Abstract
Purpose/Objectives
To determine whether improved monitoring through close follow-up with a nurse practitioner (NP) could enhance treatment compliance and decrease frequency of hospitalizations.
Design
Retrospective chart review.
Setting
An academic National Cancer Institute–designated comprehensive cancer center.
Sample
151 patients aged 45–65 years diagnosed with stage III or IV oropharyngeal cancer.
Methods
Patients were nonrandomized to one of two groups: a prechemotherapy clinic group and a weekly NP-led clinic group. After examination of descriptive statistics, multiple linear and logistic regressions were used to compare groups across patient outcomes.
Main Research Variables
Hospitalization, chemotherapy dose deviations, and chemotherapy treatment completion.
Findings
The average number of visits during traditional treatment was three and, after initiation of the NP-led clinic, the number was six. The hospitalization rate was 28% in the traditional clinic group compared to 12% in the NP-led group. The rate of chemotherapy dose deviations was 48% in the traditional clinic group compared to 6% in the NP-led clinic group. Forty-six percent of patients in the traditional clinic group received the full seven scheduled doses of chemotherapy compared to 90% of patients seen in the NP-led clinic group.
Conclusions
A weekly NP-led symptom management clinic reduces rates of hospitalization and chemotherapy dose deviations and increases chemotherapy completion in patients receiving intensive chemoradiotherapy for oropharyngeal cancer.
Implications for Nursing
Patients receiving chemoradiotherapy benefit from close monitoring for toxicities by NPs to successfully complete their treatment and avoid hospitalization.
Knowledge Translation
Early interventions to manage toxicities in patients with head and neck cancer can improve outcomes. NPs are in a key position to manage these toxicities and, when symptoms are controlled, costs are reduced.
Patients with locally advanced oropharyngeal cancer are at risk for poor outcomes because of the multimodal nature of treatment and the potential for treatment-related toxicity. Primary treatment of patients with locally advanced oropharyngeal cancer includes a nonsurgical organ-preservation approach. Chemoradiotherapy (concurrent chemotherapy with radiation therapy) for seven weeks has replaced surgery, avoiding the permanent alteration of the patient’s ability to speak and swallow (Takes et al., 2012). Although organ preservation is possible for many of these patients, the side effects of chemoradiotherapy can be debilitating. Common toxicities include pain, weight loss, dehydration, copious secretions, aspiration, mucositis, nausea, vomiting, and constipation (Argiris, Karamouzis, Raben, & Ferris, 2008). When these toxicities are not properly managed, they can lead to treatment delays, chemotherapy dose deviations, and hospitalizations (Bensinger et al., 2008). Research findings suggest that treatment with chemoradiotherapy has dramatically increased the supportive care needs of patients with advanced oropharyngeal cancer (Mallick & Waldron, 2009).
Toxicity management of patients undergoing chemoradiotherapy for advanced oropharyngeal cancer is both challenging and costly. Patients who developed severe mucositis from combined chemoradiotherapy for head and neck cancer are reported to incur 52% higher costs during their treatment phase than patients without severe mucositis (Nonzee et al., 2008). As healthcare costs continue to rise, clinicians must develop efficient and effective interventions to manage these significant toxicities. Nurse practitioners (NPs) have an important role to play in intervention development (Hinkel et al., 2010). Data suggest that NP-led clinical programs for patients with advanced cancer have excellent outcomes (McCorkle et al., 2009), and a systematic review by Newhouse et al. (2011) concluded that advanced practice nurses can provide safe, high-quality patient care across an array of clinical populations.
A review of the literature revealed that very little data exists evaluating the impact of supportive care for patients with head and neck cancer by NPs during treatment with chemoradiotherapy. One study that evaluated nurse-led treatment of patients undergoing radiation therapy to the head and neck concluded that oncology-trained nurses are well situated to manage treatment-related toxicities (Wells et al., 2008). The study did not examine the role of NP management, nor did it include patients receiving chemoradiotherapy. In addition, the study examined symptom management and satisfaction, but did not examine hospitalization, dose deviation, and failure to complete treatment because of toxicities from treatment.
