Abstract
Given documented links between individual socioeconomic status (SES) and health, it is likely that—in addition to its impacts on individuals’ wallets and bank accounts—the Great Recession also took a toll on individuals’ disease and mortality risk. Exploiting a quasi-natural experiment design, this study utilizes nationally representative, longitudinal data from the National Social Life, Health, and Aging Project (NSHAP) (2005-2011) (N=930) and individual fixed effects models to examine how household-level wealth shocks experienced during the Great Recession relate to changes in biophysiological functioning in older adults. Results indicate that wealth shocks significantly predicted changes in physiological functioning, such that losses in net worth from the pre- to the post-Recession period were associated with increases in systolic blood pressure and C-reactive protein over the six year period. Further, while the association between wealth shocks and changes in blood pressure was unattenuated with the inclusion of other indicators of SES, psychosocial well-being, and health behaviors in analytic models, we document some evidence of mediation in the association between changes in wealth and changes in C-reactive protein, which suggests specificity in the social and biophysiological mechanisms relating wealth shocks and health at older ages. Linking macro-level conditions, meso-level household environments, and micro-level biological processes, this study provides new insights into the mechanisms through which economic inequality contributes to disease and mortality risk in late life.
Keywords: The Great Recession, wealth, blood pressure, inflammation, longitudinal analysis
INTRODUCTION
The Great Recession of 2007-2009 was the worst economic downturn in the United States since the Great Depression. During the two years at the height of Recession, the net worth of American households declined drastically, with the average household losing approximately $50,000 in wealth (Pfeffer, Danziger, and Schoeni 2013). Further, the economic recovery from the Recession has been among the slowest in history. As of 2011, the net worth of the typical American household was approximately 50 percent of its 2003 value (Pfeffer, Danziger, and Schoeni 2013). Given documented links between individual socioeconomic status (SES) and health, it is likely that—in addition to its impacts on individuals’ wallets and bank accounts—the Great Recession also took a toll on individuals’ disease and mortality risk.
While the Great Recession had a profound effect on earnings and employment rates, its effect on household wealth levels is of particular concern to population heath researchers. Considered a holistic measure of financial well-being by many social scientists and public health researchers interested in socioeconomic inequality (Keister and Moller 2000; Oliver and Shapiro 1995; Pollack et al. 2007; Robert and House 1996; Spilerman 2000), wealth reflects ownership of assets such as equity in homes, retirement accounts, stocks, and bonds, and it also accounts for debts and liabilities. Several studies have found that, net of other measures of SES, wealth has a significant relationship with health (Hajat et al. 2010; Hajat et al. 2011; Robert and House 1996). Further, research suggests that the relationship between wealth and health may be strongest at older ages, as individuals exit the labor market and turn increasingly to their accumulated assets to support themselves and their families (Robert and House 1996). Accordingly, the Great Recession’s effect on the retirement accounts, investments, and housing values of older adults likely had a tremendous impact on their physiological health and well-being.
To date, research on the health effects of the Great Recession has produced inconsistent results (Stuckler et al. 2015), and critical gaps in the literature linking macro-level economic conditions and health remain. Utilizing nationally representative, longitudinal data from the National Social Life, Health, and Aging Project (NSHAP) and individual fixed effects models, this study examines how household-level wealth shocks experienced during the Great Recession relate to changes in biophysiological functioning in older adults. The period of the NSHAP data collection encompassed the Recession, with Wave 1 collected in the two years immediately preceding the recession (2005-06) and Wave 2 collected in the two years following the height of the Recession (2010-11). This unique design provides a quasi-natural experiment that allows for the direct observation of individual changes in both socioeconomic well-being and health during the Recession period. By linking changes in household wealth status to changes in inflammatory response and cardiovascular function from the pre- to post-Recession period while controlling for stable individual characteristics, this study provides convincing evidence of a causal association between wealth shocks and physiological well-being. Further, this study assesses the possible psychosocial and behavioral mechanisms relating household wealth shocks to individual health changes. Linking macro-level conditions, meso-level household environments, and microlevel biological processes, this study provides new insights into the mechanisms through which economic inequality contributes to disease and mortality risk in late life.
BACKGROUND
Older Adults and the Great Recession
The Great Recession resulted in unprecedented financial losses for many American households. Between 2007 and 2009, average housing prices in the largest metropolitan areas in the US dropped by nearly one-third. Stock prices also collapsed, with the Dow Jones Index losing approximately half of its value during the period (Pfeffer, Danziger, and Schoeni 2013). Unemployment soared, jumping from 5.0 percent in December 2007 to 10.0 percent in October 2009 (U.S. Bureau of Labor Statistics 2012). In terms of relative losses, financial declines were generally greatest for less socially advantaged groups as measured by race and ethnicity, education, and prerecession income and wealth levels (Pfeffer, Danziger, and Schoeni 2013). As a result, economic disparities, particularly wealth disparities, widened during the Recession.
While older adults generally fared better than younger adults in terms of their financial losses during this period (Pew Research Center 2011), the Great Recession was nevertheless a challenging experience for many older Americans. Between 2007 and 2011, more than 1.5 million older adults lost their homes, and the foreclosure rate for older adults in 2011 was eight times higher than pre-recession rates (Trawinski 2012). With home ownership being the greatest source of household wealth in the US, the declines in housing values and rise in foreclosure had a tremendous impact on the financial stability of older adults. The median family net worth of household heads aged 55-64 years fell by nearly one-third between 2007 and 2010, and the median net worth of household heads aged 65-74 years declined by approximately 18 percent (Ackerman, Fries, and Windle 2012). Among retirees, median household net worth declined from approximately $136,000 in 2007 to $93,000 in 2010 (Ackerman, Fries, and Windle 2012). Nearly one in four adults over 50 years reported that they exhausted their savings to weather the financial challenges posed by the Recession, and approximately one in five said that they fell behind on payments and accumulated more debt during the Recession (Rix 2011).
Economic Shocks and Health
Across the life course, movement down the socioeconomic ladder is associated with increased morbidity and mortality (Smith 2004; Willson, Shuey, and Elder Jr 2007). There is no single mechanism linking SES and health, but rather there are numerous interconnected pathways whereby SES shapes individuals’ exposure to risks and access to health promoting resources to ultimately affect health and well-being (Elo and Preston 1996; Elo 2009; Krieger, Williams, and Moss 1997; Link and Phelan 1995; Marmot et al. 1998; Williams and Collins 1995). A wide body of research links economic shocks—including involuntary job loss (Brand, Levy, and Gallo 2008; Burgard, Brand, and House 2007; Coile, Levine, and McKnight 2012; Gallo et al. 2000; Sullivan and Von Wachter 2009; Turner 1995) and losses in material goods such as food and housing (Alley et al. 2009; McLaughlin et al. 2012)—to poorer health and elevated mortality risk. While much of this research has focused on unemployment and job loss, a growing body of literature focuses on the relationship between wealth and health (Hajat et al. 2010; Hajat et al. 2011; Pollack et al. 2007). In older adult samples, household wealth levels have been linked to markers of physiological functioning, including C-reactive protein (McDade, Lindau, and Wroblewski 2011). Among younger adults, financial debt has been linked to higher perceived stress and depression, worse self-rated health, and higher blood pressure (Sweet et al. 2013).
Research on the health effects of economic shocks generally proposes three possible mechanisms through which changes in financial well-being impact health and mortality risk. First, much of the literature identifies stress as the mediating mechanism. The stress process model (Pearlin et al. 1981) suggests several pathways through which wealth shocks may relate to physical health and functioning. A wealth shock can act as a direct stressor, whereby the loss in financial resources activates physiological stress response in the short term. In addition to the acute stress associated with a recent loss in financial well-being, wealth shocks may also give rise to increases in chronic stress related to ongoing difficulties paying bills, securing a place to live, and finding new employment (Burgard, Brand, and House 2007). In response to environmental or social stressors—such as a significant loss of financial assets—activity of both the sympathetic nervous system (SNS) and hypothalamic-pituitary-adrenocortical (HPA) systems increases (Seyle 1974). While temporary activation of the SNS and HPA systems in response to acute injuries and pathogens is necessary for maintaining healthy physiological functioning, longer-term activation of these systems resulting from chronic stress exposure has been associated with physiological dysregulation, including higher levels of chronic inflammation (Cohen et al. 2012; Miller, Cohen, and Ritchey 2002; Miller, Rohleder, and Cole 2009) and metabolic dysfunction (Hawkley et al. 2006; McEwen 1998; Rozanski, Blumenthal, and Kaplan 1999). Further, wealth losses may have indirect effects on physical health and functioning through stress-related psychosocial, emotional, and cognitive processes by eroding one’s sense of mastery and coping abilities and increasing one’s sense of hopelessness, frustration, and anxiety (Drentea and Reynolds 2014). Studies have documented a link between socioeconomic status and cognitive, emotional, and psychosocial factors such as personal control, perceived stress, hostility, and anger, and evidence suggests that these factors also impact individual health outcomes (Cohen, Kaplan, and Salonen 1999; Gump, Matthews, and Räikkönen 1999; Levenstein and Kaplan 1998). In this way, psychosocial processes and resources may mediate the association between SES and health and provide an indirect, stress-related pathway through which SES affects health (Drentea and Reynolds 2014; Gallo and Matthews 2003).
