Abstract
With improvements in early detection and treatment, the number of cancer survivors has been on the rise. Studies suggest that cancer survivors do not often receive proper follow-up care despite existing guidelines. Patient engagement is key to healthy survivorship, and mHealth provides a viable platform to empower survivors with just- in-time personalized support. However, our understanding of existing mHealth solutions in cancer survivorship is limited. In this paper, we use Patient Engagement Framework to investigate existing apps to bridge this knowledge gap. App features are mapped to the framework components to determine the level of engagement facilitated. Ability to record treatment summaries has been found in five out of seven apps examined. While collaborative care and social engagement are found minimally, the majority of features (95%) are limited to information and way finding, e-tools, and interactive forms. Limitations of the existing apps and possible improvements to the framework are discussed.
Introduction and Background
“Cancer survivors” refers to those people who have been diagnosed with cancer and the people in their lives who are affected by their diagnosis, including family members, friends, and caregivers [1]. The number of cancer survivors continues to increase due to the aging and growth of the population and improvements in early detection and treatment. As of January 2014, it is estimated that there are 14.5 million cancer survivors in the United States. By January 1, 2024, that number will increase to nearly 19 million [2]. Unfortunately, the current U.S. health care system is failing to deliver the comprehensive and coordinated follow-up care cancer survivors need. As per the Institute of Medicine report in 2006, too many survivors are lost in transition once they complete the cancer treatment [3]. This population is at risk not only for cancer recurrence, but also for receiving inadequate risk-based and routine preventative health care. In response to this, the Institute of Medicine report in 2006 recommended that every cancer patient should receive an individualized survivorship care plan that includes guidelines for monitoring and maintaining their health to help improve the quality of care of survivors as they move beyond their cancer treatment [4]. The basic components of survivorship care plans (SCPs) include a personalized comprehensive care summary and follow-up plan. SCPs are intended to be a patient-centered communication tool to improve the quality of follow-up care for cancer survivors. Although many SCPs have been developed, the incorporation of these plans into processes of care coordination and the ability of SCPs in empowering patients to self-manage their care has been limited [5, 6].
Mobile health technologies play an important role in helping cancer patients to become active participants in their care. Given the ubiquity of mobile devices and the omnipresent wireless connectivity, mHealth solutions have the capability to provide just-in-time support that is both adaptive and targeted to user needs [7]. mHealth solutions can be used to generate and share patient-centered care planning, to manage late effects with cancer and its treatments, to promote lifestyle and behavioral changes, and to assist survivors with communication with health care providers. Several research projects have examined the utility of mobile tools in supporting breast cancer patients. Healthweaver Mobile project, [8] and My Journey Compass [9] afforded cancer patients the ability to engage with their health, their health providers and their support networks. Although mobile apps have the potential for helping cancer survivors to manage their care, our understanding of the current state of mHealth in cancer survivorship is limited in terms of their ability to empower cancer survivors to self-monitor their care plans and engage in healthy living.
The objectives of our study are threefold: (1) to understand the role of mHealth in the facilitation of patient engagement in cancer survivorship care, (2) to identify the strengths and shortcomings of the current mobile apps geared towards empowering cancer survivors in self-management of their care and overall well-being, (3) to examine the applicability of available engagement framework in the assessment of survivorship mobile apps. In this paper, we specifically employ the Patient Engagement Framework (PEF) to describe the engagement features facilitated by the existing mHealth apps for cancer survivors. In the next sections of the paper, we discuss in detail the various components of PEF, our evaluation methodology, and subsequent results and discussions.
Theoretical Rationale
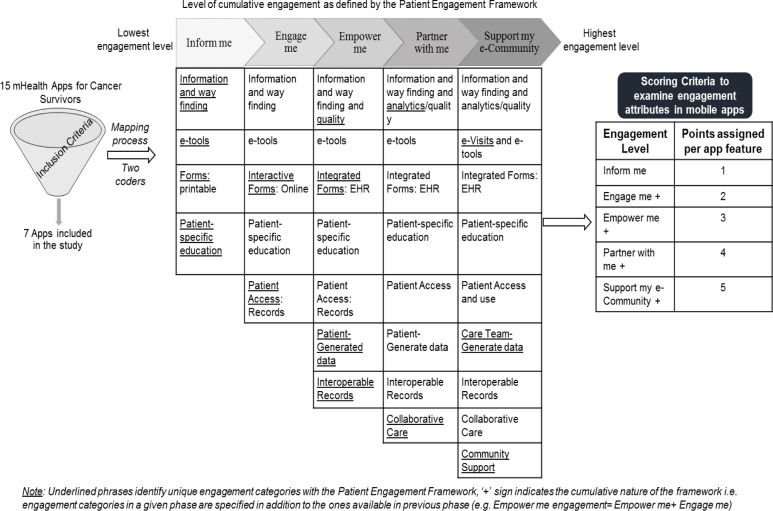
The Patient Engagement Framework (PEF) is a model created to guide healthcare organizations in developing and strengthening their patient engagement strategies through the use of eHealth tools and resources. The framework was first introduced in November 2012 by the National eHealth Collaborative [10] after a yearlong effort by over 150 top experts in healthcare, technology and human behaviors. PEF can be used as a guidance to evaluate the functionality of cancer survivor survivorship apps that potentially facilitate the adoption of SCPs, patient engagement, self-management of cancer, healthy behavioral change, goal setting and reinforcement, peer support, and assist survivors with communication with health care providers. PEF consists of five phases that begin with providing information and progress toward more active partnering and engagement [11]. The five cumulative phases to engagement that make up the framework include “inform me,” “engage me,” “empower me,” “partner with me,” and “support my e-community.” Each phase is described below along with specific examples relevant to cancer survivors.
