Abstract
Healthcare providers are moving towards tailoring self-management interventions to include the communication technologies patients use in daily life. Accurate understanding of patients’ attitudes towards both technology and involvement in managing chronic conditions will be critical for informing effective self-management strategies. The tailoring of these interventions, however, could be undermined by providers’ implicit biases based on patient age, race, and education level that have been shown to negatively affect care. To inform the design and tailoring of self-management interventions, we elicited attitudes toward technology use and participation in care of 40 participants in a maximum variation sample. The analysis revealed three participant clusters—“Proactive Techies,” “Indie Self-Managers,” and “Remind Me! Non-Techies”—that represent varying attitudes toward health behaviors and technologies that were independent of race, education level, and age. Our approach provides insight into how people prioritize important values related to health participation and technology.
Introduction
Self-management of chronic conditions, such as diabetes and asthma, creates considerable burden for patients. Effective self-management requires patients to be active participants in treatment by taking medications, making lifestyle changes, and regulating emotions1,2. The day-to-day skills involved in self-management include identifying problems, selecting solutions, using information sources, collaborating with providers, changing behavior, and evaluating results2. This dynamic process goes well beyond adhering to treatment plans, and considers the patient holistically in the context of the attitudes and values that influence their everyday behaviors.
Self-management interventions are designed to alleviate some of the burden of chronic illness care. Self-management support through the internet, over the phone, and in person have proven effective, and the delivery of programs via SMS and other mobile platforms are promising3–8. However, tailoring and personalization of self-management interventions is limited by the lack of methods for understanding how patients prioritize health information and tools to accomplish self-care goals. Moreover, implicit biases of providers, such as ascribing preferences for health information and treatments on the basis of age, race, literacy, and gender, can differentially affect provision of chronic care for underrepresented minorities9–16. Therefore, understanding patients’ attitudes toward health and technology is especially important for informing unbiased and patient-centered interventions that augment patients’ health self-management strategies in everyday life.
To address the lack of understanding of the attitudinal factors that influence patients’ preferences for health information and technology, we studied how patients prioritize tools (e.g. email, cell phones, paper tools) to strengthen their accountability for health self-management. We found that patients’ attitudes toward mobile technology, accountability, and goal-setting were the most distinguishing and influential attitudes on patients’ approaches to health self-management. We also found that patients’ attitudes and values were more influential than demographic characteristics—especially race, age, and education level—on defining health self-management behaviors. We contribute a description of a method for eliciting preferences for self-management support, including attitudes toward adopting technology to attain health goals. Our empirical evidence from this study can inform new approaches to clustering patients and tailoring appropriate self-care support based on the tools, information, and goals they perceive to be essential to managing their health.
Related Work
Previous research on self-management, disparities in use of e-health services, and patterns of technology adoption inform our work. Below, we briefly summarize this literature and describe how our approach to clustering patients based on health and technology attitudes contributes new insights for supporting self-management.
Patient Self-management
Studies show that self-management interventions are effective in supporting patients to manage chronic illness17–19. In particular, interventions that systematically support patients to build skills in the three major domains of self-management—medical, role, and emotional—offer the most comprehensive support for self-care1,2. Within all three domains, self-management interventions are more likely to succeed if they target problems and strategies that patients perceive as most significant to their health, because the focus on patients’ strategies and concerns is motivating, engaging, and empowering2. Our approach provides researchers with a holistic perspective well-suited to tailoring self-management programs based on what patients perceive as essential to managing their health. As many healthcare providers are beginning to engage patients in care activities online and over mobile devices, we investigated both health and technology attitudes to understand technology adoption in support of patients’ overarching health goals.
Intervention research
Research on targeting self-management interventions has focused on understanding the sources of variation in the use of e-health services. For example, Goel et al20 investigated racial disparities in e-health services enrollment, and found that barriers to internet access did not explain these disparities; rather attitudinal barriers were significant. Similarly, Clark et al21 found that understanding attitudes and health priorities is particularly important for tailoring self-management interventions for socioeconomically vulnerable older adults. Finally, Lyles et al22 found that differences in portal use by race and ethnicity were not fully explained by differences in age, sex, sociodemographics, health status, or provider factors—particularly for black patients. Therefore, demographic characteristics provide limited help in understanding differences in portal use and how to tailor self-management support programs to the technologies patients use. Our approach to investigating values that influence patients’ use of e-health services can provide alternative perspectives on the attitudes that drive patient engagement in self-management programs.
The importance of understanding the attitudes and beliefs that influence engagement with health technologies may become even more important as intelligent information systems are deployed to support self-management. For example, recent approaches to mHealth care include intelligent systems that adapt to users depending on the patient’s beliefs about illness, medication, and information needs23. Researchers like Clark et al21 and Koch et al24 have called for a greater emphasis on the “self” in self-management, and have brought attention to the importance of understanding patient’s priorities, expectations, and expertise in the care process. Moreover, Valdez et al25 recently emphasized a “patient work approach” to designing applications aligned with patients’ and their family members’ health-related activities. As mHealth service design becomes more adaptive and personalizable, the “self” in self-management will become a focal point for tailored interventions. We demonstrate an approach for “getting to know” the patient that provides insight into how patients prioritize different values related to health and technology.
