Abstract
Stroke is a leading cause of serious long-term disability worldwide. Functional outcome depends on stroke location, severity, and early intervention. Conventional rehabilitation strategies have limited effectiveness, and new treatments still fail to keep pace, in part due to a lack of understanding of the different stages in brain recovery and the vast heterogeneity in the poststroke population. Innovative methodologies for restorative neurorehabilitation are required to reduce long-term disability and socioeconomic burden. Neuroplasticity is involved in poststroke functional disturbances and also during rehabilitation. Tackling poststroke neuroplasticity by non-invasive brain stimulation is regarded as promising, but efficacy might be limited because of rather uniform application across patients despite individual heterogeneity of lesions, symptoms, and other factors. Transcranial direct current stimulation (tDCS) induces and modulates neuroplasticity, and has been shown to be able to improve motor and cognitive functions. tDCS is suited to improve poststroke rehabilitation outcomes, but effect sizes are often moderate and suffer from variability. Indeed, the location, extent, and pattern of functional network connectivity disruption should be considered when determining the optimal location sites for tDCS therapies. Here, we present potential opportunities for neuroimaging-guided tDCS-based rehabilitation strategies after stroke that could be personalized. We introduce innovative multimodal intervention protocols based on multichannel tDCS montages, neuroimaging methods, and real-time closed-loop systems to guide therapy. This might help to overcome current treatment limitations in poststroke rehabilitation and increase our general understanding of adaptive neuroplasticity leading to neural reorganization after stroke.
Keywords: tDCS, non-invasive brain stimulation, transcranial current stimulation, multichannel stimulation, neuroimaging, near-infrared spectroscopy
Introduction
Although spontaneous poststroke recovery occurs, between 15% and 30% of stroke survivors are left permanently disabled (1). Poststroke rehabilitation helps relearn skills that are lost when part of the brain is damaged. As an adjunct therapy, non-invasive brain stimulation (NIBS) techniques, including repetitive transcranial magnetic stimulation (rTMS) and transcranial current stimulation (tCS) – particularly direct current stimulation (tDCS) – are promising approaches to enhance the effects of standardized rehabilitation treatments in selected poststroke patients. Like rTMS, tDCS can alter cortical excitability in predictable ways. tDCS is characterized as neuromodulatory rather than neurostimulatory, since the currents delivered during tDCS are not sufficient to directly generate action potentials. tDCS-induced excitability alterations depend on the duration, current density, and direction of the current flow. Generally, anodal tDCS (a-tDCS) enhances excitability, while cathodal tDCS (c-tDCS) reduces it (2–4). Whereas after-effects of single stimulation sessions are in the time range of early-phase long-term potentiation and long-term depression (~1 h), repetitive stimulations with certain intervals can induce late-phase effects lasting longer than 24 h after intervention (3–6). tDCS is a well-tolerated technique, easily applied over cortical targets leading to adaptive neural reorganization and the reduction in maladaptive plasticity during behavioral treatment. Further, tDCS is less expensive and likely to be better accepted by patients than rTMS (7, 8), making it potentially well poised for home therapy.
Currently, the need to target not an isolated cortical region, but several functionally correlated cortical hubs involved in larger scale intrinsic brain networks is becoming increasingly recognized (9, 10). Advances in neuroimaging technology, such as functional magnetic resonance imaging (fMRI), diffusion tensor imaging, electroencephalography (EEG), and functional near-infrared spectroscopy (fNIRS), are allowing us to non-invasively visualize and quantify brain network connectivity in humans with increasing accuracy. Recently, we showed how the optimal electrode configuration of a multichannel tDCS system can be determined by using neuroimaging data to specify a target map on the cortical surface for excitatory or inhibitory stimulation (11). Multichannel tDCS is a new approach highly capable of efficiently targeting distributed brain networks to facilitate beneficial neuroplasticity and functional connectivity leading to poststroke recovery.
Portable neuroimaging solutions, such as EEG and fNIRS, can objectively capture individual brain states poststroke, which can be used to customize and adapt NIBS in real time to facilitate training (12, 13). An EEG–fNIRS-based method (14) was recently proposed for screening and monitoring of neurovascular coupling functionality in combination with tDCS. In this system, neuronal and hemodynamic responses were abstractly represented as feedback for tDCS effects. Such innovative portable EEG–fNIRS neuroimaging systems could be used to objectively guide and quantify the progress of a tDCS treatment regime in conjunction with neurorehabilitation. Moreover, system identification and parameter estimation techniques using neuronal and hemodynamic responses to tDCS can be used to track the effects, e.g., on corticospinal excitability, for closed-loop control of tDCS. Poststroke integrity of task-specific ipsilesional and/or contralesional neural pathways can be determined with EEG–fNIRS neuroimaging during task performance, which can be leveraged toward the optimization of subject-specific tDCS. The goal may be to correlate functional outcome with regard to EEG–fNIRS brain activation patterns as a marker of the underlying task-specific residual activation such that those residual brain activation patterns are facilitated with individualized brain state-dependent multichannel tDCS as an adjunct treatment during stroke rehabilitation.
Here, we introduce the potential of these two methods (11, 14) to optimize future multichannel tDCS systems for modulation of excitability of brain networks, represented by spatially extended cortical targets. Combining both models closely addresses the individual determinants of patterns of neuroplastic changes both to guide tDCS treatment and to assess functional recovery. We present potential novel application opportunities based on guided multichannel tDCS in poststroke rehabilitation. Likewise, we show how multimodal approaches pairing neuroimaging and electrophysiological measures with therapeutic tDCS can extend its potential in aiding customized and personalized long-term rehabilitation strategies, including post-acute rehabilitation after stroke.
tDCS-Based Poststroke Neurorehabilitation
Poststroke functional recovery depends on the degree of adaptive neuroplasticity in central nervous system reorganization. Adaptive neuroplasticity includes changes in synaptic connectivity and excitability in surviving neural cell population in the perilesional zone, in remote structures, and in the contralateral unaffected hemisphere in case of a mono-hemispheric lesion (15, 16). In particular, mono-hemispheric stroke is thought to result in disinhibition of the contralesional unaffected hemisphere due to release from transcallosal inhibition. This may exert an inhibitory influence on perilesional areas, negatively affecting spontaneous neuroplasticity and interfering with the ability of perilesional areas to contribute to functional recovery – with the exception of particular cases with extensive stroke lesions. This interhemispheric inhibition model provides the rationale for facilitatory stimulation of the peri-stroke areas (hypoactive cortical regions), and suppression of the contralesional hemispheric hyperactivity with NIBS in order to enhance functional performance in poststroke patients (17). Further, a recent bimodal balance-recovery model links interhemispheric balancing and functional recovery to the structural reserve spared by the stroke lesion (18). This new concept raises the question about optimal localizations and number of positions to be stimulated with tDCS.
Some meta-analyses evaluated the efficacy of tDCS on poststroke rehabilitation for limb motor impairments, impaired balance, hemineglect, aphasia, and dysphagia. In Table 1, we summarize studies extracted from recent meta-analyses and systematic reviews that satisfy the following four criteria. They were randomized controlled trials (RCTs) or randomized cross-over trials (with sham controls), with mono-hemispheric poststroke adult patients (no chronicity limits), that received tDCS combined with standardized therapy, and reported outcome measures.
Table 1.
