Abstract
Background: Iran has a high C-section rate (40.6% in 2005). The objective of this study was to assess the associations and population-attributable risks (PAR) of risk factors combinations and Csection in the Southwest Iran.
Methods: We performed a population-based cohort study using the reports provided by Shiraz University of Medical Sciences. The cohort included pregnant women within September 2012 and February 2013 (n=4229), with follow-up until delivery. Then, the actual delivery was recorded; i.e., C-section delivery, vaginal delivery, and miscarriage. A multiple logistic regression model was used to estimate the point and the interval probability. The adjusted population attributable risks (aPARs) were calculated through adjusted odds ratio from the final multiple logistic regression models for each variable.
Results: Of 4,217 deliveries, 2,624 ones were C-section (62.2%). The rate of C-section was significantly higher in healthcare departments of private clinics compared to governmental clinics. The rate increased steadily with the mother’s age, marriage age, family income and education. The multiple logistic regression analysis showed that local healthcare, supplementary insurance, maternal age, age of marriage, place of birth, family income, maternal education, education of husband and occupation were the key contributing factors to choose the mode of delivery. The multiple logistic regression analysis for reproductive factors showed that parity, previous abortion and stillbirth, previous infertility, birth weight (g) and number of live births were selected risk factors for C-section. Among the exposures, family income, location of healthcare and place of birth showed the highest population attributable risks: 43.86%, 19.2% and 18.53%; respectively.
Conclusion: In this survey, a relatively large contribution of non-medical factors was identified against the background of C-section. All of these factors influence the knowledge, attitudes and norms of the society. Thus, the attention of policymakers should be drawn to the factors associated with this mode of delivery.
Keywords: C-section, Risk factor, Public health, Iran
Introduction
Pregnancy is a physiologic phenomenon which ends in delivery, an event which may accompanied by fear and worry about death. Hence, delivery is a critical experience in a woman's life (1,2). In the last century, C-section played a major role in the reduction of maternal as well as fetal mortality. However, the increasing rate of C-section deliveries is a worrying issue in modern obstetrics and one of the main concerns of the society (3). Nowadays, most deliveries are carried out through C-section involving a large number of facilities, hospital beds, and experts. Moreover, the rate of mortality and delivery complications is considerably higher among the mothers who give birth to their children through C-section compared to those undergoing vaginal deliveries (VD). Mortality and disability rates were reported to be respectively 2-3 and 5-10 times higher in C-sections compared to VDs (4). Additionally, the infant mortality rate in C-section is 4 times higher compared to that in VD. Furthermore, the risk of primary pulmonary hypertension was 5 times higher among the infants born through C-section in comparison to those born through the VD (5). Overall, the daily increasing rate of C-section deliveries has concerned the researchers as well as health authorities. So far, the prevalence of C-section deliveries in many countries is considerably higher than the acceptable threshold announced by WHO; i.e., 10-15% of all births (6,7). The rate of C-section in the world has increased from less than 7% in 1970 to more than 25% in 2005. In the U.S., the rate of this surgery has increased annually since 1997 and reached 32.9% in 2009. This measure was higher in South America; that is to say more than 50% of all deliveries were carried out through C-section in private hospitals of Chile, Argentina, Brazil, and Paraguay (8-13).According to the report by Iran’s Ministry of Health and Medical Education (MOHME), the rates of C-section were 35% in 2000, 37% in 2002, and 39.9% in 2004 (2). Based on the latest formal statistics published by the MOHME the rate of C-section was 40.6% in Iran in 2005 (7); and the rate of C-section was 37.8% for normal pregnant population of Tehran (Iran's capital) during three decades (14). Various reasons have been suggested for this increase, including the rising maternal age at first pregnancy, technological advances that have improved the safety of the procedure, changes in women’s preferences, and a growing proportion of women who have previously had a C-section (15,16).
The aim of the present study is to determine the relationship between socioeconomic, demographic, reproductive and health service factors and the likelihood of C-section. Furthermore, in this paper, we present estimates of adjusted population attributable risks (aPARs) for the selected risk factors identified in this study population. The aPAR is defined as the proportion of cases that can be related to a given risk factor (or a set of risk factors) and is useful in assessing its impact at the population level. To our knowledge, this analysis constitutes the first attempt at a comprehensive population attributable risk study of the risk factors for C-sections.