Second, changes in health behaviors and health-related spending in response to economic downturns may also provide a link between economic shocks and health, such that the financial instability associated with economic downturns may change behaviors in ways that affect health (Burgard, Ailshire, and Kalousova 2013). As household budgets tighten in response to economic challenges, individuals and families may reduce spending on health care, groceries, and other health-related goods and resources. A number of studies document that consumption of medical and dental care declines during economic downturns (Lusardi, Schneider, and Tufano 2010; Wall, Vujicic, and Nasseh 2012). For example, using recent data from the Medical Expenditures Panel Survey, Mortensen and Chen (2013) found that physician visits, prescription drug fills, and inpatient visits were lower during the Great Recession than in the pre-recession period. Studies also show that fruit and vegetable consumption declines when unemployment rises and fast food and snack consumption increases (Dave and Kelly 2012). In addition to cutting costs related to health promoting behaviors and activities, economic shocks can also result in increased spending on harmful coping behaviors. Research suggests that spending on behaviors such as smoking and alcohol use rises during times of increased financial instability (Black, Devereux, and Salvanes 2012; Catalano et al. 2011), which can harm health in both the short- and long-term.
Finally, changes in time use may also mediate the association between economic downturns and health (Burgard, Ailshire, and Kalousova 2013; Catalano et al. 2011; Mani et al. 2013). Individuals and households have limited time and energy, and economic shocks force individuals to invest time and energy into dealing with the shock. This means that individuals may use some of the time, physical energy, and cognitive resources usually allocated to other activities (e.g., physical activity, visiting with family or friends, medical care, etc.) to deal with the challenges and responsibilities associated with a loss in household financial well-being and stability, including finding a new job, conducting a home search, and managing household budgets (Mani et al. 2013). This swap in time use resulting from the shock can have both negative (in the case of physical activity and socially supportive behavior, for example) and positive (in the case of engaging in risky social behavior or stressful work situations) health effects.
Gaps in the Literature
While a body of research links economic shocks to health, to date, research on the health effects of the Great Recession has produced largely inconsistent results (Stuckler et al. 2015), and critical gaps in the literature linking macro-level economic conditions and individual health remain. First, most studies on the health effects of the Great Recession rely on aggregate population data by examining, for example, the relationship between population unemployment rates and death rates. While recessions are indeed macro-level events, many individuals do not directly suffer the economic shocks associated with recessions (Burgard, Ailshire, and Kalousova 2013). Examining the relationships between macro-level economic conditions and health using aggregate data may, then, underestimate the effects of economic shocks on individuals and lead to inconsistent findings. Using aggregate population data, studies find evidence of both positive and negative associations between economic downturns and health. Perhaps counterintuitively, some studies find that economic downturns are associated with decreases in morbidity and mortality from several major causes (Neumayer 2004; Ruhm 2005a; Ruhm 2005b; Tapia Granados 2008). These studies offer a number of explanations for the “procyclical” or negative association between economic downturns in health, including decreased workplace accidents, less traffic and air pollution, and increased leisure and rest. On the other hand, more recent studies offer evidence of “countercyclical” or positive associations between macro-level economic downturns and health and mortality risk. For example, using data on foreclosures and hospital and emergency room visits from four states that were among the hardest hit by the recent foreclosure crisis, Currie and Tekin (2011) found that living in a neighborhood with a spike in foreclosures was associated with significant increases in urgent unscheduled hospital visits. The inconsistent findings from these aggregate-level studies suggest that additional research using individual-level data may provide more nuanced understanding of the impact of macro-level economic downturns and household-level economic shocks on individual-level outcomes.
Second, of the studies that do examine individual-level associations between economic downturns and health, most rely on cross-sectional data, which raises concerns about health selection and omitted variable bias (Burgard, Brand, and House 2007). A major concern in studies of socioeconomic status and health is health selection, where individuals who are less healthy may have a greater likelihood of experiencing an economic shock such as a job loss or a loss in wealth (McDonough and Amick 2001). Similarly, with omitted variable bias, confounding factors not included in analytic models may put individuals at risk for both a health decline and an economic loss (Burgard, Brand, and House 2007). By failing to account for these confounders, studies may find spurious associations between economic shocks and health. Whereas cross-sectional analyses are subject to concerns about reverse causality and omitted variable bias, intra-individual examinations of how changes in SES correspond to subsequent changes in disease risk provide more convincing evidence of the impact of economic shocks on health. Longitudinal analyses, including those utilizing individual fixed effects, are better able to model change in both socioeconomic factors and health over time while controlling for stable individual characteristics (Burgard, Ailshire, and Kalousova 2013).
Finally, the biophysiological pathways underlying the link between economic shocks and health remain largely unspecified and untested. Many studies, particularly those using aggregate data, focus on mortality, but recession impacts may be underestimated if physical health changes not resulting in (immediate) death are not considered (Burgard, Ailshire, and Kalousova 2013). Several studies on economic downturns and health use general indicators of health such as self-rated health (Burgard, Brand, and House 2007), physical functioning (Gallo et al. 2000), hospital visits (Currie and Tekin 2011), and self-reports of illness (Turner 1995). Other studies use markers of mental health, such as depressive symptoms (Brand, Levy, and Gallo 2008; Cagney et al. 2014; Houle 2014). Given that the literature deems stress a critical mechanism driving the association between economic downturns and health, more research on the relationship between economic forces and biomarkers of physiological functioning is needed to improve understanding of how recessions and economic shocks “get under the skin” to affect disease and mortality risk.
This study addresses these gaps in the literature by using longitudinal data and individual fixed effects models to examine how changes in household wealth from the pre-Recession to the post-Recession period relate to individual changes in two biomarkers of physiological function: systolic blood pressure and C-reactive protein. Further, this study also examines potential behavioral and psychosocial mechanisms through which household wealth shocks associated with the Great Recession induce changes in physiological functioning to affect health and disease risk. By modeling changes in two essential markers of physiological well-being as a function of changes in household wealth and interrogating the mechanisms underlying the association between wealth and health, this study provides new insights into the relationship between macro-economic shifts and individual biological processes.
DATA AND METHODS
Data
Data for the present study are from the National Social Life, Health and Aging Project (NSHAP), a nationally-representative longitudinal study of community-dwelling older adults aged 57-85 years in 2005 – 2006 (Wave 1) and followed up in 2010 – 2011 (Wave 2) in the U.S. Of the original Wave 1 respondents, 75 percent were re-interviewed at Wave 2. African-Americans, Latinos, men and the oldest-old (75-84 years at the time of screening) were over-sampled. The NSHAP collected extensive information on respondents’ socioeconomic well-being, physical and mental health, and health behaviors, primarily thorough in-home interviews. The NSHAP also includes several biomarkers measured at Waves 1 and 2 for a subset of the sample. The NSHAP data provide a unique opportunity for examining the health effects of wealth shocks experienced during the time period of the Great Recession, as Wave 1 data was collected in the two years immediately preceding the downturn (2005-06), and Wave 2 data collection was conducted in the years immediately following the height of the Recession (2010-11).