Summary of tDCS-based poststroke neurorehabilitation studies.
| Study |
Study design |
Parameters of stimulation |
Location |
Combined therapy |
Effect (+/Nd) |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Reference | Subjects | Stroke phase | Stimulation | Current intensity, current density | Duration day (min) | Num. sessions | Target electrode region | Reference region | Therapy type | Online/offline | A+/B+/C+/S+ |
| Upper limb motor impairment | |||||||||||
| Bolognini et al. (19) | 14 | Chr. | B/S | 2 mA, 0.057 mA/cm2 | 40 | 10 | A: affected M1, C: unaffected M1 | Unaffected M1 | Constraint-induced movement therapy | Online | B+ motor performance |
| Celnik et al. (20) | 9 | Chr. | A/S | 1 mA, 0.11 mA/cm2 | 20 | 4 | Affected M1 (abductor pollicis brevis muscle hot-spot) | Contralateral supraorbital area | Peripheral nerve stimulation | Offline | A+ |
| Di Lazzaro et al. (21) | 20 | Acu. | B/S | 2 mA, 0.057 mA/cm2 | 40 | 5 | A: affected M1, C: unaffected M1 (abductor pollicis brevis muscle hot-spot) | Unaffected M1 | Constraint-induced movement therapy | Online | Nd – but B reduces II |
| Fregni et al. (22) | 6 | Chr. | A/C/S | 1 mA, 0.028 mA/cm2 | 20 | 3 | A: affected M1, C: unaffected M1 (first dorsal interosseous muscle hot-spot) | Contralateral supraorbital area | JTT | Online | A+; C+ |
| Fusco et al. (23) | 11 | Acu. | C/S | 1.5 mA, 0.043 mA/cm2 | 10 | 10 | Unaffected M1 | Right shoulder | Traditional motor rehabilitation | Offline | Nd |
| Hesse et al. (24) | 96 | Acu. Sub. | A/C/S | 2 mA, 0.057 mA/cm2 | 20 | 30 | A: affected M1, C: unaffected M1 | Contralateral supraorbital area | Robotic arm training | Online | A+; C+ |
| Khedr et al. (25) | 40 | Sub. | A/C | 2 mA, 0.057 mA/cm2 | 25 | 6 | A: affected M1, C: unaffected M1 | Contralateral supraorbital area | Inpatient daily rehabilitation | Offline | A+; C+ |
| Kim et al., 2009 (26) | 10 | Sub. | A/S | 1 mA, 0.04 mA/cm2 | 20 | 2 | Affected M1 (first dorsal interosseous muscle hot-spot) | Contralateral supraorbital area | Box and block test; Finger acceleration | Online | A+ |
| Kim et al. (27) | 18 | Sub. | A/C/S | 2 mA, 0.08 mA/cm2 | 20 | 10 | A: affected M1, C: unaffected M1 (first dorsal interosseous muscle hot-spot) | Contralateral supraorbital area | Conventional occupational therapy | Online | C+ |
| Lefebvre et al. (28) | 18 | Chr. | B/S | 1 mA, 0.028 mA/cm2 | 30 | 2 | A: affected M1 (hand muscle hot-spot) | C: unaffected M1 (hand muscle hot-spot) | Motor skill learning task | Online | B+ |
| Lefebvre et al. (29) | 19 | Chr. | B/S | 1 mA, 0.028 mA/cm2 | 30 | 2 | A: affected M1 (hand muscle hot-spot) | C: unaffected M1 (hand muscle hot-spot) | Motor skill learning task | Online | B+ |
| Lindenberg et al. (30) | 20 | Chr. | B/S | 1.5 mA, 0.092 mA/cm2 | 30 | 5 | A: affected M1 | C: unaffected M1 | Conventional physical and occupational therapy | Online | B+ |
| Mortensen et al. (31) | 15 | Chr. | A/S | 1.5 mA, 0.04 mA/cm2 | 20 | 5 | Affected M1 | Contralateral supraorbital area | Conventional occupational therapy | Online | A+ |
| Nair et al. (32) | 14 | Chr. | C/S | 1 mA/? | 30 | 5 | Unaffected M1 | Contralateral supraorbital area | Conventional occupational therapy | Online | C+ |
| Rocha et al. (33) | 21 | Chr. | A/C/S | 2 mA, 0.057 mA/cm2 | A: 13 C: 9 | 12 | A: affected M1, C: unaffected M1 | Contralateral supraorbital area | Constraint-induced movement therapy (modified) | Offline | A+; C+ |
| Triccas et al. (34) | 23 | Sub. Chr. | A/S | 1 mA, 0.028 mA/cm2 | 20 | 18 | Affected M1 | Contralateral supraorbital area | Robotic therapy | Online | Nd |
| Viana et al. (35) | 20 | Chr. | A/S | 2 mA, 0.057 mA/cm2 | 13 | 15 | Affected M1 | Contralateral supraorbital area | Virtual reality therapy | Offline | Nd (A+; S+) |
| Wu et al. (36) | 90 | Sub. Chr. | C/S | 1.2 mA, 0.26 mA/cm2 | 20 | 20 | Affected primary sensorimotor cortex | Unaffected shoulder | Conventional physical therapy | Offline | C+ |
| Lower limb motor impairment and poor balance | |||||||||||
| Chang et al. (37) | 24 (12/12) | Acu. | A/S | 2 mA, 0.28 mA/cm2 | 10 | 10 | Affected tibialis anterior muscle hot-spot | Contralateral supraorbital area | Conventional physical therapy | Online | A+ |
| Madhavan et al. (38) | 9 | Chr. | A/S | 0.5 mA, 0.06 mA/cm2 | 15 | 3 | Unaffected and affected lower limb primary motor cortex | Contralateral supraorbital area | Tracking task sinusoidal waveform | Online | A+ |
| Sohn et al. (39) | 11 | Sub. | A/S | 2 mA, 0.08 mA/cm2 | 10 | 2 | Affected quadriceps femoris muscle hot-spot | Contralateral supraorbital area | Standard rehabilitation | Offline | A+ |
| Tanaka et al. (40) | 8 | Chr. | A/S | 2 mA, 0.057 mA/cm2 | 10 | 2 | Affected tibialis anterior muscle hot-spot | Contralateral supraorbital area | Knee extension task | Online | A+ |
| Hemineglect | |||||||||||
| Ko et al. (41) | 15 | Sub. | A/S | 2 mA, 0.08 mA/cm2 | 20 | 2 | Right PPC | Contralateral supraorbital area | No | Offline | A+ |
| Làdavas et al. (42) | 30 | Sub. Chr. | A/C/S | 2 mA, 0.057 mA/cm2 | 20 | 10 | A: right PPC C: left PPC | Contralateral supraorbital area | Prism adaptation treatment | Online | A+ > C+ |
| Sparing et al. (43) | 10 | Sub. Chr. | A/C/S | 1 mA, 0.04 mA/cm2 | 10 | 3 | A: right PPC and left PPC, C: left PPC | Cz | No | Offline | A+ over r-PPC; C+ |
| Sunwoo et al. (44) | 10 | Sub. Chr. | A/B/S | 1 mA, 0.04 mA/cm2 | 20 | 3 | A: right PPC, C: left PPC | Contralateral supraorbital area | No | Offline | B+ > A+ |
| Aphasia | |||||||||||
| Fiori et al. (45) | 7 | Chr. | A/S | 1 mA, 0.028 mA/cm2 | 20 | 10 | Broca’s and Wernicke’s area | Contralateral frontopolar cortex | Video naming | Online | A+ |
| Flöel et al. (46) | 12 | Chr. | A/C/S | 1 mA, 0.028 mA/cm2 | 40 | 3 | Right temporo-parietal cortex | Contralateral supraorbital area | Picture naming | Online | A+ > C+ |
| Kang et al. (47) | 10 | Chr. | C/S | 2 mA, 0.08 mA/cm2 | 20 | 5 | Right Broca’s homolog | Contralateral supraorbital area | Picture naming | Online | C+ |
| Marangolo et al. (48) | 8 | Chr. | B/S | 2 mA, 0.057 mA/cm2 | 20 | 10 | A: Broca’s area | C: right Broca’s homolog | Word repetition training | Online | B+ |
| Monti et al. (49) | 9 | Chr. | A/C/S | 2 mA, 0.057 mA/cm2 | 10 | 10 | Broca’s area | Right shoulder | Picture naming | Online | C+ |
| You et al. (50) | 21 | Sub. | A/C/S | 2 mA, 0.057 mA/cm2 | 30 | 10 | A: Wernicke’s area, C: right Wernicke’s homolog | Contralateral supraorbital area | Auditory verbal comprehension | Offline | C+ > A+ |
| Dysphagia | |||||||||||
| Kumar et al. (51) | 14 | Sub. | A/S | 2 mA, 0.13 mA/cm2 | 30 | 5 | Unaffected swallowing motor cortex | Contralateral supraorbital area | SSM | Online | A+ |
| Shigematsu et al. (52) | 20 | Chr. | A/S | 1 mA, 0.028 mA/cm2 | 20 | 10 | Affected pharyngeal motor cortex | Contralateral supraorbital area | SSM | Online | A+ |
| Yang et al. (53) | 14 | Sub. | A/S | 1 mA, 0.04 mA/cm2 | 20 | 10 | Affected pharyngeal motor cortex | Contralateral supraorbital area | SSM | Online | A+ only after follow-up |
Studies have been extracted from recent meta-analyses following aforementioned criteria.