Patients with concurrent chemoradiotherapy to the oropharynx treated at the University of Michigan Cancer Center often experienced grade 3 or 4 toxicities, requiring hospitalization, dose deviations, and treatment delays. Toxicities were graded according to the Common Terminology Criteria for Adverse Events (CTCAE), version 4 (National Cancer Institute, 2010). Patients were routinely seen at the beginning, middle, and end of treatment. They often were very ill by their second visit. Some of the treatment-related side effects included mucositis (which subsequently led to debilitating dehydration), weight loss, nausea, and vomiting. Constipation also was frequently reported because of opiate and antiemetic use. These concerns led the clinical leadership to develop a symptom management clinic for patients who received this complex treatment regimen. The clinical leadership team recognized the need to document clinical outcomes before and after implementation of this clinic.
The ability of NPs to improve outcomes for this vulnerable patient population was evaluated using a retrospective chart review to compare outcomes for patients who were managed in a weekly NP clinic to patients who were treated prior to the initiation of the NP clinic.
Nurse Practitioner Clinic Design and Operation
Prior to clinic implementation, new patients referred from the otolaryngology department were seen in the clinic by the NP and the medical oncologist to establish a treatment plan. Patients received written and verbal education regarding chemotherapy expectations and side effects during this visit. They were then seen in the middle of their radiation therapy for symptom management. Patients often were very sick at this time, requiring intervention that could lead to reductions in their chemotherapy doses. In an attempt to better manage treatment-related symptoms in patients with head and neck cancer, an independent NP clinic was established at the authors’ institution in 2006. The NP clinic is under the administrative direction of the cancer center. The medical oncologist is the supervising physician and is available during clinic hours by phone. Patients receiving concurrent chemoradiotherapy are seen weekly during active therapy. Programmatic goals are to improve patient overall quality of life during and after treatment, and to identify and manage toxicities to avoid dose deviation, treatment delays, and hospitalizations. The authors hypothesized that early, frequent intervention and support of these patients could improve clinical outcomes. Of note, the patients also are seen periodically by the radiation oncologist throughout their treatment, but management of the supportive care needs is deferred to the medical oncology department.
The NP clinic is staffed by two NPs, one RN, and several medical assistants. Patients can be seen by either NP, and usually each patient will see both during their treatment course. Patients are scheduled to be seen in the clinic on week 2 of treatment and are then seen weekly until one to two weeks after completion. Symptoms often peak when the patient completes the entire planned treatment. A dietitian and social worker also are available during visits as clinically indicated.
Each clinic visit focuses on treatment toxicities and specific concerns of the patient and their significant other. This includes physical as well as psychological, social, and spiritual needs. The patient’s weight is monitored to assess for excessive weight loss. This is coupled with an assessment of their activity, exercise, and fatigue level. Laboratory studies, including complete blood count, differential, and electrolytes, are performed and evaluated. A complete physical examination is conducted, focusing on the area affected by radiotherapy. Recommendations and supportive care treatment plans are made in partnership with the patient and their significant other. This may include pain medication, antiemetics, hydration, antidepressants, or anxiety medication. Referrals to the social worker and the dietitian or a referral for a procedure such as feeding tube placement also are made as warranted during the visit.
Operationally, two NPs are available for each clinic. Appointments are scheduled with two patients being seen every half hour throughout the day. Patients who are undergoing active treatment are scheduled in the morning to allow adequate time for laboratory evaluation and chemotherapy infusion prior to their radiation therapy. The afternoon is available for those patients who have completed treatment but require additional supportive care. The two NPs who manage the clinic also work directly with the medical oncologist on different clinic days to see new and palliative care patients with head and neck cancer.
Methods
As the NP-led clinic model is the current model of supportive care for patients with head and neck cancer treated at the authors’ institution, a retrospective chart review was completed to evaluate patient outcomes before and after clinic implementation. Retrospective reviews of the clinic’s schedules were used to identify patients seen prior to the initiation of the NP clinic as well as after. The NP reviewed the record to determine eligibility. Once eligibility was established, the patient became part of the sample and his or her chart was reviewed for outcomes. Three primary outcomes were evaluated: patient hospitalization, treatment dose deviation, and treatment completion. These outcomes were chosen given their potential impacts on costs of care, patient satisfaction, and overall patient outcome. Human subject approval was obtained prior to the start of chart review.
