Abstract
The current literature on femoroacetabular impingement (FAI) is focused on acetabular orientation and femoral head asphericity, with little emphasis on the effect of version of the femoral neck. A biomechanical model was developed to determine the causative effect, if any, of femoral retroversion on hip contact stress and, if present, delineate the type of FAI with femoral neck retroversion. Five pairs of cadaveric hips (n = 10) were tested by loading the hip in 90° of flexion and measured the peak joint pressure and the location of the peak joint pressure. The experiment was repeated after performing a subtrochanteric osteotomy and retroverting the proximal femur by 10°. Ten hips were successfully tested, with one hip excluded due to an outlier value for peak joint pressure. Retroversion of the proximal femur significantly increased the magnitude of mean peak joint pressure. With retroversion, the location of the peak joint pressure was shifted posteroinferiorly in all cases. In conclusion, femoral neck retroversion increases peak joint pressure in the flexed position and may act as a cause of femoroacetabular impingement. The location of peak joint pressure suggests a pincer-type impingement with retroversion. The version of femoral neck should be assessed as a possible causative factor in patients with FAI, especially those with pincer-type impingement.
INTRODUCTION
Femoroacetabular impingement (FAI) is a mechanical conflict between acetabulum and femoral head/neck. It has been proposed that this conflict leads to abnormal contact stresses within a physiological range of motion, resulting in degeneration of the cartilage/labrum of the acetabulum and the early onset of osteoarthritis (OA) in young patients [1–5]. Three types of impingement have been recognized, namely, cam, pincer and mixed [2, 3]. Normal motion between the femoral head and acetabulum is rotation. However, FAI adds an abnormal linear component to this rotational motion.
FAI produces damage in two places: point of impact and point of shear. In cam impingement, an aspherical femoral head contacts a spherical socket, leading to shear stresses in the anterosuperior acetabulum [1, 3, 4, 6]. This results in what is described as a carpet phenomenon or shearing off of cartilage like a carpet as well as a labral tear. In pincer-type FAI, general or local overcoverage of the femoral head leads to a nutcracker effect on the labrum which gets pinched between the acetabular rim and femoral neck in deep flexion. General overcoverage may be due to acetabular retroversion, a deep acetabulum due to coxaprofunda or acetabular protrusion. Local overcoverage may be due to bony overgrowth of the acetabular rim. This has been termed as cranial or anterosuperior acetabular retroversion. The Pincer-type FAI also produces contrecoup lesions in the posterolateral acetabulum due to high contact stresses leading to posterolateral OA [1].
Although acetabular retroversion as a cause of FAI has been well established [1, 7–9], femoral neck retroversion as a cause of FAI has not been well described. Femoral retroversion could result from developmental conditions such as focal femoral deficiency, and dysplasia or be acquired secondary to malunited subtrochanteric, intertrochanteric or femoral neck fracture, varus derotational osteotomies and slipped capital femoral epiphysis (SCFE). A clear association between femoral neck retroversion, hip pain and OA has been described [4, 10, 11]. Patients with femoral version which has been reduced to zero following varus derotational osteotomy often present with hip pain which disappears once their version is brought back to the normal version of 15–20° [10, 12, 13]. Another study noted that the mean femoral neck anteversion of their cohort with FAI was lower in comparison to the control group [4]. Femoral neck fracture healing in retroversion of the femoral neck has been associated with FAI [14]. It was suggested that femoral retroversion after subcapital fractures decreased the femoral head neck offset, leading to a cam-type impingement. A biomechanical model explaining the role of femoral retroversion in FAI has not been previously studied and the type of impingement from femoral retroversion (cam versus pincer) remains to be elucidated.
The expectation was that with normal acetabular version, a retroverted femoral neck would lead to an increase in hip contact stress secondary to abnormal contact of the neck onto the acetabular rim. The null hypothesis was that femoral neck version would have no effect on acetabular contact pressures in a flexed position. Consequently, a novel cadaveric model was developed to study this hypothesis. The aims of the study were to: (1) create an in vitro biomechanical model to study effect of femoral neck retroversion on joint contact stress and assess impingement pattern; (2) assess the effect of femoral rotation and retroversion, alone and in combination, on the magnitude of joint contact stress; and (3) assess the effect of femoral rotation and retroversion, alone and in combination, on the location of peak joint contact stress and thereby delineate the pattern of FAI.
MATERIALS AND METHODS
Five fresh frozen cadaveric pelvises (average age 63.4 years; range 39–78) with 10 intact femora and hip joints were thawed at room temperature. The absence of acetabular retroversion was confirmed with plain AP pelvis radiographs with the X-ray beam centered over the symphysis pubis. Common plain radiographic criteria were used to assess for acetabular retroversion: the cross-over sign, the ischial spine sign and the posterior wall [15]. The joint capsule was removed to facilitate consistent placement of FujiFilm patterns for testing. However, the acetabular labrum was preserved and visual inspection confirmed the joints were free of impingement, particularly for any associated cam lesions. Physiologic saline was applied in between tests to maintain specimen hydration.
