Abstract
The aim of this study is to identify intra-articular pathology and loose bodies during arthroscopic examination of young patients after hip dislocation and to correlate arthroscopic findings with preoperative imaging. Twelve hips in 12 patients (eight males, four females; mean age 16.3 years, range 11–25 years) underwent hip arthroscopy after traumatic hip dislocation. Medical records, imaging studies and intra-operative images were reviewed to determine the damage to the hip joint, acetabular morphology, including labral and/or cartilage injury and presence of loose bodies. Imaging findings were compared with arthroscopic findings and treatment. All 12 patients underwent arthroscopy, which was performed an average of 59 (range 1–359, median 17.5) days after dislocation. Ten patients had posterior hip dislocations and two patients had obturator dislocations. All patients underwent closed reduction as initial management, with one incongruent reduction. Eleven patients had computed tomography scans and four patients had magnetic resonance imaging (MRI) with three patients having both modalities. Loose bodies were identified in 6/12 (50%) patients on pre-operative imaging and in 8/12 (67%) patients at arthroscopy. The two patients with unidentified loose bodies on imaging did not have a preoperative MRI. Five patients had acetabular cartilage injuries and three patients had femoral-sided cartilage injuries. Eight patients had labral injuries at arthroscopy. Intra-articular injuries and loose bodies are common in adolescent and young adult patients undergoing arthroscopy following traumatic hip dislocation. Further studies are needed to determine whether arthroscopy after traumatic dislocation may play a role in hip preservation following these injuries.
INTRODUCTION
Traumatic hip dislocations without associated fractures are commonly treated with closed reduction and a period of protected weight bearing [1, 2]. In the setting of associated fractures, they are commonly treated with open reduction and internal fixation with irrigation of the hip joint to remove osteochondral and chondral loose bodies. In children, reported complications following traumatic hip dislocation include avascular necrosis, coxa magna, osteoarthritis and recurrent instability [2–4]. There have been multiple reports of patients undergoing hip arthroscopy after traumatic hip dislocation that reported on the incidence of loose bodies and intra-articular pathology in the adult population [5–8]. There is animal data which suggest that chondral loose bodies in the joint may lead to articular cartilage degeneration [9].
In a recent series of acetabular fracture-dislocations, intra-articular fragments were identified in 45/127 patients (35%) on post-reduction computed tomography (CT) scans [10]. The first report of arthroscopy following traumatic hip dislocation without associated fracture in adults by Mullis and Dahners [7] reported loose bodies in 33 of 36 (92%) of patients. Seven of nine patients in their series who had negative radiographs, CT and a concentric reduction on imaging had loose bodies identified at the time of arthroscopy. Similarly, Ilizaliturri et al. [6] found that 14 of 17 (82%) adult patients had loose bodies after traumatic hip dislocation. In addition, 14 had anterior labral tears, six had posterior labral tears, 16 had acetabular chondral damage and all 17 had femoral chondral damage. A report of 14 adult professional athletes showed a similar incidence of loose bodies—11 of 14 patients (79%). In this cohort, all had some degree of cartilage injury and labral tearing [5].
Despite multiple reports of arthroscopy after traumatic hip dislocations in adults, there has yet to be a report in the adolescent and young adult age group. In one series of 35 children, eight underwent open arthrotomy for intra-articular osteochondral loose bodies and labral interposition blocking congruent reduction [4]. While a rare complication of hip dislocation in young patients, the senior author’s practice had two adolescent patients go on to end-stage arthritis after hip dislocation secondary to chondrolysis. This prompted him to perform routine arthroscopy to evaluate for loose bodies and intra-articular pathology in this patient population. We hypothesized that there would be a similar incidence of loose bodies in the adolescent and young adult patients compared with prior series of adult patients. We also hypothesized that there would be a high incidence of concomitant intra-articular injuries to the cartilage and labrum as reported in prior adult series.
MATERIALS AND METHODS
Study design
Patients selected retrospectively for inclusion in this series included both young adult and pediatric patients from a registry approved by institutional review board at our institution. All patients in this study underwent hip arthroscopy with the senior author (SKA) between 2008 and 2013. The senior author has performed hip arthroscopy on over 1100 patients. Query of his database for primary diagnosis for hip dislocation identified 20 cases and there were 12 cases in patients meeting our age criteria. Inclusion criteria included a primary diagnosis of hip dislocation and patient age less than 25 years. Exclusion criteria included lack of preoperative imaging, lack of documentation of the original injury, and patient age greater than 25 years.