Finally, Pew26 data suggests that people from underserved populations, such as people with low education and ethnic minorities, are highly engaged with technology, even compared to privileged populations. These findings undermine implicit assumptions about correlations between low education level or racial minorities and low technology use. However, research by Sarkar et al27 also suggests that these populations are less likely to use technology to manage their health, which points to the need for researching the disparity between technology adoption for everyday life compared to health management. We demonstrate that qualitative research may provide important insights into the social and attitudinal barriers to adopting e-health services that can explain low technology adoption for health.
Methods
We used a mixed-methods approach that combined in-depth, semi-structured interviews with 40 participants, using a card sorting procedure called Q-methodology28,29 to elicit attitudes and opinions from persons managing a chronic illness. Q-methodology has been used in health30,31 and technology32 settings to understand patient perspectives. We conducted the interviews and Q-methodology procedure in participants’ homes, usually at their kitchen tables. Each interview lasted 1.5 to 2 hours and focused on understanding the participants’ health goals, priorities, and attitudes. The interviews were transcribed, and identifiable information was redacted to protect participants’ confidentiality. The study was reviewed and approved by the Internal Review Board of the Group Health Research Institute.
Participants
We recruited older adults with diabetes Type 1 and Type 2 (n=20), and mothers of children with asthma (n=20). We recruited these two distinct samples to maximize the variation in attitudes toward health self-management and technology use. We sampled mothers of children with asthma (rather than fathers or both parents) because women in this age group have ongoing health care needs relevant to reminders, such as screening for cervical cancer. All participants (see Table 1) were sampled from Group Health Cooperative, a large integrated healthcare delivery system in Washington State. We purposely oversampled racial and ethnic minorities, who would substantially benefit from improvements in care related to technology and chronic illness management. These interviews were the second round of interviews for 34 of the 40 participants. We had recruited these 34 participants by mail and phone from a bank of 586 people for this three-year multi-part study. The remaining 6 people were recruited from a new bank of 99 people (25 older patients, and 74 mothers). Older adults (10 of 20 were male) had a median age of 73 years, and mothers had a median age of 38 years. After the interview, they received $50 for completing the study.
Table 1.
Participant demographics by attitude cluster and cohort. A=asthma cohort; D=diabetes cohort.
| Cohort | Proactive Techies | Indie Self–Managers | Remind Me! Non–Techies | Combined | ||||
|---|---|---|---|---|---|---|---|---|
| A | D | A | D | A | D | N | % | |
| Participants | 8 | 6 | 6 | 7 | 3 | 6 | 36 | 90 |
| Male | – | 3 | – | 5 | – | 2 | 10 | 25 |
| Race/Ethnicity | ||||||||
| Black | 2 | 4 | 4 | 1 | – | 2 | 13 | 32.5 |
| Hispanic | 2 | – | – | – | – | 1 | 3 | 7.5 |
| Asian | – | – | – | 2 | – | – | 2 | 5 |
| White | 4 | 2 | 2 | 4 | 2 | 3 | 17 | 42.5 |
| Mixed/Other | – | – | – | – | 1 | – | 1 | 2.5 |
| Education | ||||||||
| High School/GED | 2 | 3 | 1 | 2 | – | 3 | 11 | 27.5 |
| Some College | 1 | 1 | 1 | 2 | 2 | 1 | 8 | 20 |
| 4-year degree | 4 | 2 | 1 | 1 | 1 | – | 9 | 22.5 |
| More than 4-year | 1 | – | 3 | 2 | – | 2 | 8 | 20 |
| Portal User | 7 | 3 | 5 | 5 | 1 | 4 | 25 | 62.5 |
In-depth Interviews and Q-methodology
The interview protocol contained open-ended questions about health goals, and a reflection on the challenges and personal significance of nationally recommended health tasks appropriate to the age and diagnoses of each participant. The Q-methodology procedure was conducted at the end of the interview. The data collection procedure for Q-methodology consists of a set of subjective statements printed on cards that the participant arranges according to what is most personally significant to them. It is a highly structured data collection procedure wherein participants arrange the statements in a grid that is shaped in a normal distribution. The extremes of the distribution represent the statements that the participant feels most strongly about (See Figure 1): “Most Agree” to “Most Disagree” are located at either end of the Q grid, with “Neutral” in the middle. The statements that participants place at the extremes receive the most weight in the cluster analysis of the data, revealing the health and technology attitudes that distinguish unique patient perspectives (See Table 2).
Figure 1.