Analyses include separate samples for the two biomarker outcomes (C-reactive protein: N=648; systolic blood pressure: N=930). The analytic samples include all respondents who have complete data on the variables used in the analyses. 2,261 respondents who were interviewed at both Waves 1 and 2 were eligible for inclusion in the analytic samples. The greatest sources of missing data included missing data on the outcomes at Waves 1 and/or 2, as well as missing wealth data at Waves 1 and/or 2. For the C-reactive protein analyses, 874 respondents were excluded from the sample because of missing data on the outcome, and an additional 656 respondents were excluded because of missing wealth data. For the systolic blood pressure analyses, 110 respondents were excluded because of missing data on the outcome, and 1,088 were excluded because of missing wealth data. For both outcomes, those excluded from the analytic sample were more likely than those included in the analytic sample to be black, older age, less educated, and female (p<0.001). To the extent that the demographic characteristics of excluded respondents are, in general, negatively associated with wealth (Pfeffer, Danziger, and Schoeni 2013; Spilerman 2000), the results can be interpreted as conservative.
Outcomes
The dependent variables for this study include two biomarker outcomes that have been linked to physiological stress response: systolic blood pressure (SBP) and C-reactive protein (CRP). SBP, a marker of cardiovascular function, is a strong predictor of chronic disease and mortality across the life course (Yang and Kozloski 2012). While younger individuals are more prone to high diastolic blood pressure, SBP is affected by increased arterial stiffness, contributing to a high prevalence of systolic hypertension in old age (Franklin et al. 1997). Unlike diastolic blood pressure, which has been found to remain constant or decline after age 50-60 years, SBP continues to increase in late life (Burt et al. 1995; Franklin et al. 1997), making it a critical marker of cardiovascular function for older adults. As part of the biomarker collection process, NSHAP respondents completed two or three seated blood pressure measures on their left arms at both Waves 1 and 2. Consistent with prior studies utilizing this measure (Cornwell and Waite 2012), we used the mean of each respondent’s SBP readings. CRP is an acute phase protein whose elevated circulating levels indicates inflammation (Finch 2010). Studies document a relationship between inflammation and health risk, including prospective associations of CRP with higher rates of coronary heart disease, stroke, and mortality (Emerging Risk Factors Collaboration 2010; Harris et al. 1999; Ridker et al. 2000). To assess levels of high-sensitivity CRP (hsCRP), NSHAP collected dried blood spots from respondents at both Waves 1 and 2. While clinicians typically use serum or plasma samples to assay CRP, the use of dried blood spots offers a convenient alternative for collecting blood samples, particularly in large population-based studies where the use of trained phlebotomists and the careful and immediate storage of samples may not be feasible (Nallanathan et al. 2008). A validation study by McDade et al. (2004) found a high correlation between dried blood spots and serum CRP. NSHAP collected dried blood spots by finger-stick. Interviewers used a disposable lancet and applied filter paper to store the samples (Nallanathan et al. 2008). As markers of physiological function, both SBP and CRP have been linked to the increased activity of the sympathetic nervous system (SNS) and hypothalamic-pituitary-adrenocortical (HPA) systems that results from exposure to social and environmental stressors (Black and Garbutt 2002; Cohen et al. 2012; McDade, Hawkley, and Cacioppo 2006; McEwen 1998; Owen et al. 2003; Yang et al. 2013; Yang, Li, and Ji 2013). Both measures are included as continuous variables in analyses. To adjust for skewedness, both measures are log transformed.
Covariates
The key independent variable in the analyses is household wealth, which is also available at both Waves 1 and 2. Research documents the critical importance of wealth for the health and financial security of older adults, in particular, who increasingly rely to their accumulated assets for consumption and stability after exiting the labor market (Robert and House 1996). At both waves, wealth was measured during the in-person interview using the following question: “Now I’d like you to think about all of the assets of your household. These are things like your house (if you own it), your cars, other rental properties and businesses you own, and financial assets like savings accounts, stocks, bonds, mutual funds, and pensions. Altogether, how much would you say that amounted to, approximately, after accounting for the loans you might have to pay off?” The measure of household wealth, then, is defined as household net worth (total assets net of debts) and is included in models as a continuous variable measured in hundreds of thousands of dollars.
In addition to wealth, we include several other measures of social status in order to assess whether it is a wealth shock, or changes in other indictors of social and financial well-being, that induces physiological changes. Other measures of social status include household income (measured in tens of thousands of dollars), employment status (1=unemployed), and marital status (1=married or cohabiting). In order to better understand the potential mechanisms underlying the link between wealth shocks and biomarker outcomes, we include several psychosocial, emotional, and health-related indicators. Measures of psychosocial and emotional well-being include depressive symptoms (a continuous measure indicated by CES-D symptoms), perceived social stress (a continuous measure using a subset of measures from Cohen’s Perceived Stress Scale), and anxiety (a continuous measure indicated by the Hospital Anxiety and Depression scale). Potential health behavior mechanisms include smoking (1=ever smoked) and drinking (number of drinks per week). We also control for changes in waist circumference (centimeters) using a continuous measure. To better account for the possibility of health selection, where changes in health status induce changes in household wealth and the individual biomarkers, we control for health status using a count index of health conditions that includes stroke, diabetes, cancer, heart disease, dementia, and arthritis (range = 0-6). Finally, we also include a measure of subjective social status, which indicates how respondents rate their household income relative to other American households (1=far below average, 2=below average, 3=average, 4=above average, 5=far above average). Other covariates include age, gender, and race. All covariates are measured at both Waves 1 and 2.
Analytic Methods
To examine the associations between wealth shocks and changes in biomarker outcomes, we first assess the bivariate associations between change in household wealth levels and change in log SBP and log CRP using two-way line plots. We then employ multivariate first difference models, which are numerically equivalent to fixed effects models for two-wave panel data. In the first difference models, changes in the log SBP and log CRP are modeled as a function of change in the independent variables, including household wealth. Time-invariant predictors, such as gender and race, are “differenced away” and omitted from model estimates, which provides a solution to the problem of unmeasured heterogeneity and omitted variable bias (Allison 1990; Gunasekara et al. 2014; Liker, Augustyniak, and Duncan 1985). Assuming that household wealth has an impact on the biomarker outcomes and that the model is measured at two time points, we can specify the model as:
| (Equation 1) |
| (Equation 2) |
In Equations 1 and 2, Wealthi1 and Wealthi2 represent household wealth at times 1 and 2. Xi1 and Xi2 represent vectors of time-varying covariates measured at times 1 and 2, and Zi represents vectors of time-constant variables, both measured and unmeasured. The difference equation can be specified by subtracting Equation 1 from Equation 2:
| (Equation 3) |
Note that, in Equation 3, the vector of Z variables are differenced out of the first difference model on the assumption that the effects of Z are time-constant. Hausman tests confirmed that the preferred model is the fixed effects or first difference model, rather than a random effects model (p<0.001).
We run models for log SBP and log CRP separately in a stepwise fashion. For each outcome, Model 1 models the biomarkers as a function of household wealth and age. Models 2-6 build on Model 1 and include additional controls and potential mediators. In addition to household wealth and age, Model 2 includes the other social status controls, including household income, employment status, and marital status. Model 3 extends Model 1 by including the psychosocial measures and assesses the extent to which the relationship between change in wealth and changes in the biomarkers is mediated by psychosocial factors, including depressive symptoms, perceived stress, and anxiety. Model 4 includes the health-related covariates. In addition to controlling for changes in health conditions to minimize possible health selection effects, Model 4 also assesses whether the relationship between changes in wealth and the biomarkers is mediated by changes in health behaviors and health status over the period. Model 5 includes the measure of subjective social status to examine whether the effect of wealth shocks on the biomarkers is mediated by respondents’ assessment of their financial standing. Finally, Model 6 is the full model that includes all covariates. As explained earlier, because race and gender are time-constant measures, they are excluded from these fixed effects models.
All models are weighted to adjust for attrition and survey design effects. Analyses were conducted in Stata 13.
RESULTS
Table 1 presents the descriptive statistics for all variables included in the analyses. The mean wealth loss in the analytic sample was approximately $5,100. While this average loss is substantially lower than the losses described by Ackerman, Fries, and Windle (2012), as described earlier, those excluded from our analytic sample were more likely than those included in the analytic sample to be black, older age, less educated, and female—all characteristics that are negatively associated with wealth. Figure 1 displays the bivariate associations between change in household wealth and change in the biomarkers. As seen in Figure 1, there is a negative relationship between change in wealth between 2005-06 and 2010-11 and change in the biomarker outcomes, where individuals experiencing the greatest wealth declines have the greatest increases in log SBP (Figure 1A) and log CRP (Figure 1B).
Table 1.