Patient evaluation
All patients presented after hip dislocation with symptoms consistent with hip pathology. They described groin and/or anterior thigh pain that was worse with activity or had pain that limited activity. On examination, patients had reproducible pain with hip range of motion. Radiographic imaging showed prior hip dislocation with post-reduction imaging showing concentric reduction in 11 of 12 cases. Some patients had advanced imaging identifying either osteochondral or chondral intra-articular loose bodies.
The patient’s sex, age, prior surgical history and intra-operative findings were obtained from their medical records. Operative reports were reviewed and intra-articular pathology was recorded and classified as previously described by Beck et al. [11]. In brief, the acetabular and femoral cartilage were defined as either normal, malacia, debonding, cleavage or defect. The acetabular labrum was defined as either normal, degeneration, full-thickness tear, detachment or ossification. The date of traumatic dislocation was recorded from the medical record and the time in days from dislocation to hip arthroscopy was determined. Patients also had pre-operative radiographic analysis with anterior–posterior (AP), frog leg lateral and false profile views of the hip. AP and false profile views were completed while the patient was weight bearing. CT and magnetic resonance imaging (MRI) of the hips were reviewed and the presence of loose bodies and intra-articular findings were recorded. Acetabular morphology including lateral center edge angle (LCEA), acetabular index (AI) and acetabular version were also recorded. The authors of the study reviewed the imaging studies (orthopaedic surgeons).
Surgical technique and rehabilitation
Patients were placed supine on the traction table (Smith and Nephew, Memphis, TN, USA). They were prepped and draped in the normal fashion and access to the hip was obtained as previously described [12]. C-arm fluoroscopy was positioned on the opposite side of the table. Two or three portals were used, an anterolateral (AL) and mid-anterior portal (MA) in all cases, with a distal anterolateral accessory portal in cases with labral repair. An interportal capsulotomy was performed to connect the AL and MA portals. Labral repairs were then performed on a case-by-case basis if the traumatic injury was not in position to heal. Thorough diagnostic arthroscopy of all areas of the joint was completed to assure identification and removal of all loose bodies. Intra-articular loose bodies were removed by the use of either a motorized shaver or grasping devices. The torn ligamentum teres was debrided to remove excess tissue in all cases. Fluoroscopic evaluation included hip extension with internal and external rotation, 45° Dunn view in neutral rotation, as well as a frogleg lateral to confirm removal of all osteochondral loose bodies. A routine capsular repair of the interportal capsulotomy was preformed with two to five non-absorbable sutures.
Formal physical therapy was initiated at 2 weeks. Patients began with touchdown weight bearing for 2 weeks, followed by partial weight bearing for two additional weeks. Crutches were discontinued at 4 weeks. No brace was worn. No hyperextension or external rotation of the foot was permitted for 6 weeks. Progression to full range of motion was encouraged during the 6- to 12-week time period. Conditioning and strengthening was continued with progression to sporting activities at 4–6 months. Naprosyn 500 mg twice daily for 3 weeks was used for heterotopic ossification prophylaxis.
RESULTS
Between 2008 and 2013, the principal investigator performed 12 hip arthroscopies on patients younger than 25 years of age that had symptoms, examination and imaging consistent with pain after traumatic hip dislocation. The mean age at the time of dislocation was 16.1 years (range 11.3–25 years). All patients were treated with closed reduction with one patient having an incongruent joint on post-reduction imaging, which was caused by posterior labral incarceration in the joint. Characteristics of the patients’ original injury presentations are presented in Table I. The majority of the dislocations were low-energy sporting injuries. In 10 patients, the direction of dislocation was posterior with two patients having obturator dislocations (Fig. 1). One patient had a sciatic nerve palsy from their injury that recovered with observation.
Table I.
