Abstract
In the collaborative hospital environment, pharmacists are important members of the healthcare team, yet compared to physicians and nurses, little is known about pharmacists’ information needs or how they interact with the electronic health record (EHR). We directly observed seven clinical inpatient pharmacists as they interacted with the EHR preparing for clinical rounds using an eye-tracking camera and contextual inquiry. Pharmacists spent 50% of their time reading information from the EHR, such as notes and medication lists, and 27% of their time copying EHR data onto paper, such as patient history and laboratory results. In an environment where minutes count, the results of this study can help inform the development of CDS tools and/or EHR designs to facilitate the information needs of the pharmacists in providing care for their patients.
Introduction
Pharmacist hospital services, such as medication reconciliation and adverse drug event (ADE) monitoring, are time-intensive processes associated with improved patient care and decreased mortality, making pharmacists integral members of the healthcare team.1–5 Meaningful Use core measures, such as electronic health record (EHR) and computerized provider order entry (CPOE) adoption have impacted the ways pharmacists work and care for patients.6–9 In 2007, only 5.7% of pharmacy departments reported that their institution had a fully electronic patient record;10 this number grew to 26.5% in 2013, with 92.6% reporting having a partial or basic EHR.11 Medication and pharmacy information are critical components of the EHR, and are related to many of the safety features and benefits of EHR use.12 In addition, EHRs have become an important communication tool for interaction between pharmacists, physicians, and nurses.13 Therefore, pharmacists should be included during the development and implementation of EHRs.13, 14 Many studies have looked at information needs and seeking behavior of physicians and nurses in the EHR,15–19 but none have evaluated pharmacists. Additionally, the lack of usability or design considerations of health information technology for pharmacists can lead to human-computer interaction problems, increased workflow complexity, loss of productivity, and a decrease in the quality of patient care.15, 20
In the Veterans Health Administration (VHA), clinical pharmacists attend clinical patient rounds and participate in patient care planning, which goes beyond medication consultation in many cases. Having a pharmacist present on clinical rounds is a common practice, with over half of all hospitals, and 85% of hospitals with more than 200 beds, having pharmacists attend rounds.11 Pharmacists involvement in clinical rounds has been associated with a significant reduction in ADEs, improved patient care, and reduced costs.3, 21–23 In preparation for clinical rounds, pharmacists spend large amounts of time using the EHR to evaluate or “work up” their patients. These evaluations typically consist of identifying potential medication problems, medication regimen review, drug-drug and drug-disease interaction checking, ADE monitoring, therapeutic effectiveness evaluation, dosing appropriateness of medications based on the context of disease states and laboratory values, medication therapy management (MTM), medication reconciliation, and evaluation of patient medication adherence.24 During patient evaluations, pharmacists need to have access to real-time patient information, as other studies have shown that timely information retrieval is important in patient care.25, 26 Missing, incomplete, or inaccurate information can lead to medication errors, adverse drug events, failure to provide prophylactic treatment, and other potential patient harm, whereas too much information can cause information overload.15, 27 Additionally, distributed and disjointed data can lead to longer times for finding, filtering, and organizing information along with a higher risk of missing important information and cause an increased burden on available resources.16
Due to the abundant and distributed nature of patient data in the EHR, the difficulty of obtaining some data, and time constraints facing pharmacists, an understanding of what information pharmacists need and how they go about finding that information is important. Such an understanding could lead to improved EHR designs or clinical decision support (CDS) tools targeted to pharmacists. Therefore, the purpose of this study is to explore pharmacists’ use of the EHR and information needs in real clinical practice settings using direct observation.
Methods
Study setting and participants
This study was carried out at the George E. Wahlen Department of Veterans Affairs Medical Center in Salt Lake City, Utah. The VHA has a long-established EHR as well as advanced clinical practice for pharmacists, such as independent prescribing privileges within their scope of practice since 1995.28 The VHA uses the Veterans Health Information Systems and Technology Architecture (VistA) as its EHR, with the Computerized Patient Record System (CPRS) as the clinician interface. A more detailed description of CPRS is available elsewhere.29 In 2009, the VHA accounted for half of all US hospitals with a comprehensive EHR,30 and has been associated with improvements in quality of care.31, 32 Study participants were clinical inpatient pharmacists. We recruited a convenience sample of seven pharmacists from a wide range of inpatient sites such as post-op care, acute medicine, telemetry, rehabilitation, and an intensive care unit. Pharmacists had on average 6.4 years experience with CPRS (range: 1–18, median: 6). Pharmacists were recruited through presentations at staff meetings, demonstrations of the study methods, and referrals from other study participants. We were not able to capture all of the rounds preparation time, but we collected data of the pharmacists evaluating 13 new and 19 familiar patients. We did not collect patient data. This study was approved by the University of Utah Institutional Review Board and VA Research Service.
