Abstract
A uterocutaneous fistula is a rare clinical presentation that occurs following Cesarean section and other pelvic operations. There are only a few reports discussing the treatments. We describe a patient with successful surgical management and review the literature. A 25-year-old woman referred to our department 13 months after her first Cesarean section. She had a history of an abdominal mass and collection 2 months after surgery and some fistula opening with discharge from her previous incision. She had a previous surgical operation and antibiotic therapy without complete response. We performed fistulography to evaluate the tracts. In the operation — she had fistula tracts, one of which was between the uterus and skin. We debrided the necrotic tissue in the uterus, excised the fistula tracts, and drained the uterine cavity. At 8 months’ postoperative follow-up, she had no recurrence. A uterocutaneous fistula is a rare condition with many causes and needs proper investigation and timely medical and surgical management.
Keywords: Cutaneous fistula, Uterine diseases, Cesarean Section, Pregnancy
What’s Known
Most uterine fistulae are between the uterine and the bladder or bowel. A fistula is a communication between 2 epithelium-lined surfaces.
What’s New
Fistula between uterine and skin is a rare condition but should be considered with signs of inflammation after cesarean section.
Introduction
A fistula is a communication between two epithelium-lined surfaces. This abnormal connection occurs after traumas or other injuries or infections.1 Most uterine fistulae are between the uterine and the bladder or bowel (uterovesical or uterocolonic) due to postoperative injuries or infectious conditions.2 A uterocutaneous fistula (communication between uterine and skin) is a rare condition, and there are only a few reports in this regard in the existing literature. The causes include multiple surgeries, use of drains, and incomplete closure of the incisions. Because of the uncommon presentation of the uterocutaneous fistula, the exact treatment is challenging.3 We describe a patient with this kind of rare fistula after Cesarean section with multiple operations. Eventually, she had successful management of the fistula. Additionally, we discuss the diagnostic modalities and treatment options for uterocutaneos fistulae.
Case Presentation
A 25-year-old woman referred to our department with infected discharge at her previous Pfannenstiel incision. We obtained the patient’s consent to report the case. She had Cesarean section 13 months before with no early complications. Her baby was healthy. Two months afterward, she presented with an abdominal wall mass around the incision. In addition, she had pain and infected vaginal discharge. She was given medical treatment with antibiotics by her treating physician. Two months later, she had surgery for the drainage of her collection with a drain left in place. However, afterward she had discharge from other points in the incision line. Finally after 2 months, she was subjected to another surgery, consisting of wound exploration, excision of the fistula tract, and open drainage. Nevertheless, the discharge continued and she referred to our clinic. On examination, she had a Cesarean section scar in the suprapubic region with some holes with a pussy discharge.
We performed fistulography by injecting the contrast material from one of the holes in the skin (figure 1) under the guidance of computed tomography (CT) (figure 2). The radiologist reported 20×9 mm complex fistula tracts in the images. Ultrasound and cell blood count were normal. We decided to perform surgery. Intraoperatively, we first injected methylene blue dye from the fistula opening and followed the tracts in the skin and subcutaneous tissue, muscles, and peritoneal cavity. We thereafter debrided the necrotic tissues. We found the main route to the abdominal cavity, and then we did laparotomy and enterolysis. The tract ended in the anterior wall of the uterus. We debrided the whole necrotic tissue in the uterus and performed drainage with a catheter (#18).
Figure 1.

Contrast material is injected from one of the holes in the skin. It shows 20×9 mm complex fistula tracts.
Figure 2.
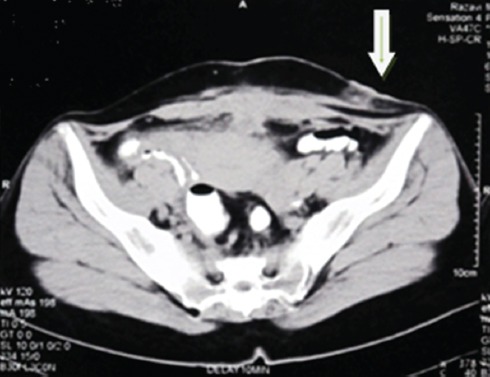
Computed tomography of the patient shows the collection site under the skin in the pelvis.