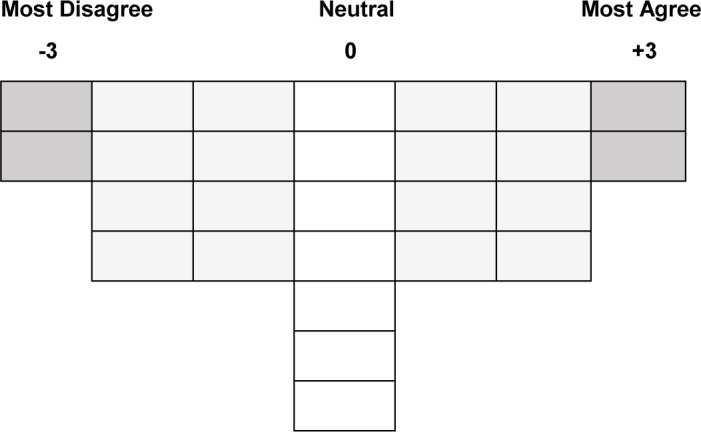
Q-methodology data collection instrument.
Table 2.
Example distinguishing statements for each attitude cluster, (p>0.05). +3=Most Agree; −3=Most Disagree.
| Distinguishing Statement | Statement Ranking | |
|---|---|---|
| Proactive Techies | I like using electronic communication with my doctor. I’m more likely to follow through on paper mail reminders. |
+3 −3 |
| Indie Self- Managers | I’m the one who is responsible for taking care of my health. My health will improve if I get better at mobile technology. |
+3 −3 |
| Remind Me! Non-techies | My health will improve if I set health goals with my doctor. I mostly keep track of health tasks in my head. |
+3 −3 |
Our Q statement set consisted of 27 statements based on a health-sciences theoretical framework. The statements were categorized into two groups: (1) attitudes toward health self-management, especially related to core self-management skills; and (2) attitudes toward using and adopting technology. We developed statements in the first category on self-management attitudes based on the three large domains of work in chronic illness care originally identified by Corbin and Strauss1 and incorporated into self-management support programs by Lorig and Holman2. These included the work of medical management, emotional support, and redefining life roles. We used prior instruments of patient activation to inform statements representing patients’ attitudes towards self-management in these domains. These include the Patient Activation Measure (PAM)34 and the Patient Assessment of Chronic Illness Care (PACIC)35. The PAM assesses patients’ self-management beliefs, knowledge, skills, and confidence. The PACIC scale assesses the extent to which the patient has received care congruent with the Chronic Care Model and includes a subscale of patient activation. We used both of these scales to inform a set of statements on a continuum of patients’ self-management beliefs, confidence, and practices36. These statements allowed us to observe how patients prioritize health and technology behaviors for health self-management. We derived the wording of statements from qualitative data from a previous round of interviews with these participants33,37.
Analysis
We analyzed the data with PQMethod38, a widely used application for conducting exploratory cluster analyses of Q-methodology data. We conducted a principal components analysis that extracted 8 components, 3 of which explained 53% of the variance in the data. We chose to retain only 3 components for interpretation based on the standard criteria for factor rotation (i.e. proportion of variance, scree test, and interpretability)39,40. We rotated the three components using varimax, a standard orthogonal rotation method.
We used the distinguishing statements—statements that distinguish each cluster based on statistical significance—to inform the qualitative analysis of the interview data (See Table 2). By checking the themes that emerged from the distinguishing statements in the cluster analysis against the qualitative data, we were able to interpret the clusters in the context of each participant’s health goals, and to report on their attitudes and beliefs using their own words. Moreover, this method of qualitative validation is especially important when working with marginalized populations41. Participant quotes are incorporated into our results, with A# identifiers denoting the words of mothers with children who have asthma, and D# identifiers denoting quotes from diabetes patients.
Results
The principle components analysis resulted in three clusters that represent three unique perspectives on both health attitudes and tools that are essential to health self-management. These three components yielded excellent interpretability and a “simple structure,” with only 4 participants whose views are excluded from analysis due to their loading significantly onto more than one component. Clusters 1 (n=14), 2 (n=13), and 3 (n=9), do not correlate with age, race, educational background, portal use, gender, or disease. Rather, each cluster represents a unique attitude towards health self-management held by a diverse subset of the sample (see Table 1). We describe each cluster below, and characterize them as: (1) Proactive Techies; (2) Indie Self-Managers; and (3) Remind Me! Non-Techies. We denote the distinguishing statements for each cluster with the ranking assigned to it, on a scale of Most Agree (+3) to Most Disagree (-3), by participants of the cluster.
Cluster 1: “Proactive Techies”
Fourteen participants (3 male) define this cluster, including six participants from the diabetes cohort (ages 63–74) and eight from the asthma cohort (ages 32–49) (see Table 1). This cluster has a high technology profile. The participants who define this cluster strongly agree that cell phones (+2), electronic communication (+3), and knowledge of the science behind health advice (+2) are essential to health self-management. They somewhat agree that electronic reminders will reduce the stress of managing their health (+1) and that online calendars are the best way to manage their health (+1). Consistent with their preference for electronic methods, they strongly disagree that paper calendars (-3) and reminders (-3) are useful for health self-management.