Procedures
Prior to the observation sessions, pharmacists were given minimal explanation of the study and asked to prepare for clinical rounds as they normally would. Sessions were carried out in the pharmacists’ usual environment and time of preparation for rounds, but were limited to approximately the first 45 minutes. We used mixed-methods approach with direct observation in the clinical setting, eye-tracking capture, and contextual inquiry. Direct observation was used because it is difficult to get unbiased responses from providers by directly asking them what their information needs are, or conducting surveys.33 We encouraged participants to describe their goals or the information they are looking for. However, we did not depend on think-aloud techniques for data collection because in the clinical setting, experts tend to function with system 1 level thought,34 most people stop talking when they are thinking or processing complex information, and it is difficult for experts to verbalize their goals and tasks.35 During the session, a researcher would ask clarifying questions to better understand goals, mental models, responsibilities, perceived usefulness of different sources of information, and task. The researcher would wait to ask questions until the pharmacist completed a task, as to not disrupt the cognitive process of complex tasks. In order to capture the rapid, dense, and variable study data, and information sources outside of the EHR, we used an eye-tracking camera from Pupil-Labs to capture video and an iPad to capture audio and additional artifacts.36 Pupil-Labs is a mobile eye-tracking device with affordable hardware and open source software written in python. The hardware consists of a 3D printed headset that the user wears like a pair of glasses, and has a camera to record the field of view and a camera to record eye movements. The Pupil-Labs camera even allows the researcher to see the pharmacists’ gaze positions in real time. The software was run on MacOS, but can be installed on Linux or Windows computers. In addition to the audio and video recording, the researcher would also document field notes during the session and ask deepening questions about information needs and goals after the session. Audio and video from the session were merged and loaded into Atlas.ti 7 (Scientific Software Development GmbH, 2015) for coding and analysis.
Analysis
The analysis of the data was mainly qualitative and descriptive using Atlas.ti for coding and times, and interquartile ranges (IQR) for descriptive statists. Because of the qualitative and descriptive nature of the study, we estimated that the sample size of seven pharmacists would be sufficient to describe a range of information needs across the inpatient setting.37 After the observation sessions, the researcher would then code the video using high-level codes to describe what the pharmacist was doing, where they were looking, and what they were writing down. The codes were reviewed and verified by a second researcher. During piloting, we found that the pupil tracker did not provide the precise location of the pharmacist’s gaze, but was able to provide a general area of where the pharmacist was looking, which helped in review of the verbal and observational data. This was because the camera calibration suffered when it was taken on and off to visit with patients, and the distance between the tracker and the information source (i.e. computer monitor) changed when the pharmacist moved. Therefore, we did not pursue direct analysis of the eye-tracking data, but rather used gaze data in the context of the rich descriptions in the audio and field notes.
Results
The average time of recorded observation per session was 39 minutes. The average time it took each pharmacist to evaluate a new patient was 11:31 (mm:ss) (median: 10:42, IQR: 9:51 to 14:46). Patients familiar to the pharmacist had an average time of 3:47 (median: 1:46, IQR: 0:56 to 4:51) for review and evaluation in the EHR.
Reading and writing
In preparing for rounds, pharmacists spent 50% of their time reading information in the EHR and 27% writing information onto paper, with the rest of their time performing other tasks such as communicating with the team or managing patient lists or notifications. The most predominant information use pattern was the back and forth of reading and writing. Of note, pharmacists switched between reading and writing an average of 4.35 times per minute. In terms of reading, pharmacists spend the most time reading notes in the EHR (such as admission notes, history and physical notes, etc.), followed by medication lists, printed papers (typically print outs of active inpatient and outpatient medication lists), laboratory results (such as reviewing recent results), provider orders (especially over the last 24 hours), and others. However, twice as much time was spent reading EHR notes compared to medication lists. Within the notes, the most time was spent reading the assessment/plan and patient history sections, respectively. In the medication lists, pharmacists spent the most time checking bar code medication administration (BCMA) data for medications administered. Table 1 shows a list of reading locations and length of time.