Injury characteristics
| Patient number | Age at injury /gender | Injury mechanism | Direction of dislocation | Initial treatment |
|---|---|---|---|---|
| 1 | 12.5/F | Ice skating | Obturator | Closed reduction |
| 2 | 19.3/M | Downhill skiing | Posterior | Closed reduction |
| 3 | 17.9/M | Downhill skiing | Posterior | Closed reduction |
| 4 | 12.1/F | Basketball | Posterior | Closed reduction |
| 5 | 12.9/M | Football | Posterior | Closed reduction |
| 6 | 19.7/M | Downhill skiing | Posterior | Closed reduction |
| 7 | 11.3/F | Sledding | Posterior | Closed reduction |
| 8 | 14.5/M | Downhill skiing | Posterior | Closed reduction – incongruent joint |
| 9 | 11.7/M | Downhill Skiing | Posterior | Closed reduction |
| 10 | 12.5/M | ATV accident | Posterior | Closed reduction |
| 11 | 24.3/M | Snowmobiling | Posterior | Closed reduction |
| 12 | 25.0/F | Fell off horse | Obturator | Closed reduction |
ATV, all-terrain vehicle.
Fig. 1.
Pre-reduction imaging of a patient with an obturator dislocation that was successfully reduced in a closed fashion.
Advanced imaging was obtained after the dislocation in all cases (Table II). Eight patients had CT alone, three had both MRI and CT and one patient had MRI alone. There were six patients with loose bodies identified on post-reduction imaging (Fig. 2). Five of the 11 CT scans identified loose bodies and two of the four MRIs. In addition, three of the four MRIs identified labral tears. Radiographic and CT/MRI images were reviewed to evaluate the presence of dysplasia or acetabular retroversion (Table III). Two patients had LCEAs of <20°, seven had an LCEA between 20° and 25° and no patients had acetabular retroversion. The mean LCEA was 24.3°, the mean acetabular index was 5.8° and the mean acetabular anteversion was 12.5° (Table III).
Table II.
Preoperative imaging findings
| Patient number | Age at injury /gender | CT scan (yes/no) | CT findings |
MRI (yes/no) | MRI findings |
|||
|---|---|---|---|---|---|---|---|---|
| Fracture | Loose bodies | Labral tear | Loose bodies | |||||
| 1 | 12.5/F | Yes | No | No | No | NA | ||
| 2 | 19.3/M | Yes | No | No | Yes | Yesa | No | |
| 3 | 17.9/M | Yes | No | No | No | NA | ||
| 4 | 12.1/F | Yes | No | No | Yes | No | No | |
| 5 | 12.9/M | Yes | No | No | No | NA | ||
| 6 | 19.7/M | Yes | No | Yes | No | NA | ||
| 7 | 11.3/F | Yes | No | Yes | No | NA | ||
| 8 | 14.5/M | Yes | No | Yes | Yes | Yesb | Yes | |
| 9 | 11.7/M | No | NA | Yes | No | Yes | ||
| 10 | 12.5/M | Yes | No | No | No | NA | ||
| 11 | 24.3/M | Yes | No | Yes | No | NA | ||
| 12 | 25.0/F | Yes | No | Yes | No | NA | ||
aSuperior labral tear.
bPosterior labral tear incarcerated in the joint.
CT, computed tomography; MRI, magnetic resonance imaging; NA, not applicable.
Fig. 2.
Post-reduction CT scan of the patient from Fig. 1 showing two intra-articular loose bodies in the joint.
Table III.
Radiographic evaluation of acetabular morphology
| Patient number | Age/gender | LCEA (degrees) | AI (degrees) | Acetabular anteversion (degrees) |
|---|---|---|---|---|
| 1 | 12.5/F | 25 | 10 | 6 |
| 2 | 19.3/M | 25 | 5 | 18 |
| 3 | 17.9/M | 18 | 6 | 16 |
| 4 | 12.1/F | 28 | 0 | 15 |
| 5 | 12.9/M | 18 | 11 | 10 |
| 6 | 19.7/M | 25 | 2 | 20 |
| 7 | 11.3/F | 28 | 4 | 13 |
| 8 | 14.5/M | 23 | 8 | 9 |
| 9 | 11.7/M | 23 | 9 | 5 |
| 10 | 12.5/M | 32 | 5 | 10 |
| 11 | 24.3/M | 25 | 6 | 12 |
| 12 | 25.0/F | 21 | 4 | 16 |
LCEA, lateral center edge angle; AI, acetabular index.
