroup (i.e., the uncensored participants) will decrease over time.
Finally, given that both positive and negative emotion-related factors are related to BP, a higher order process - such as how psychological experience is cognitively or behaviorally managed - may be at play. Emotions are generally viewed as adaptive processes [22,24], so any given emotion experience, either negative or positive, may not harm health but if the emotion persists or worsens in severity, it may become problematic.
Emotion regulation
Emotion regulation is conceptualized as the processes, either adaptive or maladaptive, by which individuals monitor and manage emotional experiences and responses [22]. Individuals who generally employ adaptive strategies are able to meet life’s demands more efficiently, compared to those who adopt maladaptive strategies more often. Processes related to regulating emotions are learned in childhood through socialization and experience, and tend to be favored/maintained throughout adulthood [31].
Two key regulatory processes that have been identified are cognitive reappraisal, altering emotions related to an event by reinterpreting the meaning of that event, and expressive suppression, defined as inhibiting emotional behavior [53,59,60]. An up-to-date meta-analysis (48 studies; N=21,150) suggested cognitive reappraisal may be more adaptive as it is associated with higher psychological well-being, whereas expressive suppression is more maladaptive as it is strongly related to higher psychological ill-being [53]. According to recent research, (in)effective emotion regulation also relates to physical health [31]. Preliminary results from experimental studies suggest that endorsing adaptive strategies is associated with healthier cardiovascular function, including BP [61-65]. For instance, neutral, negative and positive pictures were shown to 53 normotensive men, who used cognitive reappraisal strategies to control their feelings about the pictures [61]. A healthier cardiovascular response occurred when positive reappraisal was applied, compared to when no regulation was implemented.
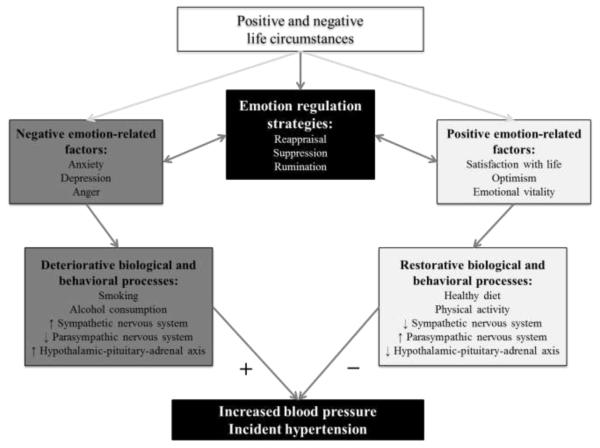
While no longitudinal studies with non-clinical samples have investigated the emotion regulation-hypertension association specifically, a theoretical model suggested by Gerin and colleagues [66] is noteworthy. They proposed rumination, another maladaptive regulation strategy, as one possible mechanism linking stress with hypertension. Rumination of emotionally-charged cognitions happening after an acute stressor induces transient physiological activation [66]. When regulation is ineffective however, rumination will persist and/or reemerge even after the stressful situation resolves. Such ruminative activity can cause long-term perturbations in the autonomic, HPA, and immune systems, implicated in hypertension onset [66]. Rumination as a determinant for hypertension is plausible given its association with both higher psychological distress and sustained high BP levels in recovery periods of experimental studies [6,66]. While the role of emotion regulatory processes on hypertension onset remains understudied, we suggest this is an important new direction for consideration. To that end, we propose a testable model of the possible interrelationships between emotions-related constructs, biological/behavioral pathways and incident hypertension (see Figure 1).
Figure 1.
Model of the potential relationships between emotion-related constructs, emotion regulation, biological/behavioral pathways and incident hypertension.
Notes. Model adapted from Boehm & Kubzansky, 2012; Gerin et al., 2012; Mittleman & Mostofsky, 2011. For the purpose of this review, other relevant psychological risk factors (e.g., social isolation, sleep, job strain) and mediators (e.g., body mass index, alteration of the immune system, inflammation) are omitted from this figure. Some other emotion regulation strategies (e.g., catastrophizing, planning) and positive emotion-related factors (e.g., purpose in life, positive affect) are not shown for the sake of parsimony. In addition, while bidirectional effects between emotion-related factors and biological/behavioral processes are likely, in keeping with the focus of the review, only single direction arrows are shown.
