Abstract
Hip arthroscopy has emerged as a diagnostic and therapeutic tool in the management of osteonecrosis (ON) of the femoral head. Direct visualization of the joint, aids the staging of the disease, while mechanical symptoms and pain can be alleviated by addressing the often coexisting intra-articular pathology (labral tears, chondral delamination, loose bodies and synovitis) thereby improving the clinical outcome in some patients. The article explores the role and possible value of hip arthroscopy as a surgical technique in the treatment of hip ON.
INTRODUCTION
Osteonecrosis (ON) of the femoral head commonly affects relatively young, active patients in the third or fourth decade of their life [1, 2]. The disease is the result of irreversible anoxia of the affected subchondral bone, resulting in both marrow-cell and osteocyte necrosis [1]. The ischaemic insult may be associated with an apparent aetiology/risk factor (secondary ON) or the aetiology might be unknown (primary ON) [3]. If left untreated, the mechanical instability may cause failure of the subchondral trabeculae and articular collapse of the femoral head which will progress to secondary osteoarthritis (OA) in 80% of the cases [4]. A review of the 2013 National Joint Registries of England and Wales and the one from Australia suggest that hip joint replacement surgery performed for secondary OA with a primary diagnosis of ON accounts for 2 and 3.5% of the total number of operations, in these two countries, respectively [5, 6]. In the United States, the corresponding rate was estimated to account between 5 and 12% [4].
Because these patients are young and relatively active, and since total hip arthroplasty has not always been associated with a lasting outcome in this population, various procedures for joint preservation have been proposed [1]. Operative treatment of hip ON can be divided broadly into femoral head-sparing or arthroplasty procedures. Candidates for joint-preserving procedures (core decompression, percutaneous drilling, vascularized and non-vascularized bone-grafting and osteotomies) are usually at the pre- or early post-collapse stage [2, 7]. These joint preserving surgeries have reported variable reported success rates [8].
The purpose of our selective review is 2-fold. First, to discuss the value of hip arthroscopy in the staging femoral head ON and second to review its efficacy to supplement traditional surgical techniques in selected cases.
IMAGING AND STAGING
The treatment of ON depends on the stage at presentation; thus, early and accurate diagnosis is essential to define appropriate management. Magnetic resonance imaging (MRI) has become the gold standard for assessing and diagnosing ON. It is 99% sensitive and 98% specific for the disease and can detect early marrow necrosis and ingrowth of vascularized mesenchymal tissue, before changes become detectable on plain radiographs [1, 8, 9]. The multiplanar imaging capability of MRI coupled with its superb contrast to noise ratio allows the accurate size and location of the ON lesion [10].
All proposed treatment algorithms have been based on staging of the disease. The imaging findings that can influence a treatment plan are: (i) the lesion being pre- or post-collapse, (ii) the size of the necrotic area [1, 8], (iii) the integrity of the articular cartilage and the presence of associated intra-articular lesions (labral tears, loose bodies etc) [11].
Computer tomography (CT) was thought to be more sensitive than MRI in detecting the presence or absence of focal collapse of the femoral head [12]. Recent articles though, suggest that application of appropriate high-resolution images allows MRI to depict subchondral fractures equally or even better than CT [10, 13]. Some MRI characteristics (degree of involvement of the weight bearing aspect of the femoral head) even appear to have good prognostic value for possible collapse [9, 14].
Advances in higher field magnets and improved designs and sequences have increased our diagnostic accuracy using high-resolution non-contrast or MR arthrographic (MRa) techniques [13, 15]. Given the recent increase in the number of hip arthroscopies performed each year, correlation between MRI and intraoperative findings has become possible. In 2004 in a comparative MRa-hip arthroscopy evaluation study, with respect to articular cartilage pathology suggested that MRa had a sensitivity of 47%, specificity of 89%, positive predictive value of 84%, negative predictive value of 59%, and accuracy of just 67% [16]. In a more recent comparable study, using standard MRa protocols, a sensitivity of 70% and a specificity of 84% were demonstrated in detecting cartilage defects identified at arthroscopy [17]. Using arthroscopy as the standard an accuracy of 87% and weighted-kappa measures of reproducibility of 0.8 (P = 0.001) for articular cartilage evaluation was demonstrated with non-contrast MRI [18]. Despite these advances, arthroscopy is still thought to be the gold standard in detecting and staging chondral lesions [19–22]. In a recent meta-analysis study reporting the diagnostic test accuracy (sensitivity/specificity) of MRI, MRa, multidetector arrays in CT arthrography (MDCT) and computer tomography arthrography (CTA) for the assessment of adults with chondral lesions of the hip in comparison to surgical findings (arthroscopic or open) as the reference, confirmed that arthroscopy remains the most accurate method of assessing the cartilage in the hip joint [22].