Table 1.
Reading locations
| Reading source | Total time | Time/pharmacist median (IQR) |
|---|---|---|
| Notes | 43:20 | 4:34 (4:23–7:55) |
| Medication lists | 20:32 | 2:56 (2:05–3:15) |
| Paper printouts | 16:14 | 2:48 (2:48–3:04) |
| Laboratory results | 12:49 | 1:55 (1:24–2:11) |
| Orders | 10:28 | 2:28 (0:23–3:04) |
| Vital signs | 01:02 | 0:10 (0:06–0:20) |
| Microbiology | 00:57 | 0:14 (0:03–0:25) |
| Other sources | 05:34 |
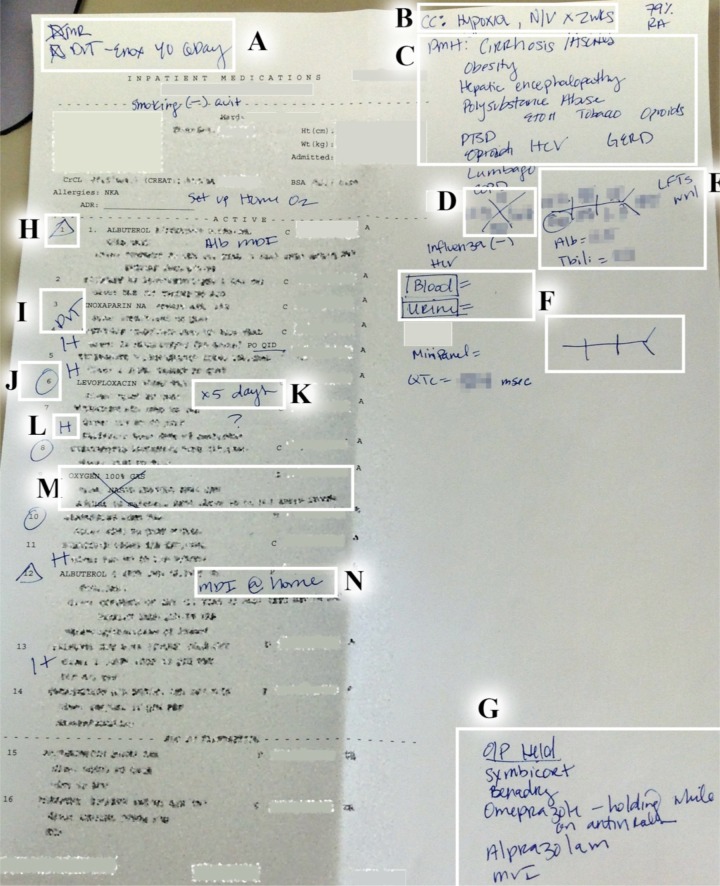
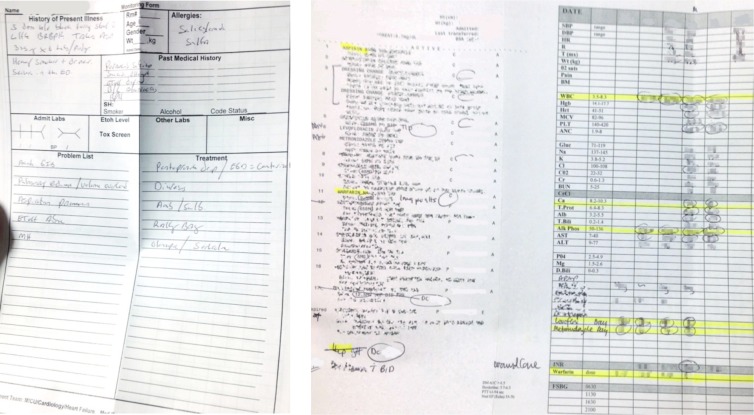
As for writing, significant paper records were kept, including active inpatient medication lists, outpatient medication lists, and medication reconciliation notes. Most information was written down on the active inpatient medication list printed from VistA, not CPRS, and was the main document used on rounds, as shown in Figure 1. Pharmacists spent the most time writing the patient’s past medical history (such as problem lists), laboratory results, reminders (such as recommendations or questions for the medical team), medication doses administered (such as frequency of PRN doses, insulin requirements, and IV infusion rates), medication lists (such as outpatient medications not restarted upon admission), and other medication or historical notes (such as highlighting changes in therapy or identifying preventative treatments). Table 2 shows a list of topics written down and times spent writing.
Figure 1.
Integrating EHR information by writing notes on an active inpatient medication list printed from VistA. A, check list for admission medication reconciliation note and deep vein thrombosis (DVT) prophylaxis. B, reason for admission. C, past medical history or problem list. D, complete blood cell count (CBC) shorthand. E, complete metabolic panel (CMP) shorthand. F, place holders (memory aids) for laboratory results that are pending. G, outpatient medications that have not been restarted. H, triangles in the medication list signal to continued outpatient medications, but with changes compared to outpatient use. I, highlighting DVT prophylaxis. J, circles in the medication list signal to new medications since admission. K, planned duration of antibiotic therapy (some pharmacist would also record which day of regimen). L, "H" in the medication list signals to outpatient medications that were continued on admission. M, items on the list that the pharmacist is not following or going to use on the discharge medication reconciliation note. N, a note that signals to changes in therapy as compared to outpatient.
Table 2.
Writing themes
| Topics written on paper | Total time | Time/pharmacist median (IQR) |
|---|---|---|
| Medical history/problem lists | 13:00 | 2:00 (1:38–2:38) |
| Laboratory results | 09:49 | 1:03 (0:18–2:26) |
| Reminders | 08:22 | 1:11 (1:01–1:49) |
| Medication doses given | 06:07 | 1:07 (0:53–1:12) |
| Medication lists | 04:39 | 0:45 (0:23–1:22) |
| Medication notes | 02:38 | 0:40 (0:36–0:43) |
| Historical notes | 01:24 | 0:42 (0:22–1:02) |
| Other topics | 14:14 |
Searching for information
Search and review strategies varied most in terms of whether the patient was new or familiar. New patients were typically evaluated before familiar patients. When evaluating a new patient, pharmacists typically started in the notes section of the EHR, followed by going to the medication or laboratory results section, followed by the coversheet, orders, or printed medication lists. When evaluating a familiar patient, pharmacists typically started in the orders section to look for updates in treatment, followed by laboratory results or notes section. The average location sequence length was 10 sections of the EHR for new patients, and 5 sections for familiar patients. Additionally, we observed that pharmacists used many different programs in addition to CPRS, such as BCMA, Essentris, VistA, VistA Imaging, and used different non-EHR sources, such as other papers, clinicians, whiteboards, etc. Some information was easier to find than others, for example, in order to find the patient’s QTC interval (or even if they had an ECG done) pharmacists had to log into VistA Imaging, which took 51 seconds just to log in.
Information Tasks
There were many tasks that the pharmacists performed when preparing for rounds. Some of the most common were comparing medication lists for medication reconciliation, correlating indications/treatments and treatments/indications, managing/optimizing drug therapy (such as insulin or warfarin management), verifying medication administration, monitoring for ADEs, and documenting notes in the EHR (such as medication reconciliation notes). Generally, there was a considerable amount of task switching and multitasking, such as checking for drug-drug interactions, drug doses, medication indications, changes in therapy, etc. when reading the medication list. In this paper, we present managing insulin doses and verifying medication administration as examples of tasks the pharmacists performed in the EHR.