Future directions
Future work will need to address the methodological and conceptual issues identified above. Additional methodological, statistical and clinical considerations are also recommended. The prevalence of hypertension rises quickly with age, from around 40% among individuals aged 40-59 years to 70% among those aged 60-79 years [1]. Consequently, considering subclinical levels of BP (e.g., SBP=120–139mmHg, DBP=80–89mmHg) or percentiles (e.g., ≤90th percentile, as recommended for children and adolescents) [67,68] as outcomes may provide early indicators of risk among adults. Because there are fewer cases of hypertension before midlife, looking at such pre-conditions among younger populations [e.g., 69] is relevant and leads to the hypothesis that early-life interventions could have a greater public health impact than treating hypertension once it is detected. Despite evidence of disparities, research available for the current review was conducted primarily among white individuals, fostering additional research amongst more diverse ethnic/cultural samples [53,63,70]. Possible sex-related differences in psychological determinants of hypertension [37,49] also deserve attention, given the higher prevalence of anxiety and depressive symptoms among women, and hostility among men [35,71,72].
Implementation of state of the art statistical methods should be explored. For example, few longitudinal studies have implemented analytic strategies like inverse probability weights [73] to mitigate the effects of differential participation related to attrition over time. Even though the emotions-BP relationship is frequently cited as bidirectional, limited research has favored statistical models for testing such a hypothesis, including path analysis [74]. Repeated measures of emotion-related factors and confounders are valuable, as variables like depressive symptoms, physical activity and smoking habits may change over time. Using techniques such as marginal structural models and inverse probability weighting would also enable appropriate adjustment for time-updated confounders lying on the causal pathway [75].
Considering emotion regulation as a higher order determinant and distinguishing the specific impact of each regulatory strategy on incident hypertension is also an important new approach. Combinations of emotions and processes should also be considered as they may exacerbate negative impact on cardiovascular health [72]. For instance, between two individuals who frequently experience high levels of anger (emotion), one who ruminates (maladaptive strategy) might be at higher risk of hypertension compared to another who reappraises (adaptive strategy).
From a clinical perspective, longitudinal intervention studies are needed to evaluate whether reducing distress, enhancing PPWB and/or improving emotion regulation abilities can alter the likelihood of developing hypertension. For example, cognitive therapy [76] could improve individuals’ ability to engage in cognitive reappraisal. Similarly, some mindfulness techniques seeking to direct people’s attention away from their negative thoughts [77] could reduce rumination. Although meditation techniques [78-81] and yoga [82,83] seem effective in lowering BP, there is risk of bias related to small samples, short follow-up periods and experimenter effect in pioneer studies [79-82]. Accordingly, American Heart Association stated that yoga and most meditation techniques were not recommended at this time [84], indicating the urgent need for more rigorous research on these approaches, as they have few side effects, tend to be inexpensive, and could be used as adjuvant to healthy diet and regular physical activity [84].
Conclusion
This literature review summarized the findings from studies published in the last three years that looked at potential emotion-related determinants of incident hypertension. Research conducted prior 2012 yields inconsistent results that may partially be explained by methodological and sample differences across studies. Notwithstanding, there is accumulating empirical evidence that anxiety, depression and anger lead to increased risk of hypertension. Early results suggest that PPWB may be associated with a lower risk of incident hypertension, although more rigorous work is needed in this area. The current review has some limitations, however. While our review prioritized the most relevant literature, it is possible that some important suitable studies were not included. Considering other psychosocial (e.g., job stress, social support/isolation) will likely be useful. One innovative aspect of this review is to consider a broader construct, emotion regulation, to provide greater understanding of the findings with both negative and positive determinants.
Hypertension is a serious public health concern, with a 90% lifetime risk of incidence among middle-aged adults with normal BP [1]. Consequently, perspectives on potential determinants of hypertension have been expanded beyond the traditional biological and behavioral risk factors to now consider psychological variables [1,84]. A deeper understanding of these determinants will not only improve our prevention and intervention strategies for this widespread condition, but also lower the risk of other chronic diseases and ultimately improve longevity.
Acknowledgments
Dr. Trudel-Fitzgerald reports a postdoctoral fellowship from Canadian Institute of Health Research. Dr. Gilsanz reports funding from National Institute of Mental Health (T32MH017119) and a Yerby Postdoctoral Fellowship from Harvard T.H. Chan School of Public Health.
