Abstract
Background
Physical activity during pregnancy is associated with reduced risk of adverse maternal and fetal outcomes. However, the majority of pregnant women are inactive and interventions designed to increase exercise during pregnancy are sparse. We evaluated the feasibility and preliminary efficacy of an exercise intervention among a diverse sample of pregnant women.
Methods
The B.A.B.Y. (Behaviors Affecting Baby and You) Study is conducted at a large tertiary care facility in Western Massachusetts. We randomized 110 prenatal care patients (60% Hispanic) to an individually tailored 12-week exercise intervention arm (n = 58) or to a health and wellness control arm (n = 52) at mean = 11.9 weeks gestation. Physical activity was assessed via the Pregnancy Physical Activity Questionnaire (PPAQ).
Results
After the 12-week intervention, the exercise arm experienced a smaller decrease (−1.0 MET-hrs/wk) in total activity vs. the control arm (−10.0 MET-hrs/wk; P = .03), and a higher increase in sports/exercise (0.9 MET-hrs/wk) vs. the control arm (−0.01 MET-hrs/wk; P = .02). Intervention participants (95%) reported being satisfied with the amount of information received and 86% reported finding the study materials interesting and useful.
Conclusions
Findings support the feasibility and preliminary efficacy of a tailored exercise intervention in increasing exercise in a diverse sample of pregnant women.
Keywords: controlled clinical trial, exercise, pregnancy, gestational diabetes, transtheoretical model
Physical activity during pregnancy has been associated with a reduced risk of a variety of maternal and fetal disorders including preeclampsia,1,2 small-for-gestational-age birth,3 preterm birth,4 as well as excessive gestational weight gain5,6 and gestational diabetes mellitus (GDM).7–9 In turn, women diagnosed with excessive gestational weight gain and GDM are at high risk for future diabetes10 and their children are at increased risk of perinatal morbidity,11–13 and, in the long-term, obesity and glucose intolerance.14–16
Current American College of Obstetricians and Gynecologists (ACOG) guidelines recommend engaging in 30 minutes of moderate intensity physical activity (eg, brisk walking) during most days of the week for pregnant women without medical or obstetrical complications.17 In 2008, the United States (US) government released physical activity guidelines for Americans including recommendations that pregnant women attain at least 150 minutes of moderate intensity aerobic activity per week if not already highly active or doing vigorous intensity activity.18 These guidelines are consistent with guidelines for nonpregnant women,19 which also emphasize the accumulation of the 30 minute minimum through bouts of at least 10 minutes in duration; such guidelines may be more acceptable to pregnant women than traditional exercise recommendations.19 However, currently the majority of pregnant women do not meet physical activity guidelines.20,21
Hispanics are the least physically active ethnic group in the United States22 and are disproportionately affected by overweight and obesity;23,24 at each level of body mass index (BMI), Hispanics have a higher prevalence of diabetes than non-Hispanic whites.23,25,26 This is critical as Hispanics are the largest minority group in the United States, with the highest birth and immigration rates.27 It is estimated that by 2050, Hispanic women will comprise 24% of the US female population.28
Individually-tailored, motivationally-matched exercise interventions have been found to be an effective, low-cost approach for enhancing physical activity participation among nonpregnant women in the community.29–32 However, to date, few primary prevention studies have intervened to test whether intervention programs can lead to an increase in physical activity during pregnancy.33–36 In addition, these studies did not include significant numbers of Hispanic women. Women receive closer medical attention during the prenatal and postpartum periods than at other times in their adult lives, and are often highly motivated to improve their health to benefit their children.37 A pregnancy exercise intervention would capitalize upon this teachable moment.
Therefore, we evaluated the feasibility and preliminary efficacy of a 12-week intervention to promote physical activity among a diverse sample of pregnant women at high risk for GDM. Specifically, we defined ‘feasibility’ as participant satisfaction with the intervention and defined ‘efficacy’ as the ability of the exercise intervention to enhance adoption of physical activity among pregnant women. We hypothesized that the intervention would produce significantly greater increases in exercise and associated process variables (ie, stages and processes of changes, self-efficacy) from pre to post intervention as compared with a health and wellness contact control condition.
Methods
Study Population and Setting
The B.A.B.Y. (Behaviors Affecting Baby and You) study is an ongoing randomized clinical trial based in the ambulatory obstetrical practices of Baystate Medical Center, a large tertiary care facility in Western Massachusetts. Baystate serves an ethnically and socioeconomically diverse population with approximately 4500 deliveries per year. Eligible women are sedentary and at high risk of GDM defined as 1) overweight/obese with a family history of diabetes or 2) a diagnosis of GDM in a prior pregnancy defined according to American Diabetes Association Criteria.38 Exclusion criteria include ages < 16 or > 40 years; history of diagnosis of diabetes outside of pregnancy, hypertension, heart disease, or chronic renal disease; current medications which adversely influence glucose tolerance; >25 weeks gestation; contraindications to participating in moderate physical activity; inability to read English at a 6th grade level; self-reported current participation in > 30 min of moderate or vigorous-intensity exercise on more than 3 days/wk; or nonsingleton pregnancy.
Study Design
The study design has been described elsewhere.39 Briefly, recruitment began in July 2007. Bilingual interviewers recruited patients at a prenatal care visit early in pregnancy (mean 11.9 weeks gestation), informed them of the aims and procedures of the study, and obtained written informed consent as approved by the Institutional Review Boards of the University of Massachusetts-Amherst and Baystate Health.
Interviewers prescreened eligible patients using demographic and medical characteristics provided on a daily roster of scheduled patients to generate a list of potential participants. Potential participants were defined as pregnant women who were, based on the daily roster, deemed to be between ages 16 and 40 years and early in pregnancy (<25 weeks gestation). On average, at the study site, we have observed that 45.5% of potential participants are not approached either because the patient did not attend her prenatal care appointment (55.0%) or because she was immediately called into her medical exam or the recruiter was with another participant (45.0%). Potential participants were asked if they would like to participate in the study and then further screened for eligibility.40 Eligible prenatal care patients were randomized in early pregnancy to either a 12-week individually tailored exercise intervention or to a comparison health and wellness intervention.
Randomization was stratified based on age (ages <30, ≥30 years), prepregnancy BMI (overweight ≥25 kg/m2 vs. normal weight BMI <25 kg/m2), and ethnicity (Hispanic vs. non-Hispanic). These 3 2-level stratification factors result in 8 possible strata. Within each stratum, a blocked randomization was used such that both treatment groups were assigned an equal number of times in each set of 4 sequentially enrolled subjects.
At the start of the intervention, health educators meet with the participants in a face-to-face session to assess stage of change, facilitators and barriers to exercise, and provide individual counseling. During follow-up, mailed, print-based materials (stage-matched manuals, tip sheets) as well as telephone booster calls provide motivationally-based individualized feedback regarding progress toward goals. Intervention materials were mailed weekly for the first 4 weeks of the intervention, and then biweekly (ie, once every 2 weeks) for the last 8 weeks of the intervention. All intervention materials were written at a 6th grade reading level. Contact time between the health educators and the participants was consistent across the 2 study arms. In this way, we controlled for contact time, while keeping the content of the 2 interventions distinct.