Methods
This study was a prospective cohort study consisting of 4,200 pregnant women. Fars province is located in the southwest of Iran. Its population was 4,596,658 according to the report by the Iranian Census of Population and Housing in 2011 and it is one of the most populous provinces, with 2, 315,914 male and 2,280,744 female people.
The study was carried out at the entire Health System of Fars province in 2012. Sampling took place between September 2012 and February 2013 at the time of routine ultrasound examination at 18 – 22 weeks of gestation in the Shiraz University of Medical Sciences; the samples were selected using simple random sampling performed through a random number excel. Considering the previous studies conducted on the issue and using the cohort studies’ sample size formula (17), a 4200-subject sample was specified for the study.
All samples were interviewed by trained health workers using a structured questionnaire that collected information on characteristics of pregnancies at the beginning of the study. The study participants were followed up until their deliveries. Then, trained health workers contacted the women using the phone numbers they had mentioned in the questionnaires and recorded the actual behavior; i.e., C-section delivery, natural vaginal delivery, and miscarriage.
The data included in this analysis were socioeconomic, demographic and health service factors such as occupation, family income, maternal education, mother’s occupation, education of spouse, maternal age, age of marriage, birthplace (town or village), location of receiving healthcare services, insurance status, supplementary insurance, and reproductive factors including parity, pervious miscarriage and stillbirth, pervious abnormal fetus, number of miscarriages, number of infertility years, type of pregnancy (wanted or unwanted), number of live births, gestational age, and birth weight.
Statistical analysis
The statistical analysis was conducted using STATA version 12 software. Descriptive measures such as the frequency and percentage were used to describe the qualitative data.
The multiple logistic regression models was used to estimate the point and interval probability of a woman having had a C-section on the basis of socioeconomic, demographic, reproductive and health service factors for C-section. Variables significant in crude analysis of known importance were included in the model in order to control their potential confounding effects. All variables were categorically represented, as the effects of the quantitative variables on the outcome were unlikely to be linear or showed no linear trends.
How much of the disease burden in a population could be eliminated if the effects of certain causal factors were eliminated from the population? To address this question, epidemiologists calculate the population attributable fraction. So, we calculated aPARs by using adjusted odds ratio (aORs) from the final multiple logistic regression models for each variable that was significantly associated with an increased risk for C-section. In this calculation, the PAR is:
Pi=Proportion of source population in ith exposure level; ORi=Adjusted odds ratio comparing ith exposure level with unexposed group (i= 0) (18-20).Assume that each risk factor exerted an independent effect. Thus, the sum of the percentages of aPAR can be more than 100%. The statistical significance was set at p< 0.05.
Results
The present study was started by a closed cohort of 4229 pregnant women. Of 4217 deliveries, 2624 were C-sections with a proportion of 62.2%; 37.67% (n=1593) underwent VD and 0.28% (n=12) experienced a miscarriage.
The proportion of women who had a C-section differed according to socioeconomics, demographics, health service and reproductive factors. Women were more likely to have had a C-section if they had received services from private clinics (76.30%), worked at home and also outside the home (79.29%), had higher educations and higher education of their husbands, higher family income and higher maternal age and age of marriage (Table 1).
Table 1 . C-section rates, crude odds ratio, adjusted odds ratio and adjusted population attributable risks (aPAR %) according to socioeconomics, demographics and health service factors in Southwest Iran, 2012 .