+, improves the effect on task performance after tDCS intervention; ?, not mentioned; A, a-tDCS; Acu., acute; B, bilateral a- and c-tDCS; C, c-tDCS; Chr., chronic; II, interhemispheric imbalance; JTT, Jebsen–Taylor Hand Function Test; M1, primary motor cortex; Nd, no differences; PPC, posterior parietal cortex; S, sham-tDCS; SSM, standardized swallowing maneuvers; Sub., subacute.
Upper Limb Motor Impairment
More than 50% of stroke survivors exhibit some degree of motor impairment and require partial assistance in activities of daily living (ADL). Restriction of the upper limb motor function can limit ADL performance, directly influencing quality-of-life. Most tDCS interventional trials with poststroke patients with arm and hand impairments showed favorable results on upper limb motor function (Table 1), influencing muscle strength (31) and muscle tone (36), too. Yet, combination of tDCS with robotic (34) or virtual reality therapy (35) was not found to improve the effect of recovery outcome. According to some systematic reviews (54–56), the effectiveness of tDCS on upper limb motor function varies, showing only small to moderate effects. A dose–response relationship was observed (57) between upper extremity motor recovery and application of tDCS dependent on electrode size, charge density, and current density.
Lower Limb Motor Impairment and Poor Balance
Gait impairment includes speed, endurance, and stability. About 57–63% of stroke survivors cannot walk independently at symptom onset and 22–50% after gait rehabilitation (58). Most studies using NIBS focused on the recovery of the paretic upper extremity rather than on the recovery of lower limb function and balance. This might be due to functional and anatomical limitations, since the lower limb motor cortex and the cerebellum may not be easily reached by NIBS techniques. Nevertheless, some studies demonstrated that tDCS protocols are able to enhance lower limb motor function (37, 38), motor cortex excitability (37), and muscle strength (39, 40) (Table 1). Considering balance impairment, static postural stability was observed to significantly improve after tDCS (39, 59). Some studies have investigated the effect of cerebellar tDCS on balance in healthy subjects and neurological patients (e.g., Parkinson), but no study so far evaluated the effects of cerebellar tDCS on poor balance in poststroke patients.
Hemineglect
Patients suffering from hemineglect do not attend or respond to information on the contralesional side of space (60). Several studies indicate that poststroke hemineglect constitutes a predictive factor of poor functional prognosis (61–63). In recent studies of hemineglect rehabilitation (16), tDCS was applied to either facilitate the right (affected) or suppress the left (unaffected) posterior parietal cortex (PPC) activation, based on the aforementioned interhemispheric inhibition model. Accordingly, a-tDCS over the right PPC was shown to improve hemineglect rehabilitation (41–44) and c-tDCS over the left PPC to reduce hemineglect symptoms (43). Further, bilateral tDCS is considered to induce stronger effects (44) (Table 1).
Aphasia
Even after speech and language therapy, 12% of poststroke survivors are left with some degree of chronic communication deficit (64–66). Following the model of interhemispheric inhibition, c-tDCS over right-hemispheric Broca’s homolog was demonstrated to significantly improve naming accuracy (47). Bihemispheric a-tDCS over left Broca’s area and c-tDCS over right Broca’s homolog was suggested to improve recovery in different language tasks (48). In contrast, a-tDCS over the right temporoparietal cortex was shown to stronger enhance the overall training effect in naming ability in comparison to c-tDCS (46). These and other tDCS trials [(45–50), Table 1] were evaluated in a meta-analysis (67) showing a moderate, but non-significant, pooled size effect favoring tDCS. This might be due to heterogeneity among study protocols and insufficient numbers of study subjects, since all trials favored tDCS. When pooling rTMS and tDCS studies that suppress activation of right-hemispheric homologous language regions, a significant effect of the intervention was identified (68).
Dysphagia
At least one out of two stroke patients experiences swallowing problems (69, 70) or dysphagia, which is potentially fatal. Recently, two meta-analyses (71, 72) have independently evaluated the effects of NIBS (rTMS and tDCS) on dysphagia with the aim to encourage more efficient rehabilitation techniques. Both meta-analyses included the same three tDCS studies (51–53). All three studies used a-tDCS, but two studies stimulated the affected hemisphere (52, 53), whereas one study stimulated the unaffected hemisphere (51) (Table 1). There was a moderate, but non-significant, pooled size effect favoring tDCS intervention vs. sham-tDCS. When pooling rTMS and tDCS studies together, a meta-analysis (71) found that stimulating the unaffected hemisphere improved swallowing significantly. Bilateral tDCS – though not explored so far – might be especially attractive for dysphagia therapy because swallowing is bilaterally innervated.
Multichannel tDCS for Distributed Cortical Targets
Heterogeneous statements about efficacy of tDCS are highly likely to be due to the variability of study protocols and the limited number of participants. Stroke is a heterogeneous disease with regard to lesion size and location requiring customized rehabilitation strategies to result in optimal effects. Here, we present methods to tackle this issue, such as a methodological tool for optimizing multichannel tDCS montages and efficiently targeting complex, distributed cortical areas (11). With a constraint on the maximal number of electrodes and currents, an optimal multichannel tDCS montage solution (electrode currents and locations) can be obtained by using neuroimaging data. The present implementation of this method (Stimweaver) relies on the fast calculation of multichannel tDCS electric fields (including components normal and tangential to the cortical boundaries) using a five-layer finite element model of a realistic head (73). Solutions are found using constrained least squares to optimize current intensities, with electrode number and location selected using a genetic algorithm.
A key aspect is the definition of the problem to be optimized. This is done by specifying two cortical surface maps. The first map provides a target electric field – in the form of the electric field component normal to the cortical surface – at each location (e.g., En = −0.25 V/m in region 1 and En = +0.25 V/m in region 2). Our current understanding of the effects of tDCS focuses on the orientation of the electric field in relation to the orientation of neurons, and in particular, pyramidal neurons in the cortex (11, 74). Based on the approximation that the effects of current stimulation are due to the linear interaction of electric fields with populations of elongated cortical neurons, we argue that the optimization problem for tDCS can be defined in terms of the component of the electric field orthogonal to the cortical surface (generally, the same methodology and logic applicable to TMS). According to this model, “inward” directed fields are excitatory and “outward” directed fields inhibitory. This (signed) target map may specify several discrete areas or just a continuous function. The second map is a cortical weight map taking positive values, specifying the importance of each target area with a weight. This methodology is particularly appropriate for the neuromodulation of cortical (distributed) networks. In the following sections, we provide two examples of the application of this methodology to the case for poststroke network modulation.
