Abstract
In recent years, Decision Support Systems (DSSs) have been developed and used to achieve “meaningful use”. One approach to developing DSSs is to translate clinical guidelines into a computer-interpretable format. However, there is no specific guideline modeling approach to translate nursing guidelines to computer-interpretable guidelines. This results in limited use of DSSs in nursing. Unified modeling language (UML) is a software writing language known to accurately represent the end-users’ perspective, due to its expressive characteristics. Furthermore, standard terminology enabled DSSs have been shown to smoothly integrate into existing health information systems. In order to facilitate development of nursing DSSs, the UML was used to represent a guideline for medication management for older adults encode with the International Classification for Nursing Practice (ICNP®). The UML was found to be a useful and sufficient tool to model a nursing guideline for a DSS.
Introduction
Clinical practice guidelines are indispensable to healthcare providers. Guidelines provide care recommendations which are synthesized from a systematic review of evidence to optimize patient care. Clinical practice guidelines are a vehicle to translate health care knowledge and outcomes of research into a user-friendly format. Many guidelines have been published by professional organizations, government agencies and health care institutions since they have been shown to reduce variation in practice and to improve the quality of care. Studies indicate that clinicians’ guideline compliance is increased when guidelines are implemented in a computerized decision support system (DSS) because they are able to deliver patient-specific care at the point of care1,2.
In recent years, meaningful use of health information technology has the expectation of improvement in the quality, safety, and even the cost of health care. Specific objectives to achieve meaningful use are developed by the Center for Medicare and Medicaid Services (CMS); one of the objectives involves using DSSs. CMS provides financial incentives to institutions that meet meaningful use requirements. To be eligible for incentive payments, one DSS should be incorporated into an institution’s electronic health record to support clinicians’ decision-making process3.
In spite of such important benefits, limited DSSs are used in nursing. One plausible reason is that DSSs developed for nurses often did not meet nurses’ information needs4,5. When a DSS is developed without accurate knowledge translated from a guideline, it does not provide accurate information to clinicians at the point of care. Studies show that formalization of guidelines as computer-interpretable guidelines (CIGs) makes a DSS more accurate and reliable6,7. Since most nursing guidelines are written in free text, tables and flow charts, it is necessary to develop CIGs to represent the underlying knowledge with explicit notations to define the semantics and provide reasoning mechanisms8. CIGs could facilitate development of various DSSs for nurses’ use, however, no formal modeling language to translate guidelines to CIGs has been developed for nursing use.
Unified Modeling Language (UML) is a software writing tool that has been widely used to model health information systems because of its useful effects of visualizing, specifying, constructing, and documenting the artifacts of a system from the end-users’ perspective9. It may also be a useful tool to model a nursing guideline from the nurses’ point of view.
DSSs also need to be integrated with existing health information systems for data reuse and patient-specific recommendations. Studies indicate that standard terminology enabled DSS can be seamlessly integrated with existing health information systems10,11. The purpose of this study is to illustrate steps involved in modeling a nursing guideline using the International Classification for Nursing Practice (ICNP®) and UML to develop a web-based medication management decision support system for older adults (Web-based medication management DSS).
Background
Computer-interpretable guidelines (CIGs)
A CIG is a systematically visualized and specified guideline by graphic notations to describe core knowledge of a guideline. This translation of a guideline has been useful to develop DSSs because it allows accurate and complete interpretation of guideline content. Studies show that CIG-based DSSs are easy to maintain (i.e. upgrading) and are adapted easily in local health care settings6,8. Accordingly, many modeling approaches have been developed to represent and execute guidelines. Three distinct modeling approaches are found in the medical informatics community and categorized as: 1) Document models (i.e. Guideline Elements Model: GEM), 2) Decision tree and probabilistic models (i.e. Fuzzy Cognitive Maps: FCM) and 3) Task-network models (i.e. Guideline Interchange Format: GLIF)7. Despite such efforts, only a few guideline modeling approaches have progressed beyond the prototype stage6.