Inform me phase is about providing basic information on how to find the facility, providers, and services and with various electronic patient education information sources.
Engage me phase is about engaging patients through health and wellness apps to monitor their diet, weight, and exercise routine and track health data, patient self-entering their health records and data, sending appointment and medication reminders by text messaging.
Empower me phase is about offering secure text messaging with providers and engaging in customized text reminders for daily care, health and symptom assessment.
Partner with me phase is about monitoring patients and tracking patient’s health data remotely.
Support my e-Community phase is about offering online e-community support forums for better information exchange between survivors.
In addition to the phases which determine the level of engagement, the framework has 14 different categories that can help facilitate the intended level of engagement. PEF categories across the five phases include 1) Information and Way-finding, 2) Analytics/Quality, 3) e-Tools, 4) e-Visits, 5) Forms: Printable, 6) Interactive Forms: Online, 7) Integrated Forms: EHR, 8) Patient-Specific Education, 9) Patient Access: Records, 10) Patient-Generated Data, 11) Care Team-Generated Data, 12) Interoperable Records, 13) Collaborative Care and 14) Community Support. Within each of these categories, sample elements were provided as part of the framework to guide the system development process. Please see Figure 1 for detailed information regarding the various components (Phase, Category, and Sample Elements) associated with the PEF. As indicated in Figure 1, patient engagement level is embedded as a cumulative dimension of the framework, i.e. engagement categories in a given phase are specified in addition to the ones available in previous phase (e.g. Empower me engagement= Empower me+ Engage me). In this paper, we used the basic version of the PEF to develop a rigorous evaluation method that enables the examination of the user engagement features facilitated by existing cancer survivorship applications on mobile platforms.
Figure 1.
Evaluation methodology using Patient Engagement Framework for mHealth apps in Cancer Survivorship
Methods
Study design
This study presents a descriptive assessment and review of the cancer survivorship applications available from the mobile app stores. Two researchers assessed each of the selected apps using PEF independently to determine phases and features of patient engagement. The features of each app were mapped to these 14 categories to assess the level of patient engagement facilitated by the apps. The app features mapped to a particular PEF category were scored based on the phase of patient engagement: 1 point for a feature with inform me phase, 2 points for a feature with engage me phase, 3 points for a feature with empower me phase, 4 points for a feature with partner with me phase and 5 points for a feature with support my e-community phase. The total PEF score for each app was computed by adding up the points assigned to all features embedded in that app.
Selecting Apps for Review
We searched Apple Store, iTunes, Google Play, Nokia Store, BlackBerry App World and Windows Phone for current available mobile applications using the keywords “cancer survivors”, “cancer survivorship”, “survivor care” and “care plan” in November 2014. Initial search returned 15 related cancer survivorship applications. The inclusion criteria defined for this study are 1) target users are cancer survivors who have completed cancer treatment, and 2) content include either follow-up care plan or late effect management or healthy lifestyle or stress management. Of the 15 apps retrieved using the search terms, seven applications were identified to meet the criteria. We examined the features of these seven apps to categorize their features using PEF as discussed in the study design. After completing mapping of the applications to PEF, two researchers assessed their reliability of agreement using Cohen’s Kappa measure. The coders had a reliability of κ=.76, indicating strong consistency and reliability in the coding process.
Results and Discussion
Table 1 shows the general descriptions for the apps. All these seven apps are designed for cancer survivors who have completed their cancer treatment. Among the seven apps, five apps have comprehensive treatment summary or follow up care plans. Three apps provide support infrastructure for late effects management, while two apps were designed for childhood cancer survivors. One application provides a networking platform to connect cancer survivors and caregivers to a network of healthcare providers specializing in cancer survivorship. Of the seven apps, two were developed by hospital entities, one by a research university and four by non-profit organizations with or without university collaborations. A detailed description for each of the apps is provided in Table 1.
