Synopsis
Injuries result in nearly 6 million deaths and incur 52 million disability-adjusted life years annually, comprising 15% of the global disease burden. More than 90% of this burden occurs in low- and middle-income countries (LMICs). Given this burden, it’s not unexpected that injuries are the leading cause of death among travelers to LMICs, namely from road traffic crashes and drowning. Opportunely, the majority of injuries are preventable. Therefore, pre-travel advice regarding foreseeable dangers and how to avoid them may significantly mitigate injury risk, such as: wearing seatbelts, helmets and personal flotation devices when appropriate; responsibly consuming alcohol; and closely supervising children. Upon return, travelers to LMICs are in a unique position; having shared injury risks while abroad, travelers can advocate for injury control initiatives that might make the world safer for travelers and local populations alike.
Keywords: road traffic injuries, drowning, burn, fall, unintentional injury, injury prevention, travel medicine, advocacy
Introduction
Injuries result in nearly 6 million deaths and incur 52 million disability-adjusted life years annually, comprising 15% of the global disease burden.2 More than 90% of this burden occurs in low- and middle-income countries (LMICs) where injury control capacity and initiatives are lacking.3 When trauma services do exist, they are often insufficiently resourced and unavailable to the majority of the injured.4 Consequently, treatable injuries frequently result in avertable death or disability.5
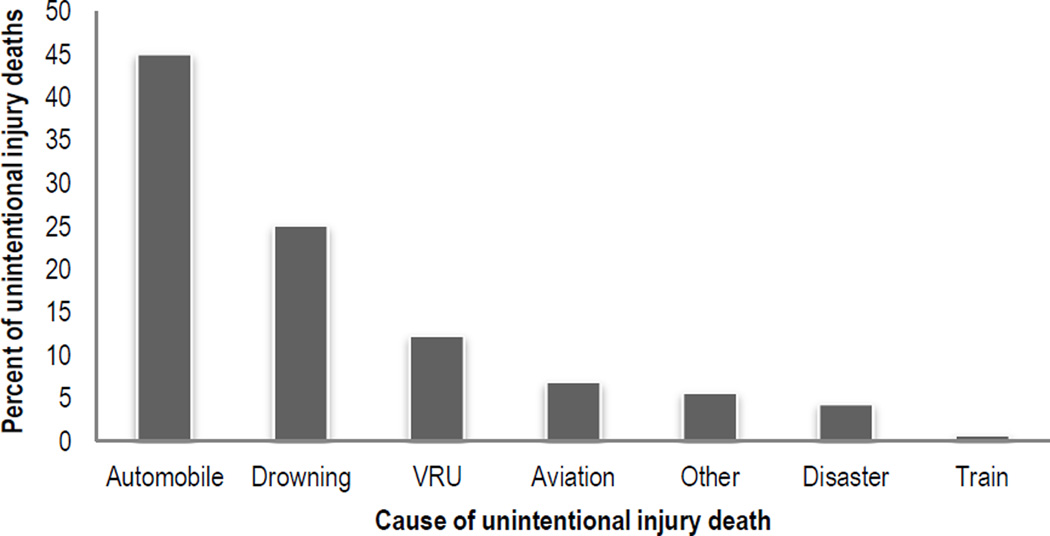
Injuries are the leading cause of death among travelers.6 Travelers are 10 times more likely to die from injury while abroad than infection, which account for <2% of traveler deaths.7 Of traveler unintentional injuries, road traffic crashes account for 57% of deaths, followed by drowning (25%), aviation crashes (7%), other causes (e.g. falls, burns; 6%), and natural disasters (4%) (Figure 1).8
Figure 1.
Percent of unintentional injury deaths by mechanism for United States travelers from 2003 to 2014 (N=4,479).
Unintentional injuries exclude homicide, suicide, and terrorism; VRU – vulnerable road user (i.e. pedestrians, drivers and riders of motorized 2–3 wheeled vehicles, bicyclists).
Data from United States Department of State - Bureau of Consular Affairs. U.S. Citizen Deaths Overseas. Available at: http://travel.state.gov/content/travel/english/statistics/deaths.html. Accessed Jul 28 2015.
