Abstract
Fecal incontinence is a challenging condition in that it exerts various psychosocial impacts on daily life. Different treatment modalities have been suggested for fecal incontinence. The present study aimed to evaluate the efficacy of biofeedback therapy in combination with surgery in the management of fecal incontinence.
The present randomized controlled trial was performed on 27 women with a complaint of fecal incontinence because of delivery trauma. The patients underwent sphincteroplasty and levatorplasty via the same method by 2 colorectal surgeons. In Group I, biofeedback therapy was performed 3 months before and 6 months after the surgery; in Group II, biofeedback therapy was applied only 6 months after the surgery; and in Group III, only surgical management was performed.
The results revealed a significant difference between the preoperative and postoperative Wexner scores of incontinence in all the 3 groups. Additionally, the difference between the preoperative and postoperative scores was significant only in Group I and Group III, but not in Group II. The reduction in the Wexner score was significantly less in Group III. However, no significant difference was observed between the 3 groups concerning the mean difference of preoperative and postoperative manometry.
The present study revealed no significant role for biofeedback therapy alone in the improvement of manometric evaluation. However, the Wexner score, which is an indicator of patient satisfaction, increased with biofeedback therapy following sphincteroplasty.
In general, surgical treatment is now reserved for selected patients with fecal incontinence and has recently been developed with biofeedback therapy. Trial Registration Number: IRCT201206039936N1
Keywords: Fecal incontinence, Sphincteroplasty, Biofeedback
What’s Known
Fecal incontinence is more common in the elderly, but young people are also affected. It is also much more prevalent in women than in men of an identical age.
Biofeedback can help in 50-100% of patients with fecal incontinence and might improve the functional results of patients after sphincteroplasty. Moreover, it is an effective treatment for fecal incontinence and can enhance quality of life.
What’s New
Currently, there is no conclusive evidence for the effectiveness of biofeedback in the treatment of fecal incontinence in patients with significant sphincter defects.
The present study revealed no significant role for biofeedback therapy in the improvement of manometry in patients with fecal incontinence resulting from obstetric traumas in the short term (6 months).
Introduction
Fecal incontinence, defined as the loss of anal sphincter control, leads to the unwanted release of stool or gas. It is a physical and psychological handicap with devastating psychosocial impacts.1-4 Fecal incontinence is one of the most common causes of institutionalization in the elderly, and accounts for over $400,000,000 per year only for diapers.5
One of the major causes of fecal incontinence in women is vaginal delivery, resulting in anal sphincter injury. Transient fecal incontinence is reported in 25% of women after first vaginal delivery. Because of obstetric factors, the incidence of fecal incontinence reaches 3% after vaginal delivery.6
When an anatomic defect is present in the anal sphincter and conservative treatment has not been successful, surgical correction is preferred. Therefore, sphincteroplasty of the anal sphincter is the preferred primary surgical treatment.7-9 Although sphincteroplasty is the main treatment, its long-term results are not satisfying, with most of the patients again suffering from incontinence at long-term follow-up.2-10,11 Only 26 to 83% of the patients with obstetric sphincter injury experience good continence and intact muscle wrap after overlapping sphincteroplasty.12
Biofeedback can help in 50 to 100% of patients with fecal incontinence and may improve the functional results of patients after sphincteroplasty. Moreover, biofeedback is an effective treatment for fecal incontinence and improvement in quality of life.13
Biofeedback therapy has enhanced the quality of life for most patients with minor anatomical defects and functional abnormality. Anal sphincter function is augmented by muscle strengthening, conferring increased sensitivity, perception, and coordination.
The present study aimed to evaluate the efficacy of biofeedback therapy in combination with surgery in the management of fecal incontinence.
Patients and Methods
The present randomized controlled trial was registered in the Iranian Registry of Clinical Trials (Registration #IRCT 201206039936N1) and conducted in Shahid Faghihi Hospital, Shiraz, Iran, from 2011 to 2012. All patients who met the inclusion criterion and had none of the exclusion criteria were enrolled. Twenty-seven women aged between 18 and 65 years with a complaint of fecal incontinence because of delivery trauma were recruited (figure 1). All the women underwent surgery in Shahid Faghihi Hospital in 2012 and were included in the study after they signed a written informed consent form. The patients were allocated to 3 groups via the permuted block randomization method.