Example 1. Managing insulin doses
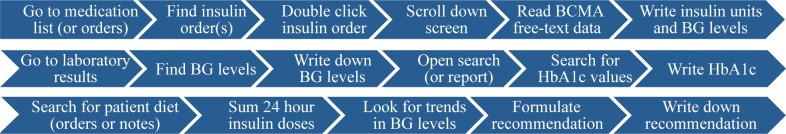
The pharmacists at this institution managed insulin doses, which required an average of 80 seconds to gather needed information to support this task, even though the patients in this study had relatively low insulin requirements. Figure 2 shows a schematic of this task, which required the pharmacist to go to the medication section (or orders section), find one of the insulin orders (such as rapid acting insulin), double click the order, scroll down to the bottom of the popup window to the BCMA data section, and then write down the ancillary blood glucose levels entered as free-text by the nursing staff and write down the insulin doses administered (also free-text entries), as shown in Figure 3. Then they would search for additional insulin orders, such as long-acting or basal insulin, and repeat the above process. The pharmacist would then go to the laboratory results section and write down additional blood glucose levels (which were sometimes different from the results reported in BCMA), and open a laboratory search (or a report) to find the most recent HbA1c lab result, and search for the patient’s diet (in the orders or the notes). The pharmacist would then sum the insulin requirements for the last 24 hours, look for trends in the blood glucose values, and provide a recommendation to the team, take no action, or modify the insulin order. To complicate the process, we found that there were multiple insulin orders (such as sliding scale, scheduled, baseline, IV drip, etc.) sometimes using different types of insulin (such as insulin aspart, regular insulin, NPH, or insulin glargine) and that not all blood glucose values were documented in the EHR.
Figure 2.
Example 1. Insulin management process. BG = blood glucose
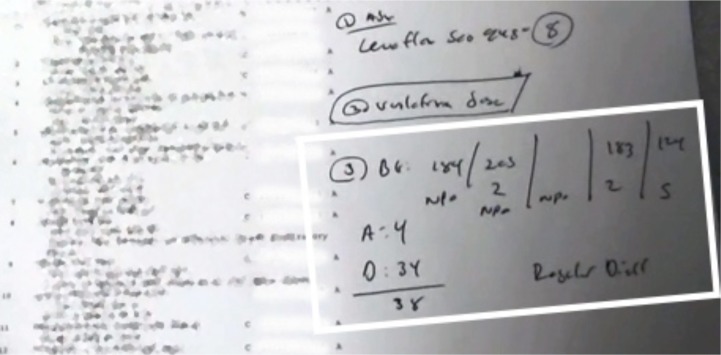
Figure 3.
Example 1. Calculating insulin requirements for blood glucose control and insulin dosing adjustment. Highlighted are blood glucose levels, insulin doses administered, and diet intake
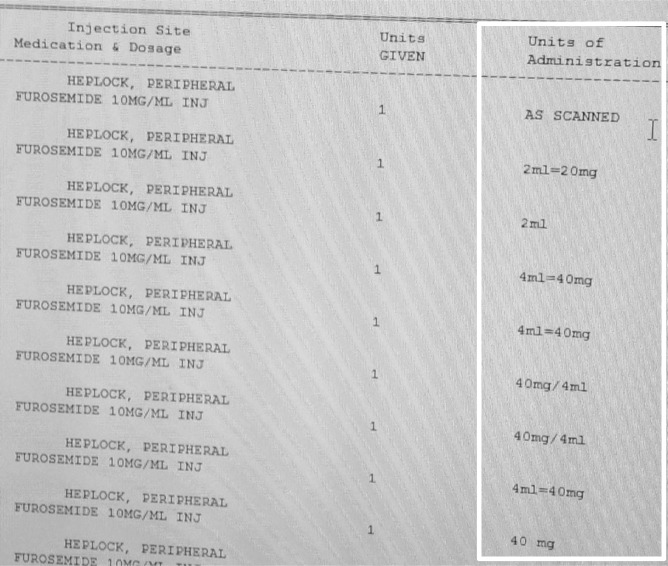
Example 2. Verifying medication administration
To verify medication administration, the pharmacists typically had to find the medication order, double click on the order, scroll down to BCMA data and write down times and doses administered. They would check if ‘as needed’ medications were administered in order to assess pain control or the patient’s ability to sleep, check administration times to correlate with drug levels, follow up on medication orders (such as making sure the patient received their warfarin dose), checking when antibiotics were started in order to calculate the treatment duration, and going to the patient’s bedside to check IV infusion rates. However, there were some limitations identified. For example, medications administered in the Emergency Department (ED) were not documented in BCMA, so the pharmacists would have to read the ED notes to find doses and administration times. Additionally, BCMA would only pull in the drug concentration and nursing would have to input the dose administered as free text. This was a challenge for one pharmacist when they were trying to find when, or if, the active 80 mg furosemide dose was given to the patient, as shown in Figure 4.
Figure 4.
BMCA drug administration data. BCMA data displays drug concentration, but nursing would have to input the dose administered as free text. The pharmacist was searching for 80 mg dose of furosemide.
Discussion
In this study we observed pharmacists as they interacted with the EHR preparing for clinical rounds. We found that pharmacists spent a considerable amount of time searching for and reading information from the EHR and integrating EHR data by writing it down information on printed medication lists, suggesting that the way information is stored or displayed in the EHR does not meet the cognitive model or needs of pharmacists.
We observed that not all information in the EHR was useful for pharmacists, or easy to obtain, even when it had been recorded to answer anticipated information needs. For example, CPRS calculates and displays the patient’s estimated kidney function using the MDRD creatinine clearance equation. One pharmacist noted that "the MDRD equation is not helpful for me because medication dosing recommendations use the Cockcroft-Gault equation", so he would use an Internet calculator to calculate creatinine clearance using the Cockcroft-Gault equation, which took about 53 seconds. The pharmacists also commented on the not being able to run drug-drug interaction checks on demand when evaluating patient lists. Additionally, the pharmacists typically did not trust the vital signs, fluid balance, or IV infusion rates reported in the EHR, as they were documented infrequently or missing in the EHR.