Pathological examination showed foreign body reaction, inflammatory necrosis of the uterine muscle, and a fistula tract in the muscular wall of the uterus with granulation tissue formation, hemorrhage, and fibrin deposition (figures 3 and 4). The patient recovered after surgery. At 8 months’ follow-up, she did not have recurrence or any gynecological problems.
Figure 3.
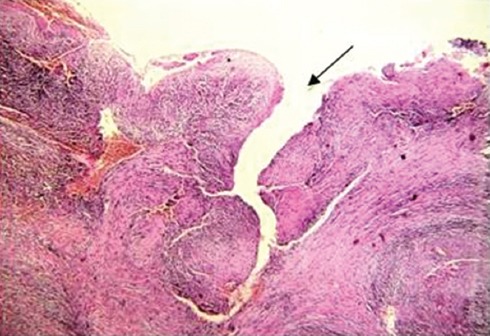
This figure shows the pathological examination of the debrided tissues with necrosis.
Figure 4.
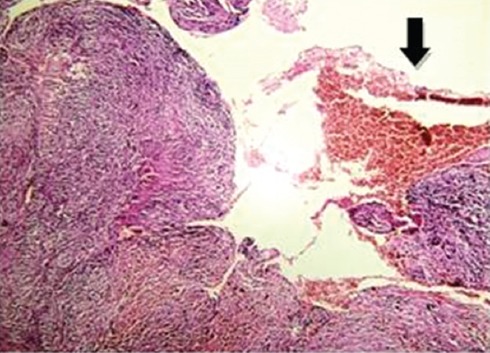
This slide shows the fistula tract in the muscular wall of the uterus with granulation tissue formation, hemorrhage, and fibrin deposition.
Discussion
Most of the fistulae in the uterus are uterovesical or uterocolonic. There are a large number of causes for the formation of uterocutaneous fistulae such as lower-segment type of Cesarean section, abdominal pregnancy, and high delivery. Inflammatory processes like the rupture of diverticulitis or sigmoid carcinoma into the bowel and uterus can lead to uterocolonic fistulae. Radiation therapy or traumas to the uterine wall during curettage can also cause this kind of fistula.2 Nonetheless, a uterocutaneous fistula is a very rare condition, whose pathophysiology is not fully understood but whose causes include multiple surgeries in the abdomen, use of drains, and in complete closure of incisions.3
Our patient had a fistula following Cesarean section, similar to the report by Dragoumis et al.4 In contrast, other reports have shown a similar presentation after septic abortion,1 pelvic abscesses,5 and true intra-abdominal pregnancy because of incomplete placenta removal.6 Uterovaginal malformation,7 infection with actinomycosis due to intrauterine devices,8 curettage, difficult vaginal delivery, or use of forceps may be the other causes.2
Our patient presented 2 months after surgery, but presentation tends to vary from 2 months to 6 years after the last surgery.3,4 Sometimes the patient has a clear finding like bloody discharge from the abdominal scar during the menstrual period; nevertheless, other investigations may be needed in some conditions such as pelvic pain or abdominal masses or abscesses. Fistulography with the injection of the contrast material through the skin opening shows the connection to the uterus.1,3 If the skin hole is too small in the case of a suspected uterocutaneous fistula, hysterosalpingography with a methylene blue injection via the cervix can be helpful.5 Magnetic resonance imaging with contrast is another modality.3
Thubert et al.3 believed that hysteroscopy is very helpful in detecting fistula opening in the uterine with its direct vision. We used fistulography and CT scan as diagnostic tools. Eldem et al.2 suggested that CT scan with an intravenous contrast and sagittal reconstructions may confer a prompt diagnosis.
Because a uterocutaneous fistula is a rare condition (fewer than 15 cases reported in the last 20 years worldwide),9 a standard treatment has yet to be introduced.
Previously, authors maintained that there was no nonsurgical treatment1 and the range of the surgeries varied from the excision of the fistula tract10 to hysterectomy,1,5 which presents a challenge in young patients. More recent reports, however, have introduced combined surgical and medical treatment for the reduction in the risk of hysterectomy.3 Seyhan et al.11 reported a patient treated with gonadotropin-releasing hormone agonist (GnRH) alone: the GnRH agonist induces atrophic changes in the epithelium and assists in the closure of the fistula. Nonetheless, a larger size of fistula opening in patients prompt surgeons to opt for the surgical approach.