Descriptive Statistics, NSHAP 2005-2011 (N=930)
| Wave 1 (2005-2006)
|
Wave 2 (2010-2011)
|
|||
|---|---|---|---|---|
| Mean/Prop. | SD | Mean/Prop. | SD | |
| Outcomes | ||||
| SBP (log) | 4.90 | 0.13 | 4.91 | 0.14 |
| SBP (not log-transformed) | 135.24 | 18.21 | 136.57 | 19.86 |
| CRP (log CRP + 1) | 0.96 | 0.61 | 1.28 | 0.75 |
| CRP (not log transformed) | 2.36 | 3.20 | 5.14 | 15.96 |
| Social Status | ||||
| Household wealth (hundreds of thousands of dollars) | 7.09 | 18.16 | 7.04 | 16.26 |
| Household income (tens of thousands of dollars) | 6.50 | 7.65 | 6.65 | 10.06 |
| Employment (1=unemployed) | 0.02 | - | 0.03 | - |
| Marital status (1=married or cohabiting) | 0.67 | - | 0.59 | - |
| Demographics | ||||
| Age (years) | 66.32 | 6.88 | 71.49 | 6.89 |
| Gender (1=female) | 0.43 | - | - | - |
| Race | ||||
| White | 0.84 | - | - | - |
| Black | 0.07 | - | - | - |
| Hispanic | 0.07 | - | - | - |
| Other | 0.02 | - | - | - |
| Psychosocial well-being | ||||
| Depressive symptoms (CES-D) (range=0-30) | 4.24 | 4.01 | 4.16 | 3.85 |
| Perceived social stress (range=0-12) | 1.45 | 2.02 | 2.52 | 2.54 |
| Anxiety (Hospital Anxiety and Depression scale) (range=0-21) | 3.10 | 3.05 | 3.90 | 3.42 |
| Health behaviors and conditions | ||||
| Smoking (1=ever smoked) | 0.60 | - | 0.64 | - |
| Drinking (number of drinks per week) | 3.92 | 6.91 | 3.59 | 7.11 |
| Health conditions (number of health problems) | 1.07 | 0.94 | 1.07 | 1.04 |
| Waist circumference (centimeters) | 98.56 | 14.32 | 101.66 | 15.1 |
| Subjective social status | ||||
| Relative household income | ||||
| Far below average | 0.08 | - | 0.07 | - |
| Below average | 0.19 | - | 0.26 | - |
| Average | 0.38 | - | 0.41 | - |
| Above average | 0.28 | - | 0.21 | - |
| Far above average | 0.07 | - | 0.05 | - |
Notes: Because they are time-invariant measures, gender and race are not included in analytic models; these measures are included in descriptive statistics for informational purposes only. Sample size based on systolic blood pressure analytic sample. Given high levels of overlap between the CRP and SBP samples, descriptive statistics were largely similar across the samples, with two exceptions: compared to the SBP sample, the CRP sample experienced greater wealth and income losses from Wave 1 to Wave 2. Descriptive statistics are weighted to account for survey design effects and attrition.
Figure 1.
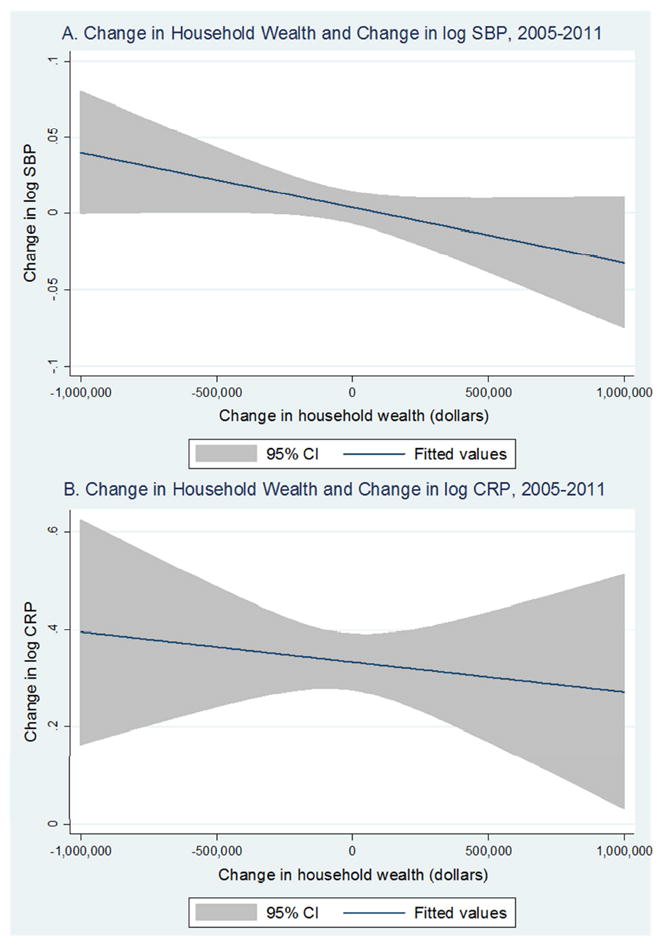
Bivariate Associations between Change in Wealth and Change in log SBP and log CRP, NSHAP (2005-2011)
Tables 2 and 3 present the results of the first difference models for log SBP and log CRP, respectively. Model 1 of Table 2 reveals a strong, negative impact of changes in household wealth on changes in log SBP (β = -0.0006, p = 0.005), such that those experiencing the greatest wealth losses also experience the greatest increases in log SBP from the pre- to the post-Recession period. Model 2 includes additional social status measures, none of which have a significant association with log SBP. These results suggest that changes in wealth are negatively associated with changes in log SBP, net of other indicators of social status. Model 3 adjusts for changes in psychosocial well-being and reveals that these indicators do not mediate the relationship between wealth and log SBP. Model 4 adjusts for changes in health status as well as changes in health behaviors. Changes in health conditions have no relationship with changes in log SBP, suggesting that health selection or reverse causality is likely not affecting the results. In Model 4 we find that changes in drinking behavior have a positive association with changes in log SBP (β = 0.002, p = 0.005), but adjusting for health behaviors and conditions in Model 4 does not attenuate the effect of household wealth change on change in log SBP over Model 1. In Model 5 we adjust for changes in subjective social status, which has no effect on log SBP. Finally, in Model 6, changes in household wealth continues to have a negative impact on changes in log SBP (β = -0.0008, p<0.001), net of all the other covariates. There is no evidence that any of the covariates in Model 6 mediate the association between changes in household wealth and changes in log SBP. In fact, in terms of coefficient magnitude and statistical significance, the relationship between changes in wealth and changes in log SBP is strongest in Model 6, the fully adjusted model.
Table 2.
First Difference Models for Log Systolic Blood Pressure, NSHAP 2005-2011 (N=930)
| Model 1 Coeff. (SE) | Model 2 Coeff. (SE) | Model 3 Coeff. (SE) | Model 4 Coeff. (SE) | Model 5 Coeff. (SE) | Model 6 Coeff. (SE) | |
|---|---|---|---|---|---|---|
| Δ Household wealth (hundreds of thousands of dollars) | -0.0006** (0.0002) | -0.0007** (0.0002) | -0.0007*** (0.0002) | -0.0006** (0.0002) | -0.0007*** (0.0002) | -0.0008*** (0.0002) |
| Δ Age (years) | 0.024† (0.012) | 0.025* (0.012) | 0.023 (0.012) | 0.021† (0.011) | 0.026† (0.013) | 0.022† (0.011) |
| Δ Household income (tens of thousands of dollars) | 0.0003 (0.0005) | 0.0004 (0.0007) | ||||
| Δ Employment (1=unemployed) | -0.021 (0.029) | -0.027 (0.029) | ||||
| Δ Marital status (1=married or cohabiting) | -0.026 (0.019) | -0.019 (0.024) | ||||
| Δ Depressive symptoms | -0.001 (0.002) | -0.002 (0.002) | ||||
| Δ Perceived social stress | 0.002 (0.002) | 0.002 (0.003) | ||||
| Δ Anxiety | -0.001 (0.001) | -0.003 (0.002) | ||||
| Δ Smoking (1=ever smoked) | 0.005 (0.014) | 0.007 (0.015) | ||||
| Δ Drinking (number of drinks per week) | 0.002** (0.001) | 0.002† (0.001) | ||||
| Δ Health conditions (number of health problems) | 0.001 (0.005) | 0.005 (0.005) | ||||
| Δ Waist circumference | 0.001 (0.001) | 0.001 (0.001) | ||||
| Δ Subjective social status | -0.001 (0.010) | -0.003 (0.009) | ||||
| Intercept | -0.118† (0.063) | -0.123† (0.062) | -0.112† (0.065) | -0.103† (0.057) | -0.126† (0.069) | -0.106† (0.061) |
p<0.001,
p<0.01,
p<0.05,
p<0.1
Note: Results from first difference models; coefficient estimates indicate how changes in the independent variables (“Δ x”) correspond to changes in log SBP (“Δ y”). All models adjust for survey design effects and attrition using sampling weights.