Footnotes
Drs. Mittleman and Kubzansky declare no conflicts of interest.
References
Papers of particular interest, published since 2012, have been highlighted as:
• Of importance
- 1 •.Go AS, et al. Heart disease and stroke statistics--2014 update: a report from the American Heart Association. Circulation. 2014;129(3):e28–e292. doi: 10.1161/01.cir.0000441139.02102.80. This report presents key information on hypertension, including clinical cutpoints of blood pressure levels, prevalence, age/gender/race/ethnicity differences, mortality rate and cost.
- 2.Havranek EP, et al. Social Determinants of Risk and Outcomes for Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation. 2015 doi: 10.1161/CIR.0000000000000228. [DOI] [PubMed] [Google Scholar]
- 3.Rutledge T, Hogan BE. A quantitative review of prospective evidence linking psychological factors with hypertension development. Psychosomatic Medicine. 2002;64(5):758–66. doi: 10.1097/01.psy.0000031578.42041.1c. [DOI] [PubMed] [Google Scholar]
- 4 •.Pan Y, et al. Association between anxiety and hypertension: a systematic review and meta-analysis of epidemiological studies. Neuropsychiatric Disease and Treatment. 2015;11:1121–30. doi: 10.2147/NDT.S77710. This meta-analysis reviewed all studies published until November 2014 that investigated the role of anxiety on hypertension onset, including 8 prospective studies with a follow-up period up to 25 years. The findings showed that anxious individuals had a 55% higher risk of future hypertension onset compared to the non-anxious counterparts.
- 5.Cuffee Y, et al. Psychosocial risk factors for hypertension: An update of the literature. Current Hypertension Reports. 2014;16(10):483. doi: 10.1007/s11906-014-0483-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Spruill TM. Chronic psychosocial stress and hypertension. Current Hypertension Reports. 2010;12(1):10–6. doi: 10.1007/s11906-009-0084-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7 •.Meng L, et al. Depression increases the risk of hypertension incidence: A meta-analysis of prospective cohort studies. Journal of Hypertension. 2012;30(5):842–51. doi: 10.1097/HJH.0b013e32835080b7. This meta-analysis reviewed all prospective cohort studies published until September 2011 that examined depression symptoms or disorder as a risk factor for hypertension onset. The results, obtained from 9 included studies with a follow-up period up to 15 years, revealed that depressed vs. non-depressed individuals had a 42% greater risk of developing hypertension over time.
- 8.Markovitz JH, Jonas BS, Davidson K. Psychologic factors as precursors to hypertension. Current Hypertension Reports. 2001;3(1):25–32. doi: 10.1007/s11906-001-0074-y. [DOI] [PubMed] [Google Scholar]
- 9.Bergmann N, Gyntelberg F, Faber J. The appraisal of chronic stress and the development of the metabolic syndrome: A systematic review of prospective cohort studies. Endocrine Connections. 2014;3(2):R55–80. doi: 10.1530/EC-14-0031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Byrd JB, Brook RD. Anxiety in the “age of hypertension”. Current Hypertension Reports. 2014;16(10):486. doi: 10.1007/s11906-014-0486-0. [DOI] [PubMed] [Google Scholar]
- 11.Alexander F. Emotional factors in essential hypertension: Presentation of a tentative hypothesis. Psychosomatic Medicine. 1939;1(1):173–179. [Google Scholar]
- 12.Moser M. Historical perspectives on the management of hypertension. Journal of Clinical Hypertension. 2006;8(8 Suppl 2):15–20. doi: 10.1111/j.1524-6175.2006.05836.x. quiz 39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Scotch NA, Geiger HJ. The epidemiology of essential hypertension: A review with special attention to psychologic and sociocultural factors. Journal of Chronic Diseases. 1963;16:1183–213. [PubMed] [Google Scholar]
- 14.Sommers-Flanagan J, Greenberg RP. Psychosocial variables and hypertension: A new look at an old controversy. Journal of Nervous and Mental Disease. 1989;177(1):15–24. doi: 10.1097/00005053-198901000-00003. [DOI] [PubMed] [Google Scholar]
- 15.Richman LS, et al. Positive emotion and health: Going beyond the negative. Health Psychology. 2005;24(4):422–9. doi: 10.1037/0278-6133.24.4.422. [DOI] [PubMed] [Google Scholar]
- 16.Richman LS, et al. The relationship between mental vitality and cardiovascular health. Psychology & Health. 2009;24(8):919–32. doi: 10.1080/08870440802108926. [DOI] [PubMed] [Google Scholar]