As such, it can be said that despite the recent imaging advances than can accurately evaluate the presence of intra-articular lesions (labral tears, loose bodies, etc.), hip arthroscopy can be useful in evaluating cartilage lesions and consequently enhance the staging and allow more accurate prognostication in ON of the femoral head.
TREATMENT
Addressing intra-articular pathology
Labrum, chondral flaps, loose bodies
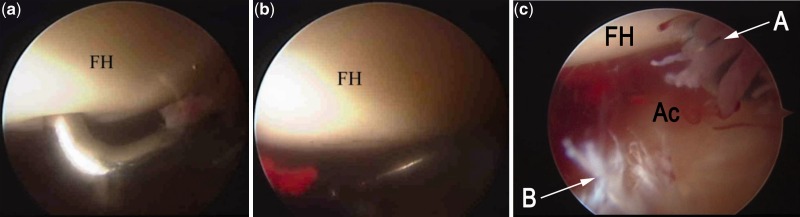
It is often that patients with ON complain of mechanical symptoms such as clicking, locking, popping or giving way. These symptoms can be the result of disorders such as labral tears, chondral flaps or even loose bodies which could not be treated conservatively but are amendable to arthroscopic treatment [23]. This intra-articular pathology is thought to be secondary to the periodic loss of the normal contour of the femoral head where the necrotic cancellous bone is unable to withstand physiologic forces causing mechanical disruption of the cartilage or labrum [11, 24]. During arthroscopy the stability of necrotic segment and the overlying articular cartilage can be assessed by with the so called ‘ballottement test’ [24]. The test is considered to be positive when gentle pressure with a probe causes the articular cartilage to buckle over the necrotic segment (Fig. 1a) and to spring back to its original state upon release of pressure (Fig. 1b). In the presence of a positive test synovitis and labrum pathology are common (Fig. 1c).
Figure 1.
(a) Arthroscopic appearance of a positive ballottement test where the articular cartilage of the femoral head buckles under the pressure of the probe. (b) The articular cartilage of the femoral head assumes its original shape after the release of pressure. (c) In the same hip, associated synovitis and a degenerative labral tear is seen. FH, femoral head; Ac, Acetabulum; a, synovitis, b labrum degeneration).
Current literature agrees that hip arthroscopy in ON is best indicated for patients with evidence of intra-articular pathology and mechanical symptoms in the absence of significant joint space narrowing and femoral head collapse. The presence of advanced ON and arthritis at the time of the index procedure is a bad prognostic indicator, with uniformly poor results [11, 23, 25, 26, 27].
Synovitis
Joint effusion, probably secondary to ON related synovitis is seen up to 72% of cases regardless of articular collapse [10].
It is the author’s opinion that an arthroscopic joint wash-out and synovectomy in selected cases can be of clinical benefit, since it reduces pain and joint effusion, improves range of motion and by reducing the capsular stress from the effusion possibly improving the blood flow to the femoral head.
Femoroacetabular impingement and ON
Even though there is no documented association of femoroacetabular impingement (FAI) and ON or their co-existence, both present at a similar age (late 30s, mid 40s) with no good clinical signs or physical examination tests to differentiate which of the two conditions are primarily responsible for the symptoms.