Baseline and follow-up assessments were conducted before randomization, at the end of the intervention, and in the third trimester to collect information on levels of and change in physical activity. Power calculations were based on 2-sided tests with a significance level of alpha = 5%. Based on a sample size of 58 in the exercise arm and 52 in the health and wellness arm, the smallest mean difference in change from baseline between study arms in sports/exercise that could be detected at 80% power was 1.1 MET-hrs/week or 0.5 standard deviations. Cohen41 defines a detectable difference of 0.5 standard deviations as a “medium” effect size.
Tailored Exercise Intervention
The overall goal of the exercise intervention was to encourage pregnant women to achieve ACOG Guidelines for physical activity during pregnancy (30 minutes or more of moderate-intensity activity on most days of the week) through increasing walking and developing a more active lifestyle in 1 daily bout or accumulated through 10-minute bouts. The intervention draws from the transtheoretical model42 and social cognitive theory43 constructs for physical activity behavior and takes into account the specific social, cultural, economic, and environmental challenges faced by pregnant women of diverse socioeconomic and ethnic backgrounds. It addresses the rapidly changing context of pregnancy which brings opportunities for adoption and maintenance of new behaviors.
In the face-to-face session, based upon responses to a 65-item tailoring questionnaire, the participant is given a stage-matched manual targeted at a specific stage of motivational readiness to adopt physical activity (precontemplation, contemplation, preparation, action, and maintenance). These manuals include motivationally targeted materials combined with stretching tips, tip sheets on goal setting, benefits of physical activity, building social support for new behavioral patterns, and strategies for overcoming barriers to physical activity that are specific to ethnically/racially diverse women and women with young children. Participants are also given an ACOG Pregnancy Fitness brochure which reviews special considerations for physical activity during pregnancy.44
Individualized week-by-week physical activity goals are determined by the health educator in conjunction with the participant. The overall activity goal is to increase the time spent in moderate activity by 10% each week with a 12-week goal of 30 minutes of moderate intensity physical activity performed on 5 or more days per week. Women choose what form of activity to engage in, from dancing to walking in a shopping mall to yard work. The accumulation of short bouts (ie, <10-minute episodes of walking) is encouraged. Participants are then provided with a digital pedometer (Omron) to encourage self-monitoring. Following the face-to-face visit, the participant receives, via mail, weekly and biweekly follow-up tailoring questionnaires (with a postage paid envelope). Return of these questionnaires triggers the mailing of individually-tailored reports generated by a computer expert system and corresponding stage-matched manuals. The individually tailored reports provide 1) an assessment of the individual’s current stage of motivational readiness to adopt a physical activity regimen;45 2) assessments of the individual’s self-efficacy,46 benefits of and barriers to the adoption of physical activity, decisional balance,47 use of cognitive and behavioral processes associated with physical activity adoption,45 and normative feedback; and 3) feedback regarding progress the individual made on these constructs and minutes of physical activity participation since the prior assessment. The individually tailored reports and the stage-matched manuals have been field tested and shown to be effective in prior interventions by Marcus and colleagues.48,49
Over the course of the intervention, weekly and biweekly booster telephone calls provide motivationally-based individualized feedback as well as review of progress toward behavioral goals including a review of the pedometer activity log. Those not achieving their weekly physical activity goals are given additional individualized physical activity counseling with a focus on overcoming barriers.
Health and Wellness (Control) Arm
In the face-to-face session with participants in the health and wellness arm, the health educator reviews general issues related to health and wellness during pregnancy. Participants are provided with a book published by ACOG covering every aspect of pregnancy from preconceptional and prenatal care, health insurance, and labor and delivery to breastfeeding, and child care options. Following the face-to-face visit, participants receive weekly and biweekly mailings of ACOG informational brochures on such topics as alcohol and drug use during pregnancy, easing back pain, travel during pregnancy, and other topics. These materials are selected to represent high-quality, standard, low-cost, self-help material currently available to the public. Weekly and biweekly booster telephone calls provide an opportunity for participants to ask questions about the materials they have received.
Outcome Measures
Pregnancy Physical Activity Questionnaire (PPAQ)
Telephone interviewers, blinded to the study arm, administered the Pregnancy Physical Activity Questionnaire (PPAQ)50 before randomization and at the end of the intervention period to collect information on levels of and change in physical activity. The PPAQ is a semi-quantitative questionnaire that asks respondents to report usual physical activity during the past month and queries the time spent participating in 32 activities including household/care-giving (13 activities), occupational (5 activities), sports/exercise (8 activities), transportation (3 activities), and inactivity (3 activities). For every participant, the number of minutes spent in each reported activity type were multiplied by its MET intensity and summed to arrive at a measure of average weekly energy expenditure (MET-hrs/wk). MET intensity scores were based upon the Compendium of Physical Activities,51 with the exception of walking and light housework activities for which field-based measures among pregnant women were used.50 Average weekly energy expenditure was further classified into categories based on activity intensity and type. Intensity categories were defined as sedentary (<1.5 METs), light (1.5–2.9 METs), moderate (3.0–6.0 METs), and vigorous (>6.0 METs). Categories of activity type included household, occupational, sports and exercise, and transportation.
If women were not reached over the telephone, interviewers mailed the PPAQ to the woman’s home, or completed the surveys in person at the time of a regular prenatal care visit. The original protocol also included an accelerometer, to be worn for a 1-week period at both the baseline and follow-up assessment periods.39 Compliance with this measure was low, and the methodological challenges faced by use of this waist-worn device in a low income, diverse pregnant population will be published in a separate manuscript.
Physical Activity Intervention Constructs
The 65 item tailoring questionnaire developed by Marcus et al.45–47,52 was used to assess physical activity intervention constructs which included processes of change, exercise self-efficacy, and decisional balance. Internal consistency for the processes-of-change scales average 0.83.45 The 5-item self-efficacy measure has an internal consistency of 0.76 and test–retest reliability over a 2-week period of 0.90.46 Internal consistency for the decisional balance measure is 0.79 for the Pros (benefits) scale and 0.95 for the Cons (costs) scale.47
Feasibility and Acceptability
After the completion of the intervention and at the time of the 3rd assessment (third trimester), the feasibility and acceptability of the individually tailored exercise program was evaluated with an adapted version of the consumer satisfaction questionnaire that has been used across multiple trials.29,31 Specifically, the consumer satisfaction survey was streamlined with an emphasis on assessing barriers to participation and comfort level with specific study activities; it was also made available in Spanish. If women were not reached over the telephone, interviewers mailed the satisfaction questionnaire to the woman’s home, or completed it in person at the time of a regular prenatal care visit.