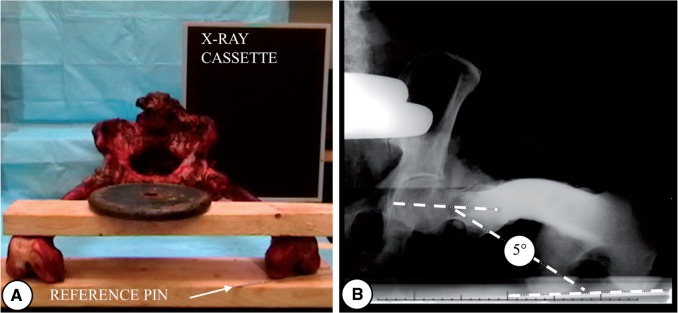
Femoral neck version was measured relative to the posterior condylar axis via axial radiographs (Fig. 1) as described previously [16]. The tube was kept at 120 cm from the center of femoral head. The femur was kept 10° abducted from midline and parallel to the floor. The posterior condylar axis was kept parallel to the floor, and a K-wire was coincidentally placed to show this alignment in X-rays. Femoral version was measured as the angle between the posterior condylar axis and the long axis of the femoral neck on the axial view. Femoral version ranged from 5° to 37° with mean of 18° (standard deviation 9.7°) comparable to that reported by others [17–20].
Fig. 1.
(A) Positioning of pelvis/femur for measurement of femoral neck version; (B) X-ray showing measurement of femoral neck version with reference to posterior condylar axis.
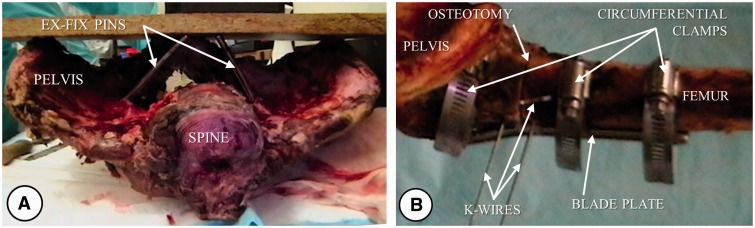
Steinmann pins were inserted in each of the iliac fossa near the arcuate line so that their free ends coincided with the plane defined by the ASIS and pubic symphysis (Fig. 2). The pelvis was split along the sagittal plane and secured in a 2″ × 3″ PVC connector using three 3.2-mm diameter K-wires and two #8 wood screws with washers prior to potting with polymethylmethacrylate (PMMA). This construct allowed rigid mounting of the pelvis onto a custom-designed fixture for testing of each hip. A rigid 3.2-mm diameter K-wire was inserted in the distal femur perpendicular to the plane of the posterior condylar axis to serve as a marker for femoral rotation. The distal femur was removed by a transverse osteotomy at 30 cm from the tip of the greater trochanter and the proximal femoral shaft was secured in a 6-cm segment of 2″ PVC tubing with two 3.2-mm diameter K-wires before potting with PMMA. This allowed secure mounting of the shaft in a custom-designed fixture attached to the Instron actuator (Fig. 3).
Fig. 2.
(A) External fixator pins to maintain pelvic plane prior to division of pelvis; (B) Subtrochanteric osteotomy with K-wires in situ prior to rotation.
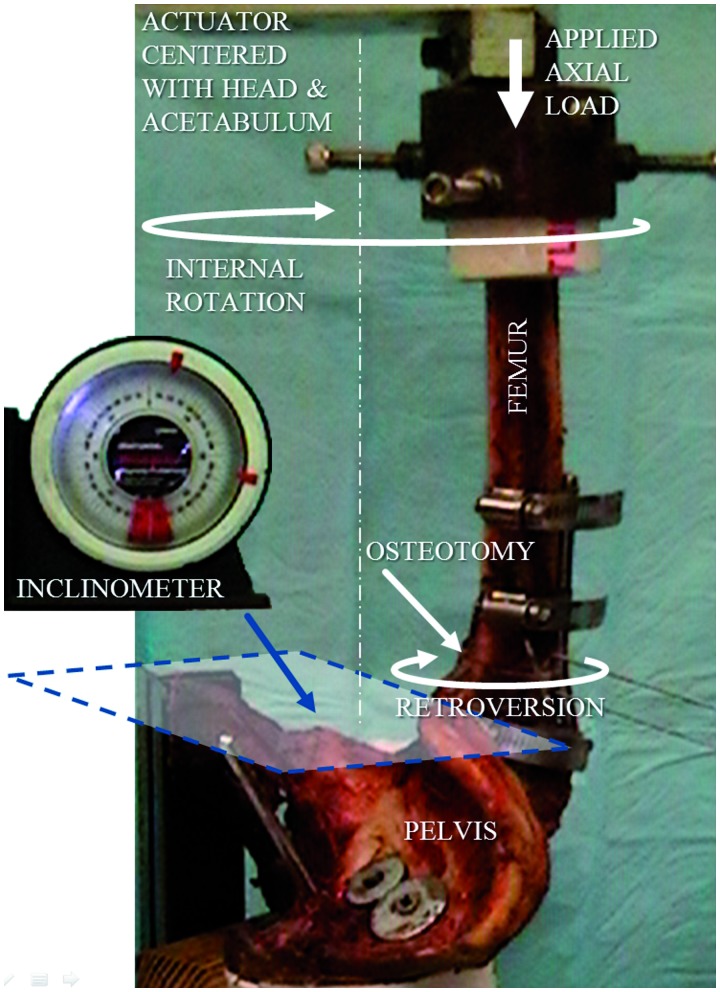
Fig. 3.