| Risk factors | CS rate (%) | n | Crude odds ratio (95%CI) | Adjusted odds ratio (95%CI) | PAR% |
| Get local health care | |||||
| Private clinics | 76.72 | 1435 | 2.72 (2.36- 3.14) | 1.85 (1.56- 2.20) | 19.2 |
| Governmental clinics | 54.74 | 2782 | 1 | 1 | |
| Insurance Status | |||||
| Yes | 62.31 | 3906 | 1.05 (0.83- 1.33) | * | |
| No | 61.09 | 311 | 1 | * | |
| Supplementary insurance | |||||
| Yes | 72.06 | 1199 | 1.84 (1.59- 2.13) | 1.19 (0.99- 1.43) | 5.1 |
| No | 58.32 | 3018 | 1 | 1 | |
| Maternal age | |||||
| >20 | 51.80 | 388 | 1 | 1 | |
| 20-35 | 63.07 | 3550 | 1.58 (1.28- 1.96) | 1.21 (0.94- 1.57) | 14.75 |
| 35+ | 65.95 | 184 | 1.80 (1.31- 2.47) | 1.77 (1.21-2.59) | 3.04 |
| Age of Marriage | |||||
| >20 | 56.76 | 1989 | 1 | 1 | |
| 20-25 | 65.64 | 1301 | 1.45 (1.25-1.68) | 1.10 (0.92- 1.32) | 2.95 |
| 25+ | 69.15 | 927 | 1.70 (1.44-2.01) | 1.29 (1.05- 1.60) | 5.49 |
| Place of Birth | |||||
| Urban | 66.05 | 3190 | 1.91 (1.66- 2.21) | 1.30 (1.10- 1.54) | 18.53 |
| Village | 50.34 | 1027 | 1 | 1 | |
| Family Income | |||||
| 1st quartile | 50.22 | 900 | 1 | 1 | |
| 2nd quartile | 57.95 | 987 | 1.93 (1.60- 2.32) | 1.84 (1.52- 2.25) | 11.90 |
| 3rd quartile | 66.75 | 1173 | 2.10 (1.76- 2.51) | 1.90 (1.57- 2.31) | 16.9 |
| 4th quartile | 75.83 | 509 | 8.19 (6.12- 10.97) | 6.95 (5.12- 9.42) | 15.06 |
| Maternal Education | |||||
| Lower High School | 50.06 | 1652 | 1 | 1 | |
| High School | 65.94 | 1568 | 1.93 (1.67- 2.22) | 1.12 (0.93- 1.35) | 4.22 |
| College education | 76.53 | 997 | 3.25 (2.72- 3.87) | 1.36 (1.03- 1.79) | 7.69 |
| Education of husband | |||||
| Lower High School | 51.60 | 1845 | 1 | 1 | |
| High School | 67.22 | 1458 | 1.92 (1.66-2.21) | 1.36 (1.14- 1.63) | 9.88 |
| College education | 75.71 | 914 | 2.92 (2.45- 3.48) | 1.34 (1.05- 1.72) | 6.69 |
| Occupation | |||||
| Home only | 60.34 | 3797 | 1 | 1 | |
| Also outside the home | 79.29 | 420 | 2.51 (1.96- 3.21) | 1.16 (0.84- 1.60) | 1.75 |
| Ethnicity | |||||
| Turk | 54.32 | 370 | 0.69 (0.55- 0.85) | 0.77 (0.60- 0.99) | -.2.27 |
| Lur | 64.69 | 388 | 1.06 (0.85- 1.32) | * | |
| Kurd | 53.85 | 65 | 0.67 (0.41- 1.11) | * | |
| Persian** | 63.22 | 3331 | 1 | 1 | |
| Arab | 49.21 | 63 | 0.56 (0.34- 0.92) | 0.91 (0.51- 1.60) | -0.11 |
*Since these variables have no significant association with outcome in form crude analysis, so in multivariate analysis were not entered the model.**Majority of the target population
As shown in Table 2, the C-section was more frequent among the women who were at lower parity, had desired pregnancy, previous miscarriage and stillbirth, previous infertility, gestational age (32-36 years), birth weight≤3000g and no live birth.
Table 2 . C-section rates, crude odds ratio, adjusted odds ratio and adjusted population attributable risks (aPAR %) according to reproductive factors in Southwest Iran, 2012 .