Covariates
At the time of recruitment, structured questionnaires were used to collect information on sociodemographic factors such as age, ethnicity, education, annual household income, marital status, living situation (eg, with a spouse or partner), and the number of adults and children in the household. Participants also self-reported pre- and early pregnancy cigarette smoking. Prepregnancy BMI was abstracted from the medical record.
Statistical Analyses
Data were analyzed using SAS version 9.2 for Windows. We conducted descriptive analyses to summarize demographic variables and feasibility and acceptability data. We assessed the equivalence of the intervention arms by comparing the distribution of covariates between each arm using chi-square tests for categorical variables or Fisher’s Exact Test if the expected cell count was less than 5. Because a test for normality confirmed the normal distribution of the outcome variable (ie, change in physical activity from pre to post intervention), we evaluated the effect of the intervention on the adoption and maintenance of physical activity using 2 sample t tests. Two sample t tests were also used to compare changes in process variables from pre to post intervention across intervention arms. Finally, we used multiple linear regression to evaluate effect modification of the treatment effect by ethnicity (Hispanic vs. not Hispanic) and prepregnancy BMI. Because only 2 women had a normal BMI and no women were underweight, we stratified prepregnancy BMI by overweight (<30 kg/m2) vs. obese (>30 kg/m2).
Results
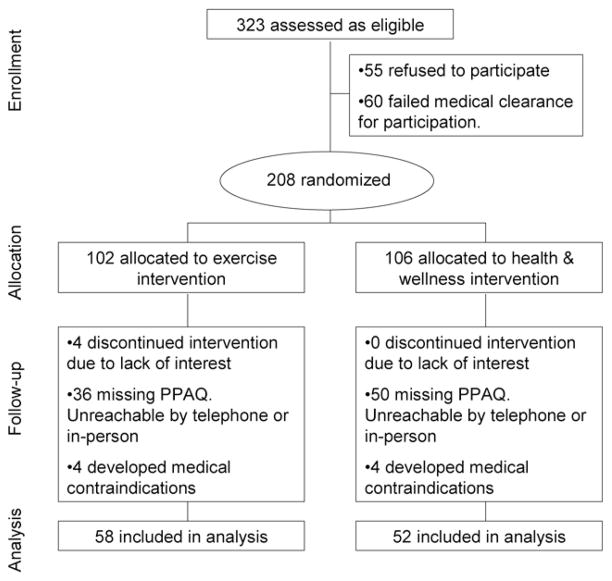
Demographic Characteristics
A total of 58 women were randomized to the exercise intervention and 52 women to the health and wellness intervention at a mean of 11.9 weeks gestation (Figure 1). Overall, participants (n = 110, 60% Hispanic) were predominantly young (51% less than or equal to age 24), overweight/obese (98%), unmarried (75%), and of low income (56% ≤ $30,000/year) (Table 1). While 31% of participants smoked before pregnancy, this percentage decreased to 12% in early pregnancy. At baseline, the intervention arms did not differ according to sociodemographic or behavioral variables (Table 1). Women missing PPAQ data did not differ from women not missing this data, and no differences in missing data were seen between arms.
Figure 1.
Flow diagram; The Behaviors Affecting Baby and You (B.A.B.Y.) Study.
Table 1.
Baseline Characteristics of Participants; The B.A.B.Y. Study, 2007–2010
| Variables | Total (n = 110)
|
Exercise arm
|
Health & wellness arm
|
P-valueb | |||
|---|---|---|---|---|---|---|---|
| na | % | n | % | n | % | ||
| Age (years) | |||||||
| 16–24 | 57 | 51.8 | 34 | 58.6 | 23 | 44.2 | 0.39 |
| 25–29 | 23 | 20.9 | 11 | 19.0 | 12 | 23.1 | |
| 30–35 | 21 | 19.1 | 8 | 13.8 | 13 | 25.0 | |
| 35–40 | 9 | 8.2 | 5 | 8.6 | 4 | 7.7 | |
| Ethnicity | |||||||
| Non-Hispanic white | 41 | 39.8 | 24 | 44.4 | 17 | 34.7 | 0.31 |
| Hispanic | 62 | 60.2 | 30 | 55.6 | 32 | 65.3 | |
| BMI (kg/m2) | |||||||
| <18.5 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0.20 |
| 18.5 to <25 | 2 | 1.8 | 2 | 3.4 | 0 | 0.0 | |
| 25 to <30 | 44 | 40.4 | 20 | 34.5 | 24 | 47.1 | |
| ≥30 | 63 | 57.8 | 36 | 62.1 | 27 | 52.9 | |
| Education | |||||||
| Less than high school | 23 | 20.9 | 9 | 15.5 | 14 | 26.9 | 0.26 |
| High school graduate | 42 | 38.2 | 22 | 37.9 | 20 | 38.5 | |
| Post high school | 45 | 40.9 | 27 | 46.6 | 18 | 34.6 | |
| Household income | |||||||
| ≤$15,000 | 47 | 56.6 | 23 | 52.3 | 24 | 61.5 | 0.43d |
| >$15,000–$30,000 | 13 | 15.7 | 9 | 20.5 | 4 | 10.3 | |
| >$30,000 | 23 | 27.7 | 12 | 27.3 | 11 | 28.2 | |
| Marital status | |||||||
| Single/separated/divorced/widowed | 82 | 74.5 | 40 | 69.0 | 42 | 80.8 | 0.19 |
| Married | 28 | 25.5 | 18 | 31.0 | 10 | 19.2 | |
| Live with spouse/partner | |||||||
| No | 39 | 35.5 | 16 | 27.6 | 23 | 44.2 | 0.07 |
| Yes | 71 | 64.5 | 42 | 72.4 | 29 | 55.8 | |
| Prepregnancy cigarette smoking | |||||||
| No | 75 | 68.8 | 41 | 71.9 | 34 | 65.4 | 0.46 |
| Yes | 34 | 31.2 | 16 | 28.1 | 18 | 34.6 | |
| Early pregnancy cigarette smoking | |||||||
| No | 95 | 88.0 | 50 | 89.3 | 45 | 86.5 | 0.66 |
| Yes | 13 | 12.0 | 6 | 10.7 | 7 | 13.5 | |
| Adults (≥18 yrs) in householdc | |||||||
| 1 | 24 | 22.0 | 8 | 14.0 | 16 | 30.8 | 0.11 |
| 2 | 53 | 48.6 | 30 | 52.6 | 23 | 44.2 | |
| ≥3 | 32 | 29.4 | 19 | 33.3 | 13 | 25.0 | |
| Children (<18 yrs) in householdc | |||||||
| 0 | 23 | 21.1 | 13 | 22.8 | 10 | 19.2 | 0.44 |
| 1 | 48 | 44.0 | 28 | 49.1 | 20 | 38.5 | |
| 2 | 29 | 26.6 | 13 | 22.8 | 16 | 30.8 | |
| ≥3 | 9 | 8.3 | 3 | 5.3 | 6 | 11.5 | |
Numbers may not total to 110 due to missing data.