Assembly showing impingement model loaded on Instron.
Osteotomy
A subtrochanteric transverse osteotomy was cut 1.5 cm distal to the most prominent part of the lesser trochanter (Fig. 2). A five-hole angled blade plate (Synthes, Inc., Paoli, PA, USA) was placed across the osteotomy site. Rigid fixation was achieved by obtaining screw purchase in at least six cortices distally. Supplemental fixation was achieved by placing a fully threaded cancellous screw in the proximal fragment and circumferential clamps proximally and distally. Supplemental circumferential clamp fixation was necessary as screw holes were close to each other when the rotation was performed and new screws inserted. This allowed testing with and without relative femoral neck retroversion which was simulated by unscrewing the blade plate from the femur distal to the osteotomy, and rotating the distal fragment externally. A relative rotation of 10°, comparable to one standard deviation of the sample population, was consistently applied to all femurs to generate a significant shift into femoral retroversion. It was hypothesized that this should be sufficient to show any abnormal effect more specifically impingement. To control the application of relative retroversion, two K-wires were inserted, one proximal and one distal to the osteotomy. A third K-wire was inserted in the proximal fragment in such a manner that it would be parallel to the K-wire in the distal fragment with external rotation of the distal fragment (simulating retroversion of the neck) by 10°. Following this, the blade plate was reattached to the shaft and supplemented with circumferential clamps. The reverse of these steps returned the femur to its nonretroverted state.
Measurement of contact stress
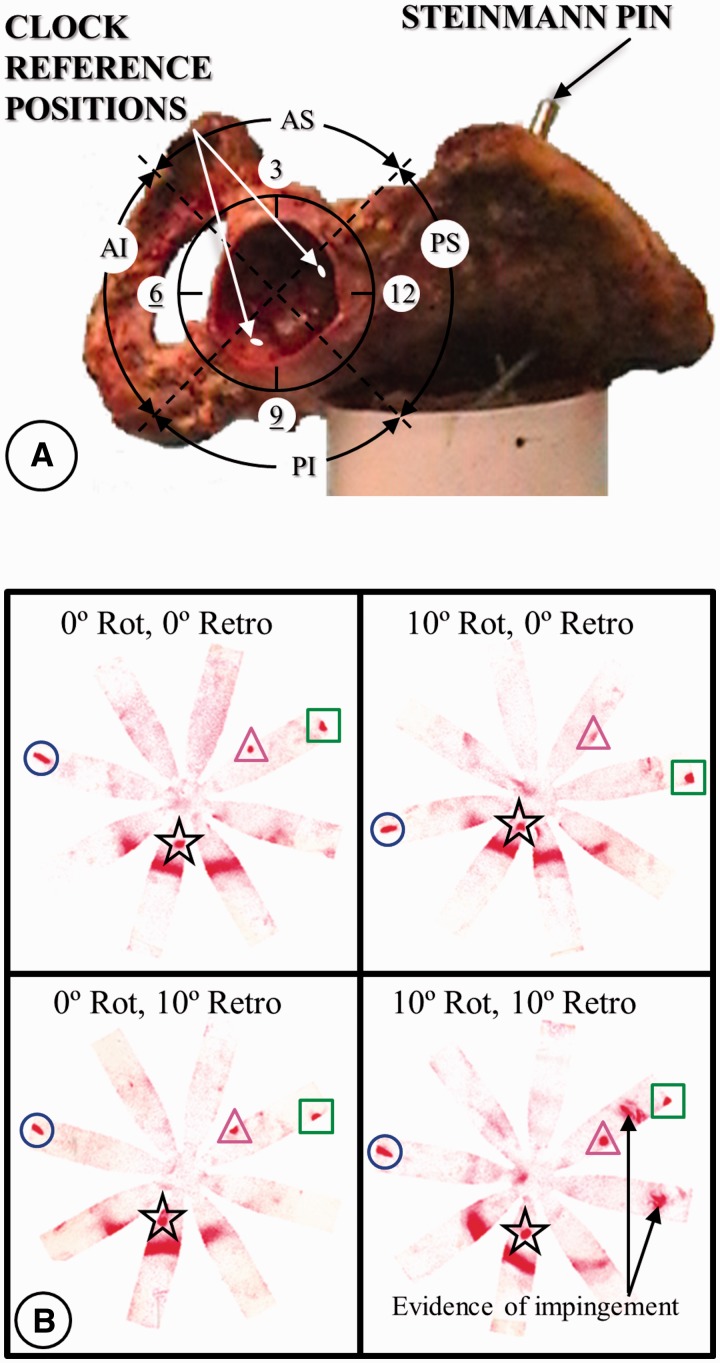
Specially prepared pre-cut Fujifilm (Low Prescale, Fujifilm Corp., Japan) was used to assess the impingement pattern and contact stress in the hip joints. The Fujifilm was calibrated with a custom fabricated pressure chamber to measure pressures from 2.5 to 13.5 MPa. While taking care to avoid wrinkling of the Fujifilm, it was pre-cut in an eight-pedal pattern, sealed with plastic wrap and contact adhesive to prevent film damage from joint fluids, and then mounted onto the femoral head for each test by covering it with the middle finger of a latex glove. A clock face and quadrants were used to facilitate description of stresses on the acetabular surface such that 6 o’clock centered on the transverse acetabular ligament, 12 o’clock was directly opposite, 3 o’clock was anterior and 9 o’clock posterior for both right and left hips [21–23]. Using a 4-mm drill bit two drill holes were made in the acetabulum 5 mm from the acetabular margin at 1 o’clock and 8 o’clock (Fig. 4). These holes provided access to manually create pressure points via smooth ended 3.2 mm rods during loading to assess the orientation of the film relative to the center of the acetabulum. Peak stress was measured from the color density of the Fujifilm using a Fuji CIPD-100 densitometer (C.Itoh & Co., Inc.). The radial distance from the center of the acetabulum to the peak pressure location was measured from digital scans of the patterns using NIH Image-J freeware (National Institutes of Health, Bethesda, MD, USA).