Table 1.
General information about mobile apps for cancer survivors evaluated in this study
| Apps | Developer | General description |
|---|---|---|
| App 1 | University Hospital | This survivor app supports patients during survivorship phase. This app includes information on recovering and remaining healthy after cancer treatment. It has interactive tools to keep track of questions to ask doctors. It provides individualized end-of-treatment summary and survivorship care plans. Unique feature is only available to testicular cancer survivors. |
| App 2 | Non-profit organization | This app connects cancer survivors and caregivers to a network of healthcare providers specializing in cancer survivorship. This app can help people in taking charge of their personal and financial health by providing education and information regarding survivorship care plan and healthy lifestyle. |
| App 3 | University | This app is for survivors who have completed their treatment for breast cancer. The app enables users to record treatment summary and then email right from their phone to any provider that they might see in the future. |
| App 4 | Collaboration of Non-profit organization and university research group | This app will help cancer survivors create Survivorship Care Plan. It allows cancer survivors to initiate their own SCP and then complete with the help of provider. The survivor and her/his healthcare team can use this app to coordinate the follow-up care and manage ongoing symptoms. |
| App 5 | Non-profit organization | This app is to help survivors understand and minimize the side effects of cancer and cancer treatment. It offers nutrition guidance and practical tips to help survivors feel better, maintain their strength, and speed their recovery from common cancer side effects. |
| App 6 | Collaboration of Non-profit organization and university research group | This app is designed for Adolescent and Young Adult (AYA) cancer survivors (ages 15–39). It is an interactive app to assess health habits and general sense of well-being. It offers personalized tips for being more active, eating better and living a healthier life. |
| App 7 | Hospital | This app offers childhood cancer survivors the resources, tips, and tools necessary to help minimize potential problems, or late effects, caused by childhood cancer and/or its treatments. |
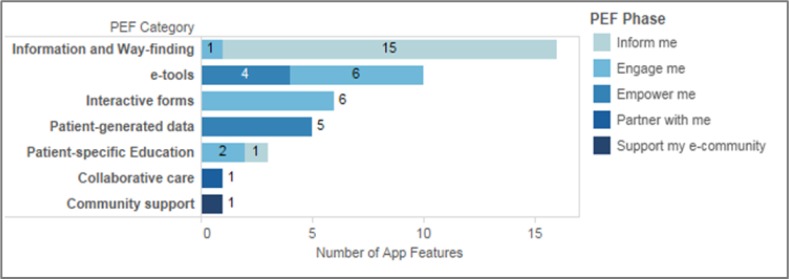
We observed 42 features in total for all of these seven applications. On average, there are six features for each app. We aligned all the observed features to the 14 categories within PEF. Overall, the 42 app features mapped to seven of the 14 PEF categories described in the previous sections. Majority of the apps (five out of seven) had the ability to record personal health information and treatment summaries. A detailed distribution of the app features across the engagement categories can be seen in Figure 2.
Figure 2.
Distribution of App features across Patient Engagement Categories
Results indicated that the survivorship app features were mapped to only half of the PEF engagement categories while there are no features to map to the other half. The PEF categories that have features mapped to include- Information and Way-finding, e-Tools, Interactive Forms, Patient-Specific Education, Patient-Generated Data, Collaborative Care and Community Support. These categories support several functions such as:
Providing basic information on how to find the facility, providers, and services and with various electronic patient education information sources and tools for care plan creation;
Facilitating patients to create care plan, self-enter their patient medical history and manage their medical documents;
Tracking health data and lifestyle (diet, weight, and exercise routine); sending appointment and medication reminders by text messaging;
Sending text reminders for daily care, health and symptom assessment;
Offering social media to potentially support better information exchange among survivors; and
Providing support environment through online communities, where cancer survivors can engage in peer-to-peer communication.
Such features can enable users to access, and organize health-related information, while promoting patient-provider communication. Through reminder capabilities, the apps allow patients to comply with care follow-up services as recommended in the survivorship care plans. Online social media and forum capabilities allow users to share their progress with peers and family, while getting exposed to a variety of social support mechanisms [12].