This challenging clinical problem could be addressed with a diagnostic intra-articular hip injection which will relieve the intra-articular pain from FAI and its associated lesions (labrum and chondral pathology) but it will not help much with the extra-articular and intra-osseous pain from ON. The accuracy of this diagnostic test is considered to be high [28, 29]. If the response is positive, then one should supplement the joint-preserving procedure chosen with hip arthroscopy so that labrum and chondral pathology can also be treated. It has even been suggested that one could also address the bony cam/pincer morphology [30]. In the author’s opinion, the priority in every case is treating ON and addressing the mechanical symptoms. If FAI surgery is needed it should wait for a later date and not prolong the operation and delay the rehabilitation of the joint.
Arthroscopic-assisted core decompression and bone grafting
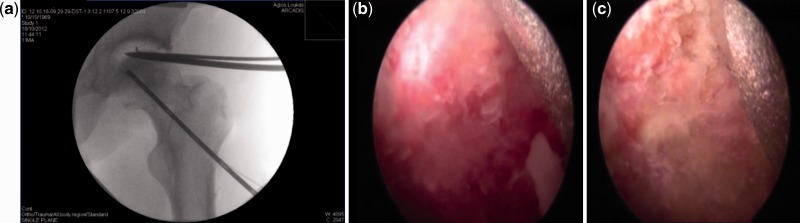
Core decompression is the most common procedure performed for small- or medium-sized lesions, especially at the pre-collapse stage [8, 31, 32]. It is a generic term that is often accompanied with supplemental procedures (vascularized or non-vascularized graft, injection of growth factors, electrical stimulation etc.) [1]. Core decompression can be technically demanding, requiring bi-planar imaging for proper placement of the core drill [33]. Hip arthroscopy can assist fluoroscopic assisted retrograde drilling, by guiding the accurate placement of the tip of the drill into the area of chonral softening or irregularity or the ‘ballottable’ segment of the femoral head which corresponds to the underlying necrotic lesion [11, 24, 33]. The direct visualization of the femoral head, also reduces the possibility of over-drilling, penetration and damage of the articular cartilage that in the author’s opinion should be avoided. Drilling can also be guided arthroscopically by direct visualization by inserting the pin thought the anterior or auxiliary portal in the direction of the centre of the necrotic lesion under image guidance [34]. Arthroscopically assisted retrograde drilling can also be supplemented with injection of biologic factors (PRP, BMP) [1, 34, 35]. The correct placement of the drill to the necrotic lesion can also be verified by bone endoscopy (insertion of the scope into the core track) [36, 37] (Fig. 2a). Endoscopically a distinct border can be seen between bleeding healthy bone and necrotic bone which appears sclerotic and white (Fig. 2b and c).
Figure 2.
(a) During bone endoscopy the −70 camera is positioned in the core track in order to ensure, that this is positioned directly to the necrotic area. (b) The camera reveals the healthy area of the femoral head as red-bleeding bone.(c) The camera in the necrotic area of the femoral head reveals sclerotic-white bone. (The metal appearing at the top end of the picture is a thin needle that washes out the track to improve our imaging capability).
Core decompression can be supplemented in some cases with non-vascularized bone grafting. The procedure provides decompression of the osteonecrotic lesion, removal of the necrotic bone and structural support and scaffolding for repair and remodelling of the subchondral bone. This can be assisted arthroscopically by opening under direct vision a cortical window at the level of head– neck junction (‘light bulb’ approach) removing the necrotic bone with either burrs or curettes and introducing bone graft [34]. The graft can also be introduced though the core track. Recently, 86% success rate (no radiological progress, no reoperation) was reported in 53 consecutive patients [38] with arthroscopic assisted core decompression curettage of the necrotic lesion (Fig. 3) and insertion of autogenic bone cylinders harvested from the iliac crest using knee osteochondral autograft transfer system (OATS). The bone cylinders act as biologic scaffold that support the necrotic area of the FH. The authors have used this technique and agree that the preliminary results are encouraging.
Figure 3.
Arthroscopic assisted core decompression and curettage of the necrotic lesion.
In a similar manner, bone grafting and stabilization of the graft under endoscopic visualization has been described for ON in the paediatric population [39].
Osteonecrosis of the femoral head (legg-calvé-perthes) in children
Legg-calvé-perthes (LCP) disease is ON of the growing femoral head and can result in hip pain and mechanical symptoms because of loose bodies, labral tears, subluxation, synovitis and chondral lesions [40, 41]. Hip arthroscopy can be used to treat these mechanical problems and reduce the symptoms without though altering the natural history of the disease [40–42].