Fig. 4.
(A) Clock pattern superimposed over a left acetabulum with quadrants denoted as AS anterosuperior, AI anteroinferior, PS posterosuperior and PI posteroinferior.; (B) Corresponding pressure measurement on Fujifilm. Femoral neck reference marks are denoted by the circles (mid-posterior) and squares (mid-anterior). Acetabular reference marks are denoted by the triangles (1 o’clock) and stars (8 o’clock).
Loading conditions
Each specimen was mounted with the pelvis horizontal and the femur in 90° of flexion via a custom fixture for testing on a biaxial servohydraulic testing machine (Instron model 1321, Instron Corp., Canton, MA, USA) retrofitted with MTS TestStar II controller (MTS Corp., Eden Prairie, MN, USA) and the axis of rotation centered with the femoral head and acetabulum for each test combination of 0° and 10° internal rotation and 0° and 10° femoral retroversion (Fig. 3). For each combination, prior to any testing, Fujifilm was inserted into the unloaded hip to ensure that no pressure artifacts would be generated by the setup. Testing consisted of a 300-lb (1334 N) axial load applied via the distal femoral shaft to the hip thereby approximating the joint reaction force one might experience in rising from or lowering into a chair [24]. Internal rotation of 10° represented rotation that has been observed in normal subjects rising from a chair [25] and the level at which hip pain has been reported for symptomatic patients [6, 26]. At the completion of each test, the orientation of the film relative to the acetabulum was registered by marking the film at 8 and 1 o’clock positions (Fig. 4). Each combination was tested three times with a fresh Fujifilm pattern being used for each test. The average of those three repetitions was taken to represent each combination.
Statistical analysis
Peak density values were analyzed via Mixed Model ANOVA followed by Tukey–Kramer post hoc pair-wise comparisons (SAS, Cary, NC, USA). P values less than 0.05 were considered significant.
RESULTS
Ten cadaveric hips were successfully tested with this new protocol. Peak pressures for one hip was excluded from analysis after processing of data because its maximum pressures for the rotation alone, retroversion alone and combined rotation/retroversion states well exceeded the calibrated range of pressures that the film could measure. Also, one repetition for one other specimen (no rotation/no retroversion state) was excluded because its peak pressure exceeded the range. However, the distances of the peak pressures from the acetabula centers for these instances were measured and included in the analysis of that parameter. For all other specimens, the peak contact pressures were within the calibration limits. One specimen had evidence of bilateral cam lesions. It’s right hip lesion was very small and did not noticeably affect its pressure patterns. In contrast, the lesion on the left hip did produce an impingement pattern prior to retroversion or rotation suggesting cam impingement contributed to the pressure pattern in this hip. The pressures clearly increased with retroversion on these hips similar to other hips without evidence of cam lesions. This still reflected the role that pincer impingement played and thus the influence of retroversion as detected in our data.
