Abstract
Introduction:
Intrauterine fetal death is an important indicator of maternal and perinatal health of a given population. This study was undertaken to study the maternal and fetal factors associated with intrauterine fetal death.
Materials and Methods:
This was a retrospective single center study. The details were entered in a preformed proforma. The details of complaints at admission, obstetrics history, menstrual history, examination findings, per vaginal examination findings, mode of delivery and fetal outcomes, placental examination, condition of cord and investigation reports were recorded.
Results:
A total of 250 intrauterine fetal deaths were reported amongst 6942 deliveries conducted during the study period. The incidence rate of intrauterine fetal death was 36/1000 live births. Two hundred and twenty-two deliveries were unbooked and unsupervised. The other observations were rural population (58%), low socioeconomic group (71.2%), previous stillbirth (9.2%), gestational hypertension (32.8%), anemia (74.4%), antepartum hemorrhage (18.8%), and congenital malformations (CMFs) (8.8%).
Conclusions:
The incidence of intrauterine fetal deaths in our population is higher than that reported from developed countries. This is associated with anemia, pregnancy-induced hypertension, illiteracy, low socioeconomic status, and higher incidence of undiagnosed CMFs.
Keywords: Gestational hypertension, intrauterine fetal death, maternal conditions
INTRODUCTION
Fetal death is an obstetric death accounting for approximately half of perinatal death. Stillbirth is an event which has always challenged the obstetricians. The mode of antenatal care has changed in past 50 years. The mode of antepartum and intrapartum surveillance for fetal wellbeing has advanced in last few decades. There are so many maternal conditions and diseases that are responsible for poor obstetrical outcomes. Stillbirth is a useful index to measure the values of antenatal and intranatal care. By proper antenatal check-ups, the high-risk cases associated with poor outcomes can be identified. The aim of this study was to analyze the maternal conditions associated with fetal death with specific reference to clinical presentations, fetal, and maternal complications and to find the preventable causes of fetal death.
MATERIALS AND METHODS
This was a single-center retrospective study of intrauterine fetal death and associated maternal conditions. The details were entered in a preformed proforma. The details of complaints at admission, obstetrics history, menstrual history, examination findings, per vaginal examination findings, mode of delivery and fetal outcomes, placental examination, condition of cord and investigation reports were recorded. The records of babies born below 28 weeks of gestation, fetus weighing below 1000 g and twin babies were excluded. The complaints included a period of amenorrhea, duration of labor pains, history of leaking, bleeding per vaginum (PV), pregnancy induced hypertension (PIH) or eclampsia, decreased or loss of fetal movements. The obstetrical history included parity, abortions, stillbirth, neonatal death, lower segment cesarian section (LSCS), preterm delivery, antipartum hemorrhage (APH) or PIH in a previous pregnancy. The records of per vaginal findings included bleeding PV, dilatation of the cervix, effacement of the cervix, presenting part, membrane, pelvis, hand prolapse, or cord prolapse. The details of the mode of delivery included vaginal delivery, LSCS, forceps, and laparotomy. Fetal outcomes recorded included fresh/macerated stillbirth, sex of the baby, weight, congenital malformations (CMFs), and birth injuries. Findings of placenta like infarction, calcification, and retroperitoneal clot and of conditions of the cord like knots, cord around neck, and any other abnormality were also recorded.
RESULTS
The present study consisted of 250 cases of intrauterine fetal death or stillbirths which occurred during the study period. A total of 6942 deliveries were conducted during this study period. The stillbirth rate was 36 per 1000 births. Of 250, 118 (47.2%) were premature and 132 (52.8%) were mature. One hundred and eight-seven were fresh stillbirths and 63 were macerated. Two hundred and twenty mothers (88%) were immunized with tetanus toxoid and 30 (12%) were unimmunized. Only 28 (11.2%) were booked and supervised deliveries whereas 222 (88.8%) were unbooked. Fifty-eight percent patients were from rural areas and 42% were from urban areas. About 71.2% were from low-income group, 17.2% were from middle-income group and 11.2% from high-income group.