Table 3.
First Difference Models for Log C-Reactive Protein, NSHAP 2005-2011 (N=648)
| Model 1 Coeff. (SE) | Model 2 Coeff. (SE) | Model 3 Coeff. (SE) | Model 4 Coeff. (SE) | Model 5 Coeff. (SE) | Model 6 Coeff. (SE) | |
|---|---|---|---|---|---|---|
| Δ Household wealth (hundreds of thousands of dollars) | -0.003* (0.001) | -0.003* (0.001) | -0.003* (0.001) | -0.003* (0.001) | -0.002† (0.001) | -0.002 (0.001) |
| Δ Age (years) | -0.116 (0.090) | -0.110 (0.083) | -0.154 (0.096) | -0.094 (0.076) | -0.107 (0.095) | -0.139 (0.087) |
| Δ Household income (tens of thousands of dollars) | -0.001 (0.004) | -0.002 (0.004) | ||||
| Δ Employment (1=unemployed) | 0.165 (0.343) | 0.187 (0.399) | ||||
| Δ Marital status (1=married or cohabiting) | -0.210 (0.274) | 0.096 (0.120) | ||||
| Δ Depressive symptoms | 0.021** (0.007) | 0.021* (0.010) | ||||
| Δ Perceived social stress | -0.002 (0.010) | -0.010 (0.013) | ||||
| Δ Anxiety | -0.005 (0.011) | -0.012 (0.013) | ||||
| Δ Smoking (1=ever smoked) | -0.168 (0.178) | -0.134 (0.217) | ||||
| Δ Drinking (number of drinks per week) | -0.005 (0.005) | -0.003 (0.006) | ||||
| Δ Health conditions (number of health problems) | -0.018 (0.027) | -0.009 (0.031) | ||||
| Δ Waist circumference | 0.007† (0.004) | 0.009* (0.004) | ||||
| Δ Subjective social status | 0.085* (0.038) | 0.092* (0.037) | ||||
| Intercept | 0.922 (0.469) | 0.870* (0.427) | 1.121* (0.502) | 0.769† (0.394) | 0.857† (0.476) | 1.033* (0.453) |
p<0.001,
p<0.01,
p<0.05,
p<0.1
Note: Results from first difference models; coefficient estimates indicate how changes in the independent variables (“Δ x”) correspond to changes in log CRP (“Δ y”). All models adjust for survey design effects and attrition using sampling weights.
Table 3 presents the results from the log CRP first difference models. Similar to the log SBP models and consistent with the bivariate association presented in Figure 1B, Model 1 reveals a negative impact of changes in household wealth on changes in log CRP (β = -0.003, p = 0.014), such that individuals with the greatest losses in household wealth over the period experience the greatest increases in log CRP from Wave 1 to Wave 2. Model 2 includes additional social status measures, none of which have a significant association with changes in log CRP. Consistent with the log SBP results, Model 2 indicates that changes in household wealth are significantly associated with changes in log CRP, net of other socioeconomic indicators. Model 3 adjusts for changes in psychosocial well-being and reveals that increases in depressive symptoms are associated with increases in log CRP (β = 0.021, p = 0.002), but adjusting for changes in psychosocial well-being does not attenuate the effect of changes in household wealth on changes in log CRP (β = -0.003, p = 0.031). Model 4 adjusts for changes in health status and changes in health behaviors. Consistent with the log SBP models, changes in health conditions have no relationship with changes in log CRP, again minimizing concerns about health selection or reverse causality. Further, changes in smoking and drinking behavior between the pre- and post-Recession periods do not significantly impact changes in log CRP. Changes in waist circumference are positively associated with changes in log CRP (β = 0.007, p = 0.090), but controlling for changes in waist circumference and the other health-related indicators in Model 4 does not attenuate the effect of household wealth change on change in log CRP. Model 5 adjusts for changes in subjective social status, which, counter to expectations, has a positive association with log CRP (β = 0.085, p = 0.032). The coefficient for subjective social status indicates that, as individuals’ subjective ratings of their relative social status increases, their log CRP also increases. Finally, Model 6 adjusts for all covariates and reveals an attenuation of the impact of household wealth changes on changes in log CRP (β = -0.002, p = 0.109) over Model 1. In the final model, changes in depressive symptoms, waist circumference, and relative social status all have significant associations with changes in log CRP and, together, may mediate the association between changes in household wealth and changes in log CRP.
DISCUSSION AND CONCLUSION
Despite a surge in studies on the health effects of the Great Recession in recent years, the literature in this area is largely inconsistent, and critical gaps in our understanding of the linkages between macro-economic downturns and health and disease risk remain. As noted, most studies on the health effects of the Great Recession rely on aggregate population data, which can underestimate the effects of economic shocks on intra-individual health change. Of the studies that do examine individual-level associations between economic downturns and health, most rely on cross-sectional data, which raises concerns about health selection and omitted variable bias. Finally, the physiological processes underlying the relationship between economic shocks and health remain largely unexplored, leaving questions about biological plausibility unanswered. Utilizing longitudinal, nationally representative data, the current study attempts to improve understanding of the relationship between macro-level economic inequality and population health by examining how wealth shocks “get under the skin” to affect health and disease risk in late life.
The NSHAP provided us a unique opportunity to examine the health effects of the Great Recession, given the timing of the study’s data collection. The quasi-natural experiment design made it possible for us to examine the impact of intra-individual changes in wealth from the pre- to the post-Recession period on changes in objective markers of cardiovascular function and inflammatory response. Another key methodological strength of this study is its use of longitudinal first difference models, which allowed us to model intra-individual change over time while controlling for stable individual characteristics that can pose as confounders in cross-sectional analyses. By modeling change in two biomarker outcomes as a function of change in household wealth from the pre- to post-Recession period, our study provides stronger evidence of a causal link between economic shocks and disease risk than previous studies.
This study revealed that household level wealth shocks experienced during the Great Recession took a toll on the physiological well-being of older adults, net of other indicators of social status. While a number of studies have documented the economic impacts of recessions on older adults (Pfeffer, Danziger, and Schoeni 2013; Rix 2011; Trawinski 2012), this study demonstrates that macro-level economic downturns also pose significant health risks for older Americans. In both the bivariate analyses presented in Figure 1 and the multivariate first difference models presented in Tables 2 and 3, we consistently document a significant, negative relationship between changes in household wealth and changes in log SBP and log CRP, such that individuals who suffered the greatest wealth losses from the pre-Recession to the post-Recession period also experienced the greatest increases in markers of physiological stress response. In Model 6 of Table 2, we find that a wealth loss of $100,000 from Wave 1 to Wave 2 corresponded to a 0.998 mmHg increase in SBP. In Models 1-4 of Table 3, we found that, for every wealth loss of $100,000 respondents, on average, experienced a 0.993 mg/L increase in CRP. While these effect sizes are moderate, it is notable that we observed these changes in physiological function in an older adult sample over a short, six year time frame.
The relationship between changes in wealth and changes in SBP and CRP remained unattenuated with the inclusion of other markers of socioeconomic well-being, suggesting that wealth shocks, in particular, pose as significant threats to the health of older adults. Several studies document a cross-sectional relationship between wealth and health among older adults (McDade, Lindau, and Wroblewski 2011; Robert and House 1996; Spilerman 2000). The current study advances this body of research by using longitudinal data to document a strong, consistent relationship between changes in wealth and changes in objective markers of health at older ages.