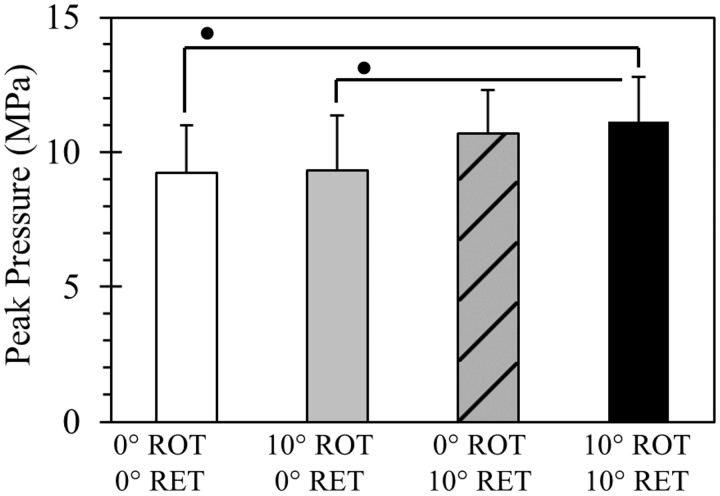
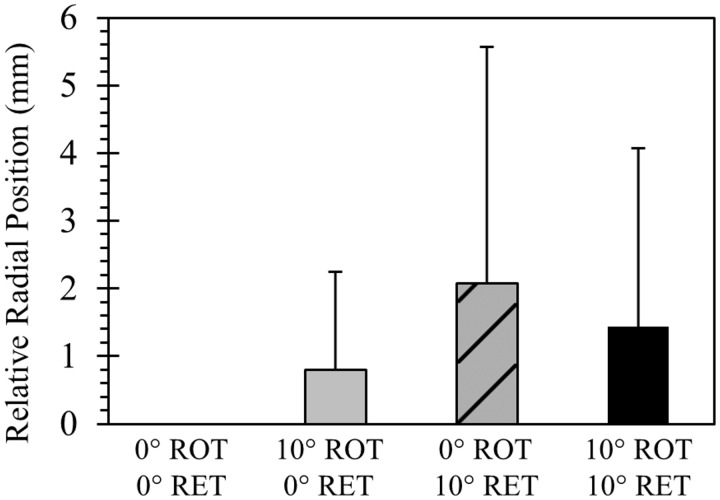
All test pressure patterns revealed contact stresses in the posteroinferior region. For tests of combined femoral retroversion and rotation, impingement was clearly evidenced by the appearance of localized contact stresses in the anterosuperior region (∼1 o’clock) of the acetabular rim (Fig. 4). Retroversion had a significant effect in increasing posteroinferior peak pressures (P < 0.001) while a significant effect was not found for rotation (P > 0.53) (Fig. 5). Post hoc pair-wise comparisons revealed that the mean peak pressure for the combined rotation and retroversion group was significantly higher than the group with no rotation or retroversion and was higher than the group with rotation alone (P < 0.03). Mean peak pressure for combined rotation and retroversion was not found to be statistically different from retroversion alone (P > 0.87). A trend was apparent, but not statistically significant, for mean peak pressure in the retroversion alone group to be higher than the no retroversion or rotation group and the rotation alone group (P > 0.13). A significant difference was not found between rotation alone and the no rotation or retroversion group (P > 0.99). Finally, a statistically significant effect in outward radial displacement of the peak contact pressure was found by retroversion (P < 0.04) but not by rotation (P > 0.89) (Fig. 6).
Fig. 5.
Peak pressures occurring for the different loading conditions: 0°ROT/0°RET = no rotation of femur and no retroversion of femoral neck prior to loading; 10°ROT/0°RET = 10° rotation of femur and no retroversion of femoral neck prior to loading; 0°ROT/10°RET = no rotation of femur and 10° retroversion of femoral neck prior to loading; 10°ROT/10°RET = 10° rotation of femur and 10° retroversion of femoral neck prior to loading. Statistically significant differences denoted by • P < 0.03.
Fig. 6.
Radial displacement of peak pressure point for the different loading conditions relative to no rotation and no retroversion: 0°ROT/0°RET = no rotation of femur and no retroversion of femoral neck prior to loading; 10°ROT/0°RET = 10° rotation of femur and no retroversion of femoral neck prior to loading; 0°ROT/10°RET = no rotation of femur and 10° retroversion of femoral neck prior to loading; 10°ROT/10°RET = 10° rotation of femur and 10° retroversion of femoral neck prior to loading.
A power analysis revealed that more than 26 hips would be required to achieve 80% power for the pair-wise comparisons for which statistical significance could not be established. However, the significant effect of femoral retroversion has already been established with the existing data and additional tests would not likely produce additional information of clinical relevance.
DISCUSSION
The current literature on FAI is focused on acetabular geometry and femoral head eccentricity. The role of femoral neck retroversion in FAI is unclear, and the pattern of FAI seen in femoral neck retroversion has been a matter of speculation [27–29]. Femoral version by definition is the angle measured in the coronal plane between the femoral neck and posterior condylar axis/transepicondylar axis of knee. Derotational osteotomies have been used to correct femoral retrotorsion and have been shown to decrease pain associated with impingement. The premise used in our model was that if derotation can correct retroversion, a rotational osteotomy should be able to produce retroversion [30]. Matsuda et al [27] corrected femoral retroversion in their case report by doing bilateral proximal femoral derotational osteotomies. Huber et al. [31] showed that decreased femoral antetorsion was associated with hip pain and possible femoral acetabular impingement. They did subtrochanteric derotational osteotomy to successfully correct impingement. Thus, it was hypothesized that femoral neck retroversion with normal acetabular version would induce a pincer-type FAI and result in increased hip contact stress secondary to the impingement. To test this hypothesis, a biomechanical model was developed to study FAI with cadaveric specimens.