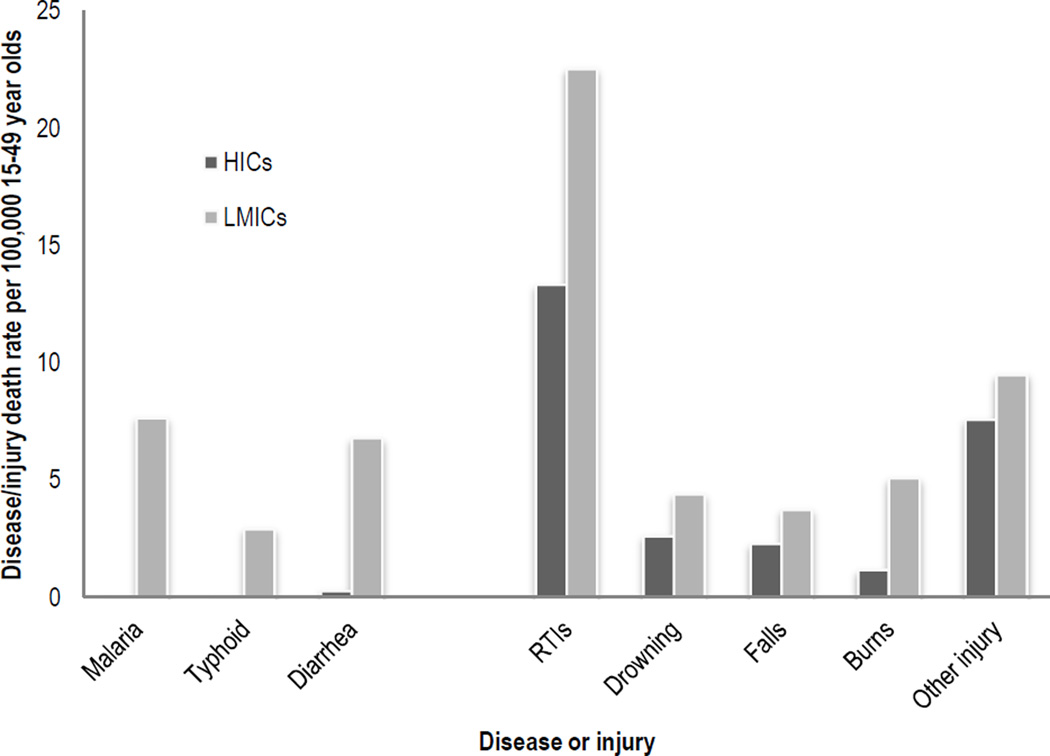
Despite high injury risk, pre-travel advice has concentrated on communicable and vaccine-preventable diseases, such as malaria, typhoid and diarrhea.9 However, among individuals aged 15 – 49 in LMICs (i.e. same age cohort as 65% high-income country travelers), road traffic injuries (RTIs) alone are responsible for more deaths than these three diseases combined (Figure 2).8, 10 A survey of travel medicine clinics worldwide found that 99% offered advice on infections; only 70% discussed ‘personal safety.’11 Fortunately, nearly two-thirds of injuries are preventable.12, 13 Therefore, pre-travel advice regarding foreseeable dangers and how to avoid them may significantly mitigate injury risk.14 Pre-travel consultations are incomplete without specific injury prevention advice.12
Figure 2.
Death rate per 100,000 15–49 year olds for selected diseases and injuries in high-income and low- and middle-income countries.
HICs – high-income countries; LMICs – low- and middle-income countries; RTIs – road traffic injuries; Other injury includes mechanical forces, non-road traffic transport injuries (e.g. aviation crashes), animal contact.
Age 15–49 years was selected since it represents the same age cohort as 65% of high-income country travelers.
Data from Institute of Health Metrics and Evaluation. GBD Cause Patterns. Available at: http://vizhub.healthdata.org/gbd-cause-patterns/. Accessed May 27 2015.
This article discusses the epidemiology, risk and pre-travel advice regarding road traffic injuries and drowning. Other causes of traveler injury, such as aviation crashes, falls, burns, and those associated with adventure activities are also mentioned.6 Upon return, travelers to LMICs are in a unique position; having been exposed to injury risks abroad, travelers can advocate for injury control initiatives that might make the world safer for travelers and local populations alike. Therefore, potentially useful advice for the returning traveler, as well as the travel medicine provider, regarding injury control advocacy is offered.