Multichannel tDCS for Poststroke Lower Limb Motor Rehabilitation
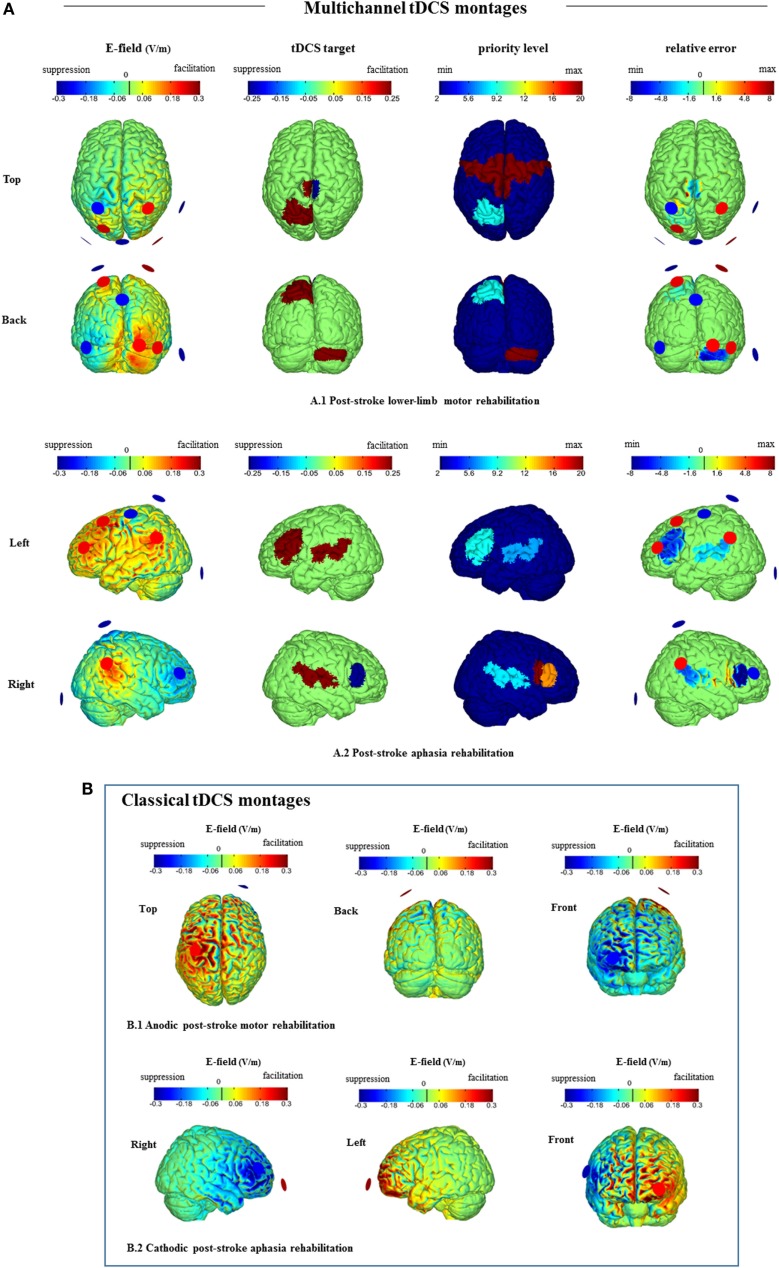
For development of multichannel tDCS on a rational basis, identification of areas relevant for rehabilitation of motor function after stroke is crucial. Following recent longitudinal studies after stroke, Figure 1A.1 targets at tDCS-induced facilitatory activity on the ipsilesional primary sensorimotor cortex (75, 76) and on contralesional cerebellum (77), which are areas associated with functional improvement. Based on a recent review (8), we also aim to upregulate excitability of ipsilesional M1 and to downregulate excitability of contralesional M1 (Figure 1A.1). For the premotor cortex (PMC), some functional brain-imaging studies have demonstrated increased activation of the ipsilesional area during movement of the affected limb after stroke (78). This activity improvement might however be dysfunctional, since the inhibitory function of the PMC was found disturbed in stroke patients with poor motor function (79). Takeuchi et al. (80) hypothesized that disinhibition of the ipsilesional PMC causes a dysbalanced activity distribution of motor cortex proximal limb representations, which results in a proximal-dominant competitive interaction between ipsilesional M1 and PMC. This widespread maladaptive activity will result in poor control of the paretic distal parts of the limb in stroke patients. To avoid such widespread disinhibition of motor-related areas that may lead to maladaptive plasticity, we attributed a high priority to “no stimulation” of the PMC in the first row of Figure 1.
Figure 1.
Stimweaver simulations for (A) guided multichannel tDCS montages vs. (B) classical tDCS montages. (A) Multichannel tDCS representations for distributed cortical targets for (A.1) poststroke lower limb motor rehabilitation (top and back views, see Multichannel tDCS for Poststroke Lower Limb Motor Rehabilitation) and (A.2) poststroke aphasia rehabilitation (left and right views, see Multichannel tDCS for Poststroke Aphasia Rehabilitation). Optimal solution using eight Neuroelectrics Pistim circular electrodes (1 cm radius and Ag/Cl). Total injected current 4 mA. Plots of the normal component of the E-field (V/m) (left), tDCS target region (center left), priority level (center right), and relative error (right) shown on the gray matter. In the left column, positive (red) colors reflect ingoing, excitatory normal electric fields (blue the opposite). In the second column, red areas denote targets to facilitate activation and blue to suppress activation. The third column colors reflect the importance (weight) of each area taking positive values up to 20. A dark blue cortical area reflects minimum/default priority and a red area maximum priority. In-between colors denote the corresponding intermediate priority. The last column provides a visual display of the match of electric fields solution to target [the relative error (10)]. Note that this model may not fit each poststroke patient with lower limb (A.1) or language (A.2) impairment because areas important for restitution are likely to be different according to lesion size and location (see Multichannel tDCS for Poststroke Lower Limb Motor Rehabilitation and Multichannel tDCS for Poststroke Aphasia Rehabilitation for details). (B) Plots of the normal component of the E-field (volts per meter) of classical tDCS montages for (B.1) anodic poststroke motor rehabilitation (top, back, and frontal views) and (B.2) cathodic poststroke aphasia rehabilitation (left, right, and frontal views). Solutions using two Neuroelectrics Pistim circular electrodes. Total injected current 2 mA. (B.1) Anodic stimulation over the M1 affected area: “active” electrode on C1 and cathode (return electrode) over the contralateral supraorbital area (38). (B.2) Cathodic stimulation over the right homolog of Broca’s area: “active” electrode on F6 and anode (return electrode) over the contralateral supraorbital area (47).
Multichannel tDCS for Poststroke Aphasia Rehabilitation
Recent neuroimaging studies on poststroke aphasia reveal neuroplastic cortical changes in both hemispheres, yet how the areas of the structural and functional language neural network contribute to language relearning success is still controversial (81). An optimized multichannel tDCS montage may allow us to facilitate and suppress activation of specifically selected language-relevant cortical areas (82, 83) aiming at individualizing optimal parameters for each poststroke aphasic patient in the near future. Figure 1A.2 presents the results of a generalized montage targeting those areas of the language network, in which tDCS had a beneficial effect on language functions in previous studies (Table 1). To improve naming ability, we target to suppress right pars triangularis activation over Broca’s homolog (47, 84), but try to minimize stimulation over the right pars opercularis (84). Further, we induce facilitatory tDCS over left Broca’s and Wernicke’s areas (45), and also over the right temporoparietal cortex (46).
Real-Time fNIRS–EEG Feedback for Multichannel tDCS
During neural activation, the electric currents from excitable membranes of brain tissue superimpose in the extracellular medium and generate a potential on the scalp (i.e., EEG). Neural activity has been shown to be closely related, spatially and temporally, to cerebral blood flow (CBF) that supplies glucose via neurovascular coupling. The hemodynamic response can be captured by fNIRS, which enables continuous monitoring of cerebral oxygenation and blood volume. This neurovascular coupling phenomenon led to the concept of the neurovascular unit (NVU), which consists of the endothelium, glia, neurons, pericytes, and the basal lamina. Recent work suggests NVU as an integrated system working in concert using feedback mechanisms to enable proper brain homeostasis and function. Capturing these mostly non-linear spatiotemporal interactions within NVU remains a challenge (85). The dynamic nature of functional connectivity may be in part due to spatiotemporal interactions between neuro- and hemodynamics. We postulate that fusing of EEG and fNIRS data provides a more robust real-time tracking of the dynamic functional connectivity during task performance. Further, multivariate machine learning methods (86) can be leveraged for fusing multimodal functional neuroimaging data.