Limitations of the study include small sample and a simplified unidirectional loading condition as opposed to the complex loads that are in effect in vivo. Secondly, the effect of various muscular vectors that might affect the peak joint pressure was not incorporated. We believe our position of loading and use of peak contact pressures did produce clinically relevant impingement. Our loading with the femur in 90° of flexion, with 10° of internal rotation, approximates the initiation of sitting to standing which has been shown as a critical activity [32] and common position for impingement in a retroverted femoral neck [28]. The load was applied axially along the femur to approximate the direction of load experienced by the hip during sitting to standing [33]. While our model is a simplification of complex interaction of forces along the hip joint, this approximates the direction and magnitude [24, 33] of peak contact force vector in sitting to standing position. Lastly, peak contact pressures were evaluated since this measure has been used as a means of predicting future OA in mathematical models of human hips [34]. Thirdly, a single fixed load of 300 pounds was imposed, which is likely to vary from person to person and with activity. Fourthly, the retroversion created by osteotomy at the subtrochanteric level may differ biomechanically from the ones seen in femoral neck fractures or SCFE. A 300-lb load was chosen as an approximation of the joint reaction force one might experience in rising from or lowering into a chair [24]. Proximal femoral and subtrochanteric osteotomies have been used to correct retroversion/retrotorsion in FAI [27, 30, 31]. Thus, a subtrochanteric osteotomy was chosen for this model as it was easily reproducible, retroversion could be calibrated and the osteotomy could be rigidly fixed. Despite the above limitations, the standardized loading conditions enable conclusions to be drawn regarding the effect of femoral retroversion on peak joint pressures and delineate its role in FAI.
Testing for FAI was successfully demonstrated by measuring peak joint pressures in hips loaded to 300 lb (1334 N) in 90° of flexion. Brown and Shaw measured hip joint contact pressures in an in vitro model using implanted transducers and found an average peak pressure of 8.8 MPa (range ∼3.8–14.5 MPa) for an applied load of 2700 N [35]. Olson et al. [36] in a cadaveric model showed peak pressures of 5.6–10.5 MPa for intact acetabula loaded to 2000 N in simulated single-leg stance. Other cadaveric models for loading the hip at or near vertical have shown peak pressures between 3.8 and 9.8 MPa over a range of loads up to 3.5 times body weight [37, 38]. The mean peak pressure with no rotation or retroversion in this study was 9.3 MPa (range 7.2–12.2 MPa). While this range is comparable to the other studies cited, it occurs at a lower applied load, likely due to the loading scenario of rising from or lowering into a chair [24]. This variation is likely from loading the hip in 90° of flexion, simulating a joint reaction force that might occur when rising from or lowering into a chair when FAI might occur, while previous studies have studied loading to simulate single leg stance.
Normal femoral version has been described to be from 15° to 20° [11]. Several studies have shown the association of decreased femoral neck version and hip pain [4, 9, 11]. While femoral head retroversion is a known cause of FAI [2] and has been postulated to cause cam FAI, no studies have conclusively shown femoral neck retroversion as a cause of pincer-type FAI. In the study by Heller et al. [39], increased anteversion by 30° in endoprosthesis lead to increased hip contact forces and bending moments up to 28%. There are no cadaveric biomechanical studies for femoral retroversion and hip contact stresses. A recent finite element analysis study showed a 10° variation in femoral version brought significant differences in hydrostatic pressures in hip joint [40]. Femoral retroversion significantly elevated the peak joint pressures in this study. Hip contact stresses are believed to be one of the key factors in development of OA of hip. Higher peak joint pressure has been shown to lead to the development of OA [15] and to earlier hip Arthroplasty [34]. The data in this study showed that femoral retroversion increases the peak joint pressure and could possibly be a factor in the etiology of FAI and OA. These findings are consistent with those of Ito et al. [4] who noted that the femoral neck version was lower in symptomatic patients with FAI when compared with matched healthy controls.
The model in this study showed visible contact of neck onto acetabular rim when it was retroverted, flexed and internally rotated suggestive of nut cracker effect seen in pincer impingement. The displacement of the peak joint pressure with femoral retroversion was radially outward within the posteroinferior quadrant of the specimens tested, further correlating with the fact that impingement with femoral neck retroversion is of the pincer type. The magnitude of displacement with combined rotation and retroversion was significantly greater when compared to rotation alone. This could be explained by the effect of impingement leading to subtle hip subluxation in a posterolateral direction. Finite element models of Liechti et al. [41] showed highest contact pressures occurred during standing to sitting in a region corresponding to clinically observed cartilage damage in the posteroinferior acetabulum of severe pincer hips. Also, Beck et al. [1] have previously demonstrated that the location of predominant cartilage damage with pincer impingement lies in the posteroinferior quadrant while that of cam impingement lies in the anterosuperior quadrant. This finding was supported by a later MRI-based study [42]. Cam-type impingement was evident with femoral neck fractures healed in retroversion. It must be noted that the majority of their cohort had subcapital femoral neck fracture and hence the retroversion was of the head relative to the neck rather than of the neck itself [14]. The mechanism of impingement might thus differ depending on the level of retroversion. While the work of Eijer et al. [14] suggests that retroversion at the subcapital level results in a cam-type impingement, the data in this study suggests that a true retroversion at or distal to the base of the neck would result in a pincer-type impingement. These findings are applicable to cases with a true retroversion of the neck.
CONCLUSION
This study supports the hypothesis that femoral neck retroversion leads to increased hip contact stresses as evidenced by the visible FAI of pincer type with correlated pressure patterns. The observed pattern of increased hip joint contact stresses correlates with the OA pattern seen clinically in pincer-type FAI. This conclusion needs to be correlated in clinical models.