Patients in this cluster were distinguished by their emphasis on the connection between health self-management and technology use. These patients used technology to take the initiative with their health care by proactively tracking health indicators, understanding scientific health information, and setting personal goals. This health tracking behavior supported these patients to set health goals for themselves and to take responsibility for their health outcomes. In particular, older adults with diabetes described using technology to track self-care activities. For example, D15, a black man with some college education, recounted how he used a spreadsheet to track his blood glucose levels, and sent it in an email to give his doctor a “heads up”:
“It’s going back about 18 months ago, I went and got it [blood glucose] on Excel in a nice little graph that looked good to me … when we had my primary care doctor and we met, she was able to say okay, you need to up your medication…[the doctor] had a heads up before I got there, not only from her examination but from me sending her information.”
Similarly, D6, a black woman with a 4-year degree, described how she used the patient portal to track a detailed history of her A1C test results:
“[On the patient portal] there’s information about the test, why they take the test, what the numbers are, whatever it is. So you know where you should be, and then they keep it - I think mine started 2008, they keep it for a long time and they have a chart so you can see where your ups and downs are.”
D7, another black woman with a 4-year degree, described how she uses her cell phone for keeping track of her health, “I keep my appointments in there [cell phone]. I have my pacer in there to track the number of steps I walk. I have things on my calendar, what days I do certain exercises and stuff on there.” Another older patient, D11, a white man with a high school education, described a very different reason that his cell phone helped him to take control of his health, “They [providers] got our home phone number and there’s times they call and leave a message on there, I’ve always got my cell phone with me and then if we’re out for the day or something, I won’t miss a message.” This patient used a cell phone to check his voicemail messages on his home phone while he was away. Although this patient may not be considered a typical example of a “high tech” self-manager, from the perspective of this patient, cell phones were explicitly prioritized for managing his health.
Many of these “proactive techies” placed a high value on health information, and especially prioritized scientific evidence to enhance accountability for acting on doctor recommendations. A20, a white woman with more than a 4-year degree, described the importance of health information and the value of email for enabling her to proactively communicate with her doctor about the accuracy of her research, “ like “I read this about my child2019s condition, is this even accurate, would you agree, disagree?”…I need someone to double-check the information that I’m finding and give me an answer.”
A12, a Hispanic woman with a high school education, also emphasized the value of health information. She expressed not having enough information, and wanted to learn more detailed scientific health information from her doctors, however: “They’re [providers are] not prepared to have details about what are the studies behind this, what were the outcomes of that study and the percentages of side effects and that kind of thing. They’re not ready at hand with that kind of thing.” This patient had the desire to have more scientific evidence for the health tests, medications, and behaviors that were recommended by her doctor. She recalled how, in the past, she had used different resources to get the information that her doctors could not provide, “The oncologist that I had connected with, I guess, told me what the options were. I researched what the options were and people who’ve gone through those options, and then came back with a decision on how to move forward with it.”
D6, a black woman with a 4-year degree, also described wanting more information so that she could be a better judge of her health status relative to the norms for her age and race,
“Unfortunately, they [providers] can’t give you information you need on genetics and heredity and stuff like that, especially for African Americans, because we may be at some point of African descent but that’s not all we are. For the majority of us, that’s not all we are, so we’re just grouped, and because this country has a 1/8 rule, we’re just grouped… if you’re African American and Asian your [A1C] numbers are higher because of the genetics there. That’s what I’m getting at - so it really matters.”
Although six patients in this cluster were over the age of 60, and five had a high school education or less, all patients in this cluster used technology to be proactive about their health. Regardless of age, race, and ethnic background, these patients prioritized technology for tracking health indicators, communicating with providers, and finding scientific health information.
Cluster 2: “Indie Self-Managers”
Thirteen participants (5 male) define this cluster, including seven participants from the diabetes cohort (ages 62–>89), and six from the asthma cohort (ages 28–43) (see Table 1). This cluster has high accountability for health self-management, expressing a strong belief that they have an active role in care (+3). Patients in this cluster considered technology to be a low priority for health. They are strongly independent (“indie”) and rely on keeping track of health tasks in their heads (+2). They disagree with the idea of needing follow-up from the doctor to stay on track with their health (−2), and with the idea that someone should check in with them to help remind them (−2). They strongly disagree that use of mobile technology is linked to better health outcomes (−3).
In contrast to cluster 1, patients in cluster 2 did not prioritize health information, nor did they connect technology use with health outcomes. Although all patients in this cluster described using a cell phone, and used it for other aspects of their lives, they did not consider it essential to their health.