P-values from Chi-square tests for categorical variables or Fisher’s Exact test if the expected cell count was <5 (ie, age, marital status, early pregnancy smoking, and children in household).
Including the participant as appropriate: if <18 yrs, include as a child; if > 18 yrs, included as an adult.
Calculated after excluding participants who reported ‘Do not know.’
Physical Activity Findings
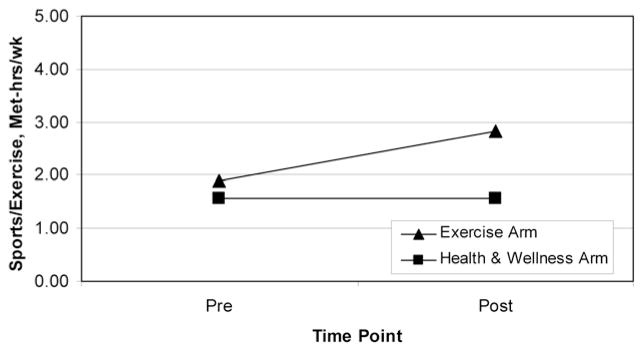
At baseline, the intervention arms did not differ according to mean total physical activity (ie, sports/exercise, household/care-giving, occupational, and transportation combined) with 49.2 MET-hrs/wk (SD = 21.5) in the exercise arm and 52.9 MET-hrs/wk (SD = 26.3) in the health and wellness arm, respectively (P = .42) (Table 2). After the 12-week intervention, the intervention arm experienced a smaller decrease in total physical activity (−1.0 MET-hrs/wk) as compared with the contact control arm (−10.0 MET-hrs/wk; P = .03) (Table 2, Figure 2).
Table 2.
Change in Physical Activity (MET-hrs/wk) from Pre- to Postintervention According to Intervention Arm; The B.A.B.Y. Study, 2007–2010
| Exercise arm (n = 58)
|
Health & wellness arm (n = 52)
|
P-valuea | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Preintervention
|
Postintervention
|
Change
|
Preintervention
|
Postintervention
|
Change
|
||||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | ||
| Summary scores | |||||||||||||
| Total MET-hrs/wk | 49.2 | 21.5 | 48.1 | 21.7 | −1.0 | 20.8 | 52.9 | 26.3 | 42.9 | 18.2 | −10.0 | 20.4 | 0.03 |
| By intensity | |||||||||||||
| Sedentary | 9.9 | 5.7 | 9.5 | 5.4 | −0.4 | 5.2 | 10.4 | 4.9 | 9.2 | 4.4 | −1.3 | 4.4 | 0.35 |
| Light | 19.1 | 8.9 | 20.4 | 9.1 | 1.3 | 9.8 | 21.8 | 11.4 | 19.6 | 9.4 | −2.2 | 9.8 | 0.06 |
| Moderate | 19.8 | 14.7 | 17.7 | 12.9 | −2.1 | 14.8 | 20.5 | 16.4 | 14.0 | 10.3 | −6.5 | 13.7 | 0.11 |
| Vigorous | 0.4 | 0.9 | 0.5 | 0.9 | 0.1 | 0.9 | 0.1 | 0.3 | 0.1 | 0.3 | 0.0 | 0.4 | 0.32 |
| Moderate + vigorous | 20.2 | 14.9 | 18.2 | 13.1 | −2.0 | 14.6 | 20.7 | 16.5 | 14.1 | 10.4 | −6.5 | 13.8 | 0.10 |
| By type | |||||||||||||
| Household/care-giving | 20.7 | 13.2 | 20.6 | 10.2 | −0.2 | 12.5 | 24.8 | 15.6 | 20.6 | 12.0 | −4.1 | 13.9 | 0.11 |
| Occupational | 14.2 | 12.5 | 11.2 | 12.7 | −3.1 | 14.8 | 13.0 | 14.9 | 8.8 | 10.1 | −4.2 | 11.4 | 0.65 |
| Sports/exercise | 1.9 | 2.2 | 2.8 | 2.2 | 0.9 | 2.2 | 1.6 | 1.4 | 1.6 | 1.9 | 0.0 | 2.0 | 0.02 |
| Transportation | 5.4 | 3.8 | 6.4 | 5.7 | 1.0 | 6.0 | 6.4 | 5.9 | 5.6 | 4.9 | −0.8 | 6.5 | 0.12 |
P-values calculated from 2 sample t tests for continuous variables.
Figure 2.
Mean sports/exercise by study arm and time point. At 12-weeks post intervention, exercise > contact control, P = .02; The Behaviors Affecting Baby and You (B.A.B.Y.) Study.
We then examined activity according to intensity (eg, sedentary, light, moderate, vigorous). While there were no significant between-arm differences, there was the suggestion of difference in change in light-intensity activity between the exercise arm (1.3 MET-hrs/wk, SD = 9.8) and the health and wellness arm (−2.19 MET-hrs/wk, SD = 9.8) (P = .06). Exercise intervention participants also reported an increase in vigorous intensity activity and a smaller decrease in moderate activity as compared with the health and wellness arm, although these between-arm differences were not statistically significant.
We then evaluated activity according to type (ie, household/care-giving, occupational, sports/exercise, and transportation). In the exercise arm, sports/exercise increased from 1.9 MET-hrs/wk (SD = 2.2) at baseline to 2.8 MET-hrs/wk (SD = 2.2) while sports/exercise stayed constant at 1.6 MET-hrs/wk in the health and wellness arm. The difference in change in exercise between the 2 arms (0.9 MET-hrs/wk vs. −0.01 MET-hrs/wk) was statistically significant (P = .02). As compared with the health and wellness arm, the exercise intervention arm also experienced smaller decreases in household/caregiving, occupational activity and an increase in transportation activity, but these between-arm differences were not statistically significant. Finally, in linear regression models, we observed no statistically significant effect modification of the treatment effect by BMI (overweight vs. obese) nor ethnicity (Hispanic vs. not Hispanic).
Changes in Associated Process Variables
Exercise intervention participants reported improvements in behavioral processes of change (mean = 0.37, SD = 0.95) while the health and wellness arm experienced a decrease (mean = −0.10, SD = 0.58) (Table 3). The exercise arm also experienced increases in cognitive processes of change (mean = 0.09, SD = 0.82) while the health and wellness arm experienced a decrease (mean = −0.19, SD = 0.69), but this was not statistically significant (P = .14). There were also no statistically significant differences between study arms in self-efficacy and decisional balance (benefits and costs) from pre to post intervention.
Table 3.