FUNDING
Department of Orthopaedic Surgery at Virginia Commonwealth University’s School of Medicine.
CONFLICT OF INTEREST STATEMENT
W.J. is a consultant for and receives royalties from DePuy, Inc.
REFERENCES
- 1.Beck M, Kalhor M, Leunig M, et al. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br 2005; 87: 1012–18. [DOI] [PubMed] [Google Scholar]
- 2.Ganz R, Parvizi J, Beck M, et al. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res 2003; 417: 112–20. [DOI] [PubMed] [Google Scholar]
- 3.Ganz R, Leunig M, Leunig-Ganz K, et al. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res 2008; 466: 264–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ito K, Minka MA, 2nd, Leunig M, et al. Femoroacetabular impingement and the cam-effect. A MRI-based quantitative anatomical study of the femoral head-neck offset. J Bone Joint Surg Br 2001; 83: 171–6. [DOI] [PubMed] [Google Scholar]
- 5.Ellermann J, Ziegler C, Nissi MJ, et al. Acetabular cartilage assessment in patients with femoroacetabular impingement by using T2* mapping with arthroscopic verification. Radiology 2014; 271: 512–23. [DOI] [PubMed] [Google Scholar]
- 6.Nötzli HP, Wyss TF, Stoecklin CH, et al. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br 2002; 84: 556–60. [DOI] [PubMed] [Google Scholar]
- 7.Lequesne M, Bellaïche L. Anterior femoroacetabular impingement: an update. Joint Bone Spine 2012; 79: 249–55. [DOI] [PubMed] [Google Scholar]
- 8.Siebenrock KA, Schoeniger R, Ganz R. Anterior femoro-acetabular impingement due to acetabular retroversion. Treatment with periacetabular osteotomy. J Bone Joint Surg Am 2003; 85: 278–86. [DOI] [PubMed] [Google Scholar]
- 9.Tibor LM, Leunig M. The pathoanatomy and arthroscopic management of femoroacetabular impingement. Bone Joint Res 2012; 1: 245–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tönnis D, Heinecke A. Diminished femoral antetorsion syndrome: a cause of pain and osteoarthritis. J Pediatr Orthop 1991; 11: 419–31. [DOI] [PubMed] [Google Scholar]
- 11.Tönnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am 1999; 81: 1747–70. [DOI] [PubMed] [Google Scholar]
- 12.Sennerich T, Sutter P, Ritter G, et al. Computerized tomography follow-up of the ante-torsion angle after femoral shaft fractures in the adult. Unfallchirurg 1992; 95: 301–5. [PubMed] [Google Scholar]
- 13.Wissing H, Spira G. Determination of rotational defects of the femur by computer tomographic determination of the antetorsion angle of the femoral neck. Unfallchirurgie 1986; 12: 1–11. [DOI] [PubMed] [Google Scholar]
- 14.Eijer H, Myers SR, Ganz R. Anterior femoroacetabular impingement after femoral neck fractures. J Orthop Trauma 2001; 15: 475–81. [DOI] [PubMed] [Google Scholar]
- 15.Jamali AA, Mladenov K, Meyer DC, et al. Anteroposterior pelvic radiographs to assess acetabular retroversion: high validity of the “cross-over-sign”. J Orthop Res 2007; 25: 758–65. [DOI] [PubMed] [Google Scholar]
- 16.Dunn DM. Anteversion of the neck of the femur; a method of measurement. J Bone Joint Surg Br 1952; 34: 181–86. [DOI] [PubMed] [Google Scholar]
- 17.Gulan G, Matovinović D, Nemec B, et al. Femoral neck anteversion: values, development, measurement, common problems. Coll Antropol 2000; 24: 521–7. [PubMed] [Google Scholar]
- 18.Khang G, Choi K, Kim CS, et al. A study of Korean femoral geometry. Clin Orthop Relat Res 2003; 406: 116–22. [DOI] [PubMed] [Google Scholar]
- 19.Koerner JD, Patel NM, Yoon RS, et al. Femoral version of the general population: does “normal” vary by gender or ethnicity? J Orthop Trauma 2013; 27: 308–11. [DOI] [PubMed] [Google Scholar]
- 20.Yun HH, Yoon JR, Yang JH, et al. A validation study for estimation of femoral anteversion using the posterior lesser trochanter line: an analysis of computed tomography measurement. J Arthroplasty 2013; 28: 1776–80. [DOI] [PubMed] [Google Scholar]
- 21.Blankenbaker DG, De Smet AA, Keene JS, et al. Classification and localization of acetabular labral tears. Skeletal Radiol 2007; 36: 391–97. [DOI] [PubMed] [Google Scholar]
- 22.Leunig M, Werlen S, Ungersböck A, et al. Evaluation of the acetabular labrum by MR arthrography. J Bone Joint Surg Br 1997; 79: 230–4. Erratum in: J Bone Joint Surg Br 1997; 79: 693. [DOI] [PubMed] [Google Scholar]
- 23.Wasielewski RC, Cooperstein LA, Kruger MP, et al. Acetabular anatomy and the transacetabular fixation of screws in total hip arthroplasty. J Bone Joint Surg Am 1990; 72: 501–8. [PubMed] [Google Scholar]