Sample
The retrospective chart review was performed with patients with head and neck cancer in a National Cancer Institute–designated comprehensive cancer center. Data were abstracted from medical charts of patients treated with stage III or IV oropharyngeal cancers. Fifty patients were selected prior to the development of the NP-led clinic, and 51 patients were selected after the development of the NP-led clinic. The patients were included if they met eligibility criteria. For group 1, treatment dates had to occur from January 2002 to August 2006. For group 2, treatment dates had to occur from September 2006 to June 2010. Both groups included patients aged 45–65 years. All patients had a confirmed diagnosis of stage III or IV oropharyngeal cancer, with a prescribed treatment plan of seven weeks of daily radiation of 2 Gy (five days weekly) and concurrent weekly chemotherapy dosed at carboplatin AUC (area under the concentration-time curve) 1 and paclitaxel 30 mg/m2. Exclusion criteria included being younger than age 45 or older than age 65 years and an Eastern Cooperative Oncology Group performance status less than 1.
Measures
Three clinical outcomes were extracted from the chart review. All were measured as dichotomous outcomes (“yes” or “no”). The first was the occurrence of any hospitalization within two weeks of treatment initiation. Only hospital admissions for treatment toxicities were included. The second outcome was chemotherapy dose reduction. Using the CTCAE, chemotherapy doses were reduced in the presence of grade 3 or 4 toxicity. The clinic’s standing protocol was to decrease paclitaxel from 30 mg/m2 to 20 mg/m2 when toxicity first occurs. Paclitaxel was discontinued if unacceptable toxicities continued. The third outcome was chemotherapy regimen completion, defined as successful completion of all seven cycles of planned chemotherapy. Chemotherapy was held until all grade 3 or 4 toxicities were resolved, and was discontinued after the second dose reduction. Variables considered in analyses included age at diagnosis (measured in years), tumor stage (III versus IV), and primary tumor location (base of tongue, tonsil, or other).
Data Analysis
Descriptive statistics were used to compare differences in important covariates, such as age at diagnosis, tumor stage, and primary tumor location between groups. Statistical analyses were performed using R, version 2.14, software. Next, unadjusted rates of hospitalization, chemotherapy dose reduction, and chemotherapy regimen completion were compared between groups. In addition, the authors compared the number of visits by the patient and number of days from referral to new patient contact, before and after the NP-led clinic. Finally, logistic regression models were used to estimate the likelihood of all three outcomes between groups, both unadjusted and results adjusted for age at diagnosis, tumor stage, and primary tumor location. Parameter estimates obtained by the logistic regression models were converted to odds ratios (ORs) with corresponding 95% confidence intervals (CIs). The number of days from referral to new patient contact was analyzed using linear regression, both unadjusted and adjusted for age, stage, and site. Finally, the authors compared the frequency of toxicities reported in the medical record notes by the medical oncologist or NPs during a seven-week time period. These were classified into discrete categories: dehydration, placement of feeding tube (percutaneous gastrostomy or Dobhoff), mucositis, pain or neuropathy, nausea and vomiting, and weight loss or malnutrition. Significance level values were not adjusted for multiple comparisons.
Results
Table 1 shows the patient characteristics and unadjusted outcomes in the two study groups. All patients in the study had a stage III or IV oropharyngeal squamous cell cancer and were similar in respect to age and baseline performance status. Compared with patients in the first group, more patients in the NP-led clinic group had stage IV cancer and tonsillar cancer (p = 0.051 and 0.02, respectively). It should be noted that both groups received the same treatment regimen, with the exception of a weekly supportive care clinic provided to patients in the second group.
Table 1.