Change in Process Variables from Pre- to Postintervention According to Intervention Arm; The B.A.B.Y. Study, 2007–2010
| Exercise arm (n = 58)
|
Health & wellness arm (n = 52)
|
P-valuea | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Preintervention
|
Postintervention
|
Change
|
Preintervention
|
Postintervention
|
Change
|
||||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | ||
| Behavioral processes | 2.6 | 0.7 | 2.9 | 0.8 | 0.4 | 0.9 | 2.8 | 0.8 | 2.7 | 0.8 | −0.1 | 0.6 | 0.02 |
| Cognitive processes | 2.8 | 0.9 | 2.9 | 0.8 | 0.1 | 0.8 | 3.1 | 0.7 | 2.9 | 0.8 | −0.2 | 0.7 | 0.14 |
| Self-efficacy | 2.5 | 0.7 | 2.6 | 0.7 | 0.1 | 0.7 | 2.3 | 0.8 | 2.4 | 0.8 | 0.1 | 0.7 | 0.84 |
| Decisional balance pro | 3.5 | 0.9 | 3.4 | 1.0 | −0.1 | 0.8 | 3.7 | 0.9 | 3.7 | 0.9 | 0.0 | 0.8 | 0.71 |
| Decisional balance con | 2.2 | 0.7 | 2.3 | 0.9 | 0.1 | 0.8 | 2.5 | 0.7 | 2.5 | 0.8 | 0.0 | 0.8 | 0.76 |
P-values calculated from 2 sample t tests for continuous variables.
Feasibility and Acceptability
Of the 20 women in the exercise arm who completed the satisfaction survey (34%), 95% reported being satisfied with the amount of information received and 86% reported finding the study materials interesting and useful while the remaining 14% found the materials sometimes useful. The primary motivation for agreeing to participate in the study was to help to find ways to prevent GDM (100%) and to learn more about their pregnancy (95%). Approximately 29% of women found it sometimes difficult to find time to read the study materials and 14% found it sometimes difficult to access a telephone for the telephone interviews; 0% found it always difficult. Forty-three percent of women reported that other commitments (eg, children, work, family responsibilities) made it difficult or sometimes difficult for them to have time to participate in parts of the study. Finally, 95% of women reported that they would definitely or possibly participate in a similar study in the future.
Discussion
Because effective, innovative interventions are needed to address exercise during pregnancy, the current study examined the use of an individually tailored motivationally-matched exercise intervention in an ethnically diverse high-risk population of pregnant women. To our knowledge, this study represents one of the first randomized clinical trials of exercise during pregnancy among a sample including a significant proportion of Hispanic women. After the 12-week intervention, during a time period in which the majority of pregnant women experience an overall decrease in physical activity,53,54 women in the exercise intervention arm experienced a smaller decrease in total activity (−1.0 MET-hrs/wk, equivalent to 15 minutes of moderate activity per week) as compared with women in the health and wellness contact control arm (−10.0 MET-hrs/wk, equivalent to 2.5 hours per week of moderate intensity activity). More importantly, women in the exercise intervention experienced a significantly larger increase in sports/exercise (0.9 MET-hrs/wk, equivalent to 14 minutes per week) as compared with women in the health and wellness arm who experienced a slight decrease.
Other interesting findings included significant improvements in behavioral processes of change in the exercise arm relative to the health and wellness arm. Such processes of change are often followed by actual increases in physical activity behavior and serve as early indicators of change. Although the exercise intervention did not result in significantly increased cognitive processes of change, self-efficacy, and decisional balance, a 12-week program in the context of the rapidly changing context of pregnancy may not be long enough to have a substantial impact on such variables. And finally, the feasibility and acceptability of using this approach to promote physical activity in the target population was evidenced by the high retention and participant satisfaction with the program at 12 weeks.
Prior pregnancy exercise interventions that reported the impact of the intervention on change in physical activity are sparse. The majority of these prior trials were unable to counteract the spontaneous decrease in physical activity over the course of pregnancy,33–36 although a nonrandomized trial55 and a pilot study56 supported a positive effect. Gray-Donald et al conducted a nonrandomized trial of a diet and activity intervention including exercise/walking groups among 112 pregnant women in 4 Cree communities as compared with a historical control group (n = 107).34 Based on self-report of usual daily activities, sedentary activity was significantly higher at 27 weeks gestation in the intervention group (61%) as compared with the control group (23%, P < .001). Polley et al conducted a randomized controlled trial of a lifestyle intervention (including diet, exercise and weight gain advice) among 120 prenatal care patients in Pittsburgh.35 There was no difference in change in exercise level (measured via the Paffenbarger Exercise Questionnaire)57 from recruitment to 30 weeks (P > .8) between women in the intervention arm as compared with women receiving usual care. Aittasalo et al conducted a controlled trial in Finland comparing the integration of physical activity and dietary counseling into 3 maternity clinics (experimental group) as compared with usual care in 3 additional maternity clinics (control group).55 Among the 132 pregnant participants, no differences in total self-reported leisure time physical activity were found at 16 to 18 weeks gestation between experimental vs. control clinics. However, at 36 to 37 weeks gestation, the weekly duration of at least moderate-intensity physical activity was 154% (95% CI 16, 455) higher in the experimental compared with the control group.
Guelinckx et al conducted a randomized controlled trial of a lifestyle intervention comparing active education to a brochure among 195 white, obese pregnant women in Belgium.33 Physical activity, assessed via the Baecke questionnaire,58 decreased in all groups and there was no significant difference between study arm. Callaway et al conducted a pilot randomized controlled trial among 50 obese pregnant women in Australia who were randomized to an individualized exercise program or to usual care.56 Of the women in the exercise program, 73% achieved more than 900 kcal/week of exercise-based activity as measured by the PPAQ at 28 weeks gestation compared with 42% of the control group (P = .047) although this difference was attenuated and no longer statistically significant at 36 weeks. There was no statistically significant difference in weekly total activity (MET-hrs/week) between study arms. Overall, the majority of these studies were limited by lack of randomized designs, use of historical control groups, lack of statistical power, measures of physical activity not validated in the study population, and use of predominantly non-Hispanic white samples.
Limitations of the current study include reliance on a self-reported measure of physical activity. Past studies have documented high levels of acquiescent and socially desirable responses in Hispanic samples.59 However, the use of a validated questionnaire, bilingual interviewers blinded to study arm, and a relatively short period of recall may reduce the magnitude of misclassification. To the degree that this occurred, this would result in an underestimate of the impact of the exercise intervention and attenuate our findings toward the null. Therefore, our observation of the impact of the exercise intervention is likely an underestimate of the true potential of the exercise intervention.
A total of 36 of the women in the exercise arm and 50 of the women in the health and wellness arm were missing data on the PPAQ. The option to complete the enrollment process in one of multiple ways (ie, telephone, mail, in-person) was viewed as removing critical barriers to enrollment and retention. However, challenges to completion of the PPAQ included the fact that our study population was predominantly young, with low levels of education, and unmarried. Indeed prior studies suggest that approximately 40% of Hispanic young girls, especially in low income families, drop out of school by eighth grade, are frequently in partnered relationships, and begin childbearing early.60 Additional challenges included the finding that, among the potential participants who were not approached, the majority did not show for their scheduled prenatal care appointment or had rescheduled. Difficulty reaching participants by mail and telephone, and low attendance to prenatal visits may be due to personal and child sickness, domestic tasks, unanticipated employment opportunities, and partner restrictions.40 This is consistent with our findings from the satisfaction survey that 43% of women reported that other commitments (eg, children, work, family responsibilities) made it difficult or sometimes difficult for them to have time to participate in parts of the study. It is important to note, however, that women missing PPAQ data did not differ significantly in terms of sociodemographic and behavioral characteristics than women not missing this data.