- 24.Johnston JD, Noble PC, Hurwitz DE, et al. Biomechanics of the Hip. In: Callaghan JJ, Rosenberg AG, Rubash HE. (eds) The Adult Hip. Vol I, 2nd ed Philadelphia, PA: Lippincott Williams & Wilkins, 2007:81–90. [Google Scholar]
- 25.Nadzadi ME, Pedersen DR, Yack HJ, et al. Kinematics, kinetics, and finite element analysis of commonplace maneuvers at risk for total hip dislocation. J Biomech 2003; 36: 577–91. [DOI] [PubMed] [Google Scholar]
- 26.Wyss TF, Clark JM, Weishaupt D, et al. Correlation between internal rotation and bony anatomy in the hip. Clin Orthop Relat Res 2007; 460: 152–8. [DOI] [PubMed] [Google Scholar]
- 27.Matsuda DK, Gupta N, Martin HD. Closed intramedullary derotational osteotomy and hip arthroscopy for cam femoroacetabular impingement from femoral retroversion. Arthrosc Tech 2014; 3: e83–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moya L, Buly R, Henn F, et al. Femoral retroversion in patients with Femoroacetabular impingement: A cofactor in the development of hip osteoarthritis. J Bone Joint Surg Br 2010; 92(suppl IV): 526. [Google Scholar]
- 29.Steppacher SD, Albers CE, Siebenrock KA, et al. Femoroacetabular impingement predisposes to traumatic posterior hip dislocation. Clin Orthop Relat Res 2013; 471: 1937–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kamath AF, Ganz R, Zhang H, et al. Subtrochanteric osteotomy for femoral mal-torsion through a surgical dislocation approach. J Hip Pres Surg 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Huber H, Haefeli M, Dierauer S, et al. Treatment of reduced femoral antetorsion by subtrochanteric rotational osteotomy. Acta Orthop Belg 2009; 75: 490–6. [PubMed] [Google Scholar]
- 32.Chegini S, Beck M, Ferguson SJ. The effects of impingement and dysplasia on stress distributions in the hip joint during sitting and walking: a finite element analysis. J Orthop Res 2009; 27: 195–201. [DOI] [PubMed] [Google Scholar]
- 33.Bergmann G, Deuretzbacher G, Heller M, et al. Hip contact forces and gait patterns from routine activities. J Biomech 2001; 34: 859–71. [DOI] [PubMed] [Google Scholar]
- 34.Recnik G, Kralj-Iglic V, Iglic A, et al. Higher peak contact hip stress predetermines the side of hip involved in idiopathic osteoarthritis. Clin Biomech (Bristol, Avon) 2007; 22: 1119–24. [DOI] [PubMed] [Google Scholar]
- 35.Brown TD, Shaw DT. In vitro contact stress distributions in the natural human hip. J Biomech 1983; 16: 373–384. [DOI] [PubMed] [Google Scholar]
- 36.Olson SA, Bay BK, Chapman MW, et al. Biomechanical consequences of fracture and repair of the posterior wall of the acetabulum. J Bone Joint Surg Am 1995; 77: 1184–92. [DOI] [PubMed] [Google Scholar]
- 37.von Eisenhart R, Adam C, Steinlechner M, et al. Quantitative determination of joint incongruity and pressure distribution during simulated gait and cartilage thickness in the human hip joint. J Orthop Res 1999; 17: 532–9. [DOI] [PubMed] [Google Scholar]
- 38.Rushfeldt PD, Mann RW, Harris WH. Improved techniques for measuring in vitro the geometry and pressure distribution in the human acetabulum – II. Instrumented endoprosthesis measurement of articular surface pressure distribution. J Biomech 1981; 14: 315–23. [DOI] [PubMed] [Google Scholar]
- 39.Heller MO, Bergmann G, Deuretzbacher G, et al. Influence of femoral anteversion on proximal femoral loading: measurement and simulation in four patients. Clin Biomech (Bristol, Avon) 2001; 16: 644–9. [DOI] [PubMed] [Google Scholar]
- 40.Sánchez Egea AJ, Valera M, Parraga Quiroga JM, et al. Impact of hip anatomical variations on the cartilage stress: a finite element analysis towards the biomechanical exploration of the factors that may explain primary hip arthritis in morphologically normal subjects. Clin Biomech (Bristol, Avon) 2014; 29: 444–50. [DOI] [PubMed] [Google Scholar]
- 41.Liechti EF, Ferguson SJ, Tannast M. Protrusio acetabuli: joint loading with severe pincer impingement and its theoretical implications for surgical therapy. J Orthop Res 2015; 33: 106–13. [DOI] [PubMed] [Google Scholar]
- 42.Bittersohl B, Steppacher S, Haamberg T, et al. Cartilage damage in femoroacetabular impingement (FAI): preliminary results on comparison of standard diagnostic vs delayed gadolinium-enhanced magnetic resonance imaging of cartilage (dGEMRIC). Osteoarthritis Cartilage 2009; 17: 1297–306. [DOI] [PubMed] [Google Scholar]