- 17.Steptoe A, Wardle J. Positive affect and biological function in everyday life. Neurobiology of Aging. 2005;26(Suppl 1):108–12. doi: 10.1016/j.neurobiolaging.2005.08.016. [DOI] [PubMed] [Google Scholar]
- 18.Pickering TG. Does psychological stress contribute to the development of hypertension and coronary heart disease? European Journal of Clinical Pharmacology. 1990;39(Suppl 1):S1–7. [PubMed] [Google Scholar]
- 19.Beilin LJ. Stress, coping, lifestyle and hypertension: A paradigm for research, prevention and non-pharmacological management of hypertension. Clinical and Experimental Hypertension. 1997;19(5-6):739–52. doi: 10.3109/10641969709083183. [DOI] [PubMed] [Google Scholar]
- 20.Lazarus RS. Theory-based stress measurement. Psychological Inquiry. 1990;1:3–13. [Google Scholar]
- 21.Kubzansky LD, Winning A, Kawachi I. Affective states and health. In: Berkman LF, Kawachi I, Glymour MM, editors. Social epidemiology. Oxford University Press; New York, NY: 2014. pp. 320–364. [Google Scholar]
- 22.Gross JJ. Part I: Foundations. Emotion regulation: Conceptual and empirical foundations. In: Gross JJ, editor. Handbook of emotion regulation. The Guilford Press; New York, NY: 2014. pp. 3–20. [Google Scholar]
- 23.Lazarus RS. From psychological stress to the emotions: A history of changing outlooks. Annual Review of Psychology. 1993;44:1–21. doi: 10.1146/annurev.ps.44.020193.000245. [DOI] [PubMed] [Google Scholar]
- 24.DeSteno D, Gross JJ, Kubzansky L. Affective science and health: The importance of emotion and emotion regulation. Health Psychology. 2013;32(5):474–86. doi: 10.1037/a0030259. [DOI] [PubMed] [Google Scholar]
- 25.Lazarus RS. The stable and unstable in emotions. In: Ekman P, Davidson RJ, editors. The nature of emotions. Oxford University Press; New York, NY: 1994. pp. 70–85. [Google Scholar]
- 26.Mittleman MA, Mostofsky E. Physical, psychological and chemical triggers of acute cardiovascular events: Preventive strategies. Circulation. 2011;124(3):346–54. doi: 10.1161/CIRCULATIONAHA.110.968776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cohen BE, Edmondson D, Kronish IM. State of the Art Review: Depression, Stress, Anxiety, and Cardiovascular Disease. American Journal of Hypertension. 2015 doi: 10.1093/ajh/hpv047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Davies SJ, Allgulander C. Anxiety and cardiovascular disease. Modern Trends in Pharmacopsychiatry. 2013;29:85–97. doi: 10.1159/000351945. [DOI] [PubMed] [Google Scholar]
- 29.Thurston RC, Rewak M, Kubzansky LD. An anxious heart: Anxiety and the onset of cardiovascular diseases. Progress in Cardiovascular Diseases. 2013;55(6):524–37. doi: 10.1016/j.pcad.2013.03.007. [DOI] [PubMed] [Google Scholar]
- 30.Hamer M, Steptoe A. Cortisol responses to mental stress and incident hypertension in healthy men and women. Journal of Clinical Endocrinology and Metabolism. 2012;97(1):E29–34. doi: 10.1210/jc.2011-2132. [DOI] [PubMed] [Google Scholar]
- 31.Appleton AA, Kubzansky LD. Part IX: Health Implications. Emotion regulation and cardiovascular disease risk. In: Gross JJ, editor. Handbook of emotion regulation. The Guilford Press; New York, NY: 2014. pp. 596–612. [Google Scholar]
- 32.Boehm JK, Kubzansky LD. The heart's content: The association between positive psychological well-being and cardiovascular health. Psychological Bulletin. 2012;138(4):655–91. doi: 10.1037/a0027448. [DOI] [PubMed] [Google Scholar]
- 33.Leventhal AM, Zvolensky MJ. Anxiety, depression, and cigarette smoking: A transdiagnostic vulnerability framework to understanding emotion-smoking comorbidity. Psychol Bull. 2015;141(1):176–212. doi: 10.1037/bul0000003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Boden JM, Fergusson DM. Alcohol and depression. Addiction. 2011;106(5):906–14. doi: 10.1111/j.1360-0443.2010.03351.x. [DOI] [PubMed] [Google Scholar]
- 35.Kessler RC, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 36.Abouzeid M, et al. Posttraumatic stress disorder and hypertension in Australian veterans of the 1991 Gulf War. Journal of Psychosomatic Research. 2012;72(1):33–8. doi: 10.1016/j.jpsychores.2011.08.002. [DOI] [PubMed] [Google Scholar]