For example, A4, a black woman with a high school education, said, “I use my cell phone and email and stuff, but I personally don’t see how that affects my health.” Similarly, D8, an Asian man and the oldest patient in our sample, described why his cell phone was not linked to his health outcomes, “a cell phone is just another convenience, you know. I don’t need it on the list of things I feel essential for managing my health.” A14, a white woman with more than a 4-year degree, made an even more explicit distinction between the use of her cell phones for everyday activities versus health activities. She described how her cell phone was directly at odds with the nature of her health self-management strategies, “my health needs me to be peaceful and relaxed and meditate and dealing with my emotional issues … a cell phone’s just a tiny little thing and it’s actually a little bit detrimental. It’s starting to become a little bit of a problem for me.” This patient noted the potential negative impacts on her health of communication technologies.
Although there was a weak link between technology and self-management for patients in this cluster, there was a strong sense of accountability. These patients felt strongly that they were responsible for their health, a statement that distinguished this cluster from others. D3, a black woman with more than a 4-year degree, gave a powerful example of how she took control of her health outcomes during a disagreement with her provider, “She [the doctor] wasn’t as receptive as I wanted her to be so I said some things at the end – it wasn’t in anger, but like ‘I’ll tell you,’ and because I said that she told me some things that’s been very beneficial to me.” Similarly, A14 described herself as an empowered patient, “I am confident, I have ownership. I feel like it’s my job to take care of that area of my life, I’m not passive, I’m an active player.” A9, a black woman with more than a 4-year degree, shared a similar sentiment about her role in care, “Just that, because it’s my body and I think I’m the expert. I know what’s going on with it versus someone that’s telling me what’s going on with it.”
Patients in this cluster prioritized health education because it helped them to be accountable for their health. The explicit connection between health education and accountability was unique for these patients. For example, A4 explained:
It empowers you, it holds you accountable versus thinking - I don’t know, I’ve seen people who are like this is what’s wrong, and they’re constantly running to the doctor type of thing, but not really fixing what the issue is, just treating it constantly. I think it is good to be educated so that you could take care of it.
A9 had a similar view, “Getting the quality of the office visits we’re getting, the education that the doctor’s able to provide…It’s nice to know what you’re talking about and be able to help a child, based on what you actually know rather than guessing.”
For these independent self-managers, their “mental attitude,” as D8 put it, was more essential to health self-management than the technologies they used in everyday life. Their low adoption of technology specifically for health self-care was due to perceived negative impacts of reliance on cell phones, and an emphasis on autonomy from both technology and provider authority. They emphasized accountability and empowerment through health education.
Cluster 3: “Remind Me! Non-Techies”
Nine participants (2 men) define this cluster, including six from the diabetes cohort (ages 63–88) and three from the asthma cohort (ages 38–45) (see Table 1). This cluster has low accountability for self-management, and a low technology profile. They strongly agree that their health will improve if they set health goals with their doctor (+3), and that they need follow up from the doctor to stay on track with their health (+2). They dislike using electronic communication with their doctor (−1), and prefer phone calls (+1). They strongly disagree with keeping track of health tasks in their heads (−3), and do not believe in using online calendars (−1) or that mobile technology will improve health outcomes (−1). They agree that their health will improve if follow-up notices are clearer (+1).
Cluster 3 was characterized by their strongly positive attitudes toward goal-setting with their doctors and follow-up care. They placed a low priority on email and mobile technology and instead preferred phone calls with providers to stay on track with their health. Although they expressed agreement with being responsible for health, these patients were distinguished by their greater reliance on health care providers to guide and motivate healthy lifestyles.
The follow-up phone calls from providers were highly prized, if not relied upon, by these patients. For example, when asked about why she preferred phone communication, A18, a woman with some college education, said, “That’s when I know I need to take action. Like if I’ve procrastinated for a while.” Similarly, A17, a white woman with more than a 4-year degree, found it difficult to prioritize health goals without the doctor checking in:
I get home and in my own brain, I sort of prioritize what was important and if life gets busy, I will prioritize other things above my health. If someone is calling you and holding you accountable to it, you feel if there’s a priority for that person to call me, I’d better respect that, and keep it a priority.
Prioritizing health goals was a common challenge among these participants. A18 explained how follow-up could help her to stay on track, “If she [doctor] could have a goal, eating better or eating more fruits or whatever it is. And then once in a while if she sends me a thing that says ‘how’s it going with this?’ – Oh yeah, I’m supposed to be doing this!”
Patients also perceived follow-up as an important source of motivation for staying on track with health goals. For example, D16, a black man with a high school education, talked about needing motivation from his provider. When asked how his doctor could motivate him, he said “Be there on me…My doctor’s cell phone, he can do more.” This patient had several health complications, including two leg amputations, and limited speech due to a stroke. D5, a Hispanic woman with a high school education, who also had complications from comorbidities, described how better follow-up from her doctor could motivate her health management, “He’d [the doctor] make sure I go to the gym. He’d make sure I’m getting dialysis. He’d make sure he checks me once a month, they check everything I have to be doing.”
