Abstract
Background: The outbreaks of foodborne diseases is a major health problem and occur daily in all countries, from the most to the least developed. This study is the first report of foodborne outbreaks in Iran that carried out from 2006 to 2011.
Methods: A retrospective, longitudinal study carried out using foodborne disease national surveillance system data from 2006-2011, which have been reported by all provincial health centers to the Center for Communicable Disease Control. Collected data were analyzed using SPSS version 18 software.
Results: Since 2006 to 2011, a total of 2250 outbreaks were reported in Iran. Analyzed data showed that the outbreak rate has increased from 0.07/100000 in 2006 to 1.38/100000 population in 2011. Khuzestan, Kermanshah and Qazvin were three provinces that reported more outbreaks than nationally expected outbreak incidence rate during 2011. Analysis of epidemiological characteristics of foodborne outbreaks during 2011 indicated that the numbers of outbreaks were highest in warm months, e.g. 17.8% of total outbreaks was just reported in August. Females and age group of 16-30 years old were more affected and 55% of cases occurred in rural area. Among 684 human samples which have been tested, E. coli, Shigella, Hepatitis A and Vibrio cholera were predominant etiologic agents respectively.
Conclusion: Increasing the detection rate of foodborne outbreaks imply the expansion of surveillance activities and improved primary health care in Iran in recent years. Foodborne disease surveillance system is a new program in Iran that should be continued and strengthened including diagnostic laboratory capacities.
Keywords: Foodborne Disease Outbreak, Surveillance, Iran
Introduction
The outbreaks of foodborne diseases occur daily in all countries, from the most to the least developed. The true dimension of the problem is unknown. Foodborne agents cause an estimated 48 million cases annually in the United States, including 9.4 million illnesses from known pathogens (1,2). A mean of ≥ 1000 foodborne disease outbreaks (FBDOs) causing ≥ 20,000 illnesses are reported to the Centers for Disease Control and Prevention (CDC) annually (3). Approximately 179 million cases of acute gastroenteritis (AGE) occur in the United States each year, and outbreaks of AGE are a substantial public health problem (3).There are limited information regarding foodborne outbreaks in Iran. Aziz A, et al have reported parasitic contamination of vegetables (4),Soltan-dallal studied on Yersinia enterocolitica (5),and Jalali studied on Listeria contamination in food products (6).Another surveys were also carried out on Campylobater infection by Ansari-Lari (7), and Vibrio spp by Hedayat Hosseini (8). Bacterial pathogens in Iranian fish investigated by Afshin Akhondzadeh Basti (9). Foods are mostly prepared at home, however part of daily diet includes industrially processed ones in Iran. According to latest information, fast foods consumption is growing. The bread, rice and vegetables are dominant in food chain. About 95.6% of urban households and 87.2% of rural households have free access to sanitary piped water in Iran.
Each of the above-mentioned studies included a small size population and did not show country level situation of foodborne disease in Iran. Since 2006 a national guideline for foodborne diseases was developed by the Center for Communicable Diseases Control and launched in the same year (10).The guideline has been approved by national technical committee and it's first step has been designed to determine five common foodborne diseases caused by Salmonella, Shigella, E.coli, Staphylococcal toxin and Botulism (10). This study is the first report of foodborne outbreaks in Iran that carried out with the aid of data collected in the mentioned national foodborne surveillance system.
Methods
Data Source
A retrospective, longitudinal study was carried out with the aid of data collected in that surveillance system during consecutive 6 years from 2006-2011. According to the foodborne outbreak definition all outbreaks have been reported via phone by all provincial health centers to the department of foodborne and waterborne disease of Center for Communicable Disease Control. A foodborne disease outbreak is defined as: "an occurrence of two or more cases with similar illness resulting from ingestion of a common food or beverage". Outbreak investigation were done for most of them. Data collected for each outbreak include, e.g. dates, location, number of patients, age, sex, etiologic agents, symptoms, setting of food preparation, number of cases admitted to hospital, and whether the illness resulted in death. In some cases human samples e.g. stool, vomits, serum and suspected food samples were collected for laboratory analysis and confirmation. Human and food samples were tested in local laboratories, however 5 to 10% of them were sent to national laboratory for additional microbiological tests and confirmation.