Unified Modeling Language (UML)
The UML is a standard software writing language that was used to design and develop software systems12. It is also an expressive language that can describe all the viewpoints needed to develop systems. It is used to: 1) visualize, 2) specify, 3) construct, and 4) document the elements of a software system. UML facilitates communication between developers and end-users of software by allowing them to examine objects in a system. Its ability to specify allows the UML to build a precise, unambiguous and complete system. A model constructed by the UML can also be mapped directly to an object-oriented programming language (i.e. Java or C++). Thus, a system prototype can be tested in early stages of the development, allowing for early refinement. In addition, UML can be used to document whole processes of developmental stages and tasks. These records help control, measure, and maintain a system after its deployment13.
Standardized terminology in decision support systems
Due to the government emphasis on “meaningful use” for Electronic Health Records, DSSs are widely introduced in healthcare institutions. However, their adoption by clinicians has been slow and many challenges have emerged in development and implementation stages. One of the challenges is incorporating standardized terminology in a DSS. According to Ahmadian and colleagues’ literature review and survey, 58% of DSS developers experienced problems at developmental stages and 92% of these problems were related to data standardization10. In addition to this, terminology standardization is an important requirement for scalable DSSs. Standard terminology and information models to represent health care data should be incorporated in DSSs for seamless integration11.
To increase adoption and interoperability potential, a standard nursing terminology, ICNP was selected because it is a compositional terminology that facilitates the development of and the cross-mapping among local terms and existing terminologies. ICNP includes nursing diagnoses, nursing interventions and nursing-sensitive patient outcomes that describe nursing practice14. The use of a standard nursing terminology such as ICNP facilitates description of nursing diagnoses, interventions, and outcomes for medication management nursing care and extraction of these data for later use15.
Older adults and medication management
For older adults, the desire to remain independent as long as possible is critical. Research suggests that the ability to remain independent is highly dependent on the ability to manage medications16,17. Multiple health conditions in the aging population often result in complex medication regimens that make this population vulnerable to adverse reactions to medications. The need for an electronic evidence-based decision support system to assist nurses in managing medications for older adults living the community is imperative. This type of computer system also has the potential to improve patients’ self-management of their health17.
In recent years, health information technology has been used to improve care for older adults. Automated assessment tools and DSSs were developed and embedded in electronic health records18. Nursing studies regarding teleHealth interventions were conducted19,20. It is the appropriate time to develop a nursing DSS for older adults living in the community.
Modeling Steps
Step 1: Selection of a guideline for medication management for older adults
In the United State, approximately three million older adults are admitted to nursing homes because of their inability of manage a complicated medication regimen. It is estimated that the annual care cost for this population is $177 billion dollars17,21. Approximately 30% of hospitalizations of older adults are drug related and older adults who are discharged from the hospital with more than five medications are more likely to visit the emergency department and to be re-hospitalized within six months22. Unfortunately, due to complications with medications, older adults may not be able to live independently in the community. Nurses, aided by evidence-based decision support can partner with older adults and families in the community to safely manage medication.
A nursing practice guideline, “Medication Management of the Community-Dwelling Older Adult” (MM-guideline) was selected as a content source for this study. This evidence-based guideline was developed through support from the US Agency for Healthcare Research and Quality23.
Step 2: Extraction of concepts related to nursing processes in a selected guideline
After reviewing the MM-guideline, concepts related to medication management nursing processes and associated elements of each process were extracted. Processes and their associated elements were tabulated in a table. For example, “Risk assessment” was identified as a nursing process with ten associated elements. A total of eight processes were extracted and validated by a nurse expert. Table 1 shows four examples of extracted nursing processes and their associated elements.
Table 1.