Sample Characteristics by Study Croup (N =101)
| Characteristic | Pre NP-Led Clinic (n = 50)
|
Post NP-Led Clinic (n = 51)
|
p | ||
|---|---|---|---|---|---|
| X̄ | SD | X̄ | SD | ||
| Age (years) | 53.9 | 5.9 | 55.8 | 5.3 | 0.09 |
| Number of clinic visits | 3.4 | 1.4 | 6 | 1 | < 0.001 |
| Days to new patient contact | 8.5 | 6 | 10.2 | 6.4 | 0.19 |
| Characteristic | n | n | p |
|---|---|---|---|
| Tumor stage | 0.05 | ||
| III | 8 | 2 | |
| IV | 42 | 49 | |
| Primary tumor location | 0.02 | ||
| Tonsil | 17 | 31 | |
| Base of tongue | 24 | 17 | |
| Other | 9 | 3 | |
| Patient outcomesa | |||
| Toxicity-related hospitalization | 14 | 6 | 0.04 |
| Chemotherapy dose reduction | 24 | 3 | < 0.001 |
| Chemotherapy treatment completion | 23 | 46 | < 0.001 |
More than one answer was passible.
NP—nurse practitioner
Compared with patients in Group 1, patients treated since the initiation of the NP-led clinic had significantly lower rates of hospitalization for toxicity (28% versus 12%) and chemotherapy dose reductions (48% versus 6%). Ninety percent of patients treated after clinic initiation completed all seven planned cycles of chemotherapy, compared with 46% in the first group. Table 2 shows the results from the logistic regression models that estimate the likelihood of hospitalization, dose reduction, and treatment completion. All three adjusted models include age, stage, and tumor location as covariates. Compared with patients treated before the NP-led clinic, patients treated after the weekly NP-led supportive care clinic had a significantly lower incidence of hospitalization and dose reduction. Patients treated in the NP-led clinic also were more likely to complete all seven cycles of planned chemotherapy, compared with those treated prior to clinic initiation.
Table 2.
Patient Outcomes Associated With Weekly NP-Led Supportive Care Clinic
| Outcome | Odds Ratio | 95% CI | p |
|---|---|---|---|
| Hospitalization | |||
|
| |||
| NP-led clinic versus non NP-led | |||
| Unadjusted | 0.34 | [0.12, 1.01] | 0.05 |
| Adjusted | 0.27 | [0.08, 0.87] | 0.03 |
|
| |||
| Chemotherapy dose reduction | |||
|
| |||
| NP-led clinic versus non NP-led | |||
| Unadjusted | 0.7 | [0.02, 0.25] | < 0.001 |
| Adjusted | 0.7 | [0.02, 0.26] | < 0.001 |
|
| |||
| Chemotherapy treatment completion | |||
|
| |||
| NP-led clinic versus non NP-led | |||
| Unadjusted | 10.8 | [3.6, 32.5] | < 0.001 |
| Adjusted | 15.2 | [4.4, 52.5] | < 0.001 |
CI—confidence interval; NP—nurse practitioner
Note. Results from unadjusted and adjusted logistic regression analysis.
Adjusted analyses control for age, stage, and site.
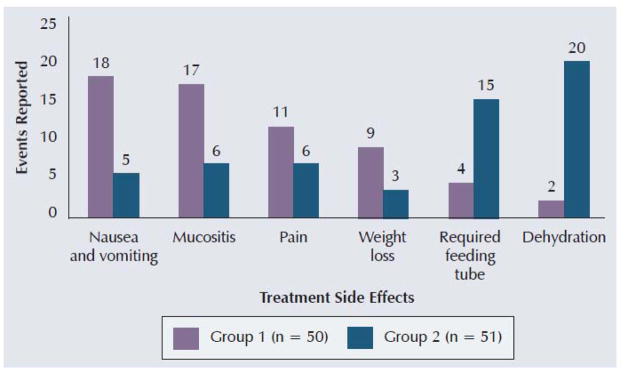
Finally, the authors examined the frequency of toxicities during the seven-week time period (see Figure 1). Because of the relatively small number of events considered, inferential statistics were not calculated. However, the frequency of nausea and vomiting, mucositis, and generalized pain were lower in the NP-led supportive care clinic group. Conversely, dehydration and placement of feeding tubes were reported more frequently in the NP-led clinic group.
Figure 1.
Frequency of Toxicities Reported by Group
Discussion
Patients receiving concurrent chemoradiotherapy for head and neck cancer have significant side effects that threaten to limit their ability to complete the treatment course without interruptions or dose reductions. Wells et al. (2008) has shown that a nurse specialist can help to manage symptoms during radiotherapy for head and neck cancer. Although the literature supports the need for these patients to be treated in an aggressive, multidisciplinary fashion (Mallick & Waldron, 2009; Murphy, 2009), NP-led symptom management clinics have not been used.