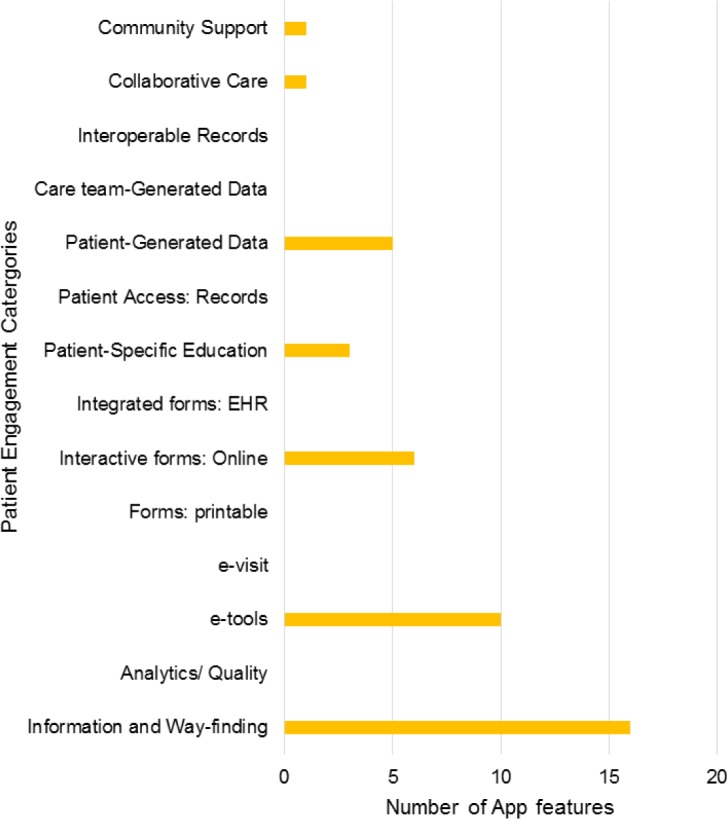
The examination of the app features using PEF (see Figure 3) indicated that the current mHealth solutions for cancer survivors had 38% of features at “inform me” level” (16 out of 42 features) and 36% at “engage me” (15 out of 42 features), 21% at “empower me” level, There are fewer features at more active phases, 2.5% at “partner with me” level and 2.5% at “support my e-community” (1 out of 42 features). As shown in Table 2, Patient Engagement Score (PES) was computed by aligning each of the features with the engagement phases described in the PEF. The scores ranged from 7 to 17, with majority of the features facilitating lower levels of engagement. Results indicate that App 5 was rated with the highest PES and seconded by App 1. Interestingly, App 5 is the only app that was rated five stars by users who downloaded the apps in both iTunes/App store and Google Play store.
Figure 3.
Apps features mapped to Patient Engagement Framework categories and phases
Table 2.
Computation of Patient Engagement Score
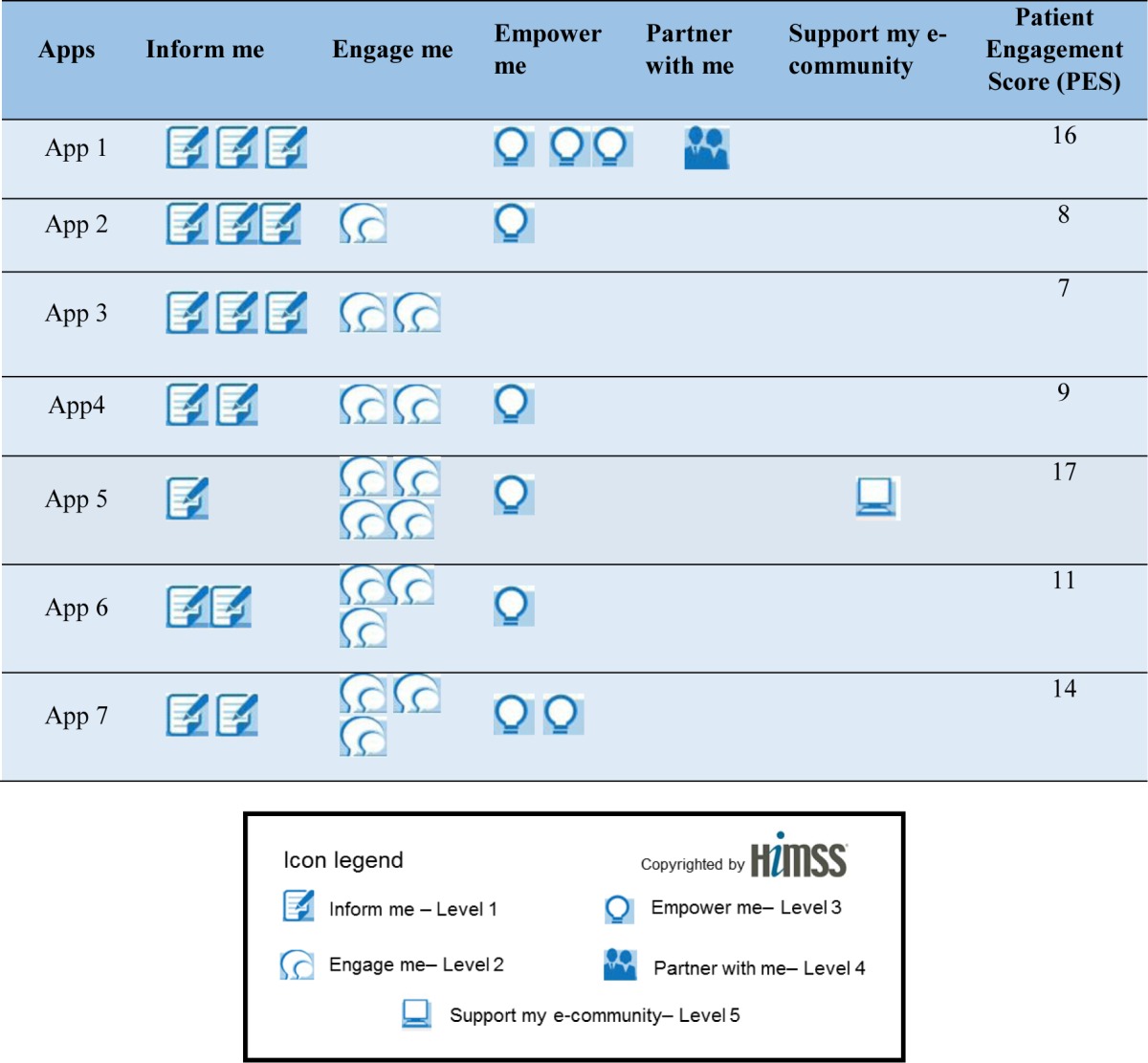
|
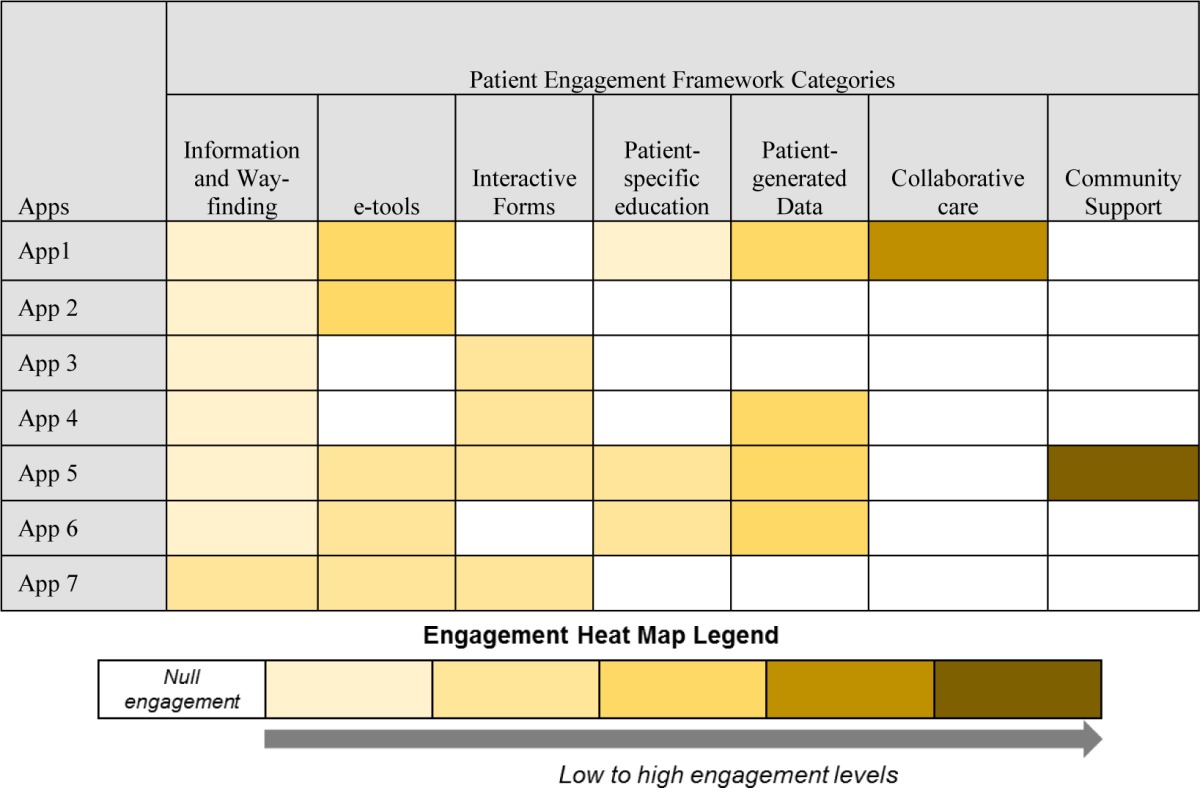
In Table 3, we attempted to depict how the apps performed in each of the PEF categories in terms of the engagement level they facilitated. The heat map highlights the sophistication in terms of the apps’ ability to engage patients with a specific information kind. For Information and Way-finding, most app features are at the “inform me” phase, while for e-tools, app features are at “engage me” and “empower me” phase. For Patient-specific education, app features reached “engage me” phase. There are features for patient-generated data at “empower me” phase, while features for collaborative care are at “partner with me” phase. None of the apps have features such as quality and safety reports on providers and healthcare organizations, or patient-specific quality indications and analytics promoting empowerment and engagement. Of the top three apps that received higher PES score, two apps were developed by a hospital entity. Given that the original objective of the PEF is to enable the health institutions engage their patients, the results are intuitive. Overall, results indicated that majority of the apps are still in initial phases of facilitating patient engagement. There is room to improve in several areas of care facilitation and patient empowerment. Two important areas include (a) harnessing social technologies to gather care information and facilitate peer-to-peer connections that offer emotional and informational support when needed, and (b) development and deployment of consumer-centered care coordination tools that facilitate efficient care transition, family involvement, and self-management of care information. Collaborative access to electronic health records, patient-centered analytics demonstrating physician feedback on patients’ self-management of care plan are other key areas that warrant specific focus to attain high levels of patient engagement.