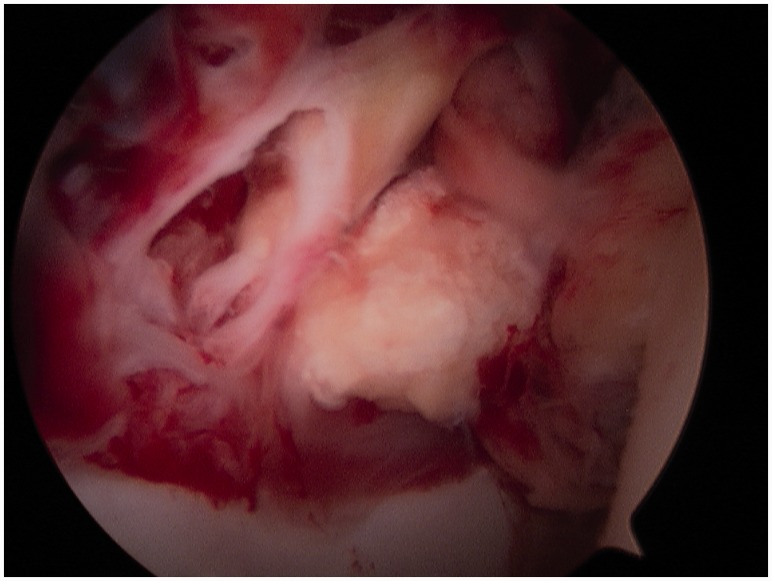
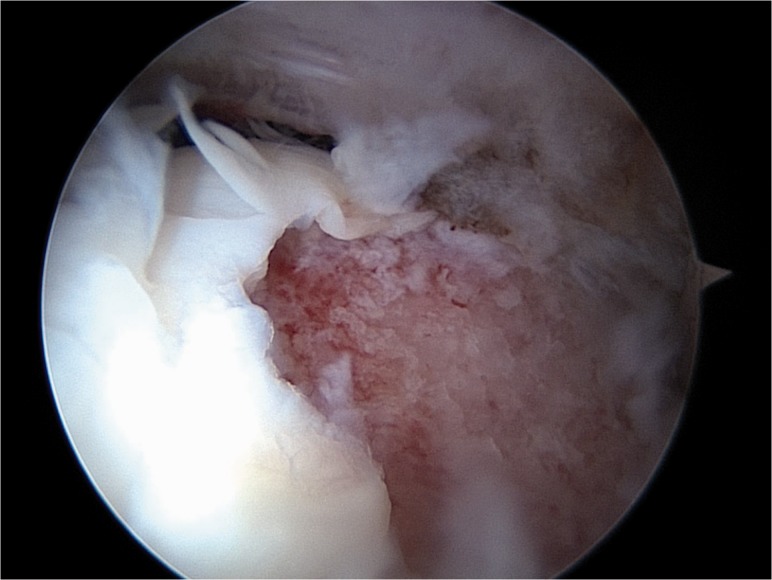
All patients underwent arthroscopy after their dislocation at a mean of 59 days after their injury (median 17 days, range 1–537 days). All but one had arthroscopy within 30 days of their injury (Table IV). Eight of 12 patients had intra-articular loose bodies at the time of arthroscopy (Fig. 3). The two patients who had chondral loose bodies that were not identified on preoperative imaging had only CT scans after their injury (Patient 3 and Patient 5). Labral injuries at the time of arthroscopy included three degenerative appearing labrums, three labrums with full thickness tears that were healing in good position and were not treated, one labrum that was separated and was repaired with suture anchors and one that was incarcerated in the joint and needed to be reduced for the hip joint to reduce properly. Femoral articular cartilage injuries included two patients with full-thickness defects and one with cartilage softening, these were debrided without other treatment as they were not in the weight bearing zone (Fig. 4). Acetabular cartilage injuries included three patients with cleavage/delamination injuries and two with cartilage softening. All 12 patients had a torn ligamentum teres that was debrided during surgery.
Table IV.