Road traffic injuries
Epidemiology
More than 1.2 million people are killed on the world’s roads each year.15 Road traffic crashes were the 8th leading cause of death in 2010; by 2030, they are expected to be the 5th.16 However, for those aged 15 – 44, road traffic crashes are the leading cause of death.1, 2 Eighty percent of road traffic deaths occur in middle-income countries, where rapid urbanization and motorization is taking place.16
For each death, another 20–50 persons are injured, some of which suffer permanent disability.15, 17 Without momentous global action, by 2020, RTIs are forecasted to be the third largest global disease burden.15
Differences in RTIs between high-income and LMICs
In addition to the large road traffic burden in LMICs compared to high-income countries (HICs), several notable epidemiological differences exist. In HICs, the most common road user killed by a road traffic crash is a car occupant, comprising nearly 60% of road traffic fatalities.16 In contrast, most vehicle occupant deaths in LMICs are passengers of minibuses, trucks and other public service vehicles.18 Pedestrians constitute 22% of road traffic deaths globally, ranging from 10 to 66% of national road fatalities.16 In LMICs, almost 70% of road deaths are vulnerable road users (i.e. pedestrians, motorists of 2-3 wheeled vehicles, bicyclists; VRUs), compared to 40% in HICs.16 This differential risk has consequences not only for health, but also for social inclusion of people cannot afford vehicular transport.19
Road safety in LMICs
Road safety depends on five factors: political support, funding and effective policies; safe roads; safe vehicles; safe road users; and timely, effective post-crash care.16 The WHO Global Status Report on Road Safety 2013 described road safety using this framework.16 Particularly informative differences are described.
Only 7% of the world’s population, most of which in HICs, is protected by a funded, comprehensive road safety strategy. Consequently, road infrastructure is lacking and less maintained in LMICs than HICs. Safety structures (e.g. guardrails, shoulders, streetlights) are often not planned for, placed or maintained. While vehicle standards may be improving in LMICs, many vehicles remain less crashworthy compared to those in HICs (i.e. older vehicle age; minimum safety regulations for imported vehicles; lack of seatbelts, airbags, and/or crumple zones). Lights, windshield wipers and tires are often not replaced when needed. Nearly all minibuses and trucks that carry passengers in LMICs are not engineered to minimize the risk of passenger injury during a crash.
Well established strategies to prevent pedestrian RTIs are poorly implemented worldwide, particularly in LMICs.16 Road safety priorities and urban design neglect VRUs or fail to consider different risks for vehicle occupants and VRUs.20 Further, drivers often do not respect VRUs and VRUs often do not respect or know road safety signals.21
Poor enforcement and road user noncompliance limit the effectiveness of road safety policies. Only 26 of the world’s 196 countries (13%) reported ‘good’ speeding enforcement (8 or above on a scale from 0 to 10). Motorcyclist and/or bicyclist helmet use is poorly enforced by two-thirds of countries. Helmet standards are rarely incorporated into helmet laws. Drink-driving laws do not protect 34% of the world’s population. In Accra, Ghana’s capital, 21% of randomly selected drivers had a blood alcohol concentration higher than 80mg/dL.22 This is markedly higher than similar studies from Denmark (0.4%) and France (3.4%).23 Additionally, 4% of bus drivers and 8% of truck drivers in Accra had blood alcohol concentrations of ≥80mg/dL.22 Seatbelt, child restraints and mobile phone use while driving laws are particularly lacking and/or under-enforced in LMICs.
The majority of RTI victims in LMICs do not have access to pre-hospital care. Good Samaritans and commercial drivers are the de facto ambulances in LMICs.24 Resultantly, around 80% of injured patients in LMICs die before reaching a hospital, even in urban centers, compared to 21% in Seattle, USA.25 Hospitals often have critical deficiencies in resources necessary to provide essential trauma care.4 Further, less than 55% of emergency care providers in Africa and Southeast Asia have had specific trauma care training.16 Resultantly, injury for injury, victims in LMICs are at greater risk of death and disability than victims in HICs.25
RTI risk among travelers
Travelers to LMICs are at twice the risk of RTI than their counterparts at home and more vulnerable than local populations.9, 10 In Bermuda, travelers were nearly 6 times more likely to sustain a motorcycle injury than Bermudians.26 A regional hospital in Greece reported that only 15% of injuries were due to road traffic among Greeks; among travelers to Greece, 40% of injuries were road traffic-related.27
The effect of driving on different sides of the road on RTI risk is poorly understood. Studies suggest that travelers from countries that drive on the opposite side of the road than the country they traveled to are more likely to be injured than those that drive on the same side of the road.27, 28 RTI risk is not unique to tourists; business travelers are at higher risk as well. World Bank Group employees reported 1 road traffic crash per 175 trips.29
Pre-travel advice on RTIs
Despite these risks, much can be done to prevent RTIs in LMICs (Table 1).30 Most of the recommendations should be practiced no matter the location; some are particularly important and are described here.
Table 1.