- 37 •.Stein DJ, et al. Associations between mental disorders and subsequent onset of hypertension. General Hospital Psychiatry. 2014;36(2):142–9. doi: 10.1016/j.genhosppsych.2013.11.002. This retrospective longitudinal study aggregated data from 19 countries and 52,095 adults to investigate the relationship of both anxiety and depressive disorders with incident hypertension over more than 10 years. The findings showed that major depressive disorder/dysthymia, panic disorder, social and specific phobias were significantly associated with 10-30% greater odds of hypertension, independent of any other psychiatric comorbidities. The relationship of bipolar disorder, generalized anxiety disorder, agoraphobia without panic, post-traumatic stress disorder and obsessive-compulsive disorder with the odds of hypertension was non-significant in the fully-adjusted models.
- 38.Bacon SL, et al. The impact of mood and anxiety disorders on incident hypertension at one year. International Journal of Hypertension. 2014:953094. doi: 10.1155/2014/953094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ginty AT, et al. Depression and anxiety are associated with a diagnosis of hypertension 5 years later in a cohort of late middle-aged men and women. Journal of Human Hypertension. 2013;27(3):187–90. doi: 10.1038/jhh.2012.18. [DOI] [PubMed] [Google Scholar]
- 40.Terracciano A, et al. Are personality traits associated with white-coat and masked hypertension? Journal of Hypertension. 2014;32(10):1987–92. doi: 10.1097/HJH.0000000000000289. discussion 1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tikhonoff V, et al. Symptoms of anxiety and depression across adulthood and blood pressure in late middle age: The 1946 British birth cohort. Journal of Hypertension. 2014;32(8):1590–8. doi: 10.1097/HJH.0000000000000244. discussion 1599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th, text rev. ed Washington, DC: 2000. [Google Scholar]
- 43.Kessler RC, et al. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62(6):617–27. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shah MT, Zonderman AB, Waldstein SR. Sex and age differences in the relation of depressive symptoms with blood pressure. American Journal of Hypertension. 2013;26(12):1413–20. doi: 10.1093/ajh/hpt135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Martin R, Watson D, Wan CK. A three-factor model of trait anger: Dimensions of affect, behavior, and cognition. Journal of Personality. 2000;68(5):869–97. doi: 10.1111/1467-6494.00119. [DOI] [PubMed] [Google Scholar]
- 46.Suls J. Anger and the heart: Perspectives on cardiac risk, mechanisms and interventions. Progress in Cardiovascular Diseases. 2013;55(6):538–47. doi: 10.1016/j.pcad.2013.03.002. [DOI] [PubMed] [Google Scholar]
- 47.Kop WJ. Chronic and acute psychological risk factors for clinical manifestations of coronary artery disease. Psychosomatic Medicine. 1999;61(4):476–87. doi: 10.1097/00006842-199907000-00012. [DOI] [PubMed] [Google Scholar]
- 48.Schum JL, et al. Trait anger, anger expression, and ambulatory blood pressure: A meta-analytic review. Journal of Behavioral Medicine. 2003;26(5):395–415. doi: 10.1023/a:1025767900757. [DOI] [PubMed] [Google Scholar]
- 49.Hashani V, Roshi E, Burazeri G. Correlates of hypertension among adult men and women in kosovo. Materia Socio-medica. 2014;26(3):213–5. doi: 10.5455/msm.2014.26.213-215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.May RW, et al. Effect of anger and trait forgiveness on cardiovascular risk in young adult females. American Journal of Cardiology. 2014;114(1):47–52. doi: 10.1016/j.amjcard.2014.04.007. [DOI] [PubMed] [Google Scholar]
- 51.Ryff CD, et al. Psychological well-being and ill-being: Do they have distinct or mirrored biological correlates? Psychotherapy and Psychosomatics. 2006;75(2):85–95. doi: 10.1159/000090892. [DOI] [PubMed] [Google Scholar]
- 52.Steptoe A, Deaton A, Stone AA. Subjective wellbeing, health, and ageing. Lancet. 2015;385(9968):640–8. doi: 10.1016/S0140-6736(13)61489-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hu T, et al. Relation between emotion regulation and mental health: A meta-analysis review. Psychological Reports. 2014;114(2):341–62. doi: 10.2466/03.20.PR0.114k22w4. [DOI] [PubMed] [Google Scholar]
- 54 •.Trudel-Fitzgerald C, et al. Taking the tension out of hypertension: a prospective study of psychological well being and hypertension. Journal of Hypertension. 2014;32(6):1222–8. doi: 10.1097/HJH.0000000000000175. This prospective study examined the role of positive psychological well-being constructs on future hypertension onset among 6,384 adults who were followed for more than 10 years. Results showed that high emotional vitality was associated with a 9-11% lower risk of incident hypertension, whereas no relation was evident with optimism.