Finally, D14, a white woman with a high school education, expressed the value of having health goals with a provider, “If you go ‘that’s the way life is,’ that’s not helping anybody, but if he [the doctor] sets a goal – ‘okay, do more exercise, drink more water,’ then you know - I’ve got goals that will help me.” This echoes a statement from D2, a black woman with more than a 4-year degree, about the importance of health goals, “I think everybody needs goals, whether health or in anything, and goals would be a motivating factor.”
Discussion
The most surprising finding from this study is that it revealed attitude clusters that each contained a broad spectrum of patients in terms of race, age, education, patient-portal use, and diagnosis. Studies confirm that providers rely on these kinds of observable cues, especially race and age, to assess patients’ health attitudes and make treatment recommendations9–16. In contrast, our findings provide evidence that patients’ attitudes toward health information and technology are not correlated with any of those observable cues. These attitudes and values are more influential than demographic characteristics on health self-management behaviors.
Our work can inform new approaches to clustering and understanding patients to inform tailored self-management interventions. In particular, our work suggests that attitudes toward health and technology can interact in unexpected ways, such as the “Indie Self-Mangers” who engage with technologies in everyday life but do not connect their technology competency with health self-management. Another example of unexpected interactions of health and technology attitudes is in “Cluster 1: Proactive Techies”, wherein six patients over the age of 60 years agreed that electronic communication and cell phones were essential to managing their health. Furthermore, A12 and A19, both women of color with high school educations, were “Proactive Techies” who expressed a strong sense of self-efficacy and technology use for health self-management. These examples are especially significant given that socioeconomic status, which encompasses education status, has been shown to have the broadest effect on physician’s perceptions of patient competence, compared to race and age12.
Researchers have extensively explored effects of race, gender, and literacy on clinician behavior9–16, but have not investigated differences in the attitudes of a diverse set of patients’ toward self-management and technology. We found that patients’ attitudes have a strong influence on technology adoption and accountability for health that have implications for patient-provider relationships. In addition, those relationships extend through at-home, patient-centered self-management programs. For example, the “Remind Me! Non-Techies” had a passive attitude toward health self-care, and relied upon providers for reminders and monitoring of progress toward health goals. Moreover, members of this cluster contradicted stereotypes of white patients with high education, who are often perceived by providers as highly motivated and effective self-managers11,12. For example, A17, a white woman with more than a four-year degree, did not use the patient portal, and relied on the doctor to keep her on track, “if the doctor’s office is calling, you feel like oh! – okay.” Our results suggest that self-management programs for these low-technology users could leverage their respect for provider authority by delivering self-management content that encourages the feeling of being mentored by a provider. In contrast, interventions for “Proactive Techies” are more likely to be adopted if they support patient-initiated exploratory approaches to health tracking and goal-setting. Similarly, interventions for “Indie Self-Mangers” can be tailored to suit their strong preference for control over decision-making in care, providing tools that encourage autonomy and self-improvement through health education.
Finally, our work suggests that patients’ attitudes toward health information and technology may be important for understanding why patients adhere to, or fail to adhere to, treatment recommendations. Differences in these attitudes may have implications for health outcomes because these attitudes affect patients’ participation in care. Moreover, understanding the attitudes that distinguish different approaches to self-management can help providers to develop nuanced approaches to tailoring interventions for patients across a spectrum, from fully “activated” to fully “passive”42. Traditional scales that provide insight into patients’ perceptions of their role in care, like the PAM34, can be complemented with methods like ours that provide insight into patients’ strategies and motivations for developing their self-care capacity. We demonstrate the advantages of observing the interaction of health and technology attitudes for providing a holistic view of the attitudes and tool-use strategies that influence self-management.
Conclusion
Our findings demonstrate three unique clusters of self-managers based on different health and technology values. These three clusters demonstrate the limitations of a “one-size fits all” approach to self-management interventions, especially when these interventions are mediated by electronic communication tools like cell phones and email. We demonstrate that Q-methodology can be a useful approach for understanding patients’ attitudes toward technology and self-management. In addition, it could inform new approaches to clustering patients and matching them with appropriate self-care support. Prior research shows that raising clinician awareness of biases mitigates the effect of those biases, thus reducing healthcare disparities16. This study suggests that an understanding of patients’ attitudes toward self-management and technology could inform unbiased, patient-centered interventions. Moreover, our approach has highlighted different values that influence technology adoption for health self-management, and this work could inform new scale development for assessing the appropriateness of computer-mediated interventions for patients. Overall, a greater awareness of the health and technology priorities of patients can help clinicians to leverage patient’s values and strategies for enhancing self-management. This work encourages clinicians and technology developers to combat implicit biases based on race, age, and education by eliciting patients’ values that define health self-management.
Acknowledgments
This project was funded by grant #R01HS021590 from the Agency for Healthcare Research and Quality (AHRQ).