| Risk factors | CS rate (%) | n | Crud odds ratio (95%CI) | Adjusted odds ratio (95%CI) | PAR% |
| Parity | |||||
| 1 | 65.84 | 2026 | 1 | 1 | |
| 2 | 60.06 | 1262 | 0.78 (0.67- 0.92) | 0.72 (0.58- 0.88) | -11.2 |
| 3 | 60.24 | 586 | 0.78 (0.65- 0.94) | 0.67 (0.52- 0.87) | -6.6 |
| 4+ | 52.19 | 343 | 0.56 (0.44- 0.71) | 0.42 (0.31- 0.58) | -9.41 |
| Type of pregnancy | |||||
| Wanted | 62.65 | 3518 | 1.11 (0.94- 1.31) | * | |
| Unwanted | 60.09 | 699 | 1 | * | |
| Previous miscarriage stillbirth | |||||
| Yes | 65.49 | 794 | 1.18 (1.01- 1.39) | 1.59 (1.30- 1.94) | 7.35 |
| No | 61.47 | 3423 | 1 | 1 | |
| Number of miscarriage | |||||
| One time | 64.51 | 603 | 1 | * | |
| Two times | 66.90 | 145 | 1.11 (0.75- 1.63) | * | |
| Three and more than three times | 75 | 46 | 1.65 (0.81- 3.33) | * | |
| Previous Abnormalities | |||||
| Yes | 73.68 | 57 | 1.71 (0.94- 3.09) | * | |
| No | 62.07 | 4160 | 1 | * | |
| Previous infertility | |||||
| Yes | 76.71 | 292 | 2.09 (1.58- 2.76) | 2.06 (1.55- 2.73) | 4.39 |
| No | 61.15 | 3925 | 1 | 1 | 1 |
| Gestational age (week) | |||||
| <32 | 69.44 | 108 | 1 | * | |
| 32-36 | 78.05 | 246 | 1.56 (0.94- 2.60) | * | |
| 37-41 | 60.90 | 3790 | 0.68 (0.45- 1.03) | * | |
| >42 | 67.12 | 73 | 0.89 (0.47- 1.69) | * | |
| Birth weight(g) | |||||
| <3000 | 66.42 | 1751 | 1 | 1 | |
| 3000-3499 | 61.16 | 1331 | 0.79 (0.68- 0.92) | 0.74 (0.64- 0.85) | -10.89 |
| 3500-3999 | 56.36 | 928 | 0.65 (0.55- 0.76) | 0.80 (0.68- 0.94) | -4.98 |
| >4000 | 59.90 | 207 | 0.75 (0.56- 1.01) | * | |
| Number of live birth | |||||
| 0 | 66.94 | 1564 | 1 | 1 | |
| 1 | 60.14 | 1533 | 0.74 (0.64- 0.86) | 0.96 (0.79- 1.16) | -1.14 |
| 2 | 57.25 | 821 | 0.66 (0.55- 0.78) | 0.93 (0.75- 1.16) | -1.34 |
| >3 | 61.87 | 299 | 0.8 (0.62- 1.03) | * |
*Since these variables have no significant association with outcome in form crude analysis, so in multiple analysis were not entered the model.
Regarding quantitative variables, i.e., maternal age, gestational age and age at marriage, the probability of C-section for these variables was adjusted for each point (Figs. 1-3).
Fig. 1 .
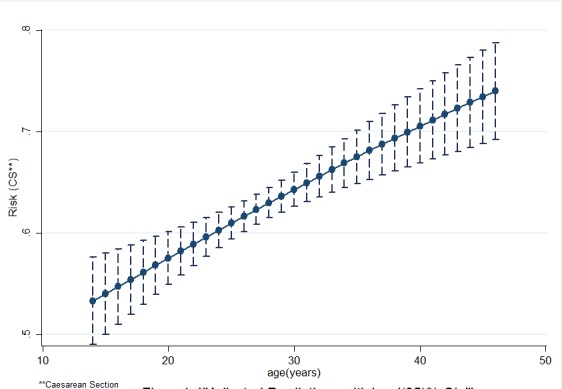
Adjusted predictions with level (95%) CLs
Fig. 2 .
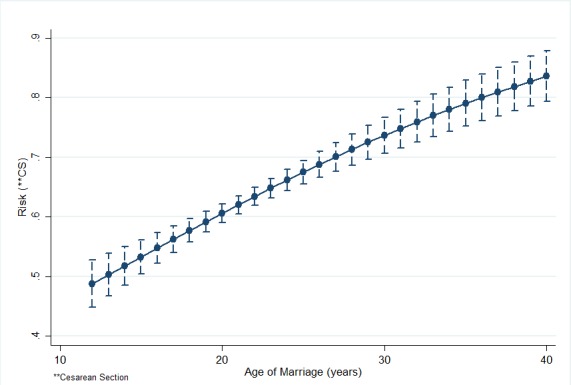
Adjusted predictions with level (95%) CLs
Fig. 3 .