- 55.Tully PJ, Cosh SM, Baune BT. A review of the affects of worry and generalized anxiety disorder upon cardiovascular health and coronary heart disease. Psychology, Health & Medicine. 2013;18(6):627–44. doi: 10.1080/13548506.2012.749355. [DOI] [PubMed] [Google Scholar]
- 56.Nabi H, et al. Trajectories of depressive episodes and hypertension over 24 years: The Whitehall II prospective cohort study. Hypertension. 2011;57(4):710–6. doi: 10.1161/HYPERTENSIONAHA.110.164061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Davies SJ, et al. A U-shaped relationship between systolic blood pressure and panic symptoms: the HUNT study. Psychological Medicine. 2012;42(9):1969–76. doi: 10.1017/S0033291711003047. [DOI] [PubMed] [Google Scholar]
- 58.Bégaud B. Dictionary of pharmacoepidemiology. John Wiley & Sons Ltd; West Sussex, UK: 2000. [Google Scholar]
- 59.John OP, Eng J. Part VI: Personality processes and individual differences. Three approaches to individual differences in affect regulation: Conceptualizations, measures and findings. In: Gross JJ, editor. Handbook of emotion regulation. The Guilford Press; New York, NY: 2014. pp. 321–345. [Google Scholar]
- 60.Zawadzki MJ. Rumination is independently associated with poor psychological health: Comparing emotion regulation strategies. Psychology & Health. 2015;30(10):1146–63. doi: 10.1080/08870446.2015.1026904. [DOI] [PubMed] [Google Scholar]
- 61.Pavlov SV, et al. The temporal dynamics of cognitive reappraisal: Cardiovascular consequences of downregulation of negative emotion and upregulation of positive emotion. Psychophysiology. 2014;51(2):178–86. doi: 10.1111/psyp.12159. [DOI] [PubMed] [Google Scholar]
- 62.Duan S, et al. Cognitive emotion regulation questionnaire in hypertensive patients. Journal of Central South University. 2011;36(6):532–8. doi: 10.3969/j.issn.1672-7347.2011.06.010. [DOI] [PubMed] [Google Scholar]
- 63.Zhou T, Bishop GD. Culture moderates the cardiovascular consequences of anger regulation strategy. International Journal of Psychophysiology. 2012;86(3):291–8. doi: 10.1016/j.ijpsycho.2012.10.010. [DOI] [PubMed] [Google Scholar]
- 64.Luong G, Charles ST. Age differences in affective and cardiovascular responses to a negative social interaction: The role of goals, appraisals, and emotion regulation. Developmental Psychology. 2014;50(7):1919–30. doi: 10.1037/a0036621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Dan-Glauser ES, Gross JJ. The temporal dynamics of two response-focused forms of emotion regulation: Experiential, expressive, and autonomic consequences. Psychophysiology. 2015;48(9):1309–22. doi: 10.1111/j.1469-8986.2011.01191.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66 •.Gerin W, et al. Rumination as a mediator of chronic stress effects on hypertension: A causal model. International Journal of Hypertension. 2012;2012:453–465. doi: 10.1155/2012/453465. This review proposes rumination as a novel potential pathway by which stress can impact blood pressure and, in turn, incident hypertension. It also discusses the role of stress duration and neurophysiological correlates in this context.