References
- 1.Corbin JM, Strauss A. Unending Work and Care: Managing Chronic Illness at Home. Jossey-Bass; 1988. [Google Scholar]
- 2.Lorig KR, Holman H. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med. 2003;26(1):1–7. doi: 10.1207/S15324796ABM2601_01. http://www.ncbi.nlm.nih.gov/pubmed/12867348. [DOI] [PubMed] [Google Scholar]
- 3.El-Gayar O, Timsina P, Nawar N, Eid W. A systematic review of IT for diabetes self-management: are we there yet? Int J Med Inform. 2013;82(8):637–652. doi: 10.1016/j.ijmedinf.2013.05.006. [DOI] [PubMed] [Google Scholar]
- 4.Vervloet M, van Dijk L, Santen-Reestman J, et al. SMS reminders improve adherence to oral medication in type 2 diabetes patients who are real time electronically monitored. Int J Med Inform. 2012;81(9):594–604. doi: 10.1016/j.ijmedinf.2012.05.005. [DOI] [PubMed] [Google Scholar]
- 5.Simon G, Ralston J, Savarino J. Randomized trial of depression follow-up care by online messaging. J Gen Intern Med. 2011;26(7):698–704. doi: 10.1007/s11606-011-1679-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Glasgow RE, Kurz D, King D, et al. Twelve-month outcomes of an Internet-based diabetes self-management support program. Patient Educ Couns. 2012;87(1):81–92. doi: 10.1016/j.pec.2011.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ralston J, Hirsch I, Hoath J. Web-based collaborative care for type 2 diabetes a pilot randomized trial. Diabetes Care. 2009;32(2):234–239. doi: 10.2337/dc08-1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lorig KR, Laurent DD, Deyo Ra, Marnell ME, Minor Ma, Ritter PL. Can a Back Pain E-mail Discussion Group improve health status and lower health care costs?: A randomized study. Arch Intern Med. 2002;162:792–796. doi: 10.1001/archinte.162.7.792. [DOI] [PubMed] [Google Scholar]
- 9.Cooper La, Roter DL, Carson Ka, et al. The associations of clinicians’ implicit attitudes about race with medical visit communication and patient ratings of interpersonal care. Am J Public Health. 2012;102(5):979–987. doi: 10.2105/AJPH.2011.300558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sabin JA, Greenwald AG. The influence of implicit bias on treatment recommendations for 4 common pediatric conditions: Pain, urinary tract infection, attention deficit hyperactivity disorder, and asthma. Am J Public Health. 2012;102(5):988–995. doi: 10.2105/AJPH.2011.300621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lutfey KE, Ketcham JD. Patient and provider assessments of adherence and the sources of disparities: Evidence from diabetes care. Health Serv Res. 2005;40:1803–1817. doi: 10.1111/j.1475-6773.2005.00433.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Van Ryn M, Burke J. The effect of patient race and socio-economic status on physicians’ perceptions of patients. Soc Sci Med. 2000;50:813–828. doi: 10.1016/s0277-9536(99)00338-x. [DOI] [PubMed] [Google Scholar]
- 13.Balsa A, McGuire T. Prejudice, clinical uncertainty and stereotyping as sources of health disparities. J Health Econ. 2003;22(1):89–116. doi: 10.1016/s0167-6296(02)00098-x. [DOI] [PubMed] [Google Scholar]
- 14.Green AR, Carney DR, Pallin DJ, et al. Implicit bias among physicians and its prediction of thrombolysis decisions for black and white patients. J Gen Intern Med. 2007;22(9):1231–1238. doi: 10.1007/s11606-007-0258-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fincher C, Williams JE, MacLean V, Allison JJ, Kiefe CI, Canto J. Racial disparities in coronary heart disease: a sociological view of the medical literature on physician bias. Ethn Dis. 2004;14(3) [PubMed] [Google Scholar]
- 16.Chapman E, Kaatz A, Carnes M. Physicians and implicit bias: how doctors may unwittingly perpetuate health care disparities. J Gen Intern Med. 2013;28(11):1504–1510. doi: 10.1007/s11606-013-2441-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Coleman K, Austin B, Brach C, Wagner E. Evidence on the Chronic Care Model in the new millennium. Health Aff. 2009;28(1):75–85. doi: 10.1377/hlthaff.28.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lorig KR, Sobel DS, Stewart AL, et al. Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization: a randomized trial. Med Care. 1999;37(1):5–14. doi: 10.1097/00005650-199901000-00003. [DOI] [PubMed] [Google Scholar]
- 19.Chodosh J, Morton SC, Mojica W, et al. Meta-analysis: chronic disease self-management programs for older adults. Ann Intern Med. 2005;143(6):427–438. doi: 10.7326/0003-4819-143-6-200509200-00007. [DOI] [PubMed] [Google Scholar]