Four examples of nursing processes and associated elements extracted from a guideline
| Processes | Associated elements |
|---|---|
| Risk assessment | name, age, living condition, chronic diseases, psychiatric diagnoses, number of medication, medication dosing schedule, complex medication, number of prescribing providers, changes in medication regimen within 1 month |
| Medication reconciliation assessment | medication list, associated diagnosis, prescriber, dose, frequency, Beers criteria, adverse drug reaction, potential drug-drug reactions |
| Medication procurement assessment | difficulty obtaining or refilling prescriptions, viewing medications as too costly, funds to pay for medications or other financial burden, pharmacy delivery and/or refill reminder |
| Care plan | problems, interventions, expected outcomes |
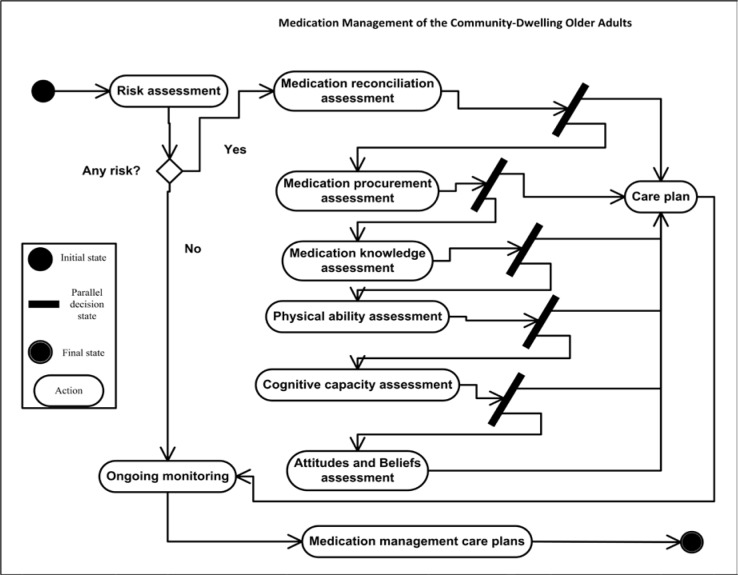
Step 3: Constructing an activity diagram
UML activity diagrams are typically used for computational and organizational processes modeling, for modeling the logic captured by use cases or scenarios, or for modeling the detailed logic of a processing rule. The activity diagram focuses on the action sequence of execution and the conditions that trigger or guard those actions. Activity diagrams are used for object-oriented software development while flow charts and data flow diagrams are used for structured software development24.
In order to create an activity diagram, actions and decisions are needed. All nursing processes in step 2 were identified as essential and necessary actions to manage medication for older adults. Then, any decision or parallel decisions which needed to be made were identified. Starting from an initial state symbol, actions were laid out in an order, and the flow from one action to another was represented using an arrow. The diagram ended with a final state symbol (Figure 1). Upon completion, a nurse expert, who specialized in community nursing with more than 10 years of research experience, validated the logical consistency of the activity diagram. Necessary revisions were made based on the nurse expert’s feedback. For instance, an assessment of each area of risk such as “Medication reconciliation” and “Medication procurement” was skipped algorithmically when there was no nursing problem identified in the first activity diagram. The nurse expert recommended that a nurse needed to assess all areas of risk even if there were no problems identified in the initial risk assessment. In the second activity diagram, this suggestion was incorporated.
Figure 1.
An activity diagram constructed for a web-based medication management DSS
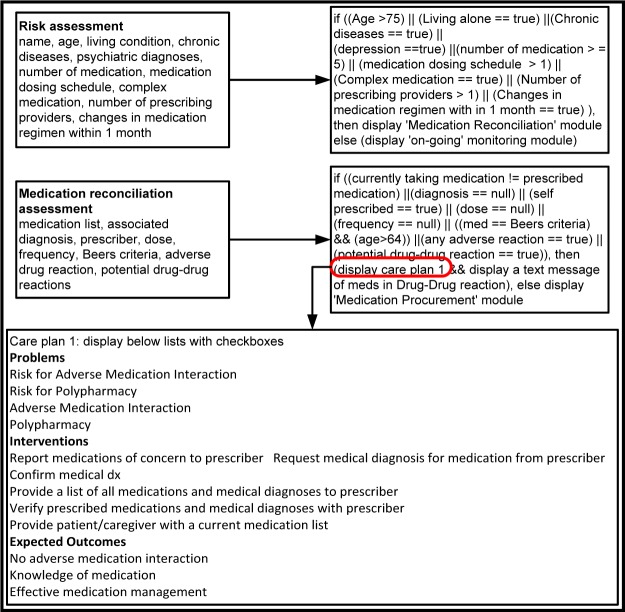
Step4: Construction of algorithms and mapping with ICNP
Algorithms are well-defined procedures and an essential part of any computer system25. They can be written in pseudocode in early software developmental stages to test logics. Psuedocode is simple English like language that allows basic entity relationships to be expressed in a concise format. It can be parsed to build software modules and be rendered to computer languages (i.e. Java, C++, or Ruby programming language, etc.).