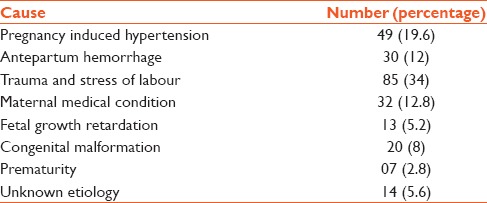
There was a history of previous stillbirth in 9.2%. Among the medical disorders, hypertension and anemia were associated with higher incidence of stillbirth. Fifty-two (32.8%) were hypertensive of which 38 (15.2%) had severe gestational hypertension. Thirty-six (14.4%) had gestational hypertension, 20 (8%) had preeclampsia and 21 (8.4%) had eclampsia. 186 (74.4%) had anemia out of which 128 (51.2%) had mild anemia, 21 (8.4%) had moderate anemia and 36 (14.4%) had severe anemia. One hundred and seventy-seven (70.8%) were delivered by normal, 40 (16%) were delivered by LSCS 18 (7.2%) underwent exploratory laparotomy for rupture uterus, 14 (5.6%) had breech delivery and one had forceps delivery. Table 1 shows the birth weight of fetuses. Twelve (4.8% had prolonged labor, 9 (3.6%) had obstructed labor, 16 (6.4%) had ruptured uterus, 6 (2.4%) had the cord around the neck. Forty-seven patients (18.8%) had APH out of which 15.6% had abruption placentae, and 3.2% had placenta previa. The other maternal medical diseases related with stillbirth were diabetes,[1] heart disease,[1] hyperpyrexia in 4 (2.4%), and infective hepatitis in 2 (0.8%). The CMFs noted in the fetuses recorded are shown in Table 2. The causes of intrauterine fetal death are shown in Table 3.
Table 1.
The birth weight of the fetus
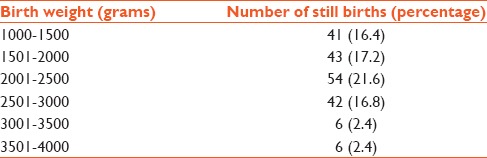
Table 2.
Congenital malformations and still birth
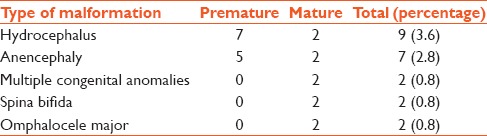
Table 3.
Causes of intrauterine fetal death
DISCUSSION
This study consists of 250 stillbirths amongst 6942 total births thus the incidence of stillbirths was 36/1000 births. The incidence of stillbirth reported from western countries ranges from 4.7% to 12.0%.[1,2,3,4,5,6,7] This is lower than that observed in our study. However, the incidence rate reported from various centers in India is higher 24.4–41.9%.[8,9,10,11,12,13] One reason of higher stillbirth at our center could be due to the selection bias due to it being a tertiary care referral center and all major obstetric complication identified in the periphery and other centers would be referred here. The other reason could be a high number of unsupervised deliveries due to various reasons like illiteracy, low socioeconomic status and the paucity of monitoring facilities in rural areas. The incidence of stillbirth is higher than that reported from South India,[12,13] and this could be due to the higher literacy rates, increased awareness, and better antenatal care. Nutritional deficiency and anemia are leading cause of poor pregnancy outcomes, the majority of our patients had anemia. The Increased risk of fetal death is present amongst the teenage group and older women. The western studies show that increased risk in present in women over 35 years of age.[14,15,16] In our study, however, the fetal deaths were more in the age group of 21–25 years. This is because most of the women in India complete the family before 35 years of age. Increased risk of stillbirth is seen amongst primigravidas and after fifth pregnancy.[9] The incidence is a higher risk amongst poor socioeconomic status.[17] Most of our patients also belonged to poor socioeconomic status. The incidence is higher amongst women with minimal or no antenatal care.[18] This is also reflected in our study where the rates were highest amongst the unsupervised deliveries. The incidence of APH in our study was 18.8%, which was similar to that reported in other studies.[8] The incidence of intrauterine growth retardation in our study was 5.2%. The other studies have reported the incidence from 2.2% to 18.4%.[8,9] The incidence of gestational hypertension in this study was 14.4% which is similar to that reported in other studies.[8] The incidence of CMF was 8.8% which was also similar to that reported from other studies.[8]
CONCLUSION