Road traffic injury risks and recommendations to avoid them for travelers from high-income countries going to low- and middle-income countries.
| Risk | Recommendations to avoid risk |
|---|---|
| Lack of seatbelts, child safety seats and airbags |
|
| Travel when visibility or traction is limited is particularly dangerous, compounded by infrequent maintenance on vehicle components (e.g. lights, brakes, windshield wipers) |
|
| Lack of signage or signage in a foreign language |
|
|
|
| Alcohol use significantly increases the risk of RTI |
|
| Pedestrians are often the most common road user injured in LMICs |
|
| Lack of emergency care |
|
Seatbelts and child safety seats reduce serious RTIs by 40 – 70%.31, 32 All possible efforts should be made to ride in vehicles with seatbelts and use them. Riding as a backseat passenger is safer than riding in a front seat, particularly when the vehicle lacks airbags.33 Child safety seats and booster seats are rarely available in LMICs.16 Travelers should bring them if traveling with children.
Road crashes are nearly three times more common during rain, at night or during national holidays.34, 35 Thus, travelers should be advised not to travel in a vehicle at night, especially on undivided high-speed interurban or rural roads or during conditions that limit visibility or traction (e.g. fog, rain, snow). If travelers are planning to drive, they should familiarize themselves with local laws, rent a vehicle with seatbelts and airbags, and pay particular attention to local driving hazards, namely driving on the opposite side of the road than accustomed. Signage might be different or in a foreign language; travelers should familiarize themselves with common signage at their destination prior to departure to avoid injury, putting others at risk and/or breaking laws.
Motorcycles or mopeds should be avoided at all costs. This advice should be stressed to travelers planning motorcycle use without significant experience operating these vehicles at their home. If a traveler must ride a 2-wheeled vehicle, a helmet should be worn. Helmets reduce the risk of death among motorcyclists 42% in HICs with developed healthcare systems; the impact of helmet use among crash victims that don’t have access to timely and effective trauma care is unknown, but likely much greater.36 Helmets that meet international safety standards are often not available in LMICs. If 2-wheeled travel is planned, travelers should be instructed to bring their helmet with them and wear it.
Alcohol use increases the risk of all causes of injury, particularly RTIs.9 Travelers should not drive after consuming alcohol or ride with someone who has. Minibuses, trucks and buses are often over-crowded, over-weight and over-speed, which makes them prone to horrific crashes with high fatality and injury rates; thus, they should be avoided.37
Lastly, travelers will likely be pedestrians during their trip. They should take particular caution when crossing roads and look both ways beforehand, paying particular attention to the side of the road drivers use; cross-walks should be sought and used when crossing streets if available. Walking roadside should be discouraged, particularly at night. Travelers planning to drive should be cognizant of VRUs and the risk they pose to them.
The effect of pre-travel injury prevention advice on RTIs has not been studied. However, these simple risk avoidance recommendations are likely to reduce RTIs amongst this high-risk group.
Drowning
Epidemiology
Around 350,000 deaths and more than 20 million disability-adjusted life years are incurred from drowning annually.1 Ninety-seven percent of this burden occurs in LMICs.38 Drowning affects predominately young children in most regions regardless of national income.1, 38
Drowning risk among travelers
Drowning is responsible for 25% of injury deaths among US travelers and is the leading cause of death among travelers to Fiji, The Bahamas, Jamaica, Costa Rica and other areas where water recreation is a major activity.6, 8 As with RTIs, travelers are three times more likely to drown abroad than they are at home.10
The greatest risk factor for child drowning in HICs and LMICs is a lack of supervision.39 In LMICs, lack of supervision is complex and related to caring for a number of children, poverty and increased maternal age.40 Among travelers, lack of supervision is related to inattention to potential water hazards, distractions and insufficient planning.38 Other risk factors for LMIC populations include travel on unsafe or overcrowded watercraft and use of small boats for subsistence fishing.41 Among travelers, unfamiliarity with local water conditions, alcohol use and inability to swim are significant factors.42
Pre-travel advice on drowning
Drowning is highly preventable; should it occur, medical treatment has little effect on the outcome.43 Therefore, primary prevention is particularly important.38 Pre-travel advice should focus on risk reduction specific to the travel destination and planned activities. PFD use and pool, open water and boat safety should be discussed. Important points are listed in Table 2.
Table 2.
Drowning risks and recommendations to avoid them for travelers from high-income countries going to low- and middle-income countries.
| Risk | Recommendations to avoid risk |
|---|---|
| Lack of personal flotation devices (PFDs) or PFDs that meet safety standards and fit properly |
|
|
|
|
|
| Unfamiliarity with local water conditions, poor swimming ability, absence of lifeguards, and presence of rip currents make open water swimming particularly high-risk |
|
| Alcohol use significantly increases drowning risk | Do not operate or ride in a watercraft, swim or supervise children after consuming alcohol |
| Scuba diving is often unregulated and occasionally does not require certification to participate |
|
| Operating or riding in a watercraft that is unfamiliar |
|
| Lack of emergency care |
|
Other unintentional causes of traveler injury
Aviation crashes, falls, burns, and injuries from adventure activities cause traveler deaths each year.6 Like other causes of unintentional injury, many of these can be prevented. Specific risks and ways to avoid them are given in Table 3.