Figure 1.
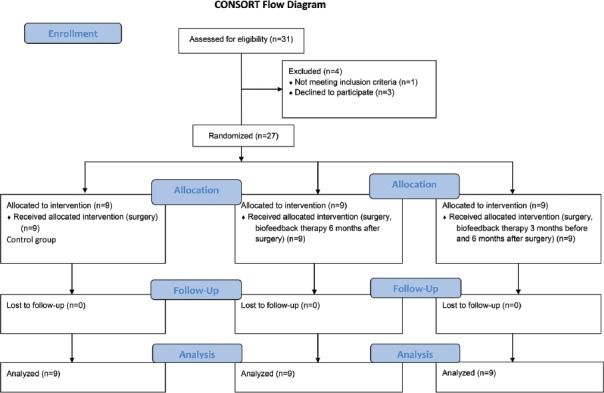
CONSORT flow diagram shows the allocation of the study population
The inclusion criterion was candidacy for sphincteroplasty due to having an anatomic anal sphincter defect after vaginal delivery more than 3 months previously or having an unsuccessful trial of pelvic-floor physical therapy. The exclusion criteria comprised planning for future vaginal childbirth; having a medical history of diabetic or neuromuscular disorders, pelvic surgery, pelvic irradiation, inflammatory bowel disease, and previous surgery on the anal sphincter; and fecal incontinence before delivery. All the patients were asked to complete the Wexner scale scoring system of incontinence at baseline. The scale consisted of items about the frequency of incontinence to feces or gas, and the results were expressed as a fecal incontinence score (Wexner score), as was described by Jorge and Wexner.2,14 The continence score ranged from 0 to 20, with higher scores representing more severe incontinency. Anoscopy, anal manometry, and endoanal sonography were done for all the patients before the operation: They had anal sphincter defects between 30 and 90° on endoanal sonography, with anal resting pressures <30 cm H2O and Wexner scores >10. Follow-up evaluation was performed after 6 months using the scoring system and manometry (anal resting pressure, anal maximum squeezing pressure, and mean pressure).
The patients underwent sphincteroplasty and levatorplasty via the same method by 2 colorectal surgeons. In Group I, biofeedback therapy was performed 3 months before and 6 months after the surgery. In Group II, biofeedback therapy was applied only 6 months after the surgery. In Group III, only surgical management (sphincteroplasty and levatorplasty) was done without any biofeedback exercises.15 Biofeedback therapy was performed by 1 specialist nurse of stomal therapy and continence. First, the specialist nurse described the position for biofeedback exercise (left lateral). Next, she asked the patients to perform a series of ten 5-second contractions of the anal canal, and checked that the contractions were done through the anal canal sphincter not though the buttock muscles. The patients were encouraged to perform 100 contractions twice a day at home. In addition, they were trained regarding high fiber diet, fluid therapy, posture during defecation, and body exercise.13
This study was approved by the Ethics Committee of Shiraz University of Medical Sciences, Shiraz, Iran, and was registered in the Iranian Registry of Clinical Trials (Registration #IRCT201206039936N1). This study was triple-blinded (patient, physician, and analyst). The primary outcome of the study was the Wexner score, and the secondary outcome was manometry evaluation in patients needing sphincteroplasty and levatorplasty for fecal incontinence.16
The data are expressed as mean±SD or median (range) for the continuous variables and count (percentage) for the categorical ones. The statistical significance of differences in the continuous variables was determined using nonparametric equivalents of the analysis of variance (Kruskal–Wallis H test) or the Student t-test for the paired or unpaired data where appropriate. In addition, significance of differences in the categorical data was determined using the Fisher exact test or the chi-square test. A P<0.05 was considered statistically significant. All the statistical analyses were performed using Statistical Package for the Social Sciences (SPSS) for Windows, version 16.
Results
All the 27 patients were female at a mean age of 40.48±14.76 years. The mean duration of incontinence in our patients was 6.00±4.67 years, and the mean preoperative Wexner score was 15.10±2.13. The baseline clinical characteristics of the patients in each group are presented in table 1.