Other studies of physicians’ use of the EHR show that they tend to focus more on the “Assessment and plan” part of clinical notes, and give very little attention to the “Medication profile” part.18, 38 Ancker et al. also studied physician use of the EHR and found significant physician level variation in utilization of EHR features.19 Using EHR log data, they found that problem lists were updated in only about 20–25% of encounters, almost always by adding problems instead of removing them. Additionally, problem lists and medication lists were marked as reviewed less than 10% of the time. Given the pharmacists’ training and role, it is understandable why pharmacists focus more on medications and medication lists in the EHR. Additionally, pharmacists’ focus on medication lists and problem lists to perform daily medication reconciliation and search for drug related problems, such as underdosing or overdosing of medications, ADEs, drug-drug and/or drug-allergy interactions, medication use without an indication, improper medication selection, and untreated medical problems.39 Similar to physicians, we observed that pharmacists obtained information from a variety of different non-EHR sources,16 and they typically had multiple systems open at the same time in addition to CPRS. However, having multiple programs open at the same time was problematic as pharmacists tend to jump from one patient to another, and there were instances where the other programs did not update and change patients to be in sync with CPRS, which could have lead to errors.
It was interesting to observe the extensive use of paper and that pharmacists spent about 1/3 of their time transcribing information from the EHR onto paper, especially in an environment that has had a comprehensive EHR in place for over a decade. The persistence of paper is not a new concept, and in 2009, Saleem et al. proposed several reasons for the persistence of paper in the VHA environment,40, 41 and other benchmark institutions with EHRs.42 Similar to their study, it seemed that pharmacists mainly used paper because of its ease of use and it helped with efficiency, memory, awareness, task specificity, task complexity, and data organization. For example, most of the pharmacists only had one computer monitor and having information written down on paper helped reduce the need to jump back and forth between tabs in the EHR. The use of paper helped memory by writing things down such as patient history, recommendations, check boxes, medication lists, and placeholders for pending laboratory results. Additionally, paper helped with identifying changes or new information, and allowed for highlighting and quick annotation. Russ et al. suggested that healthcare workers need information to be customizable, prioritized, trendable, locatable, and accessible,43 requirements that the pharmacists in our study used paper to satisfy.
One study assessed providing pharmacists with tablet computers during rounds, and found many advantages such as the ability to enter/modify/or delete medication orders in real-time, perform complicated calculations, review up-to-date and comprehensive patient data, and access information databases, patient education materials, guidelines, and institutional protocols.44 However, there were challenges with limited battery life, having to carry around a heavy device, and the limitations of the rigid EHR design, such as searching for information. Even though paper is static, it is cheap, light, flexible, easily carried on team rounds, and not limited by power supply or battery life. The use of paper has important and powerful advantages that cannot be replicated in the EHR and it can help to fill gaps in the EHR design or information;40, 42, 45, 46 therefore, perhaps we need to better support paper processes using the EHR, such as designing better paper using reports, or bringing related, yet disparate, information in the EHR together to reduce searching/reading time, or tools for associating medications, problem lists, and/or laboratory values. Pharmacists in this study constructed their own custom paper worksheet to help serve as memory aids and facilitate the evaluation process, as shown in Figure 4. In the clinical environment, every minute counts,47 and tools that can reduce time or increase efficiency are important. The findings in the study, and others, suggest that EHRs provide little cognitive support for clinicians or their workflows.33, 48
One limitation of the use of paper by the pharmacists was the creation of handwritten notes and memory aids were more up-to-date than the information in the EHR, and were not available to be handed-off to other pharmacists.49 When one of the pharmacists was asked about patient handoffs, she said that the other pharmacist will usually call and give a verbal handoff if it is a complex patient, but it is 50:50 if they get a handoff or not, thereby losing the valuable information that the pharmacist spent so much time compiling. Technologies could be developed, such as EHRs or EHR apps, that are easily developed and customized, allowing clinicians to create dashboards or reports that are relevant to their setting or role, thereby becoming part of the information system instead of persisting alongside it.50 Some have reasonably suggested that it is not possible to meet the information needs of all users, as different users have different workflows;7, 51 however, making the EHR customizable for different use cases, such as through apps or CDS tools that access core services and data in the EHR, could make it possible to meet the information and workflow needs of a spectrum of various users.52, 53
Lastly, Millonig et al. suggested that pharmacists need to have access to patient-specific health information to improve patient outcomes, including a medication profile with refill history, vital signs and laboratory test results, diagnoses and current conditions, and medical history and physical assessment data.39 While our project focused on the inpatient setting, the availability of patient-specific information to help satisfy pharmacist information needs in the ambulatory and community settings could help improve patient outcomes, especially since pharmacists are more likely to detect and prevent errors by having more access to patient information that provides the overall context of the patient.54, 55 Pharmacists, and other clinicians, should have access to the entire patient record, regardless of where care was received, such as potential outpatient medication lists and problem lists.8 As pharmacists’ scope of practice continues to expand, especially in other institutions, so too does their need for adequate patient information as meaningful users and contributors to the EHR.24, 56–58
Limitations
There are some limitations to this study that should be mentioned. Frist, we had a small sample size from only one institution, and we were not able to explore site-specific cultural needs or additional individual user preferences. Additionally, the generalizability of our results to non-VHA institutions is limited due to the unique characteristics of CPRS and the exemplary example of progressive clinical pharmacy practice in the VHA. The practice of pharmacy, roles of pharmacists, and EHR data collected or reported may be different at other institutions. However, anecdotal experience at local surrounding non-VHA hospitals suggests similar information needs and use of paper. Additionally, we were not able to have independent coding by the second researcher. The first researcher had significantly more knowledge and context of the sessions because he was a pharmacist and he was the one present for the observations; however, both coders had to agree on consensus for the coding procedures. While this project focused on the actual user workflow, future research could compare these results with the pharmacists’ perception of an ideal workflow in their clinical area of focus.