Table 3.
Other injury risks and recommendations to avoid them for travelers from high-income countries going to low- and middle-income countries.
| Topic | Risk | Recommendations to avoid risk |
|---|---|---|
| Aviation crash |
|
|
| Fall |
|
|
| Burn |
|
|
| Adventure activity |
|
|
Opportunity for advocacy
The preceding part of this article is oriented towards the need to sensitize travelers to the significant injury risks they face while abroad and to offer advice on risk reduction behaviors. Upon return, travelers have shared risks with local populations. Therefore, they can be important advocates for the promotion of safety for everyone, everywhere.
In LMICs, injury control initiatives are often considered low priority by policymakers who must choose between competing issues.44 Injury control is often neglected by policymakers because it is under-resourced, requires a stance to be taken against industry, and often impeded by political giants (e.g. alcohol industry, firearm lobby).45 To remove some of these barriers, the social value of injury control must improve and policymakers must be educated on the significant return on investment provided by injury control initiatives.
In order to heighten social awareness and educate policymakers about the burden of injury and cost-effectiveness of its control, many stakeholders need to be involved.45 Potentially important stakeholders include: individuals and groups of citizens, non-governmental organizations; industry; and governments. However, any group that campaigns for injury control and can positively influence social or political opinion should be included in advocacy efforts.45, 46 Advocacy can include the use of local or mass media (e.g. flyers, newspaper editorials, radio shows), social media, direct political lobbying, and/or community mobilization through coalition of interest groups.45 Successful examples of advocacy groups that started from a single or small group of individuals that have had a positive impact on injury control include Stop for Kids, Mothers Against Drunk Driving (MADD) and the Brain Injury Association of America (BIAA).45, 47, 48 Examples that include LMIC populations are few despite the greater burden they face.
Travel medicine providers also have a unique opportunity to advocate for injury control. Their understanding of the evidence-base and position in society give their voice particular weight.49 Many examples of physician-led advocacy groups that caused a significant national or international improvement in injury control exist (e.g. Physicians for Human Rights, International Campaign to Ban Landmines and Doctors Against Handgun Injury).50–53 Physician-led unintentional injury control campaigns are less publicized.
Key messages that travelers and travel medicine providers might share during advocacy efforts include (Figure 3):
90% of the near 6 million injury deaths annually occur in developing countries; 1 in 5 of these deaths is a child;2, 54
Families of the injured are frequently forced into poverty due to medical costs or lost wages, placing them at higher injury risk and creating an injury-poverty cycle;55–57
Road injury alone costs the world more than 500 billion dollars annually; some countries lose more on injury than they spend on healthcare;56, 58 and
Injury control is as cost-effective as HIV/AIDS treatment and vaccination.59, 60
In summary, advocacy is a way for travelers to make a difference in LMICs that lasts long after their trip and for travel medicine providers to contribute to patient and population health more broadly.
Figure 3.
Key points for injury control advocacy at home and abroad.
Key points.
Road traffic crashes are the most common cause of traveler death.
Travelers can protect themselves and set an example by: always wearing a seatbelt, never driving after consuming alcohol, and wearing a helmet when riding a motorcycle, moped or bicycle.
Drowning is the most common cause of death among travelers to water recreation destinations.
Closely supervising children, wearing a personal flotation device, and practicing pool, open water and boat safety can lower drowning risk.
Advocacy is a way for travelers to make a difference that lasts long after their trip and for travel medicine providers to contribute to patient and population health more broadly.
Acknowledgments
Funding: This study was funded by grants (R25-TW009345; D43-TW007267) from the Fogarty International Center, US National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure statement: No real or potential conflicts to disclose.
Contributor Information
Barclay Stewart, Department of Surgery, University of Washington, Seattle, WA, USA; School of Medical Sciences, Kwame Nkrumah University of Science and Technology, Kumasi, Ghana; Department of Surgery, Komfo Anokye Teaching Hospital, Kumasi, Ghana.
Isaac Kofi Yankson, Building and Road Research Institute, Kumasi, Ghana.
Francis Afukaar, Building and Road Research Institute, Kumasi, Ghana.
Martha Hijar Medina, Ministry of Health, Mexico City, Mexico.
Pham Viet Cuong, Center for Injury Policy and Prevention Research, Hanoi School of Public Health, Hanoi, Vietnam.
Charles Mock, Harborview Injury Prevention & Research Center, Seattle, WA, USA; Department of Surgery, University of Washington, Seattle, WA, USA; Department of Global Health, University of Washington, Seattle, WA, USA.