DISCUSSION
Arthroscopic surgery of the hip is a well established technique. The indications of its use in ON have been set since the initial publications on hip arthroscopy and ON more than a decade, ago when hip arthroscopy was still evolving [23–25, 27, 33]. These indications are clear and universal which might explain why the pioneer authors who published their experience and set these indications never published again on the matter. Overall, if a bone conserving operation is decided, with a lesion that is at the pre-collapse or at small post-collapse stage; in the presence of mechanical symptoms hip arthroscopy has a clear role. It will allow the accurate evaluation of the femoral head and acetabulum and treat any intra-articular lesions which are so often associated with the disease (loose bodies, labral tears, synovitis, chondral injuries). Patients with established osteoarthritis or without mechanical symptoms might not benefit from the procedure.
As instruments and experience evolve in hip arthroscopy, the new surgical techniques published, do not change the indications or alter the limitations but rather aim to supplement and augment the accuracy of established treatments such as core decompression in a minimally invasive manner [30, 34, 37, 38]. All these techniques have short follow-up and are not compared to more established surgical approaches to be certain of their efficacy.
Past concerns that the distraction of the joint and the increased intra-articular fluid pressure during the operation can compromise the blood supply of the femoral head have not been proven clinically. There have been just three known reports of patients who developed ON as a possible complication of hip arthroscopy [43]. Complications of hip arthroscopy have been documented and there is no reason to suspect that with proper surgical technique they are different in arthroscopy for femoral head ON [43].
CONCLUSION
There is encouraging published clinical evidence to support hip arthroscopy as a safe and reliable adjunct in the management of ON of the femoral head. To date, hip arthroscopy has been used successfully for improving the accuracy of staging alone or in conjunction with various techniques of core decompression. Associated lesions of the articular cartilage and labrum are also relatively easily addressed, thus improving mechanical symptoms and quality of life. As presented in this review article, the majority of the published literature is composed of case series and technical notes. There is need for more prospective randomized multicentre trials to be conducted with longer follow-up and larger numbers of patients to assess both the safety and efficacy of hip arthroscopy in ON.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1.Lieberman JR, Berry DJ, Mont MA, et al. Osteonecrosis of the hip: management in the 21st century. Instr Course Lect 2003; 52: 337–55. [PubMed] [Google Scholar]
- 2.Mont MA, Marulanda GA, Jones LC, et al. Systematic analysis of classification systems for osteonecrosis of the femoral head. J Bone Joint Surg Am 2006; 88(Suppl. 3): 16–26. [DOI] [PubMed] [Google Scholar]
- 3.Malizos KN, Karantanas AH, Varitimidis SE, et al. Osteonecrosis of the femoral head: etiology, imaging and treatment. Eur J Radiol 2007; 63: 16–28. [DOI] [PubMed] [Google Scholar]
- 4.Mont MA, Hungerford DS. Non-traumatic avascular necrosis of the femoral head. J Bone Joint Surg Am 1995; 77: 459–74. [DOI] [PubMed] [Google Scholar]
- 5.National Joint Registry for England and Wales. Annual Clinical Report 2013. Available at: http://www.njrcentre.org.uk. Accessed 24 May 2014. [Google Scholar]
- 6. National Joint replacement Registry Report 2013. Available at: http://www.dmac.adelaide.edu.au. Accessed24 May 2014.