- 20.Goel MS, Brown TL, Williams a, Cooper a J, Hasnain-Wynia R, Baker DW. Patient reported barriers to enrolling in a patient portal. J Am Med Informatics Assoc. 2011;18:i8–i12. doi: 10.1136/amiajnl-2011-000473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Clark DO, Frankel RM, Morgan DL, et al. The meaning and significance of self-management among socioeconomically vulnerable older adults. J Gerontol B Psychol Sci Soc Sci. 2008;63(5):S312–S319. doi: 10.1093/geronb/63.5.s312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lyles CR, Harris LT, Jordan L, et al. Patient Race/Ethnicity and Shared Medical Record Use Among Diabetes Patients. Med Care. 2012;50(00):434–440. doi: 10.1097/MLR.0b013e318249d81b. [DOI] [PubMed] [Google Scholar]
- 23.Piette JD, Farris KB, Newman S, An L, Sussman J, Singh S. The Potential Impact of Intelligent Systems for Mobile Health Self-Management Support: Monte Carlo Simulations of Text Message Support for Medication Adherence. Ann Behav Med. 2014;49:84–94. doi: 10.1007/s12160-014-9634-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Koch T, Jenkin P, Kralik D. Chronic illness self-management: locating the “self”. J Adv Nurs. 2004;48(5):484–492. doi: 10.1111/j.1365-2648.2004.03237.x. [DOI] [PubMed] [Google Scholar]
- 25.Valdez RS, Holden RJ, Novak LL, Veinot TC. Transforming consumer health informatics through a patient work framework: connecting patients to context. J Am Med Informatics Assoc. 2015;22(1):2–10. doi: 10.1136/amiajnl-2014-002826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pew Research Center Mobile Technology Fact Sheet. 2014. http://www.pewinternet.org/fact-sheets/mobile-technology-fact-sheet/
- 27.Sarkar U, Karter AJ, Liu JY, et al. Social disparities in internet patient portal use in diabetes: evidence that the digital divide extends beyond access. J Am Med Inform Assoc. 2011;18:318–321. doi: 10.1136/jamia.2010.006015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brown SR. Political Subjectivity: Applications of Q Methodology in Political Science. Yale Press; 1980. [Google Scholar]
- 29.Watts S, Stenner P. Doing Q Methodological Research: Theory, Method and Interpretation. LA: Sage; 2012. [Google Scholar]
- 30.Akhtar-Danesh N, Baumann A, Cordingley L. Q-Methodology in Nursing Research. West J Nurs Res. 2008;30(6):759–773. doi: 10.1177/0193945907312979. [DOI] [PubMed] [Google Scholar]
- 31.Cross RM. Exploring attitudes: the case for Q methodology. Health Educ Res. 2005;20(2):206–213. doi: 10.1093/her/cyg121. [DOI] [PubMed] [Google Scholar]
- 32.O’Leary K, Wobbrock JO, Riskin EA. Q-methodology As a Research and Design Tool for HCI; Proceedings of the SIGCHI Conference on Human Factors in Computing Systems; CHI ‘13 New York, NY, USA: ACM; 2013. pp. 1941–1950. [Google Scholar]
- 33.Kendall L, Eschler J, Lozano P, McClure JB, Vizer LM, Ralston JD PW. Engineering for reliability in at-home chronic disease management; AMIA ‘14 Proceedings of the 2014 Annual Conference of the American Medical Informatics Association; Washington D.C.; 2014. [PMC free article] [PubMed] [Google Scholar]
- 34.Hibbard JH, Mahoney ER, Stockard J, Tusler M. Development and testing of a short form of the patient activation measure. Health Serv Res. 2005;40(6 Pt 1):1918–1930. doi: 10.1111/j.1475-6773.2005.00438.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Glasgow RE, Wagner EH, Schaefer J, Mahoney LD, Reid RJ, Greene SM. Development and validation of the Patient Assessment of Chronic Illness Care (PACIC) Med Care. 2005;43(5):436–444. doi: 10.1097/01.mlr.0000160375.47920.8c. [DOI] [PubMed] [Google Scholar]
- 36.O’Leary K, Eschler J, Kendall L, Vizer L. Understanding Design Tradeoffs for Health Technologies: A Mixed-Methods Approach; Proceedings of the 33rd Annual ACM Conference on Human Factors in Computing Systems; 2015. pp. 4151–4160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Eschler J, Kendall L, O’Leary K, Vizer L, Lozano P, McClure J, Pratt W RJ. Shared calendars for home health management; CSCW’15 Proceedings of the ACM Conference on Computer Supported Cooperative Work and Social Computing; Vancouver, BC: 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schmolk P. PQMethod Software. 2014. http://schmolck.org/qmethod.
- 39.Hatcher L. Principal Component Analysis. A Step-By-Step Approach to Using SAS Syst Factor Anal Struct Equ Model. 1994:1–56. [Google Scholar]
- 40.Costello AB, Osborne J. Best practices in exploratory factor analysis: Four recommendations for getting the most from your analysis. Practical Assesment. Res Eval. 2005 [Google Scholar]
- 41.Johnson RB. Examining the validity structure of qualitative research. Education. 1997;118(2) [Google Scholar]
- 42.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: the chronic care model, Part 2. JAMA. 2002;288:1909–1914. doi: 10.1001/jama.288.15.1909. [DOI] [PubMed] [Google Scholar]