The satisfaction survey was administered at the time of the 3rd assessment period in the third trimester. Some of the women had therefore not reached that point in pregnancy at the time of this analysis. To the extent that women who did not complete the survey differed in their opinions from women who completed the survey, feasibility findings should be interpreted with caution.
Participants were recruited from the ambulatory obstetrical practices of a large tertiary care facility in Western Massachusetts and were at high risk of GDM, but were otherwise healthy and free from medical contraindications. On average, the majority of women failed medical clearance due to spontaneous abortion (33%), threatened abortion (13%), history of preterm birth (13%), and morbid obesity (13%); the most common medical contraindications which developed over the study were spontaneous abortion (67%). In addition, because subjects were recruited at their prenatal care visits, we excluded, by definition, high-risk women who did not attend prenatal care. Therefore, our study population may reflect a select group. However, our study population includes a sizeable proportion of women who were at high risk based on socioeconomic factors and ethnicity. For example, statewide data for Hispanic births in Massachusetts indicate that 64.4% of Latinas in Massachusetts begin prenatal care in the first trimester and have a total of 9 or more visits.61 In the current study, women were eligible to participate up to and including 25 weeks gestation.
The study has several strengths. The B.A.B.Y. Study is novel in developing a culturally tailored exercise intervention for a multiethnic population. Prior intervention studies reporting on exercise in pregnancy have not included Hispanic women, a group with high rates of sedentary behavior.22 We observed no differences in the efficacy of the exercise intervention between Hispanic participants vs. non-Hispanic white participants. In designing our protocol, we focused on a high-reach, low cost strategy which included telephone assessment of the exercise outcome measures as well as only 1 face-to-face session, as opposed to multiple in-person individual or group meetings. Prior reviews indicate that the time and child care pressures that pregnant women report as barriers to physical activity62 indicate that the requirement to attend groups at scheduled times and to travel to and from venues would deter many. In contrast, our research group,29 as well as others,29,63,64 have found that individually-tailored lifestyle interventions delivered via a combination of in-person, telephone, and mail produce greater or comparable changes in behavior at a more cost efficient level compared with group-based interventions.
In summary, findings support the feasibility and efficacy of an exercise intervention designed to promote physical activity in a diverse sample of pregnant women. Such high-reach, low-cost approaches have great potential to positively affect public health and reduce health disparities. The intervention protocol can readily be translated into clinical practice in underserved and minority populations.
Acknowledgments
This work was supported by a grant (R01DK074876) from the National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health. This study is registered at www.clinicaltrials.gov (No. NCT00728377).
Contributor Information
Lisa Chasan-Taber, Dept of Public Health, University of Massachusetts, Amherst, MA.
Marushka Silveira, Dept of Public Health, University of Massachusetts, Amherst, MA.
Bess H. Marcus, Behavioral and Social Sciences Section, Brown University, Providence, RI
Barry Braun, Dept of Kinesiology, University of Massachusetts, Amherst, MA.
Edward Stanek, Dept of Public Health, University of Massachusetts, Amherst, MA.
Glenn Markenson, Dept of Maternal and Fetal Medicine, Baystate Medical Center, Springfield, MA.
References
- 1.Fortner R, Pekow P, Whitcomb B, Sievert L, Markenson G, Chasan-Taber L. Physical activity and hypertensive disorders of pregnancy among Hispanic women. Med Sci Sports Exerc. 2011;43(4):639–646. doi: 10.1249/MSS.0b013e3181f58d3e. [DOI] [PubMed] [Google Scholar]
- 2.Sorensen TK, Williams MA, Lee IM, Dashow EE, Thompson ML, Luthy DA. Recreational physical activity during pregnancy and risk of preeclampsia. Hypertension. 2003;41(6):1273–1280. doi: 10.1161/01.HYP.0000072270.82815.91. [DOI] [PubMed] [Google Scholar]
- 3.Gollenberg A, Pekow P, Bertone-Johnson E, Freedson P, Markenson G, Chasan-Taber L. Physical activity and risk of small-for-gestational-age birth among pre-dominantly Puerto Rican women. Matern Child Health J. 2011;15(1):49–59. doi: 10.1007/s10995-009-0563-1. [DOI] [PubMed] [Google Scholar]
- 4.Hegaard H, Pedersen B, Nielsen B, Damm P. Leisure time physical activity during pregnancy and impact on gestational diabetes mellitus, pre-eclampsia, preterm delivery and birth weight: a review. Acta Obstet Gynecol Scand. 2007;86(11):1290. doi: 10.1080/00016340701647341. [DOI] [PubMed] [Google Scholar]
- 5.Stuebe A, Oken E, Gillman M. Associations of diet and physical activity during pregnancy with risk for excessive gestational weight gain. American Journal of Obstetrics and Gynecology. 2009;201(1):58.e1–58.e8. doi: 10.1016/j.ajog.2009.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Olson CM, Strawderman MS. Modifiable behavioral factors in a biopsychosocial model predict inadequate and excessive gestational weight gain. J Am Diet Assoc. 2003;103(1):48–54. doi: 10.1053/jada.2003.50001. [DOI] [PubMed] [Google Scholar]
- 7.Oken E, Ning Y, Rifas-Shiman SL, Radesky JS, Rich-Edwards JW, Gillman MW. Associations of physical activity and inactivity before and during pregnancy with glucose tolerance. Obstet Gynecol. 2006;108(5):1200–1207. doi: 10.1097/01.AOG.0000241088.60745.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhang C, Solomon CG, Manson JE, Hu FB. A prospective study of pregravid physical activity and sedentary behaviors in relation to the risk for gestational diabetes mellitus. Arch Intern Med. 2006;166(5):543–548. doi: 10.1001/archinte.166.5.543. [DOI] [PubMed] [Google Scholar]
- 9.Chasan-Taber L, Schmidt MD, Pekow P, et al. Physical activity and gestational diabetes mellitus among hispanic women. J Womens Health (Larchmt) 2008;17(6):999–1008. doi: 10.1089/jwh.2007.0560. [DOI] [PubMed] [Google Scholar]