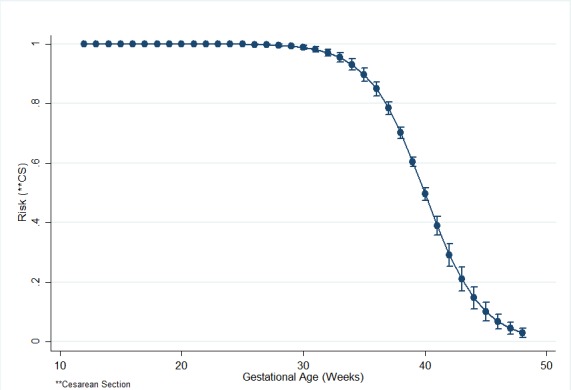
Adjusted predictions with level (95%) CLs
Table 1 indicates the results of univariate (crude) and multiple logistic regression analyses for variables within each exposure group, and the final multiple model showing frequency and sample size, percentages, and crude odds ratio (ORs), aORs, and aPAR% (in order to identify factors likely to be responsible for the C-section in the population).
Among the health care exposures, the proportion of studied C-section who exposed private clinic healthcare was 41.96%. The proportion of C-section in the study population that could be attributed to the clinic healthcare was estimated to be 19.2 % (Table 1). Among the family income exposures, the proportion of studied C-section who reported family income 4th quartile was 17.6%. The proportion of C-section in the study population that could be attributed to the family income 4th quartile was estimated to be 15.06%. A further 11.90% of C-section in the population could be attributed to 2nd quartile and 16.9% of C-section attributed to 3rd quartile. The overall PAR associated with family income was 43.86% (Table 1).
Discussion
C-section is medically indicated when a significant risk of an adverse outcome for the mother or fetus is present. In contrast, non-medically indicated (elective) C-section occurs for reasons other than a risk of adverse outcome (21). The C-section rate in Southwest Iran is excessive. The WHO has pointed out that ‘there is no justification for any region to have a C-section rate higher than 10-15%. (22) . In Iran, although a biological indication for the surgery was emphasized in the medical record, this indication may have been solely a socially permitted justification to perform C-section. Non–clinical factors (private clinics, maternal age ≥ 20, age of marriage≥20, urban birth place, high income family, high education) better explained the variation in C-section rates. Reproductive factors variables were the ones most closely associated with the likelihood of C-section delivery.
The strong association found in the unadjusted analysis between supplementary insurance, maternal age (20-35 years) and occupation and C-section disappeared after the adjustment. It seem to be mediated by other variables that reflect reproductive beliefs, health service and demographics factors. Results of other studies that investigated the relationship between variables and C-section were consistent with that of the present study (23-25). Our study found that women who had 2 or more parities and 1 or 2 alive children showed high probability to perform C-section. This suggests that women’s attitudes, expectations and knowledge have a strong influence on C-section delivery rates. Results of other studies that investigated the relationship between variables and C-section, were consistent with the present study (26-28).
After controlling other factors, the risk of C-section delivery remained low only for infants weighing≥4000g and it was non-significant compared to those who were ≤3000g (baseline). The reason is that this group (≥4000g) is likely to have a lower sample size than the baseline group.
In our study, one of the greatest increases in C-section rate occurred among the women who had previous miscarriages and stillbirths (65.49%), as well as previous infertility (76.71%). All these factors were strongly related to the risk of C-section; as well, the population attributable risks for these variables were 7.35% and 4.39%, respectively. It means that 7.35% and 4.39% of the population risks of C-section would be eliminated if miscarriages and stillbirths, and infertility treatment were to be eliminated from the population. Our study has shown that a reduction of 0.192 C-section per 100-population is expected if women were not referred to private clinics. In other words, the idealized interpretation of our findings is that approximately 19% of C-section among women in our population would be prevented if all women in the population did not refer to private clinics.
Average population attributable fraction estimates 0.0844 and 0.1779 across the three categories of age marriage and age strata, respectively; it means that 8.44% and 17.79% of the population risks of C-section would be eliminated if marriage age and pregnancy age changed in the population. Our study has shown that the population attributable fraction estimates 18.53% for women who were born in urban areas. This suggests that urban women’s attitudes and knowledge have a strong influence on C-section. Hence, 18.53% of C-section among women in our population would be prevented if urban women’s attitudes and knowledge about C-section changed.