Data Analysis
Frequency of outbreaks, outbreak rate, and frequencies of general or household outbreaks, hospitalization and death were calculated. Seasonal trend and variation in reporting by provinces were also assessed. Outbreaks with more than 5 patients have been considered as general and less than 5 patients as households. Expected incidence rate of foodborne outbreaks for Iran has been set at 5 outbreaks per 100000 population by national technical committee in Center for Communicable Disease Control. Collected data were analyzed using SPSS version 18 software.
Results
From 2006 to 2011, a total of 2250 outbreaks were reported in Iran. Analyzed data showed that the outbreak rate has increased from 0.07/100000 in 2006 to 1.38/100000 population in 2011 (Table 1). Khuzestan, Kermanshah and Qazvin were three provinces with high national expected level of outbreak incidence rates during 2011. (Graph 1) The number of provinces that were reporting outbreaks to Center for Communicable Disease Control grew gradually, therefore in 2011 the total 31 provinces of country have joined this surveillance system (Graph 1).
Table 1 . Reported Foodborne Disease Outbreaks in Iran from 2006 - 2011 .
|
Total Population |
No. of Foodborne Outbreaks | Outbreak rate /100000 | No. of General outbreaks >5 | No. of household Outbreaks <5 |
No. of Cases |
No. of Admitted to hospitals |
No. of Death |
|
| 2006 | 71532063 | 54 | 0.07 | 25 | 29 | 4618 | 570 | 11 |
| 2007 | 72583587 | 111 | 0.16 | 67 | 44 | 6762 | 1525 | 12 |
| 2008 | 73650566 | 240 | 0.3 | 173 | 68 | 6117 | 647 | 13 |
| 2009 | 74293123 | 267 | 0.36 | 143 | 126 | 6083 | 448 | 17 |
| 2010 | 74626387 | 540 | 0.73 | 281 | 265 | 12588 | 1688 | 14 |
| 2011 | 75161594 | 1038 | 1.38 | 393 | 645 | 10283 | 1385 | 26 |
Graph 1 .
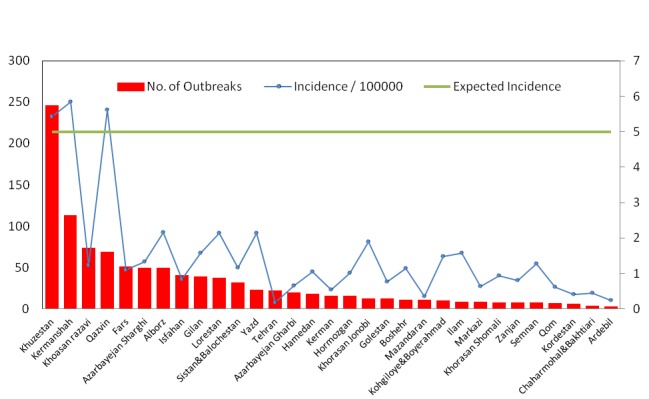
Incidence of foodborne disease outbreaks by provinces in Iran, 2011 (Total: 1038)
Analysis of epidemiological characteristics of foodborne outbreaks during 2011 indicated that the number of outbreaks were highest in warm months, e.g. 17.8% of total outbreaks was just reported in August. Females and age group of 16-30 years old were more affected and 55% of cases occurred in rural area. Among 684 human samples which have been tested, E. coli, Shigella, Hepatitis A and Vibrio cholera were predominant etiologic agents respectively. (Table 2) The total 113 of food samples testing indicate that E.coli, Staphylococcal toxin, Shigella and Salmonella were common contaminant respectively.
