Abstract
For congenital teratomas, oropharyngeal cavity is one of the rarest sites (2% of all teratomas). They are rarely picked up by prenatal ultrasonography. Postnatally, newborns present with respiratory distress and at this point role of pediatricians is very crucial in establishing secure airway after which they need to be carefully evaluated and surgically managed. We present a female neonate with palatal teratoma which was treated successfully with surgery.
Keywords: Cleft palate, oropharyngeal cavity, teratoma
INTRODUCTION
Teratomas are true neoplasms composed of tissue derived from all three germinal layers.[1] They may be seen in midline or para-axial location, from the brain to the sacral area. They display a particular tendency to locate in the sacrococcygeal and pre-sacral regions.[2] Reported incidence of tumors at these sites is 1:20,000 to 1:40,000 live births.[3]
The oropharyngeal cavity is exceedingly rare for teratomas, 2% of all teratomas, present as large masses protruding from the oropharyngeal area. Incidence is more in females.
Though oropharyngeal teratomas have a benign histopathology, they are potentially lethal as they may cause airway obstruction and respiratory compromise. So, principles of management in such patients comprise of the immediate postpartum establishment of a secure airway, if needed via tracheostomy and complete surgical resection of the mass.
CASE REPORT
A 1980 g female infant born to 22-year-old mother after 38 weeks gestation presented with a growth in oral cavity associated with respiratory distress. The mother had undergone ultrasonography examination during pregnancy, but the report of the same was unavailable. On examination, cleft palate was present and a palatal tumor of size 4 cm × 3 cm was found in the cleft area [Figure 1]. It was hampering feeding. Computed tomography scan – showed mass lesion in the palatal region (attached to the palate, more on the right side). No intracranial extension [Figure 2].
Figure 1.

Preoperative photo
Figure 2.

Computed tomography scan image
After due preparation, the patient was operated, and the mass was excised in toto [Figure 3]. Histopathologic examination – revealed a teratoma composed of mature glial tissue, choroid plexus, glands lined by respiratory type, columnar mucin secreting, and melanin pigment bearing epithelium. Pools of myxoid matrix bearing physaliferous cells are present (notochord – like/chondroid areas) [Figures 4 and 5].
Figure 3.