In EEG and fNIRS, the sensors measuring brain activity are located outside of the head, thus a source space representation of the sensor readings (inverse problem) has to be inferred from a physical model that maps cortical (source) activity to the sensors (forward problem). MRI-based fast individualized quasistatic bioelectromagnetic forward simulations can be performed using open source software developed for EEG analysis [e.g., OpenMEEG (87)]. In the case of fNIRS, the MRI-based individualized physical model involves optical properties, such as absorption and scattering coefficients of different tissue types, and describes the photon transport through the tissue (88). Diffuse optical tomography (89) extends fNIRS by applying overlapping “high density” measurements, thus providing three-dimensional imaging with improved spatial resolution. In the source space, the multimodal (EEG–fNIRS) functional connectivity needs to be analyzed in real time for closed-loop control of multichannel tDCS.
Computational methods to investigate the dynamic functional connectivity in the source space can be developed based on prior works in fMRI–EEG (90, 91). Moreover, for motor tasks, sparse linear regression analysis has been shown to be well suited to reconstruct the electromyogram from human cortical activations using fMRI (92) and EEG (93). Thus, multichannel tDCS systems (11) can be optimized to target relevant cortical activations (source space) – related to functional connectivity hubs – found from EEG–fNIRS joint neuroimaging during task performance to facilitate poststroke rehabilitation (94). The real added value to the neuroimaging-guided multichannel tDCS paradigm is that EEG–fNIRS data can be used to individualize NIBS protocols not only based statically on the “hot spots” of beneficial neuroplasticity in a given patient but also to adjust stimulation protocols dynamically based on physiological feedback to approach optimal activation of the target regions in the time domain.
Conclusion
Transcranial direct current stimulation is a promising evolving adjunctive therapy in stroke rehabilitation based on enhancement of beneficial and reduction of maladaptive plasticity. However, the current state of the art suffers from relevant limitations, which hinder the full integration of tDCS methodology in clinical practice. First, small sample sizes, heterogeneity of samples (e.g., lesion type, poststroke severity, and time after stroke), and differences between stimulation protocols might be the main reasons for so far limited magnitude of tDCS effects and heterogeneity of results. Second, efficacy of stimulation might be relevantly limited by current restriction to stimulation of one or two target areas in most studies, not taking into account the complex networks involved in respective functions. Third, in a disease characterized by heterogeneous lesions, largely ignoring individual differences of lesion size, location, and baseline activation, as well as anatomical factors relevant for the efficacy of intervention, e.g., head size and brain anatomy, might furthermore limit the efficacy of current stimulation approaches. Larger controlled studies are necessary to determine the best parameters of stimulation (including the optimal cortical target locations) according to each subtype of stroke, the time course of stroke recovery, and individual factors. With the introduction of neuroimaging-guided multichannel tDCS protocols, most of these problems may be solved, and these approaches might relevantly help to determine the real potential of tDCS to improve clinical symptoms after stroke.
Author Contributions
BO, AD, AF, PM, MN, and GR have substantially contributed to the conception, design, and interpretation of data for this work. OR has substantially contributed to the analysis and simulations of this work. DE, AK, and TI have substantially contributed to the interpretation of data. All authors have also drafted the work and revised it critically with contribution related to author order. All authors have approved the final version prior to submission and are in agreement.
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Advancing Translational Science or the National Institutes of Health.
Conflict of Interest Statement
GR is co-owner of Neuroelectrics and Starlab and holds patents on multisite tCS. PM and MN are members of Neuroelectrics’ advisory board.
References
- 1.Asplund K, Stegmayr B, Peltonen M. From the twentieth to the twenty-first century: a public health perspective on stroke. In: Ginsberg MD, Bogousslavsky J, editors. Cerebrovascular Disease Pathophysiology, Diagnosis, and Management Vol. 2, Chapter 64. Malden, MA: Blackwell Science; (1998). p. 901–18. [Google Scholar]
- 2.Nitsche A, Paulus W. Excitability changes induced in the human motor cortex by weak transcranial direct current stimulation. J Physiol (2000) 527(Pt 3):633–9. 10.1111/j.1469-7793.2000.t01-1-00633.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nitsche MA, Paulus W. Sustained excitability elevations induced by transcranial DC motor cortex stimulation in humans. Neurology (2001) 57(10):1899–901. 10.1212/WNL.57.10.1899 [DOI] [PubMed] [Google Scholar]
- 4.Nitsche MA, Nitsche MS, Klein CC, Tergau F, Rothwell JC, Paulus W. Level of action of cathodal DC polarisation induced inhibition of the human motor cortex. Clin Neurophysiol (2003) 114(4):600–4. 10.1016/S1388-2457(02)00412-1 [DOI] [PubMed] [Google Scholar]
- 5.Monte-Silva K, Kuo MF, Liebetanz D, Paulus W, Nitsche MA. Shaping the optimal repetition interval for cathodal transcranial direct current stimulation (tDCS). J Neurophysiol (2010) 103(4):1735–40. 10.1152/jn.00924.2009 [DOI] [PubMed] [Google Scholar]
- 6.Monte-Silva K, Kuo MF, Hessenthaler S, Fresnoza S, Liebetanz D, Paulus W, et al. Induction of late LTP-like plasticity in the human motor cortex by repeated non-invasive brain stimulation. Brain Stimul (2013) 6(3):424–32. 10.1016/j.brs.2012.04.011 [DOI] [PubMed] [Google Scholar]
- 7.Schlaug G, Renga V, Nair D. Transcranial direct current stimulation in stroke recovery. Arch Neurol (2008) 65(12):1571–6. 10.1001/archneur.65.12.1571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Flöel A. tDCS-enhanced motor and cognitive function in neurological diseases. Neuroimage (2014) 85(Pt 3):934–47. 10.1016/j.neuroimage.2013.05.098 [DOI] [PubMed] [Google Scholar]
- 9.Sporns O. Structure and function of complex brain networks. Dialogues Clin Neurosci (2013) 15(3):247–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fox MD, Buckner RL, Liu H, Chakravarty MM, Lozano AM, Pascual-Leone A. Resting-state networks link invasive and noninvasive brain stimulation across diverse psychiatric and neurological diseases. Proc Natl Acad Sci U S A (2014) 111(41):E4367–75. 10.1073/pnas.1405003111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ruffini G, Fox MD, Ripolles O, Miranda PC, Pascual-Leone A. Optimization of multifocal transcranial current stimulation for weighted cortical pattern targeting from realistic modeling of electric fields. Neuroimage (2014) 89:216–25. 10.1016/j.neuroimage.2013.12.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schestatsky P, Morales-Quezada L, Fregni F. Simultaneous EEG monitoring during transcranial direct current stimulation. J Vis Exp (2013) 76:50426. 10.3791/50426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liang WK, Lo MT, Yang AC, Peng CK, Cheng SK, Tseng P, et al. Revealing the brain’s adaptability and the transcranial direct current stimulation facilitating effect in inhibitory control by multiscale entropy. Neuroimage (2014) 90:218–34. 10.1016/j.neuroimage.2013.12.048 [DOI] [PubMed] [Google Scholar]