- 10.Kjos SL. Postpartum care of the woman with diabetes. Clin Obstet Gynecol. 2000;43(1):75–86. doi: 10.1097/00003081-200003000-00008. [DOI] [PubMed] [Google Scholar]
- 11.Schmidt MI, Duncan BB, Reichelt AJ, et al. Brazilian Gestational Diabetes Study Group. Gestational diabetes mellitus diagnosed with a 2-h 75-g oral glucose tolerance test and adverse pregnancy outcomes. Diabetes Care. 2001;24(7):1151–1155. doi: 10.2337/diacare.24.7.1151. [DOI] [PubMed] [Google Scholar]
- 12.Naylor CD, Sermer M, Chen E, Sykora K. Cesarean delivery in relation to birth weight and gestational glucose tolerance: Pathophysiology or practice style? Toronto tri-hospital gestational diabetes investigators. JAMA. 1996;275(15):1165–1170. [PubMed] [Google Scholar]
- 13.Magee MS, Walden CE, Benedetti TJ, Knopp RH. Influence of diagnostic criteria on the incidence of gestational diabetes and perinatal morbidity. JAMA. 1993;269(5):609–615. [PubMed] [Google Scholar]
- 14.Pettitt DJ, Knowler WC. Long-term effects of the intrauterine environment, birth weight, and breast-feeding in Pima Indians. Diabetes Care. 1998;21(Suppl 2):B138–B141. [PubMed] [Google Scholar]
- 15.Silverman BL, Rizzo TA, Cho NH, Metzger BE. Long-term effects of the intrauterine environment. the northwestern university diabetes in pregnancy center. Diabetes Care. 1998;21(Suppl 2):B142–B149. [PubMed] [Google Scholar]
- 16.Vohr BR, McGarvey ST, Tucker R. Effects of maternal gestational diabetes on offspring adiposity at 4–7 years of age. Diabetes Care. 1999;22(8):1284–1291. doi: 10.2337/diacare.22.8.1284. [DOI] [PubMed] [Google Scholar]
- 17.ACOG Committee Obstetric Practice. ACOG committee opinion. number 267, January 2002: exercise during pregnancy and the postpartum period. Obstet Gynecol. 2002;99(1):171–173. doi: 10.1016/s0029-7844(01)01749-5. [DOI] [PubMed] [Google Scholar]
- 18.U.S. Department of Health and Human Services. 2008 Physical Activity Guidelines for Americans. July. U.S. Department of Health and Human Services; 2011. pp. 1–61. [Google Scholar]
- 19.Haskell WL, Lee IM, Pate RR, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39(8):1423–1434. doi: 10.1249/mss.0b013e3180616b27. [DOI] [PubMed] [Google Scholar]
- 20.Evenson K, Wen F. National trends in self-reported physical activity and sedentary behaviors among pregnant women: NHANES 1999–2006. Prev Med. 2010;50(3):123–128. doi: 10.1016/j.ypmed.2009.12.015. [DOI] [PubMed] [Google Scholar]
- 21.Gollenberg A, Pekow P, Markenson G, Tucker K, Chasan-Taber L. Dietary behaviors, physical activity, and cigarette smoking among pregnant puerto rican women. Am J Clin Nutr. 2008;87(6):1844–1851. doi: 10.1093/ajcn/87.6.1844. [DOI] [PubMed] [Google Scholar]
- 22.Giardina E, Laudano M, Hurstak E, et al. Physical activity participation among Caribbean Hispanic women living in New York: relation to education, income, and age. J Womens Health (Larchmt) 2009;18(2):187–193. doi: 10.1089/jwh.2008.0946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zambrana RE, Logie LA. Latino child health: need for inclusion in the US national discourse. Am J Public Health. 2000;90(12):1827–1833. doi: 10.2105/ajph.90.12.1827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.National Center for Health Statistics. CDC growth charts, United States; 2000. September 9, 2010;February 13, 2011.
- 25.Centers for Disease Control and Prevention (CDC) Prevalence of physical activity, including lifestyle activities among adults–United States, 2000–2001. MMWR Morb Mortal Wkly Rep. 2003;52(32):764–769. [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention (CDC) Health disparities experienced by Hispanics–United States. Morbidity and Mortality Weekly Report. 2004;53(40):935–937. [PubMed] [Google Scholar]
- 27.U.S. Department of Commerce Economics and Statistics Administration. US Census Bureau. The American Community—Hispanics: 2004. 2007. [Google Scholar]
- 28.Misra D. The women’s health data book. 3. Washington, DC: Jacob’s Women’s Health Institute; 2001. [Google Scholar]
- 29.Marcus BH, Lewis BA, Williams DM, et al. A comparison of internet and print-based physical activity interventions. Arch Intern Med. 2007;167(9):944–949. doi: 10.1001/archinte.167.9.944. [DOI] [PubMed] [Google Scholar]
- 30.Marcus BH, Lewis BA, Williams DM, et al. Step into motion: a randomized trial examining the relative efficacy of internet vs. print-based physical activity interventions. Contemp Clin Trials. 2007;28(6):737–747. doi: 10.1016/j.cct.2007.04.003. [DOI] [PubMed] [Google Scholar]
- 31.Marcus BH, Napolitano MA, King AC, et al. Telephone versus print delivery of an individualized motivationally tailored physical activity intervention: Project STRIDE. Health Psychology: Official Journal of the Division of Health Psychology, American Psychological Association. 2007;26(4):401–409. doi: 10.1037/0278-6133.26.4.401. [DOI] [PubMed] [Google Scholar]
- 32.Marcus BH, Napolitano MA, King AC, et al. Examination of print and telephone channels for physical activity promotion: Rationale, design, and baseline data from project STRIDE. Contemp Clin Trials. 2007;28(1):90–104. doi: 10.1016/j.cct.2006.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Guelinckx I, Devlieger R, Mullie P, Vansant G. Effect of lifestyle intervention on dietary habits, physical activity, and gestational weight gain in obese pregnant women: a randomized controlled trial. Am J Clin Nutr. 2010;91(2):373–380. doi: 10.3945/ajcn.2009.28166. [DOI] [PubMed] [Google Scholar]
- 34.Gray-Donald K, Robinson E, Collier A, David K, Renaud L, Rodrigues S. Intervening to reduce weight gain in pregnancy and gestational diabetes mellitus in Cree communities: an evaluation. Canadian Medical Association Journal = Journal De l’Association Medicale Canadienne. 2000;163(10):1247–1251. [PMC free article] [PubMed] [Google Scholar]
- 35.Polley BA, Wing RR, Sims CJ. Randomized controlled trial to prevent excessive weight gain in pregnant women. International Journal of Obesity and Related Metabolic Disorders. Journal of the International Association for the Study of Obesity. 2002;26(11):1494–1502. doi: 10.1038/sj.ijo.0802130. [DOI] [PubMed] [Google Scholar]
- 36.Kinnunen TI, Pasanen M, Aittasalo M, et al. Preventing excessive weight gain during pregnancy—a controlled trial in primary health care. Eur J Clin Nutr. 2007;61(7):884–891. doi: 10.1038/sj.ejcn.1602602. [DOI] [PubMed] [Google Scholar]