Conclusion
Pharmacists spend a significant amount of time searching for patient information in the EHR, and writing it down onto paper. This study suggests that current EHR designs do not readily support the information needs or workflow requirements of pharmacists. In an environment where every minute counts, the results of this study can help inform the development of CDS tools and/or EHR designs to facilitate the information needs of the pharmacists in providing care for their patients.
Figure 4.
Examples of custom paper worksheets
Acknowledgments
During this study, Dr. Nelson was supported by the VA Advanced Fellowship Program in Medical Informatics of the Office of Academic Affiliations, Department of Veterans Affairs.
Footnotes
Disclaimer
The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
References
- 1.Bond CA, Raehl CL. Clinical pharmacy services, pharmacy staffing, and hospital mortality rates. Pharmacotherapy. 2007;27(4):481–93. doi: 10.1592/phco.27.4.481. [DOI] [PubMed] [Google Scholar]
- 2.Viktil KK, Blix HS. The impact of clinical pharmacists on drug-related problems and clinical outcomes. Basic Clin Pharmacol Toxicol. 2008;102(3):275–80. doi: 10.1111/j.1742-7843.2007.00206.x. [DOI] [PubMed] [Google Scholar]
- 3.Kaboli PJ, Hoth AB, McClimon BJ, Schnipper JL. Clinical pharmacists and inpatient medical care: a systematic review. Arch Intern Med. 2006;166(9):955–64. doi: 10.1001/archinte.166.9.955. [DOI] [PubMed] [Google Scholar]
- 4.Dasta JF, Jacob J. The critical care pharmacist: what you get is more than what you see. Crit Care Med. 1994;22(6):906–9. [PubMed] [Google Scholar]
- 5.Montazeri M, Cook DJ. Impact of a clinical pharmacist in a multidisciplinary intensive care unit. Crit Care Med. 1994;22(6):1044–8. doi: 10.1097/00003246-199406000-00027. [DOI] [PubMed] [Google Scholar]
- 6.Meaningful Use, Baltimore MD. Centers for Medicare & Medicaid Services; 2014. [cited 2014]. Available from: http://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Meaningful_Use.html. [Google Scholar]
- 7.Brown MA, Bloodworth L, Ross LA. Health information technology use in a rural clinic: the pharmacist’s perspective. J Health Care Poor Underserved. 2013;24(1 Suppl):15–9. doi: 10.1353/hpu.2013.0045. [DOI] [PubMed] [Google Scholar]
- 8.Fox BI. Health information technology: are we aware and engaged? Am J Pharm Educ. 2013;77(6):113. doi: 10.5688/ajpe776113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McMullen CK, Macey TA, Pope J, Gugerty B, Slot M, Lundeen P, et al. Effect of computerized prescriber order entry on pharmacy: Experience of one health system. Am J Health Syst Pharm. 2015;72(2):133–42. doi: 10.2146/ajhp140106. [DOI] [PubMed] [Google Scholar]
- 10.Pedersen CA, Gumpper KF. ASHP national survey on informatics: assessment of the adoption and use of pharmacy informatics in U.S. hospitals–2007. Am J Health Syst Pharm. 2008;65(23):2244–64. doi: 10.2146/ajhp080488. [DOI] [PubMed] [Google Scholar]
- 11.Pedersen CA, Schneider PJ, Scheckelhoff DJ. ASHP national survey of pharmacy practice in hospital settings: Prescribing and transcribing—2013. Am J Health Syst Pharm. 2014;71(11):924–42. doi: 10.2146/ajhp140032. [DOI] [PubMed] [Google Scholar]
- 12.Zlabek JA, Wickus JW, Mathiason MA. Early cost and safety benefits of an inpatient electronic health record. J Am Med Inform Assoc. 2011;18(2):169–72. doi: 10.1136/jamia.2010.007229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hagland M. Is there a pharmacist house? When it comes to clinical IT implementations, healthcare IT leaders are turning to the 'third discipline' for leadership and involvement in clinical informatics. Healthc Inform. 2010;27(12):18, 20–2. passim. [PubMed] [Google Scholar]
- 14.Troiano D, Jones MA, Smith AH, Chan RC, Laegeler AP, Le T, et al. The need for collaborative engagement in creating clinical decision-support alerts. Am J Health Syst Pharm. 2013;70(2):150–3. doi: 10.2146/ajhp120435. [DOI] [PubMed] [Google Scholar]
- 15.Clarke MA, Belden JL, Koopman RJ, Steege LM, Moore JL, Canfield SM, et al. Information needs and information-seeking behaviour analysis of primary care physicians and nurses: a literature review. Health Info Libr J. 2013;30(3):178–90. doi: 10.1111/hir.12036. [DOI] [PubMed] [Google Scholar]
- 16.Kannampallil TG, Franklin A, Mishra R, Almoosa KF, Cohen T, Patel VL. Understanding the nature of information seeking behavior in critical care: implications for the design of health information technology. Artif Intell Med. 2013;57(1):21–9. doi: 10.1016/j.artmed.2012.10.002. [DOI] [PubMed] [Google Scholar]
- 17.Xu X, Rocha RA, Bigelow SM, Wallace CJ, Hanna T, Roemer LK. Understanding nurses’ information needs and searching behaviour in acute care settings. AMIA Annu Symp Proc. 2005:839–43. [PMC free article] [PubMed] [Google Scholar]