- 14.Dutta A, Jacob A, Chowdhury SR, Das A, Nitsche MA. EEG-FNIRS based assessment of neurovascular coupling during anodal transcranial direct current stimulation-a stroke case series. J Med Syst (2015) 39(4):1–9. 10.1007/s10916-015-0205-7 [DOI] [PubMed] [Google Scholar]
- 15.Hamilton RH, Chrysikou EG, Coslett B. Mechanisms of aphasia recovery after stroke and the role of noninvasive brain stimulation. Brain Lang (2011) 118:40–50. 10.1016/j.bandl.2011.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mylius V, Ayache SS, Zouari HG, Aoun-Sebaïti M, Farhat WH, Lefaucheur JP. Stroke rehabilitation using noninvasive cortical stimulation: hemispatial neglect. Expert Rev Neurother (2012) 12(8):983–91. 10.1586/ern.12.78 [DOI] [PubMed] [Google Scholar]
- 17.Shah PP, Szaflarski JP, Allendorfer J, Hamilton RH. Induction of neuroplasticity and recovery in post-stroke aphasia by non-invasive brain stimulation. Front Hum Neurosci (2013) 7:888. 10.3389/fnhum.2013.00888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Di Pino G, Pellegrino G, Assenza G, Capone F, Ferreri F, Formica D, et al. Modulation of brain plasticity in stroke: a novel model for neurorehabilitation. Nat Rev Neurol (2014) 10(10):597–608. 10.1038/nrneurol.2014.162 [DOI] [PubMed] [Google Scholar]
- 19.Bolognini N, Vallar G, Casati C, Latif LA, El-Nazer R, Williams J, et al. Neurophysiological and behavioral rffects of tDCS combined with constraint-induced movement therapy in poststroke patients. Neurorehabil Neural Repair (2011) 25(9):819–29. 10.1177/1545968311411056 [DOI] [PubMed] [Google Scholar]
- 20.Celnik P, Paik NJ, Vandermeeren Y, Dimyan M, Cohen LG. Effects of combined peripheral nerve stimulation and brain polarization on performance of a motor sequence task after chronic stroke. Stroke (2009) 40(5):1764–71. 10.1161/STROKEAHA.108.540500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Di Lazzaro V, Dileone M, Capone F, Pellegrino G, Ranieri F, Musumeci G, et al. Immediate and late modulation of interhemispheric imbalance with bilateral transcranial direct current stimulation in acute stroke. Brain Stimul (2014) 7(6):841–8. 10.1016/j.brs.2014.10.001 [DOI] [PubMed] [Google Scholar]
- 22.Fregni F, Boggio PS, Mansur CG, Wagner T, Ferreira MJ, Lima MC, et al. Transcranial direct current stimulation of the unaffected hemisphere in stroke patients. Neuroreport (2005) 16(14):1551–5. 10.1097/01.wnr.0000177010.44602.5e [DOI] [PubMed] [Google Scholar]
- 23.Fusco A, Assenza F, Iosa M, Izzo S, Altavilla R, Paolucci S, et al. The ineffective role of cathodal tDCS in enhancing the functional motor outcomes in early phase of stroke rehabilitation: an experimental trial. Biomed Res Int (2014) 2014:547290. 10.1155/2014/547290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hesse S, Waldner A, Mehrholz J, Tomelleri C, Pohl M, Werner C. Combined transcranial direct current stimulation and robot-assisted arm training in subacute stroke patients: an exploratory, randomized multicenter trial. Neurorehabil Neural Repair (2011) 25(9):838–46. 10.1177/1545968311413906 [DOI] [PubMed] [Google Scholar]
- 25.Khedr EM, Shawky OA, El-Hammady DH, Rothwell JC, Darwish ES, Mostafa OM, et al. Effect of anodal versus cathodal transcranial direct current stimulation on stroke rehabilitation: a pilot randomized controlled trial. Neurorehabil Neural Repair (2013) 27(7):592–601. 10.1177/1545968313484808 [DOI] [PubMed] [Google Scholar]
- 26.Kim DY, Ohn SH, Yang EJ, Park CI, Jung KJ. Enhancing motor performance by anodal transcranial direct current stimulation in subacute stroke patients. Am J Phys Med Rehabil (2009) 88(10):829–36. 10.1097/PHM.0b013e3181b811e3 [DOI] [PubMed] [Google Scholar]
- 27.Kim DY, Lim JY, Kang EK, You DS, Oh MK, Oh BM, et al. Effect of transcranial direct current stimulation on motor recovery in patients with subacute stroke. Am J Phys Med Rehabil (2010) 89(11):879–86. 10.1097/PHM.0b013e3181f70aa7 [DOI] [PubMed] [Google Scholar]
- 28.Lefebvre S, Laloux P, Peeters A, Desfontaines P, Jamart J, Vandermeeren Y. Dual-tDCS enhances online motor skill learning and long-term retention in chronic stroke patients. Front Hum Neurosci (2013) 6:343. 10.3389/fnhum.2012.00343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lefebvre S, Dricot L, Laloux P, Gradkowski W, Desfontaines P, Evrard F, et al. Neural substrates underlying stimulation-enhanced motor skill learning after stroke. Brain (2015) 138(Pt 1):149–63. 10.1093/brain/awu336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lindenberg R, Renga V, Zhu LL, Nair D, Schlaug G. Bihemispheric brain stimulation facilitates motor recovery in chronic stroke patients. Neurology (2010) 75(24):2176–84. 10.1212/WNL.0b013e318202013a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mortensen J, Figlewski K, Andersen H. Combined transcranial direct current stimulation and home-based occupational therapy for upper limb motor impairment following intracerebral hemorrhage: a double-blind randomized controlled trial. Disabil Rehabil (2016) 38(7):637–43. 10.3109/09638288.2015.1055379 [DOI] [PubMed] [Google Scholar]
- 32.Nair DG, Renga V, Lindenberg R, Zhu L, Schlaug G. Optimizing recovery potential through simultaneous occupational therapy and non-invasive brain-stimulation using tDCS. Restor Neurol Neurosci (2011) 29(6):411–20. 10.3233/RNN-2011-0612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rocha S, Silva E, Foerster Á, Wiesiolek C, Chagas AP, Machado G, et al. The impact of transcranial direct current stimulation (tDCS) combined with modified constraint-induced movement therapy (mCIMT) on upper limb function in chronic stroke: a double-blind randomized controlled trial. Disabil Rehabil (2016) 38(7):653–60. 10.3109/09638288.2015.1055382 [DOI] [PubMed] [Google Scholar]
- 34.Triccas LT, Burridge JH, Hughes A, Verheyden G, Desikan M, Rothwell J. A double-blinded randomised controlled trial exploring the effect of anodal transcranial direct current stimulation and uni-lateral robot therapy for the impaired upper limb in sub-acute and chronic stroke. NeuroRehabilitation (2015) 37(2):181–91. 10.3233/NRE-151251 [DOI] [PubMed] [Google Scholar]
- 35.Viana RT, Laurentino GE, Souza RJ, Fonseca JB, Silva Filho EM, Dias SN, et al. Effects of the addition of transcranial direct current stimulation to virtual reality therapy after stroke: a pilot randomized controlled trial. NeuroRehabilitation (2014) 34(3):437–46. 10.3233/NRE-141065 [DOI] [PubMed] [Google Scholar]
- 36.Wu D, Qian L, Zorowitz RD, Zhang L, Qu Y, Yuan Y. Effects on decreasing upper-limb poststroke muscle tone using transcranial direct current stimulation: a randomized sham-controlled study. Arch Phys Med Rehabil (2013) 94(1):1–8. 10.1016/j.apmr.2012.07.022 [DOI] [PubMed] [Google Scholar]