Table 1.
Baseline characteristics of the study population
| Group I | Group II | Group III | P value | |
|---|---|---|---|---|
| Age (year) | 41.10 (13.12) | 36.80 (16.45) | 44.85 (15.32) | 0.426 |
| Duration of incontinence (year) | 8.40 (5.58) | 5.10 (4.04) | 3.85 (2.65) | 0.199 |
*P values are based on the Kruskal–Wallis H test to compare the baseline characteristics between the 3 groups
Our results revealed a significant difference between the preoperative and postoperative Wexner scores and anal resting pressure in all the 3 groups. Additionally, the differences between the preoperative and postoperative anal maximum squeezing pressure and mean pressure were significant only in Group I and Group III, but not in Group II (table 2).
Table 2.
Differences between the preoperative and postoperative values in each group
| Group I | Group II | Group III | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Preoperative | Postoperative | P value | Preoperative | Postoperative | P value | Preoperative | Postoperative | P value | |
| Wexner score | 15.10 (2.13) | 3.40 (2.01) | 0.005** | 15.70 (2.71) | 4.40 (3.33) | 0.005** | 15.00 (3.41) | 12.00 (3.05) | 0.024** |
| ARD | 10.50 (8.19) | 22.30 (10.60) | 0.007** | 11.00 (7.78) | 19.70 (4.83) | 0.008** | 9.57 (9.58) | 13.42 (9.19) | 0.027** |
| AMD | 37.40 (14.39) | 52.80 (15.75) | 0.012** | 55.00 (20.19) | 63.00 (12.21) | 0.139 | 36.14 (18.16) | 40.42 (17.13) | 0.018** |
| MEAN | 11.30 (8.40) | 25.10 (11.34) | 0.005** | 20.80 (14.36) | 24.30 (5.18) | 0.541 | 10.28 (9.19) | 15.71 (9.62) | 0.018** |
*P values are based on the MannWhitney U test to compare the preoperative and postoperative values in each group.
Statistically significant difference exists. ARD: Anal resting pressure; AMD: Anal maximum squeezing pressure; MEAN: Mean pressure
As is depicted in table 3, the reduction in the Wexner score was significantly lower in Group III. However, no significant differences were observed between the 3 groups concerning the mean difference of preoperative and postoperative anal resting pressure, anal maximum squeezing pressure, and mean pressure.
Table 3.
Comparison of the mean differences between the preoperative and postoperative values
| Group I | Group II | Group III | P value | |
|---|---|---|---|---|
| Wexner score | 11.70 (2.45) | 11.30 (4.13) | 3.00 (1.52) | 0.000** |
| ARD | −11.80 (9.60) | −8.70 (5.75) | −3.85 (3.38) | 0.106 |
| AMD | −15.40 (11.72) | −8.00 (16.68) | −4.28 (2.69) | 0.154 |
| MEAN | −13.80 (10.65) | −3.50 (14.05) | −5.42 (3.59) | 0.145 |
*P values are based on the Kruskal–Wallis H test to compare the changes in the preoperative and postoperative values between the 3 groups.