Table 2 . Results of analysis of Reported Foodborne Disease Outbreaks in Iran, 2011 .
| No. | % | |
|
Frequency of Foodborne Outbreaks by Months (1038) | ||
| January | 37 | 3.8 |
| February | 50 | 4.8 |
| March | 42 | 4 |
| April | 53 | 5.2 |
| May | 76 | 7.3 |
| June | 99 | 9.5 |
| July | 134 | 13 |
| August | 184 | 17.8 |
| September | 141 | 13.6 |
| October | 86 | 8.3 |
| November | 77 | 7.5 |
| December | 54 | 5.3 |
| Frequency of Foodborne Disease cases by Age Groups (10283) | ||
| 0-5 years old | 2468 | 24 |
| 6-15 years old | 2262 | 22 |
| 16-30 years old | 3394 | 33 |
| 31-45 years old | 1440 | 14 |
| ≥46 years old | 720 | 7 |
| Frequency of Foodborne Disease cases by Gender (10283) | ||
| Male | 4833 | 47 |
| Female | 5450 | 53 |
| Frequency of Foodborne Outbreaks by Residency (1038) | ||
| Rural Area | 571 | 55 |
| Urban Area | 467 | 45 |
| Frequency of Investigated cases by Etiology, Total Samples (684) | ||
| E.coli (Non-pathogen) | 198 | 29 |
| Shigella spp | 94 | 13.8 |
| Hepatitis A | 92 | 13.5 |
| Vibrio cholera | 72 | 10.5 |
| Entamoeba histolytica | 47 | 6.9 |
| Salmonella spp | 35 | 5.1 |
| Staphylococcal Toxin | 32 | 4.6 |
| Giardia intestinalis | 27 | 3.9 |
| Botulism | 19 | 2.8 |
| Chemicals | 17 | 2.5 |
| Yersinia enterocolitica | 3 | 0.4 |
| Rotavirus | 2 | 0.3 |
| Others | 46 | 6.7 |
Discussion
Worldwide surveillance for foodborne outbreaks does not have a long history; actually the oldest reports were done since three decade ago. In Iran, foodborne outbreaks surveillance system is a new program and we believe that within the Eastern Mediterranean region, Iran is one of the first countries which has developed such a surveillance system. Foodborne diseases are among global and regional health problems which are growing worldwide. For example, diarrheal disease outbreak happened in European Union countries especially Germany in 2011 with Vero-cytotoxin Producing Escherichia coli O104:H4 with the origin of raw fruits, vegetables and beans sprouts was one of the most important foodborne outbreaks (11).During 2008, 1034 foodborne disease outbreaks were reported in the United States. Among the 479 investigated outbreaks with a laboratory confirmed single etiologic agent, Norovirus was the first and Salmonella was the second most common etiologic agents (12,13). According to the European Food Safety Authority (EFSA) network report in 2006, Salmonella was the most common cause of foodborne outbreaks in European countries (14). Aplenty of reports from different countries shows human Salmonellosis remains as an important agent for foodborne outbreaks, particularly among children (15-18). In Iran during 2011 the most common etiologic agent in human and food collected samples was E.coli; meanwhile in the United States during 1998-2007 the E.coli was the second etiologic agent in over 100 multistate foodborne disease outbreak (18).
Globally, due to limitations of laboratory capacities in diagnosis of etiology, most of foodborne outbreak agents remain unknown. Sometimes countries within one WHO region need to share their experience and capacities. For example, sharing information of food investigations was facilitated by the European Epidemic Intelligence Information System between French and Belgium listeriosis surveillance systems (19). Botulism in Poland is still an important epidemiological problem due to consumption of homemade canned foods (20). In our study also Botulism was identified in 2.8% of outbreaks as an etiologic agent (Table 2). Hepatitis A was the third etiologic agent for foodborne outbreaks in Iran (Table 2), which has been identified rarely as an etiologic agent in other countries. Although Vibrio cholera is mostly known as a waterborne agent, due to endemicity of the disease in Iran, in 10.5% (72 cases) of human samples that were investigated during foodborne outbreaks (Tbale 2), the infection source was identified as contaminated vegetable. National Cholera surveillance system in Iran register all cases in epidemic or sporadic form. Among 1187 cholera cases reported in 2011, 72 cases occurred in the epidemic form while remainders were sporadic. Also two consecutive outbreaks of foodborne cholera were associated with consumption of chicken rice in northwestern Thailand (21).