Table 3.
Heat map indicating engagement levels for seven apps in each information engagement category
|
Supplements to the Patient Engagement Framework
Integrating behavior change theories is vital to engage users in self-management of health. For example, Engaging Consumers in Health with Health Care (ECHC) framework incorporates traditional theories of behavior change in a simplified manner by considering individuals, their social and environmental interactions [13]. However, researchers question the validity of traditional theories in digital health era [14]. Existing behavior change theories may be insufficient to inform mobile intervention development, given the novelty and distinctions in the interaction and connectivity paradigm associated with mobile platforms. It is important to understand the nature of health-related behaviors and evolution of user needs in the context of web-based and mobile platforms through development of multi-disciplinary analytics that offer both depth and scale [15–17]. Based on the lessons learned from this study, we suggest the integration of behavior change strategies [18] using technology development frameworks [19,20] that consider the role of human cognition and social-technical factors surrounding users’ health-related behaviors. Such theory-driven, ecologically-modeled mobile health technologies can form the crux of user-inclusive care management models. Subsequently, the resulting mobile ecosystem can presumably engage the “digital consumer” in self-management of health conditions (e.g. cancer survivorship). In addition, existing patient and user engagement frameworks are limited to the operationalization of engagement attributes as technology features. However, to fully analyze and realize the benefits of such technology accessories, the current realm of engagement models should be expanded to provide standardized assessment criteria that facilitate the evaluation of health outcomes. Such an integrated framework results in mHealth solutions that can potentially promote cancer survivor engagement in their own care, while providing an account of the ways in which such increased engagement may result in superior health outcomes.
Limitations and Future Work
The study described in the paper is not without limitations. The search strategy employed limited our focus to the official application stores. A more comprehensive search such as searching scientific literature or app clearinghouse websites [21] may retrieve more apps for cancer survivorship care. This study only examined the features of the cancer survivorship care apps in terms of the HIMSS Patient Engagement Framework. Given the complexity of cancer