- 37.Chang MC, Kim DY, Park DH. Enhancement of cortical excitability and lower limb motor function in patients with stroke by transcranial direct current stimulation. Brain Stimul (2015) 8(3):561–6. 10.1016/j.brs.2015.01.411 [DOI] [PubMed] [Google Scholar]
- 38.Madhavan S, Weber KA, II, Stinear JW. Non-invasive brain stimulation enhances fine motor control of the hemiparetic ankle: implications for rehabilitation. Exp Brain Res (2011) 209:9–17. 10.1007/s00221-010-2511-0 [DOI] [PubMed] [Google Scholar]
- 39.Sohn MK, Jee SJ, Kim YW. Effect of transcranial direct current stimulation on postural stability and lower extremity strength in hemiplegic stroke patients. Ann Rehabil Med (2013) 37(6):759–65. 10.5535/arm.2013.37.6.759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tanaka S, Takeda K, Otaka Y, Kita K, Osu R, Honda M, et al. Single session of transcranial direct current stimulation transiently increases knee extensor force in patients with hemiparetic stroke. Neurorehabil Neural Repair (2011) 25(6):565–9. 10.1177/1545968311402091 [DOI] [PubMed] [Google Scholar]
- 41.Ko MH, Han SH, Park SH, Seo JH, Kim YH. Improvement of visual scanning after DC brain polarization of parietal cortex in stroke patients with spatial neglect. Neurosci Lett (2008) 448(2):171–4. 10.1016/j.neulet.2008.10.050 [DOI] [PubMed] [Google Scholar]
- 42.Làdavas E, Giulietti S, Avenanti A, Bertini C, Lorenzini E, Quinquinio C, et al. a-tDCS on the ipsilesional parietal cortex boosts the effects of prism adaptation treatment in neglect. Restor Neurol Neurosci (2015) 33(5):647–62. 10.3233/RNN-140464 [DOI] [PubMed] [Google Scholar]
- 43.Sparing R, Thimm M, Hesse MD, Küst J, Karbe H, Fink GR. Bidirectional alterations of interhemispheric parietal balance by non-invasive cortical stimulation. Brain (2009) 132(Pt 11):3011–20. 10.1093/brain/awp154 [DOI] [PubMed] [Google Scholar]
- 44.Sunwoo H, Kim YH, Chang WH, Noh S, Kim EJ, Ko MH. Effects of dual transcranial direct current stimulation on post-stroke unilateral visuospatial neglect. Neurosci Lett (2013) 554:94–8. 10.1016/j.neulet.2013.08.064 [DOI] [PubMed] [Google Scholar]
- 45.Fiori V, Cipollari S, Di Paola M, Razzano C, Caltagirone C, Marangolo P. tDCS stimulation segregates words in the brain: evidence from aphasia. Front Hum Neurosci (2013) 7:269. 10.3389/fnhum.2013.00269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Flöel A, Meinzer M, Kirstein R, Nijhof S, Deppe M, Knecht S, et al. Short-term anomia training and electrical brain stimulation. Stroke (2011) 42(7):2065–7. 10.1161/STROKEAHA.110.609032 [DOI] [PubMed] [Google Scholar]
- 47.Kang EK, Kim YK, Sohn HM, Cohen LG, Paik NJ. Improved picture naming in aphasia patients treated with cathodal tDCS to inhibit the right Broca’s homologue area. Restor Neurol Neurosci (2011) 29(3):141–52. 10.3233/RNN-2011-0587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Marangolo P, Fiori V, Cipollari S, Campana S, Razzano C, Di Paola M, et al. Bihemispheric stimulation over left and right inferior frontal region enhances recovery from apraxia of speech in chronic aphasia. Eur J Neurosci (2013) 38(9):3370–7. 10.1111/ejn.12332 [DOI] [PubMed] [Google Scholar]
- 49.Monti A, Cogiamanian F, Marceglia S, Ferrucci R, Mameli F, Mrakic-Sposta S, et al. Improved naming after transcranial direct current stimulation in aphasia. J Neurol Neurosurg Psychiatry (2008) 79(4):451–3. 10.1136/jnnp.2007.135277 [DOI] [PubMed] [Google Scholar]
- 50.You DS, Kim DY, Chun MH, Jung SE, Park SJ. Cathodal transcranial direct current stimulation of the right Wernicke’s area improves comprehension in subacute stroke patients. Brain Lang (2011) 119(1):1–5. 10.1016/j.bandl.2011.05.002 [DOI] [PubMed] [Google Scholar]
- 51.Kumar S, Wagner C, Frayne C, Zhu L, Selim M, Feng W, et al. Noninvasive brain stimulation may improve stroke-related dysphagia: a pilot study. Stroke (2011) 42:1035–40. 10.1161/STROKEAHA.110.602128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Shigematsu T, Fujishima I, Ohno K. Transcranial direct current stimulation improves swallowing function in stroke patients. Neurorehabil Neural Repair (2013) 27:363–9. 10.1177/1545968312474116 [DOI] [PubMed] [Google Scholar]
- 53.Yang EJ, Baek SR, Shin J, Lim JY, Jang HJ, Kim YK. Effects of transcranial direct current stimulation (tDCS) on post-stroke dysphagia. Restor Neurol Neurosci (2012) 30:303–11. 10.3233/RNN-2012-110213 [DOI] [PubMed] [Google Scholar]
- 54.Butler AJ, Shuster M, O’Hara E, Hurley K, Middlebrooks D, Guilkey K. A meta-analysis of the efficacy of anodal transcranial direct current stimulation for upper limb motor recovery in stroke survivors. J Hand Ther (2013) 26(2):162–70. 10.1016/j.jht.2012.07.002 [DOI] [PubMed] [Google Scholar]
- 55.Kang N, Summers JJ, Cauraugh JH. Transcranial direct current stimulation facilitates motor learning post-stroke: a systematic review and meta-analysis. J Neurol Neurosurg Psychiatry (2015). 10.1136/jnnp-2015-311242 [DOI] [PubMed] [Google Scholar]
- 56.Marquez J, van Vliet P, McElduff P, Lagopoulos J, Parsons M. Transcranial direct current stimulation (tDCS): does it have merit in stroke rehabilitation? A systematic review. Int J Stroke (2015) 10(3):306–16. 10.1111/ijs.12169 [DOI] [PubMed] [Google Scholar]
- 57.Chhatbar PY, Ramakrishnan V, Kautz S, George MS, Adams RJ, Feng W. Transcranial direct current stimulation post-stroke upper extremity motor recovery studies exhibit a dose-response relationship. Brain Stimul (2016) 9(1):16–26. 10.1016/j.brs.2015.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chieffo R, Comi G, Leocani L. Noninvasive neuromodulation in poststroke gait disorders: rationale, feasibility, and state of the art. Neurorehabil Neural Repair (2015) 30(1):71–82. 10.1177/1545968315586464 [DOI] [PubMed] [Google Scholar]
- 59.Dumont AJ, Araujo MC, Lazzari RD, Santos CA, Carvalho DB, Franco de Moura RC, et al. Effects of a single session of transcranial direct current stimulation on static balance in a patient with hemiparesis: a case study. J Phys Ther Sci (2015) 27(3):955–8. 10.1589/jpts.27.955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Vallar G, Bolognini N. Unilateral spatial neglect. In: Nobre AC, Kastner S, editors. Oxford Handbook of Attention. Oxford: Oxford University Press; (2014). p. 972–1027. [Google Scholar]
- 61.Cherney LR, Halper AS, Kwasnica CM, Harvey RL, Zhang M. Recovery of functional status after right hemisphere stroke: relationship with unilateral neglect. Arch Phys Med Rehabil (2001) 82(3):322–8. 10.1053/apmr.2001.21511 [DOI] [PubMed] [Google Scholar]
- 62.Jehkonen M, Laihosalo M, Kettunen JE. Impact of neglect on functional outcome after stroke: a review of methodological issues and recent research findings. Restor Neurol Neurosci (2006) 24(4–6):209–15. [PubMed] [Google Scholar]
- 63.Nijboer TC, Kollen BJ, Kwakkel G. Time course of visuospatial neglect early after stroke: a longitudinal cohort study. Cortex (2013) 49(8):2021–7. 10.1016/j.cortex.2012.11.006 [DOI] [PubMed] [Google Scholar]