In recent years, some of factors like changing eating habits, global trade of foodstuff, population growth and movements, climate change, increased awareness and better diagnostic tools are among some of the main drivers affecting the emergence or re-emergence of many foodborne parasitic diseases (22,23). Thus, foodborne parasitic disease will be a challenging issue in the future. Diagnosis of chemicals and toxins as etiologic agents of foodborne outbreaks also require equipped laboratories. On the other hand, foodborne disease outbreak surveillance systems are complex, and strengthening them needs a multi-faceted approach to identify and overcome barriers (24).One of the benefits of this surveillance system is increasing incidence rate of Foodborne Disease outbreaks, which does not necessarily imply the worsening of health status in Iran, indicates strengthening of the surveillance system. One of the important limitations of this study was shortage in laboratory diagnosis of some etiologic agents such as listeria and campylobacter.
Increasing the detection rate of foodborne outbreaks imply the expansion of surveillance activities and improved primary health care in Iran in recent years. Foodborne disease surveillance system is a new program in Iran that should be continued and strengthened even more, such as an increase in diagnostic laboratory capacities.
Acknowledgment: The authors would like to acknowledge the kind collaboration of all the staff at provincial and district health centers and lab technicians in different provinces for data collection. Also we would like to appreciate Dr. Payman Hemmati for his collaboration in this article.
Conflict of interest
No conflict of interest to declare
Cite this article as: Masoumi Asl H, Gouya MM, Soltan-dallal MM, Aghili N. Surveillance for foodborne disease outbreaks in Iran, 2006-2011. Med J Islam Repub Iran 2015 (3 November). Vol. 29:285.
References
- 1.Scallan E, Hoekstra RM, Angulo FJ, Tauxe RV, Widdowson M-A, Roy SL. et al. Foodborne illness acquired in the United States-major pathogens. Emerg Infect Dis. 2011;17:1–5. doi: 10.3201/eid1701.P11101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Scallan E, Griffin PM, Angulo FJ, Tauxe RV, Hoekstra RM. Foodborne illness acquired in the United States-unspecified agents. Emerg Infect Dis. 2011;17(1):16–22. doi: 10.3201/eid1701.P21101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Murphree R, Garman K, Phan Q, Everstine K, Gould LH, Jones TF. Characteristics of foodborne disease outbreak investigations conducted by Foodborne Diseases Active Surveillance Network (FoodNet) sites, 2003–2008. Clin Infect Dis. 2012;54(suppl 5):S498–S503. doi: 10.1093/cid/cis232. [DOI] [PubMed] [Google Scholar]
- 4.Fallah AA, Pirali-Kheirabadi K, Shirvani F, Saei-Dehkordi SS. Prevalence of parasitic contamination in vegetables used for raw consumption in Shahrekord, Iran: influence of season and washing procedure. Food control. 2012;25(2):617–20. [Google Scholar]
- 5.Soltan-Dallal MM, Tabarraie A, MoezArdalan K. Comparison of four methods for isolation of Yersinia enterocolitica from raw and pasteurized milk from northern Iran. International journal of food microbiology. 2004;94(1):87–91. doi: 10.1016/j.ijfoodmicro.2003.10.017. [DOI] [PubMed] [Google Scholar]
- 6.Jalali M, Abedi D. Prevalence of Listeria species in food products in Isfahan, Iran. International journal of food microbiology. 2008;122(3):336–40. doi: 10.1016/j.ijfoodmicro.2007.11.082. [DOI] [PubMed] [Google Scholar]
- 7.Ansari-Lari M, Hosseinzadeh S, Shekarforoush SS, Abdollahi M, Berizi E. Prevalence and risk factors associated with campylobacter infections in broiler flocks in Shiraz, southern Iran. International journal of food microbiology. 2011;144(3):475–9. doi: 10.1016/j.ijfoodmicro.2010.11.003. [DOI] [PubMed] [Google Scholar]
- 8.Hosseini H, Cheraghali AM, Yalfani R, Razavilar V. Incidence of Vibrio spp in shrimp caught off the south coast of Iran. Food control. 2004;15(3):187–90. [Google Scholar]
- 9.Basti AA, Misaghi A, Salehi TZ, Kamkar A. Bacterial pathogens in fresh, smoked and salted Iranian fish. Food control. 2006;17(3):183–8. [Google Scholar]
- 10. Masoumi Asl H. National Guideline of foodborne diseases surveillance. Tehran: Ministry of Health and Medical Education Publication of Iran 2006:1-5.