survivorship care, the framework may not be detailed enough to cover all of mobile features for survivorship care. For example, based on this definition for “Patient engagement”, that is, “patients, families… and health professionals working in active partnership at various levels across the health care system… to improve health and health care…”[22], the family-centered nature of cancer survivorship has not been captured by the framework. Furthermore, the framework used in the study is aimed at health institutions to develop solutions that are patient-engaging. However, the framework is not completely suitable to identify engagement features for technology solutions that solely involve health consumers. In this paper, we did not intend to evaluate the apps for their effectiveness and performance. The patient engagement score determined in the study does not account for the impact on patient health care outcomes. For example, a feature at Support my e-community level may not necessarily have five times the impact on health outcome than a feature at inform me patient engagement level and more features for a single PEF elements may not necessarily indicate superior engagement levels. Further work on the evaluation of the usefulness and effectiveness of the mobile apps in improving health outcomes are needed. In addition, we have limited our review to mobile platforms, and therefore our paper does not provide an exhaustive evaluation of all the survivorship application that may be available only on web platforms. This study is an attempt to use Patient Engagement framework to evaluate the cancer survivorship mobile app features to understand the ways in which technology facilitates user engagement in self-management of care. PEF is created for healthcare organizations to develop and strengthen their patient engagement strategies. However, the cancer survivorship apps evaluated in this study were developed by a variety of organizations to help survivors engage in their own care. In addition, the Patient Engagement framework provides an account of technology-related functionalities alone, however, user engagement can be facilitated in several dimensions through use of novel inter- and intra-personal interactions distributed among the user, the app, and the environment in which the user interacts with the app [23]. Therefore, sole reliance on the Patient Engagement Framework for the design of consumer-facing mobile apps may not result in the elevation of engagement levels in all these aspects. Broader evaluation frameworks that provide us deeper understanding of the utility and implementation of traditional behavior change strategies, contemporary theories of user interactions are needed for the design and evaluation of the mobile applications that potentially promote cancer survivor engagement in their own care.