Arthroscopic findings
| Patient Number | Age/gender | Time to surgery (days) | Loose bodies |
Labral injury | Acetabular cartilage injury | Femoral cartilage injury | LT tear | |
|---|---|---|---|---|---|---|---|---|
| Y/N | Type | |||||||
| 1 | 12.5/F | 28 | No | NA | None | None | None | Yes |
| 2 | 19.3/M | 537 | No | NA | Separation | Malacia | None | Yes |
| 3 | 17.9/M | 9 | Yes | C | None | Delaminationa | Full-thicknessb | Yes |
| 4 | 12.1/F | 25 | No | NA | None | None | None | Yes |
| 5 | 12.9/M | 14 | Yes | C | Degenerated | None | Malacia | Yes |
| 6 | 19.7/M | 11 | Yes | OC | Full-thickness tear | Delaminationa | Full-thicknessb | Yes |
| 7 | 11.3/F | 1 | Yes | OC | None | None | None | Yes |
| 8 | 14.5/M | 1 | Yes | OC | Posterior labrum incarcerated | None | None | Yes |
| 9 | 11.7/M | 30 | Yes | C | Full-thickness tear | None | None | Yes |
| 10 | 12.5/M | 19 | No | NA | Degeneration | None | None | Yes |
| 11 | 24.3/M | 21 | Yes | OC | Full-thickness tear | Delaminationa | None | Yes |
| 12 | 25.0/F | 16 | Yes | OC | Degeneration | Malacia | None | Yes |
aAll delaminations were in the anterosuperior aspect of the joint.
bBoth full thickness defects were in the AL aspect of the femoral neck and were debrided.
NA—not applicable, C—chondral, OC—osteochondral, LT—ligamentum teres.
Fig. 3.
Arthroscopic image of patient from Figs 1 and 2 showing significant synovitis and osteochondral loose body in the joint that was removed.
Fig. 4.
Arthroscopic Image of patient with full-thickness AL femoral neck cartilage injury/defect with loose chondral flaps.
DISCUSSION
Pediatric and adolescent hip dislocation is an uncommon injury [2]. It is commonly treated with closed reduction and non-operative treatment. Vialle et al. [4] reported a series of 35 patients in which eight patients needed operative treatment due to osteochondral fragments or interposed soft tissues. Similarly, Mehlman et al. [3] reported on 42 children with traumatic hip dislocations and found that three needed operative treatment for open reduction with removal of interposed soft tissue or osteochondral fragments. Pediatric dislocations are less commonly associated with periarticular fractures compared with adults and are therefore less likely to undergo open operative intervention. Classical case series have reported good intermediate to long-term outcomes after hip dislocations in the young population with epiphyseal avascular necrosis being the most devastating complication and time to reduction the most important variable predictive of avascular necrosis [3]. Development of post-traumatic osteoarthritis seems to be less prevalent in the pediatric population. However, in the senior authors practice two adolescent patients developed severe post-traumatic arthritis after hip dislocation. This, along with the reports of a high incidence of loose bodies in adult patients, prompted the senior author to begin routine arthroscopic evaluation of patients after traumatic hip dislocation.
Recent studies in adults demonstrate a high percentage of patients with traumatic hip dislocations have intra-articular loose bodies at the time of arthroscopic evaluation [5–7]. Theoretically, these loose bodies can lead to third body wear within the joint causing joint degeneration and advanced osteoarthritis [9]. Mullis and Dahners [7] found intra-articular loose bodies in 33 of 36 patients including seven of nine with negative preoperative imaging [7]. Philippon et al. [5] found that all 14 professional athletes that underwent arthroscopy for continued hip pain after dislocation had labral and cartilage injuries requiring treatment. In their cohort, six patients underwent labral repair, eight underwent labral debridement and nine underwent microfracture for chondral defects. Similarly, Ilizaliturri et al. [6] reported 16 of 17 patients with labral damage and cartilage defects in all patients with intra-articular loose bodies in 14 patients . Our study is the first report on arthroscopic findings after dislocation in adolescent and young adult patients. We found eight of 12 patients with intra-articular loose bodies, two of which were not discovered on pre-operative imaging. We also found five patients with femoral or acetabular articular cartilage irregularities, two of which had both acetabular and femoral injuries. Eight of the 12 had labral injuries with one requiring fixation and one requiring reduction. Overall, compared with Ilizaliturri et al. [6] and Philippon et al. [5], we found fewer patients with labral and articular cartilage injury at the time of arthroscopy compared with their adult populations. This may be due to the fact that younger patients appear to have dislocations as a result of lower energy injuries compared with adults. Prior authors hypothesized this is due to more soft-tissue compliance in this age group [2]. We further investigated the patient’s acetabular morphology and found two patients with acetabular dysplasia (LCEA <20°) and seven with borderline dysplasia (LCEA between 20° and 25°). Some degree of dysplasia may be contributing to these low-energy hip dislocations in this young patient population. None of these studies, including ours, have compared a cohort of patients undergoing arthroscopy to those undergoing closed treatment alone, so we are unable to determine whether loose body removal and treatment of intra-articular pathology serves to prevent the development of post-traumatic osteoarthritis in the short and/or long-term following injury.