In addition to examining the impact of household wealth shocks on changes in cardiovascular function and inflammatory response, this study also attempted to identify the possible mechanisms linking changes in household wealth to changes in individual physiology. Results in Table 2 showed that changes in drinking behavior significantly predicted changes in SBP, but this change in health behavior did not mediate the effect of wealth changes on SBP changes over the period. In fact, Model 6, which adjusts for all of the psychosocial and behavioral covariates, reveals the greatest impact of wealth changes on SBP changes in terms of coefficient magnitude and statistical significance. The results of the log CRP models in Table 3 show some evidence of possible mediation. In Model 6, the full model, changes in depressive symptoms, waist circumference, and subjective social status all significantly impacted changes in CRP, and the effect of changes in household wealth on log CRP was no longer significant. These results speak to the specificity of the social and biophysiological mechanisms linking wealth shocks to health in late life. Results from the SBP analyses showed that household wealth shocks experienced during the Great Recession acted as direct stressors by increasing physiological stress response and inducing changes in cardiovascular function. The SBP findings indicate that the depreciation or loss of assets and accumulation of new debts that occurred during the Great Recession acted as daily or “quotidian” stressors (Pearlin 1989) that served to increase blood pressure and promote physiological dysregulation in older adults. Rather than impacting SBP indirectly through changes in health behaviors or psychosocial well-being, our results demonstrate that wealth shocks acted as direct stressors to impact cardiovascular function. Alternatively, results from the CRP analysis revealed that changes in depressive symptoms, waist circumference, and subjective social status may mediate the association between changes in wealth and changes in CRP. Whereas SBP may be more of a long-term, stable indicator of physiological status, our results suggest that CRP is more responsive to changes in these proximal mediators in the short term. Across the two outcomes, this study demonstrates that individuals who experienced a direct wealth shock during the economic downturn experienced the greatest increase in physiological dysregulation from the pre- to the post-Recession period.
While this study contributes new knowledge of the health effects of the Great Recession, it is not without limitations. For one, because of data limitations, we were unable to investigate the role other potential mediators, such as changes in time use or spending, which could underlie the relationship between wealth shocks and changes in the biomarkers. While our use of longitudinal first difference models eliminates the bias introduced by unmeasured time-invariant factors such as the stable characteristics of individuals, there are possibly other unmeasured time-varying factors, such as changes in medication use, which could serve as mediators or sources of unmeasured confounding. Also, because the NSHAP only includes a single measure of household net worth, we are unable to determine how changes in different sources of wealth (e.g., stocks, housing, retirement accounts) relate to changes in the biomarkers. Additionally, the use of a single measure of wealth may result in measurement error. Future studies should consider using multidimensional indicators of household net worth to improve measurement and to examine how various sources of wealth and debt contribute to health inequality. Third, because of relatively small sample sizes, we were unable to run stratified models by race, socioeconomic status, or gender, which could provide additional insights into the processes through which the Great Recession affected population health disparities. Fourth, in our CRP analyses, we were unable to determine if respondents had an active infection at the time of the biomarker collection at Wave 2, which may have contributed to increases in CRP. Supplementary analyses that excluded participants with elevated CRP (≥10 mg/L) suffered from power issues, so we do not show them here. Future research with larger samples should include sensitivity analyses excluding respondents with acutely high elevations in CRP and further consider whether the development of infections is a possible biological mechanism linking wealth shocks to biomarkers of health. Finally, while we utilize two waves of longitudinal data, the release of the third wave of the NSHAP will allow researchers to further examine how economic changes impacted disease risk in the post-Recession recovery period.
While recessions are, indeed, macro-level societal events, as demonstrated in this study, they also impact micro-level biological processes. Findings from this study suggest that economic policies and interventions aimed at reducing the financial insecurity of older adults can impact public health during times of economic downturn. Policies targeting predatory lending practices and interventions designed to prevent foreclosure, for example, can reduce population health risk by decreasing the physiological stress associated with financial insecurity. Future research on the health impacts of recessions and other environmental shocks can help to further specify mechanisms and identify the vulnerable subpopulations to target with public health intervention.
Our study also suggests the importance of including multiple dimensions of SES in assessing health of older adults from a life course perspective. Unlike shorter-term measures of SES such as annual income, indicators of household wealth uniquely capture the life-long accumulation process of economic status that buffers against unpredictable stressors as one ages. Results from this study point to the distinctive effects of wealth on biomarkers of health, net of other indictors of SES, and speak to the need for incorporating measures of wealth into studies of health inequality, particularly in studies of aging populations. The findings presented here also suggest that it is especially important to aid in building the wealth and financial security of individuals early on in the adult life course to protect health and well-being later in life.
Though older adults experienced fewer financial losses than their younger counterparts during the Great Recession, their reliance on their accumulated assets and their relative biological frailty may have made older adults particularly susceptible to the wealth shocks and physiological stress associated with this most recent recession. As job numbers, housing values, and stock prices continue to improve, it remains to be seen whether the bodies of those who experienced financial losses will also recover.
Examines health effects of Great Recession for older adults using biomarker data
Combines a quasi-natural experiment design with longitudinal fixed effects models
Reveals causal association of changes in wealth and changes in SBP and CRP
Assesses psychosocial and behavioral mechanisms linking wealth changes and health
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ackerman, Robert A, Fries Gerhard, Windle Richard A. Changes in US Family Finances from 2007 to 2010: Evidence from the Survey of Consumer Finances. Federal Reserve Bulletin. 2012;100:1–80. [Google Scholar]
- Alley DE, Soldo BJ, Pagan JA, McCabe J, DeBlois M, Field SH, Asch DA, Cannuscio C. Material Resources and Population Health: Disadvantages in Health Care, Housing, and Food among Adults Over 50 Years of Age. American Journal of Public Health. 2009;99(Suppl 3):S693–701. doi: 10.2105/AJPH.2009.161877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allison Paul D. Change Scores as Dependent Variables in Regression Analysis. Sociological Methodology. 1990;20(1):93–114. [Google Scholar]
- Black Paul H, Garbutt Lisa D. Stress, Inflammation and Cardiovascular Disease. Journal of Psychosomatic Research. 2002;52(1):1–23. doi: 10.1016/s0022-3999(01)00302-6. [DOI] [PubMed] [Google Scholar]
- Black Sandra E, Devereux Paul J, Salvanes Kjell G. Losing Heart? the Effect of Job Displacement on Health. 2012 NBER Working Paper No 18660. [Google Scholar]