- 18.Brown PJ, Marquard JL, Amster B, Romoser M, Friderici J, Goff S, et al. What Do Physicians Read (and Ignore) in Electronic Progress Notes? Applied Clinical Informatics. 2014;5(2):430–44. doi: 10.4338/ACI-2014-01-RA-0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ancker JS, Kern LM, Edwards A, Nosal S, Stein DM, Hauser D, et al. How is the electronic health record being used? Use of EHR data to assess physician-level variability in technology use. J Am Med Inform Assoc. 2014;21(6):1001–8. doi: 10.1136/amiajnl-2013-002627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Smelcer JB, Miller-Jacobs H, Kantrovich L. Usability of Electronic Medical Records. Journal of Usability Studies. 2009;4(2):70–84. [Google Scholar]
- 21.Kucukarslan SN, Peters M, Mlynarek M, Nafziger DA. Pharmacists on rounding teams reduce preventable adverse drug events in hospital general medicine units. Archives of internal medicine. 2003;163(17):2014–8. doi: 10.1001/archinte.163.17.2014. [DOI] [PubMed] [Google Scholar]
- 22.Cupit GC. The role of the clinical pharmacist in the institutional setting. J Clin Pharmacol. 1981;21(5–6):251–2. doi: 10.1002/j.1552-4604.1981.tb02556.x. [DOI] [PubMed] [Google Scholar]
- 23.Yee DK, Veal JH, Trinh B, Bauer S, Freeman CH. Involvement of HMO-based pharmacists in clinical rounds at contract hospitals. Am J Health Syst Pharm. 1997;54(6):670–3. doi: 10.1093/ajhp/54.6.670. [DOI] [PubMed] [Google Scholar]
- 24.The Roadmap for Pharmacy Health Information Technology Integration in U.S. Health Care . Alexandria, VA: Pharmacy e-Health Information Technology Collaborative; 2011. Available from: http://www.accp.com/docs/positions/misc/HITRoadMap2011.pdf. [Google Scholar]
- 25.Bates DW, Cohen M, Leape LL, Overhage JM, Shabot MM, Sheridan T. Reducing the frequency of errors in medicine using information technology. J Am Med Inform Assoc. 2001;8(4):299–308. doi: 10.1136/jamia.2001.0080299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Friedman C, Gatti G, Elstein A, Franz T, Murphy G, Wolf F. Are clinicians correct when they believe they are correct? Implications for medical decision support. Stud Health Technol Inform. 2001;84(Pt 1):454–8. [PubMed] [Google Scholar]
- 27.Zeng Q, Cimino JJ, Zou KH. Providing concept-oriented views for clinical data using a knowledge-based system: an evaluation. J Am Med Inform Assoc. 2002;9(3):294–305. doi: 10.1197/jamia.M1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Clause S, Fudin J, Mergner A, Lutz JL, Kavanaugh MM, Fessler K, et al. Prescribing privileges among pharmacists in Veterans affairs medical centers. Am J Health Syst Pharm. 2001;58(12):1143–5. doi: 10.1093/ajhp/58.12.1143. [DOI] [PubMed] [Google Scholar]
- 29.Brown SH, Lincoln MJ, Groen PJ, Kolodner RM. VistA–U.S. Department of Veterans Affairs national-scale HIS. Int J Med Inform. 2003;69(2–3):135–56. doi: 10.1016/s1386-5056(02)00131-4. [DOI] [PubMed] [Google Scholar]
- 30.Jha AK, DesRoches CM, Campbell EG, Donelan K, Rao SR, Ferris TG, et al. Use of electronic health records in U.S. hospitals. N Engl J Med. 2009;360(16):1628–38. doi: 10.1056/NEJMsa0900592. [DOI] [PubMed] [Google Scholar]
- 31.Jha AK, Perlin JB, Kizer KW, Dudley RA. Effect of the transformation of the Veterans Affairs Health Care System on the quality of care. N Engl J Med. 2003;348(22):2218–27. doi: 10.1056/NEJMsa021899. [DOI] [PubMed] [Google Scholar]
- 32.Perlin JB. Transformation of the US Veterans Health Administration. Health Econ Policy Law. 2006;1:99–105. doi: 10.1017/S1744133105001222. [DOI] [PubMed] [Google Scholar]
- 33.Weir C, Drews FA, Leecaster MK, Barrus RJ, Hellewell JL, Nebeker JR. The orderly and effective visit: impact of the electronic health record on modes of cognitive control. AMIA Annu Symp Proc. 2012;2012:979–87. [PMC free article] [PubMed] [Google Scholar]
- 34.Kahneman D. Thinking Fast and Slow. New York: Ferrar, Straus and Giroux; 2011. [Google Scholar]
- 35.Cooke L, Cuddihy E, editors. Using eye tracking to address limitations in think-aloud protocol; Professional Communication Conference, 2005 IPCC 2005 Proceedings International; IEEE; 2005. [Google Scholar]
- 36.Kassner MP, Patera WR. PUPIL: constructing the space of visual attention. Massachusetts Institute of Technology; 2012. [Google Scholar]
- 37.Patton M. Qualitative Research and Evaluation Methods. Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- 38.Zheng K, Padman R, Johnson MP, Diamond HS. An interface-driven analysis of user interactions with an electronic health records system. J Am Med Inform Assoc. 2009;16(2):228–37. doi: 10.1197/jamia.M2852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Millonig MK, Jackson TL, Ellis WM. Improving medication use through pharmacists’ access to patient-specific health care information. J Am Pharm Assoc (Wash) 2002;42(4):638–45. doi: 10.1331/108658002763029616. [DOI] [PubMed] [Google Scholar]