- 37.Phelan S. Pregnancy: A “teachable moment” for weight control and obesity prevention. American Journal of Obstetrics and Gynecology. 2010;202(2):135.e1–135.e8. doi: 10.1016/j.ajog.2009.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2004;27(Suppl 1):S5–S10. doi: 10.2337/diacare.27.2007.s5. [DOI] [PubMed] [Google Scholar]
- 39.Chasan-Taber L, Marcus B, Stanek E, et al. A randomized controlled trial of prenatal physical activity to prevent gestational diabetes: design and methods. J Womens Health (Larchmt) 2009;18(6):851–859. doi: 10.1089/jwh.2008.1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chasan-Taber L, Fortner RT, Hastings V, Markenson G. Strategies for recruiting hispanic women into a prospective cohort study of modifiable risk factors for gestational diabetes mellitus. BMC Pregnancy Childbirth. 2009;9:57. doi: 10.1186/1471-2393-9-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- 42.Prochaska JO, DiClemente CC, Velicer WF, Rossi JS. Standardized, individualized, interactive, and personalized self-help programs for smoking cessation. Health Psychology: Official Journal of the Division of Health Psychology, American Psychological Association. 1993;12(5):399–405. doi: 10.1037//0278-6133.12.5.399. [DOI] [PubMed] [Google Scholar]
- 43.Bandura A. Self-efficacy: the exercise of control. New York: Freeman; 1997. [Google Scholar]
- 44.The American College of Obstetricians and Gynecologists. Exercise during pregnancy. Atlanta, GA: ACOG Distribution Center; 2010. [Google Scholar]
- 45.Marcus BH, Rossi JS, Selby VC, Niaura RS, Abrams DB. The stages and processes of exercise adoption and maintenance in a worksite sample. Health Psychology: Official Journal of the Division of Health Psychology, American Psychological Association. 1992;11(6):386–395. doi: 10.1037//0278-6133.11.6.386. [DOI] [PubMed] [Google Scholar]
- 46.Marcus BH, Selby VC, Niaura RS, Rossi JS. Self-efficacy and the stages of exercise behavior change. Res Q Exerc Sport. 1992;63(1):60–66. doi: 10.1080/02701367.1992.10607557. [DOI] [PubMed] [Google Scholar]
- 47.Marcus BH, Rakowski W, Rossi JS. Assessing motivational readiness and decision making for exercise. Health Psychology: Official Journal of the Division of Health Psychology, American Psychological Association. 1992;11(4):257–261. doi: 10.1037//0278-6133.11.4.257. [DOI] [PubMed] [Google Scholar]
- 48.Marcus BH, Bock BC, Pinto BM, Forsyth LH, Roberts MB, Traficante RM. Efficacy of an individualized, motivationally- tailored physical activity intervention. Annals of Behavioral Medicine: A Publication of the Society of Behavioral Medicine. 1998;20(3):174–180. doi: 10.1007/BF02884958. [DOI] [PubMed] [Google Scholar]
- 49.Marcus BH, Emmons KM, Simkin-Silverman LR, et al. Evaluation of motivationally tailored vs. standard self-help physical activity interventions at the workplace. American Journal of Health Promotion: AJHP. 1998;12(4):246–253. doi: 10.4278/0890-1171-12.4.246. [DOI] [PubMed] [Google Scholar]
- 50.Chasan-Taber L, Schmidt MD, Roberts DE, Hosmer D, Markenson G, Freedson PS. Development and validation of a pregnancy physical activity questionnaire. Medicine and Science in Sports and Exercise. 2004;36(10):1750–6. doi: 10.1249/01.mss.0000142303.49306.0d. quiz 1757–60. [DOI] [PubMed] [Google Scholar]
- 51.Ainsworth BE, Haskell WL, Whitt MC, et al. Compendium of physical activities: An update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32(9, Suppl):S498–S504. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- 52.Marcus BH, Banspach SW, Lefebvre RC, Rossi JS, Carleton RA, Abrams DB. Using the stages of change model to increase the adoption of physical activity among community participants. American Journal of Health Promotion: AJHP. 1992;6(6):424–429. doi: 10.4278/0890-1171-6.6.424. [DOI] [PubMed] [Google Scholar]
- 53.Chasan-Taber L, Schmidt MD, Pekow P, Sternfeld B, Manson J, Markenson G. Correlates of physical activity in pregnancy among Latina women. Matern Child Health J. 2007;11(4):353–363. [Google Scholar]
- 54.Schmidt MD, Pekow P, Freedson PS, Markenson G, Chasan-Taber L. Physical activity patterns during pregnancy in a diverse population of women. Journal of Women’s Health. 2006;15(8):909–918. doi: 10.1089/jwh.2006.15.909. [DOI] [PubMed] [Google Scholar]
- 55.Aittasalo M, Pasanen M, Fogelholm M, Kinnunen T, Ojala K, Luoto R. Physical activity counseling in maternity and child health care—a controlled trial. BMC Womens Health. 2008;8:14. doi: 10.1186/1472-6874-8-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Callaway L, Colditz P, Byrne N, et al. Prevention of gestational diabetes: feasibility issues for an exercise intervention in obese pregnant women. Diabetes Care. 2010;33(7):1457. doi: 10.2337/dc09-2336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Paffenbarger RS, Hyde RT, Wing AL, Hsieh CC. Physical activity, all-cause mortality, and longevity of college alumni. N Engl J Med. 1986;314(10):605. doi: 10.1056/NEJM198603063141003. [DOI] [PubMed] [Google Scholar]
- 58.Baecke JA, Burema J, Frijters JE. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Am J Clin Nutr. 1982;36(5):936–942. doi: 10.1093/ajcn/36.5.936. [DOI] [PubMed] [Google Scholar]
- 59.Marín G, Marín BV. Research with Hispanic populations. Newbury Park, CA: Sage Publications; 1991. [Google Scholar]
- 60.Lindenberg CS, Strickland O, Solorzano R, Galvis C, Dreher M, Darrow VC. Correlates of alcohol and drug use among low-income Hispanic immigrant childbearing women living in the USA. Int J Nurs Stud. 1999;36(1):3–11. doi: 10.1016/s0020-7489(98)00046-7. [DOI] [PubMed] [Google Scholar]
- 61.Averbach AR, Judge C, Orejuela M, et al. Hispanic births in Massachusetts 1996–1997. 2001. [Google Scholar]
- 62.Marquez D, Bustamante E, Bock B, Markenson G, Tovar A, Chasan-Taber L. Perspectives of Latina and non-Latina white women on barriers and facilitators to exercise in pregnancy. Women Health. 2009;49(6):505–521. doi: 10.1080/03630240903427114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Smith B, Cheung NW, Bauman A, Zehle K, McLean M. Postpartum physical activity and related psychosocial factors among women with recent gestational diabetes mellitus. Diabetes Care. 2005;28(11):2650–2654. doi: 10.2337/diacare.28.11.2650. [DOI] [PubMed] [Google Scholar]
- 64.Cardinal BJ, Sachs ML. Effects of mail-mediated, stage-matched exercise behavior change strategies on female adults’ leisure-time exercise behavior. J Sports Med Phys Fitness. 1996;36(2):100–107. [PubMed] [Google Scholar]