- 64.Wade DT, Hewer RL, David RM, Enderby PM. Aphasia after stroke: natural history and associated deficits. J Neurol Neurosurg Psychiatry (1986) 49(1):11–6. 10.1136/jnnp.49.1.11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lazar RM, Minzer B, Antoniello D, Festa JR, Krakauer JW, Marshall RS. Improvement in aphasia scores after stroke is well predicted by initial severity. Stroke (2010) 41:1485–8. 10.1161/STROKEAHA.109.577338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Brady MC, Kelly H, Godwin J, Enderby P. Speech and language therapy for aphasia following stroke. Cochrane Database Syst Rev (2012) 5:CD000425. 10.1002/14651858.CD000425.pub3 [DOI] [PubMed] [Google Scholar]
- 67.Elsner B, Kugler J, Pohl M, Mehrholz J. Transcranial direct current stimulation (tDCS) for improving aphasia in patients after stroke. Cochrane Database Syst Rev (2015) 6:CD009760. 10.1002/14651858.CD009760.pub3 [DOI] [PubMed] [Google Scholar]
- 68.Otal B, Olma M, Flöel A, Wellwood I. Inhibitory non-invasive brain stimulation to homologous language regions as an adjunct to speech and language therapy in post-stroke aphasia: a meta-analysis. Front Hum Neurosci (2015) 9:236. 10.3389/fnhum.2015.00236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hamdy S. Role of neurostimulation and neuroplasticity in the rehabilitation of dysphagia after stroke. Perspect Swallowing Swallowing Disord (Dysphagia) (2010) 19:3–9. 10.1044/sasd19.1.3 [DOI] [Google Scholar]
- 70.Meng NH, Wang TG, Lien IN. Dysphagia in patients with brainstem stroke: incidence and outcome. Am J Phys Med Rehabil (2000) 79(2):170–5. 10.1097/00002060-200003000-00010 [DOI] [PubMed] [Google Scholar]
- 71.Pisegna JM, Kaneoka A, Pearson WG, Jr, Kumar S, Langmore SE. Effects of non-invasive brain stimulation on post-stroke dysphagia: a systematic review and meta-analysis of randomized controlled trials. Clin Neurophysiol (2016) 127(1):956–68. 10.1016/j.clinph.2015.04.069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Yang SN, Pyun SB, Kim HJ, Ahn HS, Rhyu BJ. Effectiveness of non-invasive brain stimulation in dysphagia subsequent to stroke: a systematic review and meta-analysis. Dysphagia (2015) 30(4):383–91. 10.1007/s00455-015-9619-0 [DOI] [PubMed] [Google Scholar]
- 73.Miranda PC, Mekonnen A, Salvador R, Ruffini G. The electric field in the cortex during transcranial current stimulation. Neuroimage (2013) 15(70):48–58. 10.1016/j.neuroimage.2012.12.034 [DOI] [PubMed] [Google Scholar]
- 74.Ruffini G, Wendling F, Merlet I, Molaee-Ardekani B, Mekkonen A, Salvador R, et al. Transcranial current brain stimulation (tCS): models and technologies. IEEE Trans Neural Syst Rehabil Eng (2013) 21:333–45. 10.1109/TNSRE.2012.2200046 [DOI] [PubMed] [Google Scholar]
- 75.Dijkhuizen RM, Ren J, Mandeville JB, Wu O, Ozdag FM, Moskowitz MA, et al. Functional magnetic resonance imaging of reorganization in rat brain after stroke. Proc Natl Acad Sci U S A (2001) 98(22):12766–71. 10.1073/pnas.231235598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Feydy A, Carlier R, Roby-Brami A, Bussel B, Cazalis F, Pierot L, et al. Longitudinal study of motor recovery after stroke: recruitment and focusing of brain activation. Stroke (2002) 33(6):1610–7. 10.1161/01.STR.0000017100.68294.52 [DOI] [PubMed] [Google Scholar]
- 77.Small SL, Hlustik P, Noll DC, Genovese C, Solodkin A. Cerebellar hemispheric activation ipsilateral to the paretic hand correlates with functional recovery after stroke. Brain (2002) 125(Pt 7):1544–57. 10.1093/brain/awf148 [DOI] [PubMed] [Google Scholar]
- 78.Johansen-Berg H, Rushworth MFS, Bogdanovic MD, Kischka U, Wimalaratna S, Matthews PM. The role of ipsilateral premotor cortex in hand movement after stroke. Proc Natl Acad Sci U S A (2002) 99(22):14518–23. 10.1073/pnas.222536799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Takeuchi N, Izumi SI. Maladaptive plasticity for motor recovery after stroke: mechanisms and approaches. Neural Plast (2012) 2012:359728. 10.1155/2012/359728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Takeuchi N, Tada T, Chuma T, Matsuo Y, Ikoma K. Disinhibition of the premotor cortex contributes to a maladaptive change in the affected hand after stroke. Stroke (2007) 38(5):1551–6. 10.1161/STROKEAHA.106.470187 [DOI] [PubMed] [Google Scholar]
- 81.Meinzer M, Breitenstein C. Functional imaging of treatment-induced recovery in chronic aphasia. Aphasiology (2008) 22:1251–68. 10.1080/02687030802367998 [DOI] [Google Scholar]
- 82.Vigneau M, Beaucousin V, Hervé PY, Duffau H, Crivello F, Houdé O, et al. Meta-analyzing left hemisphere language areas: phonology, semantics, and sentence processing. Neuroimage (2006) 30(4):1414–32. 10.1016/j.neuroimage.2005.11.002 [DOI] [PubMed] [Google Scholar]
- 83.Frey S, Campbell JS, Pike GB, Petrides M. Dissociating the human language pathways with high angular resolution diffusion fiber tractography. J Neurosci (2008) 28(45):11435–44. 10.1523/JNEUROSCI.2388-08.2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Naeser MA, Martin PI, Ho M, Treglia E, Kaplan E, Bashir S, et al. Transcranial magnetic stimulation and aphasia rehabilitation. Arch Phys Med Rehabil (2012) 93(1 Suppl):S26–34. 10.1016/j.apmr.2011.04.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Dutta A. Bidirectional interactions between neuronal and hemodynamic responses to transcranial direct current stimulation (tDCS): challenges for brain-state dependent tDCS. Front Syst Neurosci (2015) 9:107. 10.3389/fnsys.2015.00107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Dahne S, Biessmann F, Samek W, Haufe S, Goltz D, Gundlach C, et al. Multivariate machine learning methods for fusing multimodal functional neuroimaging data. Proc IEEE (2015) 103:1507–30. 10.1109/JPROC.2015.2425807 [DOI] [Google Scholar]
- 87.Gramfort A, Papadopoulo T, Olivi E, Clerc M. OpenMEEG: opensource software for quasistatic bioelectromagnetics. Biomed Eng Online (2010) 9:45. 10.1186/1475-925X-9-45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Fang Q, Boas DA. Monte Carlo simulation of photon migration in 3D turbid media accelerated by graphics processing units. Opt Express (2009) 17(22):20178–90. 10.1364/OE.17.020178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Habermehl C, Steinbrink J, Müller KR, Haufe S. Optimizing the regularization for image reconstruction of cerebral diffuse optical tomography. J Biomed Opt (2014) 19:96006. 10.1117/1.JBO.19.9.096006 [DOI] [PubMed] [Google Scholar]
- 90.Hutchison RM, Womelsdorf T, Allen EA, Bandettini PA, Calhoun VD, Corbetta M, et al. Dynamic functional connectivity: promise, issues, and interpretations. Neuroimage (2013) 80:360–78. 10.1016/j.neuroimage.2013.05.079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Tagliazucchi E, Laufs H. Multimodal imaging of dynamic functional connectivity. Front Neurol (2015) 6:10. 10.3389/fneur.2015.00010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Ganesh G, Burdet E, Haruno M, Kawato M. Sparse linear regression for reconstructing muscle activity from human cortical fMRI. Neuroimage (2008) 42:1463–72. 10.1016/j.neuroimage.2008.06.018 [DOI] [PubMed] [Google Scholar]
- 93.Choi K. Electroencephalography (EEG)-based neurofeedback training for brain-computer interface (BCI). Exp Brain Res (2013) 231(3):351–65. 10.1007/s00221-013-3699-6 [DOI] [PubMed] [Google Scholar]
- 94.Dutta A, Paulus W, Nitsche MA. Facilitating myoelectric-control with transcranial direct current stimulation: a preliminary study in healthy humans. J Neuroeng Rehabil (2014) 11:13. 10.1186/1743-0003-11-13 [DOI] [PMC free article] [PubMed] [Google Scholar]