References
- 1.Data Visualizations. Seattle, WA: Institute of Health Metrics and Evaluation; 2013. [cited 2015 May 27]. Available from: http://vizhub.healthdata.org/gbd-causepatterns/. [Google Scholar]
- 2.Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mock C, Juillard C, Joshipura M, et al. Geneva: World Health Organization; 2010. Strengthening care for the injured: success stories and lessons learned from around the world. [Google Scholar]
- 4.Wong EG, Gupta S, Deckelbaum DL, et al. Prioritizing injury care: a review of trauma capacity in low and middle-income countries. Journal of Surgical Research. 2014 doi: 10.1016/j.jss.2014.08.055. [DOI] [PubMed] [Google Scholar]
- 5.Yeboah D, Mock C, Karikari P, et al. Minimizing preventable trauma deaths in a limited-resource setting: a test-case of a multidisciplinary panel review approach at the Komfo Anokye Teaching Hospital in Ghana. World J Surg. 2014;38(7):1707–1712. doi: 10.1007/s00268-014-2452-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.New York: Centers for Disease Control and Prevention; 2012. Health information for international travel 2012. [Google Scholar]
- 7.Hargarten SW, Baker TD, Guptill K. Overseas fatalities of United States citizen travelers: an analysis of deaths related to international travel. Ann Emerg Med. 1991;20(6):622–626. doi: 10.1016/s0196-0644(05)82379-0. [DOI] [PubMed] [Google Scholar]
- 8.Washington, D.C.: United States Department of State; Death of US citizens abroad by non-natural causes. [Google Scholar]
- 9.Sanford C. Urban medicine: threats to health of travelers to developing world cities. J Travel Med. 2004;11(5):313–327. doi: 10.2310/7060.2004.19108. [DOI] [PubMed] [Google Scholar]
- 10.Tonellato DJ, Guse CE, Hargarten SW. Injury deaths of US citizens abroad: new data source, old travel problem. J Travel Med. 2009;16(5):304–310. doi: 10.1111/j.1708-8305.2009.00318.x. [DOI] [PubMed] [Google Scholar]
- 11.Hill DR, Behrens RH. A Survey of Travel Clinics Throughout the World. J Travel Med. 1996;3(1):46–51. doi: 10.1111/j.1708-8305.1996.tb00696.x. [DOI] [PubMed] [Google Scholar]
- 12.Wadhwaniya S, Hyder AA. Pre-travel consultation without injury prevention is incomplete. J Travel Med. 2013;20(4):217–220. doi: 10.1111/jtm.12041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Philippakis A, Hemenway D, Alexe DM, et al. A quantification of preventable unintentional childhood injury mortality in the United States. Inj Prev. 2004;10(2):79–82. doi: 10.1136/ip.2003.004119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hanson DW, Finch CF, Allegrante JP, et al. Closing the gap between injury prevention research and community safety promotion practice: revisiting the public health model. Public Health Rep. 2012;127(2):147–155. doi: 10.1177/003335491212700203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Peden M. Global collaboration on road traffic injury prevention. Int J Inj Contr Saf Promot. 2005;12(2):85–91. doi: 10.1080/15660970500086130. [DOI] [PubMed] [Google Scholar]
- 16.Toroyan T, Iaych K, Peden M. Geneva: World Health Organization: Department of Violence and Injury Prevention and Disability; 2013. Global Status Report on Road Safety: 2013. [DOI] [PubMed] [Google Scholar]
- 17.Gosselin RA, Spiegel DA, Coughlin R, et al. Injuries: the neglected burden in developing countries. Bull World Health Organ. 2009;87(4):246–246a. doi: 10.2471/BLT.08.052290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sethi D, Zwi A. Traffic accidents another disaster? European Journal of Public Health. 1999;9(1):65–67. [Google Scholar]
- 19.Azetsop J. Social Justice Approach to Road Safety in Kenya: Addressing the Uneven Distribution of Road Traffic Injuries and Deaths across Population Groups. Public Health Ethics. 2010;3(2):115–127. doi: 10.1093/phe/phq013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Trevino-Siller S, Hijar M, Mora G. Prioritisation of road traffic injury interventions: results of a participative research with stakeholders in Mexico. Int J Inj Contr Saf Promot. 2011;18(3):219–225. doi: 10.1080/17457300.2011.569891. [DOI] [PubMed] [Google Scholar]