Statistically significant difference exists. ARD: Anal resting pressure; AMD: Anal maximum squeezing pressure; MEAN: Mean pressure
Discussion
Fecal incontinence is a challenging condition because of its various psychosocial impacts on daily life and quality of life. Sphincteroplasty is the best choice for patients with incontinence. It is aimed at treating the defects of the anterior sphincter, similar to what happens in obstetric trauma, and restoring the anatomy of the anal sphincter.17 Nevertheless, some patients continue to have the symptoms of incontinence even after sphincteroplasty.18 Studies have shown that the results of sphincteroplasty deteriorate over time.3
In 1974, Engel, Nikoomanesh, and Schuster19 described biofeedback for fecal incontinence for the first time. Anorectal biofeedback is a technique for increasing patients’ awareness of the physiological process and is deemed a safe option for alleviating their symptoms and enhancing their quality of life.20 Several studies have suggested anorectal biofeedback as a useful, first-line therapy for fecal incontinence, constipation, and chronic pelvic pain.20 Additionally, biofeedback training has led to significant reductions in the severity and duration of fecal incontinence.15 Biofeedback seems to be helpful for patients with persistent fecal incontinence after sphincteroplasty, but its mechanism of success is not clear.18 Some studies have demonstrated that sensory thresholds, but not resting or squeeze pressure, are improved by biofeedback. Also, a theory suggests that biofeedback helps by increasing the sensory awareness of the anorectal function.18
In the current study, the Wexner score and manometric parameters were improved in almost all the groups (except for anal maximum squeezing pressure and mean pressure in Group II) after the surgery. Moreover, the improvement in the Wexner score was significantly higher with biofeedback therapy (Group I and Group II). However, no significant differences were found between the 3 groups regarding the changes in the manometric parameters. Thus, the present study revealed no significant role for biofeedback therapy in the improvement of manometric parameters in the patients with fecal incontinence resulting from obstetric trauma in short term (6 months). However, the Wexner score, which is an indicator of patient satisfaction, increased with biofeedback therapy following sphincteroplasty.
Overall, studies have suggested that there is a serious need for powerful, randomized controlled trials to evaluate issues in incontinence therapy, such as surgery versus biofeedback, for the initial treatment of patients with sphincter defects.3 Currently, there is no conclusive evidence of the effectiveness of biofeedback in the treatment of fecal incontinence in patients with significant sphincter defects. Moreover, there is a paucity of high-quality data on the effectiveness of biofeedback therapy. Yet, biofeedback therapy is advised for most patients with fecal incontinence needing surgical or nonsurgical management. Finally, it seems that the successful treatment of these patients requires attention to each patient’s severity of incontinence because the available treatments range from medications and physical therapy to complex surgical procedures.
First and foremost among the limitations in the present study is its small sample size. Another weakness of note is that we did not perform nerve conduction velocity and electromyography.6 Therefore, more fundamental research should be conducted to advance the field of fecal incontinence therapy.
Conclusion
In general, surgical treatment is now reserved for moderate-to-severe fecal incontinence and recently developed treatments such as biofeedback should be individualized to the patient.
Acknowledgement
The present article was extracted from a research proposal (#3274) and was financially supported by the Research Vice Chancellorship of Shiraz University of Medical Sciences. The authors are grateful to Ms. A. Keivanshekouh at the Research Improvement Center of Shiraz University of Medical Sciences for improving the use of English in the manuscript.
Conflict of Interest: None declared.
References
- 1.Van Koughnett JA, Wexner SD. Current management of fecal incontinence: choosing amongst treatment options to optimize outcomes. World J Gastroenterol. 2013;19:9216–30. doi: 10.3748/wjg.v19.i48.9216. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jorge JM, Wexner SD. Etiology and management of fecal incontinence. Dis Colon Rectum. 1993;36:77–97. doi: 10.1007/BF02050307. [DOI] [PubMed] [Google Scholar]