Postoperative photo
Figure 4.
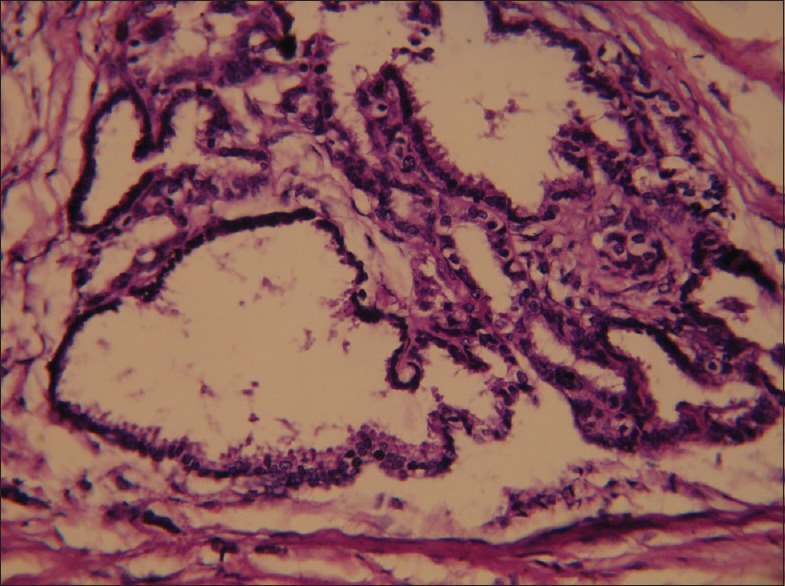
Microscopic picture 1
Figure 5.
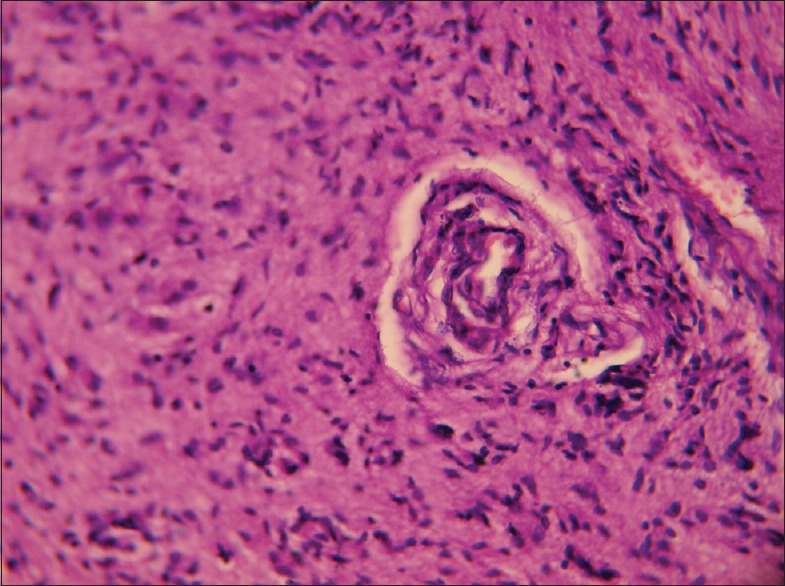
Microscopic picture 2
Following excision, patient recovered faster and gained weight. The weight of the patient on discharge was 2.5 kg. Now, the patient is under routine follow-up, and palatoplasty has been done.
DISCUSSION
Teratomas are the tumors which contain tissues derived from all three germ layers. These contain tissues foreign to the anatomical site of origin. Most of the teratomas in the pediatric age group are benign, but reports of malignant teratoma do exist.
Basic histological classifications which are widely used (Arnold's system) are:
Dermoid tumors: These are composed of ectoderm plus mesoderm. This is the most common form of teratoma
Teratoids: These are poorly differentiated tumors and contain all three germ layers
Teratomas: These also contain tissue from all three germ layers. They are histologically more identifiable
Epignathus: These are tumors which contain fully developed organs and appendages. The large cervical and nasopharyngeal teratomas which obstruct fetal swallowing of amniotic fluid may contribute to polyhydramnios. Association of polyhydramnios is not clearly described in pure oral teratomas. Masses with solid and cystic components are more in favor of teratoma.
Plain radiographs of head demonstrate calcifications within the lesion. Other imaging technique such as magnetic resonance imaging, is useful in finding out the anatomical relationship of these tumors. The important blood investigation is alpha-fetoprotein (AFP).[4] AFP is generally elevated and it returns to normal after total excision.
Clinical differential diagnoses of oropharyngeal teratoma are cystic hygroma, lymphangioma, duplications and neuroblastoma. Moreover, the histopathological differential diagnosis includes hamartoma, dermoid cyst, and a heterotopic gastrointestinal cyst. With growth, oral teratomas extend outside the mouth rather than toward oropharynx. That is why, the respiratory distress may be less. The neonates with oral teratomas may have other congenital anomalies such as cleft palate, cystic hygroma. The basic principle of management of oropharyngeal teratomas is the establishment and maintenance of a secure airway. If an oropharyngeal teratoma is diagnosed antenatally, elective delivery or lower segment cesarean section is carried out. If orotracheal/nasotracheal intubation is failed/or difficult, tracheostomy must be done.
Early surgical intervention is necessary. Surgical goal is to remove the complete mass in toto, as a residual tumor may cause recurrence. Adjuvant chemotherapy and radiotherapy are indicated; if histology shows malignant component. Associated cleft palate can be repaired when the child grows up, that is, at the age of 1½ years.[5] During follow-up, AFP should be monitored. In our case, all the AFP levels were within normal range.
The overall prognosis for oral teratomas is good. Oropharyngeal, cervical teratoma as may cause more severe respiratory symptoms. They are very less likely to produce any problems antenatally.
Postnatally, early surgical intervention is necessary. Early diagnosis, the establishment of the good airway, complete excision of tumor and timely follow-up should increase the survival of newborns with oral teratomas.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Wiilis RA. The Borderland of Embryology and Pathology. 2nd ed. London: Butterworth's; 1962. [Google Scholar]
- 2.Altman RP, Randolph JG, Lilly JR. Sacrococcygeal teratoma: American Academy of Pediatrics Surgical Section Survey-1973. J Pediatr Surg. 1974;9:389–98. doi: 10.1016/s0022-3468(74)80297-6. [DOI] [PubMed] [Google Scholar]
- 3.Azizkhan RG, Haase GM, Applebaum H, Dillon PW, Coran AG, King PA, et al. Diagnosis, management, and outcome of cervicofacial teratomas in neonates: A Childrens Cancer Group study. J Pediatr Surg. 1995;30:312–6. doi: 10.1016/0022-3468(95)90580-4. [DOI] [PubMed] [Google Scholar]
- 4.Marras T, Poenaru D, Kamal I. Perinatal management of nasopharyngeal teratoma. J Otolaryngol. 1995;24:310–2. [PubMed] [Google Scholar]
- 5.Liang CC, Lai JP, Lui CC. Cleft palate with congenital midline teratoma. Ann Plast Surg. 2003;50:550–4. doi: 10.1097/01.SAP.0000037462.83232.1E. [DOI] [PubMed] [Google Scholar]