- 21.Hijar M, Trostle J, Bronfman M. Pedestrian injuries in Mexico: a multi-method approach. Soc Sci Med. 2003;57(11):2149–2159. doi: 10.1016/s0277-9536(03)00067-4. [DOI] [PubMed] [Google Scholar]
- 22.Mock C, Asiamah G, Amegashie J. A random, roadside breathalyzer survey of alcohol impaired driving in Ghana. Journal of Crash Prevention and Injury Control. 2001;2(3):193–202. [Google Scholar]
- 23.Ross HL. Prevalence of alcohol-impaired driving: an international comparison. Accid Anal Prev. 1993;25(6):777–779. doi: 10.1016/0001-4575(93)90042-u. [DOI] [PubMed] [Google Scholar]
- 24.Mock CN, Tiska M, Adu-Ampofo M, et al. Improvements in prehospital trauma care in an African country with no formal emergency medical services. Journal of Trauma. 2002;53(1):90–97. doi: 10.1097/00005373-200207000-00018. [DOI] [PubMed] [Google Scholar]
- 25.Mock C, Jurkovich G, nii-Amon-Kotei D. Trauma mortality patterns in three nations at different economic levels: implications for global trauma system development. Journal of Trauma. 1998;44:804–814. doi: 10.1097/00005373-199805000-00011. [DOI] [PubMed] [Google Scholar]
- 26.Carey MJ, Aitken ME. Motorbike injuries in Bermuda: a risk for tourists. Ann Emerg Med. 1996;28(4):424–429. doi: 10.1016/s0196-0644(96)70009-4. [DOI] [PubMed] [Google Scholar]
- 27.Petridou E, Askitopoulou H, Vourvahakis D, et al. Epidemiology of road traffic accidents during pleasure travelling: the evidence from the Island of Crete. Accid Anal Prev. 1997;29(5):687–693. doi: 10.1016/s0001-4575(97)00038-9. [DOI] [PubMed] [Google Scholar]
- 28.Page SJ, Meyer D. Tourist accidents. Annals of Tourism Research. 1996;23(1):666–690. [Google Scholar]
- 29.Goldoni Laestadius J, Selod AG, Ye J, et al. Can business road travel be safe? Experience of an international organization. J Travel Med. 2011;18(2):73–79. doi: 10.1111/j.1708-8305.2010.00491.x. [DOI] [PubMed] [Google Scholar]
- 30.Mock C, Quansah R, Krishnan R, et al. Strengthening the prevention and care of injuries worldwide. Lancet. 2004;363(9427):2172–2179. doi: 10.1016/S0140-6736(04)16510-0. [DOI] [PubMed] [Google Scholar]
- 31.Washington, DC: Department of Transportation, National Highway Traffic Safety Administration; 1984. Final regulatory impact analysis amendment to Federal Motor Vehicle Safety Standard 208. Contract No.: Publication no. DOT-HS-806-572. [Google Scholar]
- 32.Kahane C. Washington, D.C.: US Department of Transport, National Highway Traffic Safety Administration; 1986. An evaluation of child passenger safety: the effectiveness and benefits of safety seats. Contract No: DOT HS 806 890. [Google Scholar]
- 33.Smith KM, Cummings P. Passenger seating position and the risk of passenger death in traffic crashes: a matched cohort study. Inj Prev. 2006;12(2):83–86. doi: 10.1136/ip.2005.010306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mogaka EO, Ng'ang'a Z, Oundo J, et al. Factors associated with severity of road traffic injuries, Thika, Kenya. Pan Afr Med J. 2011;8:20. doi: 10.4314/pamj.v8i1.71076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ngo AD, Rao C, Hoa NP, et al. Road traffic related mortality in Vietnam: evidence for policy from a national sample mortality surveillance system. BMC Public Health. 2012;12:561. doi: 10.1186/1471-2458-12-561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Crandon IW, Harding HE, Cawich SO, et al. The impact of helmets on motorcycle head trauma at a tertiary hospital in Jamaica. BMC Res Notes. 2009;2:172. doi: 10.1186/1756-0500-2-172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Odero W. Road traffic accidents in Kenya: an epidemiological appraisal. East Afr Med J. 1995;72(5):299–305. [PubMed] [Google Scholar]
- 38.Cortes LM, Hargarten SW, Hennes HM. Recommendations for water safety and drowning prevention for travelers. J Travel Med. 2006;13(1):21–34. doi: 10.1111/j.1708-8305.2006.00002.x. [DOI] [PubMed] [Google Scholar]
- 39.Hyder AA, Borse NN, Blum L, et al. Childhood drowning in low- and middle-income countries: Urgent need for intervention trials. J Paediatr Child Health. 2008;44(4):221–227. doi: 10.1111/j.1440-1754.2007.01273.x. [DOI] [PubMed] [Google Scholar]