- 3.Madoff RD. Surgical treatment options for fecal incontinence. Gastroenterology. 2004;126:S48–54. doi: 10.1053/j.gastro.2003.10.015. [DOI] [PubMed] [Google Scholar]
- 4.Baumgartner U. The artificial sphincter: therapy for faecal incontinence. Zentralbl Chir. 2012;137:340–4. doi: 10.1055/s-0032-1315109. [DOI] [PubMed] [Google Scholar]
- 5.Cheskin LJ, Schuster SM. Fecal incontinence. In: Hazzard WR, Andres R, Bierman EL, Blass JP, editors. Principles of geriatric medicine and gerontology. 2rd ed. New York: McGraw-Hill; 1990. pp. 1143–5. [Google Scholar]
- 6.Mahony R, Behan M, O’Connell PR, O’Herlihy C. Effect of second vaginal delivery on anal function in patients at risk of occult anal sphincter injury after first forceps delivery. Dis Colon Rectum. 2008;51:1361–6. doi: 10.1007/s10350-008-9302-8. [DOI] [PubMed] [Google Scholar]
- 7.Mevik K, Norderval S, Kileng H, Johansen M, Vonen B. Long-term results after anterior sphincteroplasty for anal incontinence. Scand J Surg. 2009;98:234–8. doi: 10.1177/145749690909800408. [DOI] [PubMed] [Google Scholar]
- 8.Novi JM, Mulvihill BH, Morgan MA. Combined anal sphincteroplasty and perineal reconstruction for fecal incontinence in women. J Am Osteopath Assoc. 2009;109:234–6. [PubMed] [Google Scholar]
- 9.Bharucha AE, Fletcher JG, Melton LJ, 3rd, Zinsmeister AR. Obstetric trauma, pelvic floor injury and fecal incontinence: a population-based case-control study. Am J Gastroenterol. 2012;107:902–11. doi: 10.1038/ajg.2012.45. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bravo Gutierrez A, Madoff RD, Lowry AC, Parker SC, Buie WD, Baxter NN. Long-term results of anterior sphincteroplasty. Dis Colon Rectum. 2004;47:727–31. doi: 10.1007/s10350-003-0114-6. discussion 31-2. [DOI] [PubMed] [Google Scholar]
- 11.Halverson AL, Hull TL. Long-term outcome of overlapping anal sphincter repair. Dis Colon Rectum. 2002;45:345–8. doi: 10.1007/s10350-004-6180-6. [DOI] [PubMed] [Google Scholar]
- 12.Wexner SD, Marchetti F, Jagelman DG. The role of sphincteroplasty for fecal incontinence reevaluated: a prospective physiologic and functional review. Dis Colon Rectum. 1991;34:22–30. doi: 10.1007/BF02050202. [DOI] [PubMed] [Google Scholar]
- 13.Byrne CM, Solomon MJ, Young JM, Rex J, Merlino CL. Biofeedback for fecal incontinence: short-term outcomes of 513 consecutive patients and predictors of successful treatment. Dis Colon Rectum. 2007;50:417–27. doi: 10.1007/s10350-006-0846-1. [DOI] [PubMed] [Google Scholar]
- 14.Azizi R, Alvandipour M, Shoar S, Mahjoubi B. Combination of pseudocontinent perineal colostomy and appendicostomy: a new approach in the treatment of low rectal cancer. Surg Innov. 2013;20:471–7. doi: 10.1177/1553350612469280. [DOI] [PubMed] [Google Scholar]
- 15.Heymen S, Scarlett Y, Jones K, Ringel Y, Drossman D, Whitehead WE. Randomized controlled trial shows biofeedback to be superior to pelvic floor exercises for fecal incontinence. Dis Colon Rectum. 2009;52:1730–7. doi: 10.1007/DCR.0b013e3181b55455. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang JY, Patterson TR, Hart SL, Varma MG. Fecal incontinence: does age matter? Characteristics of older vs. younger women presenting for treatment of fecal incontinence. Dis Colon Rectum. 2008;51:426–31. doi: 10.1007/s10350-007-9138-7. [DOI] [PubMed] [Google Scholar]
- 17.Bondurri A, Zbar AP, Tapia H, Boffi F, Pescatori M. The relationship between etiology, symptom severity and indications of surgery in cases of anal incontinence: a 25-year analysis of 1,046 patients at a tertiary coloproctology practice. Tech Coloproctol. 2011;15:159–64. doi: 10.1007/s10151-011-0682-8. [DOI] [PubMed] [Google Scholar]
- 18.Jensen LL, Lowry AC. Biofeedback improves functional outcome after sphincteroplasty. Dis Colon Rectum. 1997;40:197–200. doi: 10.1007/BF02054988. [DOI] [PubMed] [Google Scholar]
- 19.Engel BT, Nikoomanesh P, Schuster MM. Operant conditioning of rectosphincteric responses in the treatment of fecal incontinence. N Engl J Med. 1974;290:646–9. doi: 10.1056/NEJM197403212901202. [DOI] [PubMed] [Google Scholar]
- 20.Bartlett LM, Sloots K, Nowak M, Ho YH. Biofeedback therapy for faecal incontinence: a rural and regional perspective. Rural Remote Health. 2011;11:1630. [PubMed] [Google Scholar]