Conclusions
Mobile technology holds promise in promoting communication between cancer survivors and healthcare providers, patient engagement, and care coordination [26,27]. However, there are few apps that are targeted to cancer survivors when compared to the growing market of mobile health applications. The development and adoption of mobile apps for cancer survivorship care is still in its infancy. Using Patient Engagement Framework, we have discovered that there is a lot of room for improvement in several areas, specifically, integration of data analytics and dashboard features that establish two-way communication among providers and patients, facilitation of peer-to-peer communication through online community infrastructure inbuilt within the app, and provision of mobile access to patients’ electronic health records. Majority of the already operationalized features (95%) are at beginning or intermediate levels of patient engagement (inform me, engagement me and empower me) in terms of documentation of treatment summary and implementation of cancer survivorship care plan. Most active patient engagement features such as facilitating collaborative care and online community integration need to further evolve. Furthermore, we need to develop a new health consumer engagement model that solely aids in the incorporation of user engagement attributes that capture health-related socio-behavioral constructs, and facilitate outcome-based technology modeling and evaluation. Such an integrated approach will afford a design, development, and evaluation process that results in mobile apps that are consumer-centered, user-engaging, and theoretically-aligned.
References
- 1.National Cancer Institute. Office of Cancer Survivorship Survivorship Definitions. Available from: http://cancercontrol.cancer.gov/ocs/statistics/definitions.html.
- 2.DeSantis CE, Lin CC, Mariotto AB, Siegel RL, Stein KD, Kramer JL, et al. Cancer treatment and survivorship statistics, 2014. CA: a cancer journal for clinicians. 2014;64(4):252–71. doi: 10.3322/caac.21235. [DOI] [PubMed] [Google Scholar]
- 3.Kirsch B. Many US cancer survivors still lost in transition. The Lancet. 2012;379(9829):1865–6. doi: 10.1016/s0140-6736(12)60794-6. [DOI] [PubMed] [Google Scholar]
- 4.Hewitt M GS, Stovall E, editors. From Cancer Patient to Cancer Survivor: Lost in Transition. Washington, DC: National Academies Press; 2006. [Google Scholar]
- 5.Grunfeld E, Julian JA, Pond G, Maunsell E, Coyle D, Folkes A, et al. Evaluating survivorship care plans: results of a randomized, clinical trial of patients with breast cancer. Journal of clinical oncology: official journal of the American Society of Clinical Oncology. 2011;29(36):4755–62. doi: 10.1200/JCO.2011.36.8373. [DOI] [PubMed] [Google Scholar]
- 6.Stricker CT, Jacobs LA, Risendal B, Jones A, Panzer S, Ganz PA, et al. Survivorship care planning after the institute of medicine recommendations: how are we faring? Journal of cancer survivorship : research and practice. 2011;5(4):358–70. doi: 10.1007/s11764-011-0196-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Heron KE, Smyth JM. Ecological momentary interventions: incorporating mobile technology into psychosocial and health behaviour treatments. British journal of health psychology. 2010;15(1):1–39. doi: 10.1348/135910709X466063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Klasnja P, Hartzler A, Powell C, Pratt W. Supporting cancer patients’ unanchored health information management with mobile technology; AMIA Annual Symposium proceedings / AMIA Symposium AMIA Symposium; 2011. pp. 732–41. [PMC free article] [PubMed] [Google Scholar]
- 9.Jacobs M, Clawson J, Mynatt ED, editors. My journey compass: A preliminary investigation of a mobile tool for cancer patients; Conference on Human Factors in Computing Systems - Proceedings; 2014. [Google Scholar]
- 10.National eHealth Collaborative The patient Engagement Framework. 2012. Available from: http://www.nationalehealth.org/patient-engagement-framework.