- 40.Ahmed MK, Rahman M, van Ginneken J. Epidemiology of child deaths due to drowning in Matlab, Bangladesh. Int J Epidemiol. 1999;28(2):306–311. doi: 10.1093/ije/28.2.306. [DOI] [PubMed] [Google Scholar]
- 41.Geneva, Switzerland: World Health Organization; 2014. Drowning. Contract No.: Fact sheet N°347. [Google Scholar]
- 42.Gulliver P, Begg D. Usual water-related behaviour and 'near-drowning' incidents in young adults. Aust N Z J Public Health. 2005;29(3):238–243. doi: 10.1111/j.1467-842x.2005.tb00761.x. [DOI] [PubMed] [Google Scholar]
- 43.Kyriacou DN, Arcinue EL, Peek C, et al. Effect of immediate resuscitation on children with submersion injury. Pediatrics. 1994;94(2 Pt 1):137–142. [PubMed] [Google Scholar]
- 44.Debinski B, Clegg Smith K, Gielen A. Public opinion on motor vehicle-related injury prevention policies: a systematic review of a decade of research. Traffic Inj Prev. 2014;15(3):243–251. doi: 10.1080/15389588.2013.816419. [DOI] [PubMed] [Google Scholar]
- 45.Sethi D, Mitis F. Geneva, Switzerland: World Health Organization European Centre for Environment and Health; 2009. APOLLO Policy Briefing. [Google Scholar]
- 46.Loue S. Community health advocacy. J Epidemiol Community Health. 2006;60(6):458–463. doi: 10.1136/jech.2004.023044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mothers Against Drunk Driving (MADD) [cited 2015 May 16th]; Available from: http://www.madd.org. [Google Scholar]
- 48.Brain Injury Association of America. [cited 2015 May 16th]; Available from: http://www.biausa.org. [Google Scholar]
- 49.Dharamsi S, Ho A, Spadafora SM, et al. The physician as health advocate: translating the quest for social responsibility into medical education and practice. Acad Med. 2011;86(9):1108–1113. doi: 10.1097/ACM.0b013e318226b43b. [DOI] [PubMed] [Google Scholar]
- 50.Hall P. Physicians for Human Rights (UK) BMJ. 1991;303(6817):1562–1563. doi: 10.1136/bmj.303.6817.1562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kushner A, Raymond N. Health Care Hobbled: Ambulatory Care Treatment of Cambodian Landmine Survivors. Journal of Ambulatory Care Management. 2000;23(3):88–89. [Google Scholar]
- 52.Longjohn MM, Christoffel KK. Are medical societies developing a standard for gun injury prevention? Inj Prev. 2004;10(3):169–173. doi: 10.1136/ip.2003.004531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kendrick D, Hayes M, Ward H, et al. Preventing unintentional injuries: what does NICE guidance mean for primary care? Br J Gen Pract. 2012;62(595):62–63. doi: 10.3399/bjgp12X625012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Harvey A, Towner E, Peden M, et al. Injury prevention and the attainment of child and adolescent health. Bull World Health Organ. 2009;87(5):390–394. doi: 10.2471/BLT.08.059808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Shrime MG, Dare AJ, Alkire BC, et al. Catastrophic expenditure to pay for surgery worldwide: a modelling study. Lancet Glob Health. 2015;3(Suppl 2):S38–S44. doi: 10.1016/S2214-109X(15)70085-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wesson HK, Boikhutso N, Bachani AM, et al. The cost of injury and trauma care in low- and middle-income countries: a review of economic evidence. Health Policy and Planning. 2014 doi: 10.1093/heapol/czt064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Thanh NX, Hang HM, Chuc NT, et al. Does "the injury poverty trap" exist? A longitudinal study in Bavi, Vietnam. Health Policy. 2006;78(2–3):249–257. doi: 10.1016/j.healthpol.2005.10.003. [DOI] [PubMed] [Google Scholar]
- 58.Dalal K, Lin Z, Gifford M, et al. Economics of global burden of road traffic injuries and their relationship with health system variables. Int J Prev Med. 2013;4(12):1442–1450. [PMC free article] [PubMed] [Google Scholar]
- 59.Bishai DM, Hyder AA. Modeling the cost effectiveness of injury interventions in lower and middle income countries: opportunities and challenges. Cost Eff Resour Alloc. 2006;4:2. doi: 10.1186/1478-7547-4-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Grimes CE, Henry JA, Maraka J, et al. Cost-effectiveness of surgery in low- and middle-income countries: a systematic review. World J Surg. 2014;38(1):252–263. doi: 10.1007/s00268-013-2243-y. [DOI] [PubMed] [Google Scholar]