For other variables, including maternal education, husband's education, family income and maternal occupational population, the attributable risk was calculated. It was shown that a considerable proportion of C-sections are attributed to these variables. Since most of these variables suggest that factors of attitude, knowledge, norms and behavior control can be influenced, interventions should be done to improve the factors in order to reduce C-section rates in the population
Conclusion
On the other hand, since women’s attitudes, expectations and knowledge seem to have a strong influence on C-section rate, useful investigations in this area could be carried out in order to determine women’s attitudes toward C-section and support the mechanism for their beliefs and how easy it would be to change them.
Acknowledgements
This research was performed by AbdolhalimRajabi, in partial fulfillment of the requirements for certification as an MSc in epidemiology at Shiraz University of Medical Sciences in Shiraz, Iran. We would like to acknowledge the staff of the Health Centers and mothers participated in this study.
Conflict of interest
Authors have no conflict of interest.
Cite this article as: Rajabi A, Maharlouei N, Rezaianzadeh A, Rajaeefard A, Gholami A. Risk factors for C-section delivery and population attributable risk for C-section risk factors in Southwest of Iran: a prospective cohort study. Med J Islam Repub Iran 2015 (16 November). Vol. 29:294.
References
- 1.Villar J. Caesarean delivery rates and pregnancy outcomes: The 2005 WHO global survey on maternal and prenatal health in Latin America. Lancet. 2006;367:1819–29. doi: 10.1016/S0140-6736(06)68704-7. [DOI] [PubMed] [Google Scholar]
- 2.Garmaroudi G, Eftekhar H, Batebi A. Cesarean section and related factors in Tehran, Iran. Payesh. 2002 [Google Scholar]
- 3. Cunningham F, Leveno K, Bloom S, Hauth J, Gilstrap III L. Williams Obstetrics. New York: McGraw-Hill; 2005: 544-638.
- 4.Gholami A, Faraji Z, Lotfabadi P, Foroozanfar Z, Rezaof M, Rajabi A. Factors associated with preference for repeat cesarean in Neyshabur pregnant women. Int J Prev Med. 2014 Sep;5(9):1192–8. [PMC free article] [PubMed] [Google Scholar]
- 5.Richardson DK, Corcoran JD, Escobar GJ, Lee SK. SNAP-II and SNAPPE-II: simplified newborn illness severity and mortality risk scores J. Pediatr. 2001;138(1):92–100. doi: 10.1067/mpd.2001.109608. [DOI] [PubMed] [Google Scholar]
- 6.Ahmad-Nia S, Delavar B, Eini-Zinab H, Kazemipour S, Mehryar A, Naghavi M. Caesarean section in the Islamic Republic of Iran: prevalence and some sociodemographic correlates. East Mediterr Health J. 2009;15(6):1389–98. [PubMed] [Google Scholar]
- 7.Frass K, Al Harazi A. Outcome of vaginal birth after caesarean section in women with one previous section and spontaneous onset of labour. EMHJ. 2011;17(8):646–650. [PubMed] [Google Scholar]
- 8.Alexander JM, Leveno KJ, Hauth JC, Landon MB, Gilbert S, Spong CY. et al. Failed operative vaginal delivery. ISRN Obstet Gynecol. 2009;114(5):1017. doi: 10.1097/AOG.0b013e3181bbf3be. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bragg F, Cromwell DA, Edozien LC, Gurol-Urganci I, Mahmood TA, Templeton A. et al. Variation in rates of caesarean section among English NHS trusts after accounting for maternal and clinical risk: cross sectional study. BMJ. 2010;341:c5065. doi: 10.1136/bmj.c5065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Festin MR, Laopaiboon M, Pattanittum P, Ewens MR, Henderson-Smart DJ, Crowther CA. Caesarean section in four South East Asian countries: reasons for, rates, associated care practices and health outcomes. BMC Pregnancy Childbirth. 2009;9(1):17. doi: 10.1186/1471-2393-9-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kealy MA, Small RE, Liamputtong P. Recovery after caesarean birth: a qualitative study of women's accounts in Victoria, Australia. BMC Pregnancy Childbirth. 2010;10(1):47. doi: 10.1186/1471-2393-10-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ostovar R, Rashidian A, Pourreza A, Rashidi BH, Hantooshzadeh S, Ardebili HE. et al. Developing criteria for cesarean section using the RAND appropriateness method. BMC Pregnancy Childbirth. 2010;10(1):52. doi: 10.1186/1471-2393-10-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Torloni MR, Daher S, Betrán AP, Widmer M, Montilla P, Souza JP. et al. Portrayal of caesarean section in Brazilian women’s magazines: 20 year review. BMJ. 2011;342 doi: 10.1136/bmj.d276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Badakhsh MH, Khamseh ME, Malek M, Shafiee G, Aghili R, Moghimi S. et al. A thirty-year analysis of cesarean section rate in gestational diabetes and normal pregnant population in Tehran, Iran: a concerning trend. J Gynaecol Endocrinol. 2012;28(6):436–9. doi: 10.3109/09513590.2011.633654. [DOI] [PubMed] [Google Scholar]
- 15. Francome C. Caesarean birth in Britain: Middlesex University Press; 1993.