Limitations
This is an uncontrolled case series describing the incidence of intra-articular loose bodies and chondral and labral injuries after hip dislocation at the time of arthroscopy in young patients. Functional outcomes were not measured and there is no comparison to patients that had hip dislocations treated in a closed fashion without arthroscopy or those with open arthrotomy. Therefore, it is unclear as to whether the removal of chondral or osteochondral loose bodies leads to decreased third body wear and therefore preservation of the joint as has been hypothesized. There is also a selection bias as the senior author works at a large tertiary care pediatric medical center and patients referred there for treatment may be more likely to be symptomatic than a representative sample of all young patients with traumatic hip dislocations.
Conclusions
Intra-articular injuries and loose bodies are common in adolescent and young adult patients. Further studies are needed to determine whether arthroscopy after traumatic dislocation with loose body removal and treatment of intra-articular injuries helps to prevent the development of post-traumatic osteoarthritis.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1.Foulk DM, Mullis BH. Hip dislocation: evaluation and management. J Am Acad Orthop Surg 2010; 18: 199–209. [DOI] [PubMed] [Google Scholar]
- 2.Herrera-Soto JA, Price CT. Traumatic hip dislocations in children and adolescents: Pitfalls and complications. J Am Acad Orthop Surg 2009; 17: 15–21. [DOI] [PubMed] [Google Scholar]
- 3.Mehlman CT, Hubbard GW, Crawford AH, et al. Traumatic hip dislocation in children. Long-term followup of 42 patients. Clin Orthop Relat Res 2000; 376: 68–79. [PubMed] [Google Scholar]
- 4.Vialle R, Odent T, Pannier S, et al. Traumatic hip dislocation in childhood. J Pediatr Orthop 2005; 25: 138–44. [DOI] [PubMed] [Google Scholar]
- 5.Philippon MJ, Kuppersmith DA, Wolff AB, et al. Arthroscopic findings following traumatic hip dislocation in 14 professional athletes. Arthroscopy 2009; 25: 169–74. [DOI] [PubMed] [Google Scholar]
- 6.Ilizaliturri VM, Gonzalez-Gutierrez B, Gonzalez-Ugalde H, et al. Hip arthroscopy after traumatic hip dislocation. Am J Sports Med 2011; 39: 50S–7S. [DOI] [PubMed] [Google Scholar]
- 7.Mullis BH, Dahners LE. Hip arthroscopy to remove loose bodies after traumatic dislocation. J Orthop Trauma 2006; 20: 22–6. [DOI] [PubMed] [Google Scholar]
- 8.Keene GS, Villar RN. Arthroscopic loose body retrieval following traumatic hip dislocation. Injury 1994; 25: 507–10. [DOI] [PubMed] [Google Scholar]
- 9.Evans CH, Mazzocchi RA, Nelson DD, et al. Experimental arthritis induced by intraarticular injection of allogenic cartilaginous particles into rabbit knees. Arthritis & Rheum 1984; 27: 200–7. [DOI] [PubMed] [Google Scholar]
- 10.Pascarella R, Maresca A, Reggiani LM, et al. Intra-articular fragments in acetabular fracture-dislocation. Orthopedics 2009; 32: 402. [DOI] [PubMed] [Google Scholar]
- 11.Beck M, Kalhor M, Leunig M, et al. Hip morphology influences the pattern of damage to the acetabular cartilage: Femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br 2005; 87: 1012–8. [DOI] [PubMed] [Google Scholar]
- 12.Aoki SK, Beckmann JT, Wylie JD. Hip arthroscopy and the anterolateral portal: Avoiding labral penetration and femoral articular injuries. Arthrosc Tech 2012; 1: e155–60. [DOI] [PMC free article] [PubMed] [Google Scholar]