Thubert et al.3 used medical treatment and minimally invasive surgery (laparoscopy) for the excision of a fistula tract. We injected methylene blue through the external opening of the patient’s skin to find the tracts and excise the fistula. Sonmezer et al.5 injected the blue dye from the cervix and internal opening and successfully treated their patients. Finally, we believe it is advisable that this kind of rare fistula be borne in mind if the patient has chronic pelvic pain secondary to a uterine abscess.2
Conclusion
Despite the uncommon presentation of a uterocutaneous fistula, it should be considered after Cesarean section, injury during operation, and abortion. All surgeonsshould follow uppatients with signs of inflammation. Fistulaeneed proper investigation and timely medical and surgical management such as antibiotics and drainage.
Acknowledgement
This work was supported by the Deputyship of Research, Mashhad University of Medical Sciences, Mashhad, Iran. It was performed in the Endoscopic and Minimally Invasive Surgery Research Center, Mashhad University of Medical Sciences. We specially thank Ms. Sima Beigoli for her assistance in preparing this article.
Conflict of Interest: None declared.
References
- 1.Gupta SK, Shukla VK, Varma DN, Roy SK. Uterocutaneous fistula. Postgrad Med J. 1993;69:822–3. doi: 10.1136/pgmj.69.816.822. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Eldem G, Turkbey B, Balas S, Akpinar E. MDCT diagnosis of uterocutaneous fistula. European Journal of Radiology Extra. 2008;67:e129–e30. doi: 10.1016/j.ejrex.2008.05.009. [DOI] [Google Scholar]
- 3.Thubert T, Denoiseux C, Faivre E, Naveau A, Trichot C, Deffieux X. Combined conservative surgical and medical treatment of a uterocutaneous fistula. J Minim Invasive Gynecol. 2012;19:244–7. doi: 10.1016/j.jmig.2011.10.010. [DOI] [PubMed] [Google Scholar]
- 4.Dragoumis K, Mikos T, Zafrakas M, Assimakopoulos E, Stamatopoulos P, Bontis J. Endometriotic uterocutaneous fistula after cesarean section. A case report. Gynecol Obstet Invest. 2004;57:90–2. doi: 10.1159/000075384. [DOI] [PubMed] [Google Scholar]
- 5.Sonmezer M, Sahincioglu O, Cetinkaya E, Yazici F. Uterocutaneous fistula after surgical treatment of an incomplete abortion: methylene blue test to verify the diagnosis. Arch Gynecol Obstet. 2009;279:225–7. doi: 10.1007/s00404-008-0683-7. [DOI] [PubMed] [Google Scholar]
- 6.Promsonthi P, Herabutya Y. Uterocutaneous fistula in term abdominal pregnancy. Eur J Obstet Gynecol Reprod Biol. 2007;132:239–41. doi: 10.1016/j.ejogrb.2006.04.041. [DOI] [PubMed] [Google Scholar]
- 7.Shukla D, Pandey S, Pandey LK, Shukla VK. Repair of uterocutaneous fistula. Obstet Gynecol. 2006;108:732–3. doi: 10.1097/01.AOG.0000188067.74163.40. [DOI] [PubMed] [Google Scholar]
- 8.Tedeschi A, Di Mezza G, D’Amico O, Ermann A, Montone L, Siciliano M, et al. A case of pelvic actinomycosis presenting as cutaneous fistula. Eur J Obstet Gynecol Reprod Biol. 2003;108:103–5. doi: 10.1016/S0301-2115(02)00361-5. [DOI] [PubMed] [Google Scholar]
- 9.Ruiz Arteaga JD, Valdez Murillo AN, Hernandez Trejo MC. Utero-cutaneous fistula: a case report and literature review. Ginecol Obstet Mex. 2012;80:95–8. [PubMed] [Google Scholar]
- 10.Okoro O, Onwere S. Retained products of conception in a utero cutaneous fistula: a case report. Niger J Clin Pract. 2008;11:170–1. [PubMed] [Google Scholar]
- 11.Seyhan A, Ata B, Sidal B, Urman B. Medical treatment of uterocutaneous fistula with gonadotropin-releasing hormone agonist administration. Obstet Gynecol. 2008;111:526–8. doi: 10.1097/01.AOG.0000281670.94265.5c. [DOI] [PubMed] [Google Scholar]