- 16.Porreco RP, Thorp JA. The cesarean birth epidemic: trends, causes, and solutions. Am J Obstet Gynecol. 1996;175(2):369–74. doi: 10.1016/s0002-9378(96)70148-5. [DOI] [PubMed] [Google Scholar]
- 17.Schlesselman JJ. Sample size requirements in cohort and case-control studies of disease. Am J Epidemiol. 1974;99(6):381–4. doi: 10.1093/oxfordjournals.aje.a121625. [DOI] [PubMed] [Google Scholar]
- 18.Bruzzi P, Green Sb, Byar Dp, Brinton La, Schairer C. Estimating the population attributable risk for multiple risk factors using case-control data. Am J Epidemiol. 1985;122(5):904–14. doi: 10.1093/oxfordjournals.aje.a114174. [DOI] [PubMed] [Google Scholar]
- 19.Rockhill B, Newman B, Weinberg C. Use and misuse of population attributable fractions. Am J Public Health Res. 1998;88(1):15–9. doi: 10.2105/ajph.88.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Walter SD. Effects of interaction, confounding and observational error on attributable risk estimation. Am J Epidemiol. 1983;117(5):598–604. doi: 10.1093/oxfordjournals.aje.a113582. [DOI] [PubMed] [Google Scholar]
- 21.Penna L, Arulkumaran S. Cesarean section for non-medical reasons. Obstet Gynecol Int J. 2003;82(3):399–409. doi: 10.1016/s0020-7292(03)00217-0. [DOI] [PubMed] [Google Scholar]
- 22.Moore B. Appropriate technology for birth. The Lancet. 1985;326(8458):787. [Google Scholar]
- 23.Al Rowaily MA, Alsalem FA, Abolfotouh MA. Cesarean section in a high-parity community in Saudi Arabia: clinical indications and obstetric outcomes. BMC Pregnancy Childbirth. 2014;14(1):92. doi: 10.1186/1471-2393-14-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bragg F, Cromwell DA, Edozien LC, Gurol- Urganci I, Mahmood TA, Templeton A. Variation in rates of caesarean section among English NHS trusts after accounting for maternal and clinical risk: cross sectional study. Br Med J. 2010;341(5065):1–8. doi: 10.1136/bmj.c5065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Klemetti R, Che X, Gao Y, Raven J, Wu Z, Tang S. et al. Cesarean section delivery among primiparous women in rural China: an emerging epidemic. Am J Obstet Gynecol. 2010;202(1):65 .e1.–e6. doi: 10.1016/j.ajog.2009.08.032. [DOI] [PubMed] [Google Scholar]
- 26.Gholami A, Salarilak S. Why do some pregnant women prefer cesarean delivery in first pregnancy? Iran J Reprod Med. 2013;11(4):301. [PMC free article] [PubMed] [Google Scholar]
- 27.Gomes UA, Silva AA, Bettiol H, Barbieri MA. Risk factors for the increasing caesarean section rate in Southeast Brazil: a comparison of two birth cohorts, 1978-1979 and 1994. Int J Epidemio. 1999;28(4):687–94. doi: 10.1093/ije/28.4.687. [DOI] [PubMed] [Google Scholar]
- 28.Tang S, Li X, Wu Z. Rising cesarean delivery rate in primiparous women in urban China: evidence from three nationwide household health surveys. Am J Obstet Gynecol. 2006;195(6):1527–32. doi: 10.1016/j.ajog.2006.03.044. [DOI] [PubMed] [Google Scholar]