- 67.Conen D, et al. Age-specific differences between conventional and ambulatory daytime blood pressure values. Hypertension. 2014;64(5):1073–9. doi: 10.1161/HYPERTENSIONAHA.114.03957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Riley M, Bluhm B. High blood pressure in children and adolescents. American Family Physician. 2012;85(7):693–700. [PubMed] [Google Scholar]
- 69.Davidson K, et al. Do depression symptoms predict early hypertension incidence in young adults in the CARDIA study? Coronary Artery Risk Development in Young Adults. Archives of Internal Medicine. 2000;160(10):1495–500. doi: 10.1001/archinte.160.10.1495. [DOI] [PubMed] [Google Scholar]
- 70.Kitayama S, et al. Expression of anger and ill health in two cultures: An examination of inflammation and cardiovascular risk. Psychol Science. 2015;26(2):211–20. doi: 10.1177/0956797614561268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Jackson B, et al. Does harboring hostility hurt? Associations between hostility and pulmonary function in the Coronary Artery Risk Development in (Young) Adults (CARDIA) study. Health Psychology. 2007;26(3):333–40. doi: 10.1037/0278-6133.26.3.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Low CA, Thurston RC, Matthews KA. Psychosocial factors in the development of heart disease in women: Current research and future directions. Psychosomatic Medicine. 2010;72(9):842–54. doi: 10.1097/PSY.0b013e3181f6934f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hernan MA, Brumback B, Robins JM. Marginal structural models to estimate the causal effect of zidovudine on the survival of HIV-positive men. Epidemiology. 2000;11(5):561–70. doi: 10.1097/00001648-200009000-00012. [DOI] [PubMed] [Google Scholar]
- 74.Stewart JC, et al. A prospective evaluation of the directionality of the depression-inflammation relationship. Brain, Behavior, and Immunity. 2009;23(7):936–44. doi: 10.1016/j.bbi.2009.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Robins JM, Hernan MA, Brumback B. Marginal structural models and causal inference in epidemiology. Epidemiology. 2000;11(5):550–60. doi: 10.1097/00001648-200009000-00011. [DOI] [PubMed] [Google Scholar]
- 76.Beck AT, Haigh EA. Advances in cognitive theory and therapy: The generic cognitive model. Annual Review of Clinical Psychology. 2014;10:1–24. doi: 10.1146/annurev-clinpsy-032813-153734. [DOI] [PubMed] [Google Scholar]
- 77.Wolkin JR. Cultivating multiple aspects of attention through mindfulness meditation accounts for psychological well-being through decreased rumination. Psychology Research and Behavior Management. 2015;8:171–80. doi: 10.2147/PRBM.S31458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bai Z, et al. Investigating the effect of transcendental meditation on blood pressure: A systematic review and meta-analysis. Journal of Human Hypertension. 2015 doi: 10.1038/jhh.2015.6. [DOI] [PubMed] [Google Scholar]
- 79.Chiesa A, Serretti A. A systematic review of neurobiological and clinical features of mindfulness meditations. Psychological Medicine. 2010;40(8):1239–52. doi: 10.1017/S0033291709991747. [DOI] [PubMed] [Google Scholar]
- 80.Goldstein CM, et al. Current perspectives on the use of meditation to reduce blood pressure. International Journal of Hypertension. 2012;2012:578397. doi: 10.1155/2012/578397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hartley L, et al. Transcendental meditation for the primary prevention of cardiovascular disease. Cochrane Database of Systematic Reviews. 2014;12:CD010359. doi: 10.1002/14651858.CD010359.pub2. [DOI] [PubMed] [Google Scholar]
- 82.Hagins M, et al. Effectiveness of yoga for hypertension: Systematic review and meta-analysis. Evidence-Based Complementary and Alternative Medicine. 2013;2013:649836. doi: 10.1155/2013/649836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Tyagi A, Cohen M. Yoga and hypertension: A systematic review. Alternative Therapies in Health and Medicine. 2014;20(2):32–59. [PubMed] [Google Scholar]
- 84.Brook RD, et al. Beyond medications and diet: Alternative approaches to lowering blood pressure. A scientific statement from the American Heart Association. Hypertension. 2013;61(6):1360–83. doi: 10.1161/HYP.0b013e318293645f. [DOI] [PubMed] [Google Scholar]