- 11.Shapiro-Mathews E, Barton AJ. Using the Patient Engagement Framework to Develop an Institutional Mobile Health Strategy. Clinical Nurse Specialist. 2013;27(5):221–3. doi: 10.1097/NUR.0b013e3182a0b9e2. [DOI] [PubMed] [Google Scholar]
- 12.Heaney CA, Israel BA. Social networks and social support. Health behavior and health education: Theory, research, and practice. 2008;4:189–210. [Google Scholar]
- 13.Mittler JN, Martsolf GR, Telenko SJ, Scanlon DP. Making sense of “consumer engagement” initiatives to improve health and health care: a conceptual framework to guide policy and practice. Milbank Quarterly. 2013;91(1):37–77. doi: 10.1111/milq.12002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Riley WT, Rivera DE, Atienza AA, Nilsen W, Allison SM, Mermelstein R. Health behavior models in the age of mobile interventions: are our theories up to the task? Behav Med Pract Policy Res. 2011;1(1):53–71. doi: 10.1007/s13142-011-0021-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cavallo DN, Chou WYS, McQueen A, Ramirez A, Riley WT. Cancer prevention and control interventions using social media: User-generated approaches. Cancer Epidemiology Biomarkers & Prevention. 2014;23(9):1953–1956. doi: 10.1158/1055-9965.EPI-14-0593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Myneni S, Cobb NK, Cohen T. Finding meaning in social media: content-based social network analysis of QuitNet to identify new opportunities for health promotion. Studies of health technology and informatics. 2013;192:807–11. [PubMed] [Google Scholar]
- 17.Myneni S, Fujimoto K, Cobb N, Cohen T. Content-Driven Analysis of an Online Community for Smoking Cessation: Integration of Qualitative Techniques, Automated Text Analysis, and Affiliation Networks. American journal of public health. 2015;105(6):1206–1212. doi: 10.2105/AJPH.2014.302464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Abraham C, Michie S. A taxonomy of behavior change techniques used in interventions. Health psychology. 2008;27(3):379. doi: 10.1037/0278-6133.27.3.379. [DOI] [PubMed] [Google Scholar]
- 19.Oinas-Kukkonen H. A foundation for the study of behavior change support systems. Personal and ubiquitous computing. 2013;17(6):1223–1235. [Google Scholar]
- 20.Mohr CD, Schueller MS, Montague E, Burns NM, Rashidi P. The Behavioral Intervention Technology Model: An Integrated Conceptual and Technological Framework for eHealth and mHealth Interventions. J Med Internet Res. 2014;16(6):e146. doi: 10.2196/jmir.3077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Boudreaux E, Waring M, Hayes R, Sadasivam R, Mullen S, Pagoto S. Evaluating and selecting mobile health apps: strategies for healthcare providers and healthcare organizations. Behav Med Pract Policy Res. 2014;4(4):363–71. doi: 10.1007/s13142-014-0293-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Carman KL, Dardess P, Maurer M, Sofaer S, Adams K, Bechtel C, et al. Patient and family engagement: a framework for understanding the elements and developing interventions and policies. Health Affairs. 2013;32(2):223–31. doi: 10.1377/hlthaff.2012.1133. [DOI] [PubMed] [Google Scholar]
- 23.O’Brien HL, Toms EG. What is user engagement? A conceptual framework for defining user engagement with technology. Journal of the American Society for Information Science and Technology. 2008;59(6):938–955. [Google Scholar]
- 24.Schubart JR, Stuckey HL, Ganeshamoorthy A, Sciamanna CN. Chronic health conditions and internet behavioral interventions: a review of factors to enhance user engagement. Computers Informatics Nursing. 2011;29(2):81–92. doi: 10.1097/NCN.0b013e3182065eed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hesse BW, Beckjord E, Rutten LJF, Fagerlin A, Cameron LD. Cancer communication and informatics research across the cancer continuum. American Psychologist. 2015;70(2):198. doi: 10.1037/a0036852. [DOI] [PubMed] [Google Scholar]
- 26.Pandey A, Hasan S, Dubey D, Sarangi S. Smartphone apps as a source of cancer information: changing trends in health information-seeking behavior. J Cancer Educ. 2013 Mar;28(1):138–42. doi: 10.1007/s13187-012-0446-9. [DOI] [PubMed] [Google Scholar]
- 27.Bender JL, Yue RYK, To MJ, Deacken L, Jadad AR. A lot of action, but not in the right direction: Systematic review and content analysis of smartphone applications for the prevention, detection, and management of cancer. J Med Internet Res. 2013;15(12) doi: 10.2196/jmir.2661. [DOI] [PMC free article] [PubMed] [Google Scholar]