As seen in the results of this retrospective study, weekly visits with an oncology NP appears to be associated with improved chemotherapy completion as well as reduced hospitalization rates and chemotherapy dose deviations in patients receiving intensive chemoradiotherapy for oropharyngeal cancer. Anecdotally, patients also expressed satisfaction in the weekly clinic and the supportive care they received. These findings may translate to cost reductions with fewer hospitalizations as well as the ability for patients to successfully complete their entire course of treatment, allowing for better tumor control. Symptoms common in the first group decreased in the NP-led clinic group; however, more patients were identified as dehydrated and more feeding tubes were placed. This may be explained by earlier diagnoses of nutritional and hydration deficits in these patients, allowing for more aggressive follow-up.
Patients seen in the weekly NP clinic had blood drawn, often signaling possible dehydration with an elevated creatinine and blood urea nitrogen or possibly malnutrition with low protein and albumin levels. History and physical examination concentrated on weight loss, ability to eat, complaints of dizziness, or feelings of lightheadedness. Feeding tubes were placed based on the patient’s ability to maintain adequate nutrition as established by a registered dietitian. The goal was to place the feeding tube before excessive weight loss occurred. The patient’s ability to remain active also was used in determining the need for supplemental feedings.
One motivation to establish the NP-led clinic was to free up time for the medical oncologist to evaluate new patients. The authors compared the number of days from receipt of referral to scheduled appointment with the oncologist. Across the sample, the mean number of days to a new patient visit was 10.2 in the NP-led clinic and 8.5 days in the non–NP-led clinic. This difference was not statistically significant in the adjusted analysis (p = 0.14). Therefore, the authors cannot conclude that any difference exists between the two clinics in access to care for incoming patients.
Although the authors did not directly compare costs, average costs from the institution for the care provided to these patients suggest the NP-led clinic may confer efficiency. An average of 2.6 more clinic visits took place in the NP-led clinic. However, the cost of a 2–3 day hospitalization stay with IV hydration and antiemetics is about $8,729. An NP outpatient visit is $85, and an outpatient infusion appointment for IV hydration and antiemetics is about $112.
Additional prospective studies of cost effectiveness, patient satisfaction, improved toxicity management, and eventual tumor outcomes are needed to expand on this research. A prospective study could include randomization to weekly versus every other week clinic visits controlling for age and tumor stage. The inclusion of additional covariates such as performance status, baseline weight, and nutritional status may increase the ability to risk-adjust patient outcomes. Assessment of patient and caregiver or spouse satisfaction would enable assessment of patient-centered care.
Limitations
A retrospective design, which included chart review for two separate time frames, has the risk of intervening variables that are not controlled. For example, a change in an antiemetic regimen from one time period to the next could influence the outcome. A prospective study would allow the ability to evaluate more variables related to cost effectiveness, such as the percentage of patients who require IV hydration and the duration of this treatment. The number of patients who require enteral feeding tubes and the costs associated with this care also could be assessed. This would enable the authors to more accurately evaluate cost effectiveness, tumor outcome, and patient satisfaction. In addition, an assessment of patient and caregiver or spouse satisfaction would help to document the unique role that NPs play in the care of patients with cancer. Nurses have historically excelled in the area of patient-centered care, focusing on physical, psychological, and spiritual needs of patients and caregivers. Another limitation of this study would be the relatively small sample size and lack of sample size estimation.
Conclusions
NPs are in a position to advance their practice while improving patient care, particularly in oncology where the expertise of NPs in the area of symptom management gives them a clear advantage. This study illustrates the importance of symptom management for patients receiving chemoradiotherapy for oropharyngeal cancers. Although nurses always have been diligent about symptom management for patient comfort, controlling symptoms also can decrease costs and improve overall outcomes for patients. NPs are encouraged to demonstrate their value as it relates to cost containment as well as the provision of quality patient care. This study adds to the body of literature addressing this timely topic and provides a focus for additional study.