- 40.Saleem JJ, Russ AL, Justice CF, Hagg H, Ebright PR, Woodbridge PA, et al. Exploring the persistence of paper with the electronic health record. Int J Med Inform. 2009;78(9):618–28. doi: 10.1016/j.ijmedinf.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 41.Saleem JJ, Russ AL, Justice CF, Hagg H, Woodbridge PA, Doebbeling BN, editors. Paper Use with the Electronic Medical Record: An Important Supplement or Negative Circumvention?; Proceedings of the Human Factors and Ergonomics Society Annual Meeting; SAGE Publications; 2008. [Google Scholar]
- 42.Flanagan ME, Saleem JJ, Millitello LG, Russ AL, Doebbeling BN. Paper- and computer-based workarounds to electronic health record use at three benchmark institutions. J Am Med Inform Assoc. 2013;20(e1):e59–66. doi: 10.1136/amiajnl-2012-000982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Russ AL, Saleem JJ, Justice CF, Hagg H, Woodbridge PA, Doebbeling BN, editors. Healthcare Workers’ Perceptions of Information in the Electronic Health Record; Proceedings of the Human Factors and Ergonomics Society Annual Meeting; SAGE Publications; 2009. [Google Scholar]
- 44.Cockerham M. Use of a tablet personal computer to enhance patient care on multidisciplinary rounds. American journal of health-system pharmacy. AJHP: official journal of the American Society of Health-System Pharmacists. 2009;66(21):1909–11. doi: 10.2146/ajhp080593. [DOI] [PubMed] [Google Scholar]
- 45.Dykstra RH, Ash JS, Campbell E, Sittig DF, Guappone K, Carpenter J, et al. Persistent paper: the myth of "going paperless". AMIA Annu Symp Proc. 2009;2009:158–62. [PMC free article] [PubMed] [Google Scholar]
- 46.Waterson P, Glenn Y, Eason K. Preparing the ground for the 'paperless hospital': a case study of medical records management in a UK outpatient services department. Int J Med Inform. 2012;81(2):114–29. doi: 10.1016/j.ijmedinf.2011.10.011. [DOI] [PubMed] [Google Scholar]
- 47.Bates DW, Kuperman GJ, Wang S, Gandhi T, Kittler A, Volk L, et al. Ten commandments for effective clinical decision support: making the practice of evidence-based medicine a reality. J Am Med Inform Assoc. 2003;10(6):523–30. doi: 10.1197/jamia.M1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Stead WW, Lin HS. Computational Technology for Effective Health Care: Immediate Steps and Strategic Directions. Washington (DC): 2009. [PubMed] [Google Scholar]
- 49.Wears RL. The chart is dead–long live the chart. Ann Emerg Med. 2008;52(4):390–1. doi: 10.1016/j.annemergmed.2008.04.005. [DOI] [PubMed] [Google Scholar]
- 50.Morrison C, Fitzpatrick G, Blackwell A. Multi-disciplinary collaboration during ward rounds: embodied aspects of electronic medical record usage. Int J Med Inform. 2011;80(8):e96–111. doi: 10.1016/j.ijmedinf.2011.01.007. [DOI] [PubMed] [Google Scholar]
- 51.Baysari MT, Lehnbom EC, Richardson K, O'Reilly B, Heywood M, Melocco T. Electronic Medication Information Sources: Understanding the Needs and Preferences of Health Professionals. Journal of Pharmacy Practice & Research. 2013;43(4) [Google Scholar]
- 52.Mandl KD, Mandel JC, Murphy SN, Bernstam EV, Ramoni RL, Kreda DA, et al. The SMART Platform: early experience enabling substitutable applications for electronic health records. J Am Med Inform Assoc. 2012;19(4):597–603. doi: 10.1136/amiajnl-2011-000622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bosl W, Mandel J, Jonikas M, Ramoni RB, Kohane IS, Mandl KD. Scalable decision support at the point of care: a substitutable electronic health record app for monitoring medication adherence. Interact J Med Res. 2013;2(2):e13. doi: 10.2196/ijmr.2480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Rupp MT, DeYoung M, Schondelmeyer SW. Prescribing problems and pharmacist interventions in community practice. Med Care. 1992;30(10):926–40. doi: 10.1097/00005650-199210000-00005. [DOI] [PubMed] [Google Scholar]
- 55.Rupp MT. Value of community pharmacists’ interventions to correct prescribing errors. Ann Pharmacother. 1992;26(12):1580–4. doi: 10.1177/106002809202601218. [DOI] [PubMed] [Google Scholar]
- 56.Traynor K. Privileging expands pharmacists’ role. Am J Health Syst Pharm. 2014;71(9):686–7. doi: 10.2146/news140031. [DOI] [PubMed] [Google Scholar]
- 57.Abramowitz PW, Shane R, Daigle LA, Noonan KA, Letendre DE. Pharmacist interdependent prescribing: A new model for optimizing patient outcomes. Am J Health Syst Pharm. 2012;69(22):1976–81. doi: 10.2146/ajhp120546. [DOI] [PubMed] [Google Scholar]
- 58.Victor RG. Expanding pharmacists’ role in the era of health care reform. Am J Health Syst Pharm. 2012;69(22):1959. doi: 10.2146/ajhp120569. [DOI] [PubMed] [Google Scholar]