- 7.Mont MA, Jones LC, Sotereanos DG, et al. Understanding and treating osteonecrosis of the femoral head. Instr Course Lect 2000; 49: 169–85. [PubMed] [Google Scholar]
- 8.Mont MA, Jones LC, Hungerford DS. Nontraumatic osteonecrosis of the femoral head: ten years later. J Bone Joint Surg Am 2006; 88: 1117–32. [DOI] [PubMed] [Google Scholar]
- 9.Petrigliano FA, Lieberman JR. Osteonecrosis of the hip: novel approaches to evaluation and treatment. Clin Orthop Relat Res 2007; 465: 53–62. [DOI] [PubMed] [Google Scholar]
- 10.Karantanas AH. Accuracy and limitations of diagnostic methods for avascular necrosis of the hip. Expert Opin Med Diagn 2013; 7: 179–87. [DOI] [PubMed] [Google Scholar]
- 11.Dienst M. Lehrbuch und Atlas Hüftarthroskopie: Diagnostik - Technik – Indikationen. München: Elsevier, 2009. [Google Scholar]
- 12.Stevens K, Tao C, Lee SU, et al. Subchondral fractures in osteonecrosis of the femoral head: comparison of radiography, CT, and MR imaging. Am J Roentgenol 2003; 180: 363–8. [DOI] [PubMed] [Google Scholar]
- 13.Potter HG, Schachar J. High resolution noncontrast MRI of the hip. J Magn Reson Imag 2010. 31: 268–78. [DOI] [PubMed] [Google Scholar]
- 14.Ha YC, Jung WH, Kim JR, et al. Prediction of collapse in femoral head osteonecrosis: a modified Kerboul method with use of magnetic resonance images. J Bone Joint Surg Am 2006; 88(Suppl 3): 35–40. [DOI] [PubMed] [Google Scholar]
- 15.Gold SL, Burge AJ, Potter HG. MRI of Hip Cartilage Clin Orthop Relat Res 2012; 470: 3321–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Keeney JA, Peelle MW, Jackson J, et al. Magnetic resonance arthrography versus arthroscopy in the evaluation of articular hip pathology. Clin Orthop Relat Res 2004; 429: 163–9. [DOI] [PubMed] [Google Scholar]
- 17.Blankenbaker DG, Ullrick SR, Kijowski R, et al. MR arthrography of the hip: comparison of IDEAL-SPGR volume sequence to standard MR sequences in the detection and grading of cartilage lesions. Radiology 2011; 261: 863–71. [DOI] [PubMed] [Google Scholar]
- 18.Mintz DN, Hooper T, Connell D, et al. Magnetic resonance imaging of the hip: detection of labral and chondral abnormalities using noncontrast imaging. Arthroscopy 2005; 21: 385–93. [DOI] [PubMed] [Google Scholar]
- 19.Zlatkin MB, Pevsner D, Sanders TG, et al. Acetabular labral tears and cartilage lesions of the hip: indirect MR arthrographic correlation with arthroscopy–a preliminary study. Am J Roentgenol 2010; 194: 709–14. [DOI] [PubMed] [Google Scholar]
- 20.Sutter R, Zubler V, Hoffmann A, et al. Hip MRI: how useful is intraarticular contrast material for evaluating surgically proven lesions of the labrum and articular cartilage? Am J Roentgenol 2014; 202: 160–9. [DOI] [PubMed] [Google Scholar]
- 21.Perdikakis E, Karachalios T, Katonis P, et al. Comparison of MR-arthrography and MDCT-arthrography for detection of labral and articular cartilage hip pathology. Skeletal Radiol 2011; 40: 1441–7. [DOI] [PubMed] [Google Scholar]
- 22.Smith TO, Simpson M, Ejindu V, et al. The diagnostic test accuracy of magnetic resonance imaging, magnetic resonance arthrography and computer tomography in the detection of chondral lesions of the hip. Eur J Orthop Surg Traumatol 2013; 23: 335–4. [DOI] [PubMed] [Google Scholar]
- 23.McCarthy J, Puri L, Barsoum W, et al. Articular cartilage changes in avascular necrosis: an arthroscopic evaluation. Clin Orthop Relat Res 2003; 406: 64–70. [DOI] [PubMed] [Google Scholar]
- 24.Sekiya JK, Ruch DS, Hunter DM, et al. Hip arthroscopy in staging avascular necrosis of the femoral head. J South Orthop Assoc 2000; 9: 254–61. [PubMed] [Google Scholar]
- 25.Byrd JW, Jones KS. Prospective analysis of hip arthroscopy with 2-year follow-up. Arthroscopy 2000;16: 578–87. [DOI] [PubMed] [Google Scholar]