Acknowledgments
The authors gratefully acknowledge Christopher R. Friese, PhD, RN, AOCN®, FAAN, and Peg Esper, DNP(c), ANP-BC, AOCN®, for their mentorship, without which this project and study could not have been completed.
Contributor Information
Heidi Mason, The University of Michigan Medical Center in Ann Arbor.
Mary Beth DeRubeis, The University of Michigan Medical Center in Ann Arbor.
Jared C. Foster, The Biostatistics and Bioinformatics Branch of the Division of Intramural Population Health Research at the Eunice Kennedy Shriver National Institute of Child Health and Human Development in Bethesda, MD.
Jeremy M.G. Taylor, Biostatistics at the University of Michigan School of Public Health.
Francis P. Worden, The Hematology/Oncology Fellowship Program at the University of Michigan Health System in Ann Arbor.
References
- Argiris A, Karamouzis MV, Raben D, Ferris RL. Head and neck cancer. Lancet. 2008;371:1695–1709. doi: 10.1016/S0140-6736(08)60728-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bensinger W, Schubert M, Ang K, Brizel D, Brown E, Eilers J, … Trotti A. NCCN task force report: Prevention and management of mucositis in cancer care. Journal of the National Comprehensive Cancer Network. 2008;6(Suppl 1):S1–S21. [PubMed] [Google Scholar]
- Hinkel J, Vandergrift J, Perkel S, Waldinger M, Levy W, Stewart M. Practice and productivity of physician assistants and nurse practitioners in outpatient oncology clinics at National Comprehensive Cancer Center Network institutions. Journal of Oncology Practice. 2010;6(4):182–187. doi: 10.1200/JOP.777001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mallick I, Waldron J. Radiation therapy for head and neck cancers. Seminars in Oncology Nursing. 2009;25:193–202. doi: 10.1016/j.soncn.2009.05.002. [DOI] [PubMed] [Google Scholar]
- McCorkle R, Dowd M, Ercolano E, Schulman-Green D, Williams AL, Siefert ML, … Schwartz P. Effects of a nursing intervention on quality-of-life outcomes in post-surgical women with gynecological cancers. Psycho-Oncology. 2009;18:62–70. doi: 10.1002/pon.1365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy B. Advances in quality of life and symptom management for head and neck cancer patients. Current Opinion in Oncology. 2009;21:242–247. doi: 10.1097/CCO.0b013e32832a230c. [DOI] [PubMed] [Google Scholar]
- National Cancer Institute. Common Terminology Criteria for Adverse Events (CTCAE), version 4.0. 2010 Retrieved from http://evs.nci.nih.gov/ftp1/CTCAE/About.html.
- Newhouse RP, Stanik-Hutt J, White KM, Johantgen M, Bass EB, Zangaro G, … Weiner JP. Advanced practice nurse outcomes 1990–2008: A systematic review. Nursing Economic$ 2011;29(5):230–250. [PubMed] [Google Scholar]
- Nonzee N, Dandade NA, Markossian T, Agulnik M, Argiris A, Patel J, … Bennett CL. Evaluating the supportive care costs of severe radiochemotherapy-induced mucositis and pharyngitis. Results from a Northwestern University Costs of Cancer Program pilot study with head and neck and non-small cell lung cancer patients who receive care at a county hospital, a Veterans Administration hospital, or a comprehensive cancer care center. Cancer. 2008;113:1446–1452. doi: 10.1002/cncr.23714. [DOI] [PubMed] [Google Scholar]
- Takes RP, Strojan P, Silver CE, Bradley PJ, Haigentz M, Wolf GT, … Ferlito A. Current trends in initial management in hypopharyngeal cancer: The declining use of open surgery. Head and Neck. 2012;34:270–281. doi: 10.1002/hed.21613. [DOI] [PubMed] [Google Scholar]
- Wells M, Donnan PT, Sharp L, Ackland C, Fletcher J, Dewar JA. A study to evaluate nurse-led on-treatment review for patients undergoing radiotherapy for head and neck cancer. Journal of Clinical Nursing. 2008;17:1428–143. doi: 10.1111/j.1365-2702.2007.01976.x. [DOI] [PubMed] [Google Scholar]