- Brand JE, Levy BR, Gallo WT. Effects of Layoffs and Plant Closings on Depression among Older Workers. Research on Aging. 2008;30(6):701–721. doi: 10.1177/0164027508322574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgard Sarah A, Ailshire Jennifer A, Kalousova Lucie. The Great Recession and Health People, Populations, and Disparities. The Annals of the American Academy of Political and Social Science. 2013;650(1):194–213. [Google Scholar]
- Burgard SA, Brand JE, House JS. Toward a Better Estimation of the Effect of Job Loss on Health. Journal of Health and Social Behavior. 2007;48(4):369–384. doi: 10.1177/002214650704800403. [DOI] [PubMed] [Google Scholar]
- Burt VL, Whelton P, Roccella EJ, Brown C, Cutler JA, Higgins M, Horan MJ, Labarthe D. Prevalence of Hypertension in the US Adult Population. Results from the Third National Health and Nutrition Examination Survey, 1988-1991. Hypertension. 1995;25(3):305–313. doi: 10.1161/01.hyp.25.3.305. [DOI] [PubMed] [Google Scholar]
- Cagney Kathleen A, Browning Christopher R, Iveniuk James, English Ned. The Onset of Depression during the Great Recession: Foreclosure and Older Adult Mental Health. Journal Information. 2014;104(3) doi: 10.2105/AJPH.2013.301566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catalano R, Goldman-Mellor S, Saxton K, Margerison-Zilko C, Subbaraman M, LeWinn K, Anderson E. The Health Effects of Economic Decline. Annual Review of Public Health. 2011;32:431–450. doi: 10.1146/annurev-publhealth-031210-101146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen Sheldon, Kaplan George A, Salonen Jukka T. The Role of Psychological Characteristics in the Relation between Socioeconomic Status and Perceived Health1. Journal of Applied Social Psychology. 1999;29(3):445–468. [Google Scholar]
- Cohen S, Janicki-Deverts D, Doyle WJ, Miller GE, Frank E, Rabin BS, Turner RB. Chronic Stress, Glucocorticoid Receptor Resistance, Inflammation, and Disease Risk. Proceedings of the National Academy of Sciences of the United States of America. 2012;109(16):5995–5999. doi: 10.1073/pnas.1118355109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coile Courtney C, Levine Phillip B, McKnight Robin. Recessions, Older Workers, and Longevity: How Long are Recessions Good for Your Health? 2012 NBER Working Paper No 18361. [Google Scholar]
- Cornwell EY, Waite LJ. Social Network Resources and Management of Hypertension. Journal of Health and Social Behavior. 2012;53(2):215–231. doi: 10.1177/0022146512446832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Currie Janet, Tekin Erdal. Is there a Link between Foreclosure and Health? 2011 doi: 10.1257/pol.20120325. NBER Working Paper No 17310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dave Dhaval M, Kelly Inas R. How does the Business Cycle Affect Eating Habits? Social Science & Medicine. 2012;74(2):254–262. doi: 10.1016/j.socscimed.2011.10.005. [DOI] [PubMed] [Google Scholar]
- Drentea Patricia, Reynolds John R. Where does Debt Fit in the Stress Process Model? Society and Mental Health. 2014;5(1):16–32. doi: 10.1177/2156869314554486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elo Irma T. Social Class Differentials in Health and Mortality: Patterns and Explanations in Comparative Perspective. Annual Review of Sociology. 2009;35:553–572. [Google Scholar]
- Elo Irma T, Preston Samuel H. Educational Differentials in Mortality: United States 1979–1985. Social Science & Medicine. 1996;42(1):47–57. doi: 10.1016/0277-9536(95)00062-3. [DOI] [PubMed] [Google Scholar]
- Emerging Risk Factors Collaboration. C-Reactive Protein Concentration and Risk of Coronary Heart Disease, Stroke, and Mortality: An Individual Participant Meta-Analysis. The Lancet. 2010;375(9709):132–140. doi: 10.1016/S0140-6736(09)61717-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finch Caleb E. The Biology of Human Longevity:: Inflammation, Nutrition, and Aging in the Evolution of Lifespans. Academic Press; 2010. [Google Scholar]
- Franklin SS, Gustin W, 4th, Wong ND, Larson MG, Weber MA, Kannel WB, Levy D. Hemodynamic Patterns of Age-Related Changes in Blood Pressure. the Framingham Heart Study. Circulation. 1997;96(1):308–315. doi: 10.1161/01.cir.96.1.308. [DOI] [PubMed] [Google Scholar]
- Gallo Linda C, Matthews Karen A. Understanding the Association between Socioeconomic Status and Physical Health: Do Negative Emotions Play a Role? Psychological Bulletin. 2003;129(1):10. doi: 10.1037/0033-2909.129.1.10. [DOI] [PubMed] [Google Scholar]
- Gallo WT, Bradley EH, Siegel M, Kasl SV. Health Effects of Involuntary Job Loss among Older Workers: Findings from the Health and Retirement Survey. The Journals of Gerontology Series B, Psychological Sciences and Social Sciences. 2000;55(3):S131–40. doi: 10.1093/geronb/55.3.s131. [DOI] [PubMed] [Google Scholar]
- Gump Brooks B, Matthews Karen A, Räikkönen Katri. Modeling Relationships among Socioeconomic Status, Hostility, Cardiovascular Reactivity, and Left Ventricular Mass in African American and White Children. Health Psychology. 1999;18(2):140. doi: 10.1037//0278-6133.18.2.140. [DOI] [PubMed] [Google Scholar]
- Gunasekara FI, Richardson K, Carter K, Blakely T. Fixed Effects Analysis of Repeated Measures Data. International Journal of Epidemiology. 2014;43(1):264–269. doi: 10.1093/ije/dyt221. [DOI] [PubMed] [Google Scholar]
- Hajat A, Kaufman JS, Rose KM, Siddiqi A, Thomas JC. Do the Wealthy have a Health Advantage? Cardiovascular Disease Risk Factors and Wealth. Social Science & Medicine. 2010;71(11):1935–1942. doi: 10.1016/j.socscimed.2010.09.027. [DOI] [PubMed] [Google Scholar]
- Hajat A, Kaufman JS, Rose KM, Siddiqi A, Thomas JC. Long-Term Effects of Wealth on Mortality and Self-Rated Health Status. American Journal of Epidemiology. 2011;173(2):192–200. doi: 10.1093/aje/kwq348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris Tamara B, Ferrucci Luigi, Tracy Russell P, Corti MC, Wacholder Sholom, Ettinger Walter H, Heimovitz Harley, Cohen Harvey J, Wallace Robert. Associations of Elevated Interleukin-6 and C-Reactive Protein Levels with Mortality in the Elderly. The American Journal of Medicine. 1999;106(5):506–512. doi: 10.1016/s0002-9343(99)00066-2. [DOI] [PubMed] [Google Scholar]
- Hawkley Louise C, Masi Christopher M, Berry Jarett D, Cacioppo John T. Loneliness is a Unique Predictor of Age-Related Differences in Systolic Blood Pressure. Psychology and Aging. 2006;21(1):152. doi: 10.1037/0882-7974.21.1.152. [DOI] [PubMed] [Google Scholar]
- Houle Jason N. Mental Health in the Foreclosure Crisis. Social Science & Medicine. 2014;118:1–8. doi: 10.1016/j.socscimed.2014.07.054. [DOI] [PubMed] [Google Scholar]
- Keister Lisa A, Moller Stephanie. Wealth Inequality in the United States. Annual Review of Sociology. 2000;26:63–81. ( http://www.jstor.org/stable/223437) [Google Scholar]
- Krieger Nancy, Williams David R, Moss Nancy E. Measuring Social Class in US Public Health Research: Concepts, Methodologies, and Guidelines. Annual Review of Public Health. 1997;18(1):341–378. doi: 10.1146/annurev.publhealth.18.1.341. [DOI] [PubMed] [Google Scholar]
- Levenstein Susan, Kaplan George A. Socioeconomic Status and Ulcer: A Prospective Study of Contributory Risk Factors. Journal of Clinical Gastroenterology. 1998;26(1):14–17. doi: 10.1097/00004836-199801000-00005. [DOI] [PubMed] [Google Scholar]
- Liker Jeffrey K, Augustyniak Sue, Duncan Greg J. Panel Data and Models of Change: A Comparison of First Difference and Conventional Two-Wave Models. Social Science Research. 1985;14(1):80–101. [Google Scholar]
- Link Bruce G, Phelan Jo. Social Conditions as Fundamental Causes of Disease. Journal of Health and Social Behavior. 1995:80–94. [PubMed] [Google Scholar]
- Lusardi Annamaria, Schneider Daniel J, Tufano Peter. The Economic Crisis and Medical Care Usage. 2010 NBER Working Paper No 15843. [Google Scholar]
- Mani A, Mullainathan S, Shafir E, Zhao J. Poverty Impedes Cognitive Function. Science (New York, N.Y.) 2013;341(6149):976–980. doi: 10.1126/science.1238041. [DOI] [PubMed] [Google Scholar]
- Marmot MG, Fuhrer R, Ettner SL, Marks NF, Bumpass LL, Ryff CD. Contribution of Psychosocial Factors to Socioeconomic Differences in Health. The Milbank Quarterly. 1998;76(3):403–48. 305. doi: 10.1111/1468-0009.00097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDade TW, Burhop J, Dohnal J. High-Sensitivity Enzyme Immunoassay for C-Reactive Protein in Dried Blood Spots. Clinical Chemistry. 2004;50(3):652–654. doi: 10.1373/clinchem.2003.029488. [DOI] [PubMed] [Google Scholar]