This study shows that the incidence of stillbirths in our population is similar to most of the other Indian studies, but higher than those reported from developed countries. This is associated with anemia, rural area, poor socioeconomic status, multiparity, previous history of pregnancy loss, unsupervised deliveries, gestational hypertension, and CMFs. Proper screening and antenatal supervision can play an important role in decreasing the rate of stillbirths.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Fretts RC, Boyd ME, Usher RH, Usher HA. The changing pattern of fetal death, 1961-1988. Obstet Gynecol. 1992;79:35–9. [PubMed] [Google Scholar]
- 2.Löfgren O, Polberger S. Perinatal mortality: Changes in the diagnostic panorama 1974-1980. Acta Paediatr Scand. 1983;72:327–32. doi: 10.1111/j.1651-2227.1983.tb09723.x. [DOI] [PubMed] [Google Scholar]
- 3.Hovatta O, Lipasti A, Rapola J, Karjalainen O. Causes of stillbirth: A clinicopathological study of 243 patients. Br J Obstet Gynaecol. 1983;90:691–6. doi: 10.1111/j.1471-0528.1983.tb09296.x. [DOI] [PubMed] [Google Scholar]
- 4.Machin GA. A perinatal mortality survey in south-east London, 1970-73: The pathological findings in 726 necropsies. J Clin Pathol. 1975;28:428–34. doi: 10.1136/jcp.28.6.428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Magani IM, Rafla NM, Mortimer G, Meehan FP. Stillbirths: A clinicopathological survey (1972-1982) Pediatr Pathol. 1990;10:363–74. doi: 10.3109/15513819009067124. [DOI] [PubMed] [Google Scholar]
- 6.Morrison I, Olsen J. Weight-specific stillbirths and associated causes of death: An analysis of 765 stillbirths. Am J Obstet Gynecol. 1985;152:975–80. doi: 10.1016/0002-9378(85)90542-3. [DOI] [PubMed] [Google Scholar]
- 7.Whitfield CR, Smith NC, Cockburn F, Gibson AA. Perinatally related wastage - A proposed classification of primary obstetric factors. Br J Obstet Gynaecol. 1986;93:694–703. [PubMed] [Google Scholar]
- 8.Misra PK, Thakur S, Kumar A, Tandon S. Perinatal mortality in rural India with special reference to high risk pregnancies. J Trop Pediatr. 1993;39:41–4. doi: 10.1093/tropej/39.1.41. [DOI] [PubMed] [Google Scholar]
- 9.Dasgupta S, Saha I, Mandal AK. A study on profile of stillbirths. J Indian Med Assoc. 1997;95:175, 178. [PubMed] [Google Scholar]
- 10.Kumari R, Mengi V, Kumar D. Maternal risk factors and pregnancy wastage in a rural population of Jammu District. JK Sci. 2013;15:82–5. [Google Scholar]
- 11.Shah U, Pratinidhi AK, Bhatlawande PV. Perinatal mortality in rural India: A strategy for reduction through primary care. I Stillbirths. J Epidemiol Community Health. 1984;38:134–7. doi: 10.1136/jech.38.2.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jadhav MA, Christopher LG. Perinatal mortality in Vellore. Part I: A study of 21,585 infants. Indian J Pediatr. 1986;53:347–52. doi: 10.1007/BF02760413. [DOI] [PubMed] [Google Scholar]
- 13.Bai NS, Mathews E, Nair PM, Sabarinathan K, Harikumar C. Perinatal mortality rate in a south Indian population. J Indian Med Assoc. 1991;89:97–8. [PubMed] [Google Scholar]
- 14.Little RE, Weinberg CR. Risk factors for antepartum and intrapartum stillbirth. Am J Epidemiol. 1993;137:1177–89. doi: 10.1093/oxfordjournals.aje.a116620. [DOI] [PubMed] [Google Scholar]
- 15.Milaat WA, Florey CD. Perinatal mortality in Jeddah, Saudia Arabia. Int J Epidemiol. 1992;21:82–90. doi: 10.1093/ije/21.1.82. [DOI] [PubMed] [Google Scholar]
- 16.Raymond EG, Cnattingius S, Kiely JL. Effects of maternal age, parity, and smoking on the risk of stillbirth. Br J Obstet Gynaecol. 1994;101:301–6. doi: 10.1111/j.1471-0528.1994.tb13614.x. [DOI] [PubMed] [Google Scholar]
- 17.Daga AS, Daga SR. Epidemiology of perinatal loss in rural Maharashtra. J Trop Pediatr. 1993;39:83–5. doi: 10.1093/tropej/39.2.83. [DOI] [PubMed] [Google Scholar]
- 18.Moyo SR, Tswana SA, Nyström L, Mahomed K, Bergström S, Ljungh A. An incident case-referent study of stillbirths at Harare Maternity Hospital: Socio-economic and obstetric risk factors. Gynecol Obstet Invest. 1994;37:34–9. doi: 10.1159/000292517. [DOI] [PubMed] [Google Scholar]