- 11.Frank C, Werber D, Cramer JP, Askar M, Faber M, an der Heiden M. et al. Epidemic profile of Shiga-toxin–producing Escherichia coli O104: H4 outbreak in Germany. N Engl J Med. 2011;365(19):1771–80. doi: 10.1056/NEJMoa1106483. [DOI] [PubMed] [Google Scholar]
- 12.Control CfD, Prevention Prevention. Surveillance for foodborne disease outbreaks--United States, 2008. MMWR. 2011;60(35):1197. [PubMed] [Google Scholar]
- 13.Hall AJ, Eisenbart VG, Etingüe AL, Gould LH, Lopman BA, Parashar UD. Epidemiology of foodborne norovirus outbreaks, United States, 2001–2008. Emerg Infect Dis. 2012;18(10):1566. doi: 10.3201/eid1810.120833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Helwigh B, Korsgaard H. The community summary report on trends and sources of zoonoses, zoonotic agents, antimicrobial resistance and foodborne outbreaks in the European Union in 2006: EFSA; 2007.
- 15.Loharikar A, Vawter S, Warren K, Marshall Deasy I, Moll M, Sandt C. et al. Outbreak of human Salmonella Typhimurium infections linked to contact with baby poultry from a single agricultural feed store chain and mail-order hatchery, 2009. Pediatr Infect Dis J. 2013;32(1):8–12. doi: 10.1097/INF.0b013e3182755e28. [DOI] [PubMed] [Google Scholar]
- 16.Group OW. Monitoring the incidence and causes of diseases potentially transmitted by food in Australia: annual report of the Ozfoodnet Network, 2006. Communicable diseases intelligence quarterly report. 2007;31(4):345. [PubMed] [Google Scholar]
- 17.Baumann-Popczyk A, Sadkowska-Todys M. [Foodborne infections and intoxications in Poland in 2010] Przegl Epidemiol. 2011;66(2):241–8. [PubMed] [Google Scholar]
- 18.Purayidathil FW, Jennifer Ibrahim M. A summary of health outcomes: multistate foodborne disease outbreaks in the US, 1998-2007. J Environ Health. 2012;75(4):8. [PubMed] [Google Scholar]
- 19. Yde M, Naranjo M, Mattheus W, Stragier P, Pochet B, Beulens K, et al. Usefulness of the European Epidemic Intelligence Information System in the management of an outbreak of listeriosis, Belgium, 2011. Euro Surveill 2012; 17(38):pii: 20279. [PubMed]
- 20.Czerwiński M, Czarkowski M, Kondej B. [Botulism in Poland in 2010] Przegl Epidemiol. 2011;66(2):267–71. [PubMed] [Google Scholar]
- 21.Swaddiwudhipong W, Hannarong S, Peanumlom P, Pittayawonganon C, Sitthi W. Two consecutive outbreaks of food-borne cholera associated with consumption of chicken rice in northwestern Thailand. Southeast Asian J Trop Med Public Health. 2012;43(4):927–32. [PubMed] [Google Scholar]
- 22.Broglia A, Kapel C. Changing dietary habits in a changing world: emerging drivers for the transmission of foodborne parasitic zoonoses. Vet Parasitol. 2011;182(1):2–13. doi: 10.1016/j.vetpar.2011.07.011. [DOI] [PubMed] [Google Scholar]
- 23.Stypułkowska-Misiurewicz H, Baumann-Popczyk A. [Dysentery and amoebiasis in Poland in 2010] Przegl Epidemiol. 2011;66(2):235–9. [PubMed] [Google Scholar]
- 24.Jones TF, Rosenberg L, Kubota K, Ingram LA. Variability among states in investigating foodborne disease outbreaks. Foodborne Pathog Dis. 2013;10(1):69–73. doi: 10.1089/fpd.2012.1243. [DOI] [PubMed] [Google Scholar]