- McDade TW, Hawkley LC, Cacioppo JT. Psychosocial and Behavioral Predictors of Inflammation in Middle-Aged and Older Adults: The Chicago Health, Aging, and Social Relations Study. Psychosomatic Medicine. 2006;68(3):376–381. doi: 10.1097/01.psy.0000221371.43607.64. [DOI] [PubMed] [Google Scholar]
- McDade TW, Lindau ST, Wroblewski K. Predictors of C-Reactive Protein in the National Social Life, Health, and Aging Project. The Journals of Gerontology Series B, Psychological Sciences and Social Sciences. 2011;66(1):129–136. doi: 10.1093/geronb/gbq008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonough Peggy, Amick Benjamin C. The Social Context of Health Selection: A Longitudinal Study of Health and Employment. Social Science & Medicine. 2001;53(1):135–145. doi: 10.1016/s0277-9536(00)00318-x. [DOI] [PubMed] [Google Scholar]
- McEwen Bruce S. Stress, Adaptation, and Disease: Allostasis and Allostatic Load. Annals of the New York Academy of Sciences. 1998;840(1):33–44. doi: 10.1111/j.1749-6632.1998.tb09546.x. [DOI] [PubMed] [Google Scholar]
- McLaughlin Katie A, Nandi Arijit, Keyes Katherine M, Uddin Monica, Aiello Allison E, Galea Sandro, Koenen KC. Home Foreclosure and Risk of Psychiatric Morbidity during the Recent Financial Crisis. Psychological Medicine. 2012;42(07):1441–1448. doi: 10.1017/S0033291711002613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller Gregory E, Cohen Sheldon, Ritchey AK. Chronic Psychological Stress and the Regulation of Pro-Inflammatory Cytokines: A Glucocorticoid-Resistance Model. Health Psychology. 2002;21(6):531. doi: 10.1037//0278-6133.21.6.531. [DOI] [PubMed] [Google Scholar]
- Miller GE, Rohleder N, Cole SW. Chronic Interpersonal Stress Predicts Activation of Pro- and Anti-Inflammatory Signaling Pathways 6 Months Later. Psychosomatic Medicine. 2009;71(1):57–62. doi: 10.1097/PSY.0b013e318190d7de. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mortensen Karoline, Chen Jie. The Great Recession and Racial and Ethnic Disparities in Health Services Use. JAMA Internal Medicine. 2013;173(4):315–317. doi: 10.1001/jamainternmed.2013.1414. [DOI] [PubMed] [Google Scholar]
- Nallanathan B, Williams S, McDade T, Lindau ST. Dried Blood Spot Measurement of C-reactive protein in Wave I of the National Social Life, Health & Aging Project (NSHAP) NORC and the University of Chicago; 2008. [Google Scholar]
- Neumayer Eric. Recessions Lower (some) Mortality Rates:: Evidence from Germany. Social Science & Medicine. 2004;58(6):1037–1047. doi: 10.1016/s0277-9536(03)00276-4. [DOI] [PubMed] [Google Scholar]
- Oliver Melvin L, Shapiro Thomas M. Black Wealth/White Wealth 1995 [Google Scholar]
- Owen Natalie, Poulton Terry, Hay Frank C, Mohamed-Ali Vidya, Steptoe Andrew. Socioeconomic Status, C-Reactive Protein, Immune Factors, and Responses to Acute Mental Stress. Brain, Behavior, and Immunity. 2003;17(4):286–295. doi: 10.1016/s0889-1591(03)00058-8. [DOI] [PubMed] [Google Scholar]
- Pearlin Leonard I. The Sociological Study of Stress. Journal of Health and Social Behavior. 1989;30(3):241–256. [PubMed] [Google Scholar]
- Pearlin Leonard I, Menaghan Elizabeth G, Lieberman Morton A, Mullan Joseph T. The Stress Process. Journal of Health and Social Behavior. 1981;22(4):337–356. [PubMed] [Google Scholar]
- Pew Research Center. Angry Silents, Disengaged Millennials: The Generation Gap and the 2012 Election. Washington, DC: Pew Research Center; 2011. [Google Scholar]
- Pfeffer Fabian T, Danziger Sheldon, Schoeni Robert F. Wealth Disparities before and After the Great Recession. The Annals of the American Academy of Political and Social Science. 2013;650(1):98–123. doi: 10.1177/0002716213497452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollack Craig E, Chideya Sekai, Cubbin Catherine, Williams Brie, Dekker Mercedes, Braveman Paula. Should Health Studies Measure Wealth?: A Systematic Review. American Journal of Preventive Medicine. 2007;33(3):250–264. doi: 10.1016/j.amepre.2007.04.033. [DOI] [PubMed] [Google Scholar]
- Ridker Paul M, Hennekens Charles H, Buring Julie E, Rifai Nader. C-Reactive Protein and Other Markers of Inflammation in the Prediction of Cardiovascular Disease in Women. New England Journal of Medicine. 2000;342(12):836–843. doi: 10.1056/NEJM200003233421202. [DOI] [PubMed] [Google Scholar]
- Rix Sara E. Recovering from the Great Recession: Long Struggle Ahead for Older Americans. AARP Policy Institute 2011 [Google Scholar]
- Robert S, House JS. SES Differentials in Health by Age and Alternative Indicators of SES. Journal of Aging and Health. 1996;8(3):359–388. doi: 10.1177/089826439600800304. [DOI] [PubMed] [Google Scholar]
- Rozanski A, Blumenthal JA, Kaplan J. Impact of Psychological Factors on the Pathogenesis of Cardiovascular Disease and Implications for Therapy. Circulation. 1999;99(16):2192–2217. doi: 10.1161/01.cir.99.16.2192. [DOI] [PubMed] [Google Scholar]
- Ruhm Christopher J. Healthy Living in Hard Times. Journal of Health Economics. 2005a;24(2):341–363. doi: 10.1016/j.jhealeco.2004.09.007. [DOI] [PubMed] [Google Scholar]
- Ruhm CJ. Commentary: Mortality Increases during Economic Upturns. International Journal of Epidemiology. 2005b;34(6):1206–1211. doi: 10.1093/ije/dyi143. [DOI] [PubMed] [Google Scholar]
- Seyle Hans. Stress without Distress. Lippincott Williams & Wilkins; 1974. [Google Scholar]
- Smith James P. Unraveling the SES: Health Connection. Population and Development Review. 2004:108–132. [Google Scholar]
- Spilerman Seymour. Wealth and Stratification Processes. Annual Review of Sociology. 2000;26:497–524. [Google Scholar]
- Stuckler David, Reeves Aaron, Karanikolos Marina, McKee Martin. The Health Effects of the Global Financial Crisis: Can we Reconcile the Differing Views? A Network Analysis of Literature Across Disciplines. Health Economics, Policy and Law. 2015;10(01):83–99. doi: 10.1017/S1744133114000255. [DOI] [PubMed] [Google Scholar]
- Sullivan Daniel, Wachter Till Von. Job Displacement and Mortality: An Analysis using Administrative Data. The Quarterly Journal of Economics. 2009;124(3):1265–1306. [Google Scholar]
- Sweet Elizabeth, Nandi Arijit, Adam Emma K, McDade Thomas W. The High Price of Debt: Household Financial Debt and its Impact on Mental and Physical Health. Social Science & Medicine. 2013;91:94–100. doi: 10.1016/j.socscimed.2013.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tapia Granados Jose A. Macroeconomic Fluctuations and Mortality in Postwar Japan. Demography. 2008;45:323–343. doi: 10.1353/dem.0.0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trawinski Lori A. Nightmare on Main Street: Older Americans and the Mortgage Market. Crisis AARP Public Policy Institute; 2012. [Google Scholar]
- Turner JB. Economic Context and the Health Effects of Unemployment. Journal of Health and Social Behavior. 1995;36(3):213–229. [PubMed] [Google Scholar]
- U.S. Bureau of Labor Statistics. The Recession of 2007-2009 2012 [Google Scholar]
- Wall TP, Vujicic M, Nasseh K. Recent Trends in the Utilization of Dental Care in the United States. Journal of Dental Education. 2012;76(8):1020–1027. [PubMed] [Google Scholar]
- Williams David R, Collins Chiquita. US Socioeconomic and Racial Differences in Health: Patterns and Explanations. Annual Review of Sociology. 1995:349–386. [Google Scholar]
- Willson Andrea E, Shuey Kim M, Elder Glen H., Jr Cumulative Advantage Processes as Mechanisms of Inequality in Life Course Health1. American Journal of Sociology. 2007;112(6):1886–1924. [Google Scholar]
- Yang Yang, Kozloski Michael. Change of Sex Gaps in Total and Cause-Specific Mortality Over the Life Span in the United States. Annals of Epidemiology. 2012;22(2):94–103. doi: 10.1016/j.annepidem.2011.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang YC, McClintock MK, Kozloski M, Li T. Social Isolation and Adult Mortality: The Role of Chronic Inflammation and Sex Differences. J Health Soc Behav. 2013;54(2):182–202. doi: 10.1177/0022146513485244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Yang, Li Ting, Ji Yinchun. Impact of Social Integration on Metabolic Functions: Evidence from a Nationally Representative Longitudinal Study of US Older Adults. BMC Public Health. 2013;13(1):1210. doi: 10.1186/1471-2458-13-1210. ( http://www.biomedcentral.com/1471-2458/13/1210) [DOI] [PMC free article] [PubMed] [Google Scholar]