- 26.Larson CM, Swaringen J, Morrison G. A review of hip arthroscopy and its role in the management of adult hip pain. Iowa Orthop J 2005; 25: 172–9. [PMC free article] [PubMed] [Google Scholar]
- 27.O’leary JA, Berend K, Vail TP. The relationship between diagnosis and outcome in arthroscopy of the hip. Arthroscopy 2001; 17: 181–8. [DOI] [PubMed] [Google Scholar]
- 28.Byrd JW, Jones KS. Diagnostic accuracy of clinical assessment, magnetic resonance imaging, magnetic resonance arthrography, and intra-articular injection in hip arthroscopy patients. Am J Sports Med 2004; 32: 1668–74. [DOI] [PubMed] [Google Scholar]
- 29.Kivlan BR, Martin RL, Sekiya JK. Response to diagnostic injection in patients with femoroacetabular impingement, labral tears, chondral lesions, and extra-articular pathology. Arthroscopy 2011; 27: 619–27. [DOI] [PubMed] [Google Scholar]
- 30.Beck DM, Park BK, Youm T, et al. Arthroscopic treatment of labral tears and concurrent avascular necrosis of the femoral head in young adults. Arthrosc Tech 2013; 2: e367–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Marker DR, Seyler TM, Ulrich SD, et al. Do modern techniques improve core decompression outcomes for hip osteonecrosis? Clin Orthop Relat Res 2008;466: 1093–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Scully SP, Aaron RK, Urbaniak JR. Survival analysis of hips treated with core decompression or vascularized fibular grafting because of avascular necrosis. J Bone Joint Surg Am 1998; 80: 1270–5. [DOI] [PubMed] [Google Scholar]
- 33.Ruch DS, Satterfield W. The use of arthroscopy to document accurate position of core decompression of the hip. Arthroscopy 1998; 14: 617–9. [DOI] [PubMed] [Google Scholar]
- 34.Guadilla J, Fiz N, Andia I, et al. Arthroscopic management and platelet-rich plasma therapy for avascular necrosis of the hip. Knee Surg Sports Traumatol Arthrosc 2012; 20: 393–8. [DOI] [PubMed] [Google Scholar]
- 35.Zhuo N, Wan Y, Lu X, et al. [Comprehensive management of early stage avascular necrosis of femoral head by arthroscopic minimally invasive surgery] (in Chinese). Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2012; 26: 1041–4. [PubMed] [Google Scholar]
- 36.Brannon JK. Nontraumatic osteonecrosis of the femoral head: endoscopic visualization of its avascular burden. Orthopedics 2012; 35: e1314–22. [DOI] [PubMed] [Google Scholar]
- 37.Govaers K, Meermans G, Bortier H, et al. Endoscopically assisted core decompression in avascular necrosis of the femoral head. Acta Orthop Belg 2009; 75: 631–6. [PubMed] [Google Scholar]
- 38.Ellenrieder M, Tischer T, Kreuz PC, et al. [Arthroscopically assisted therapy of avascular necrosis of the femoral head] (in German). Oper Orthop Traumatol 2013; 25: 85–94. [DOI] [PubMed] [Google Scholar]
- 39.Wells L, Hosalkar HS, Crawford EA, et al. Thorough debridement under endoscopic visualization with bone grafting and stabilization for femoral head osteonecrosis in children. J Pediatr Orthop 2009; 29: 319–26. [DOI] [PubMed] [Google Scholar]
- 40.Ross JR, Nepple JJ, Baca G, et al. Intraarticular abnormalities in residual Perthes and Perthes-like hip deformities. Clin Orthop Relat Res 2012; 470: 2968–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Freeman CR, Jones K, Byrd JW. Hip arthroscopy for Legg-Calvè-Perthes disease: minimum 2-year follow-up. Arthroscopy 2013; 29: 666–74. [DOI] [PubMed] [Google Scholar]
- 42.Majewski M, Hasler CC, Kohler G. Arthroscopic mobilization of the hip joint in children with aseptic necrosis of the femur head. J Pediatr Orthop B 2010; 19: 135–9. [DOI] [PubMed] [Google Scholar]
- 43.Papavasiliou A, Bardakos N. Complications of arthroscopic surgery of the hip. Bone Joint Res 2012; 1: 131–44. [DOI] [PMC free article] [PubMed] [Google Scholar]