After algorithms were constructed based on nursing processes and logics from step 2 and 3, pseudocodes for each nursing process were written. Figure 2 shows examples of pseudocodes written for a web-based medication management DSS. Total seven care plans were extracted from the MM-guideline and data items of problem, intervention and expected outcomes of all seven care plans were mapped with ICNP.
Figure 2.
Examples of algorithms constructed for a web-based medication management DSS
Step 5: Identifying software requirement specification
A software requirements specification is a comprehensive description of software under development. It describes what the software will do, how it will interact with end users, what the boundary of the software is and how it will be expected to perform. Purpose of this description is to minimizes the time, effort and cost required by developers to achieve desired goals for software users. In this study, guidelines from IEEE26 were used to describe the web- based medication management DSS.
For example, eight required functionalities were identified and written as:
Web-based medication management DSS shall display data entry screens for user.
Web-based medication management DSS shall allow user to select a patient.
Web-based medication management DSS shall allow user to enter new patient.
Web-based medication management DSS shall display screens with data entry tools such as checkboxes, dropdown menu, or text-field.
Web-based medication management DSS shall allow user to move screens forward and backward.
Web-based medication management DSS shall display nursing intervention list.
Web-based medication management DSS shall allow user select interventions from the list.
Web-based medication management DSS shall allow user to save identified risk factors and provided nursing interventions into database.
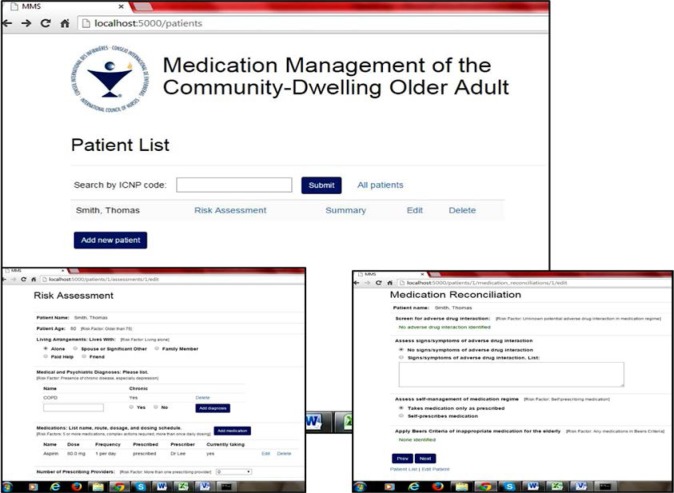
Step 6: A web-based medication management DSS
A web-based medication management DSS was programmed based on information from steps 1 to 5. Only two instances of clarification between team members and a programmer were needed. Once a prototype was programmed, team members performed alpha testing for a web-based medication management DSS. Three functions of a web-based system were not working correctly and were adjusted during alpha testing. Figure 3 shows the initial (middle), risk assessment (left lower) and Medication reconciliation assessment (right lower) screens of a developed system.
Figure 3.
First three screens of a web-based medication management DSS modeled with UML and ICNP (©copyright International Council of Nurses)
Discussion
Unified Modeling Language (UML) was developed to compose software and to assist the developer to model a computer system. Its descriptive nature describes a potential computer system accurately before implementation. For this reason, the UML was selected as the tool for modeling a guideline in this study. During the modeling processes, the UML was found to be a useful and sufficient tool to describe the Medication Management of the Community-Dwelling Older Adult guideline for a web-based system. It may be recommended that nurse informaticians utilize the UML when they model a nursing guideline for a decision support system for nurses’ use.
The UML has been used for modeling in many studies, but only one study27 has been reported in the nursing domain. Therefore, representing this nursing guideline with the UML is a significant first step in preparing nursing guidelines for implementation as decision support systems. Since there are limited computer systems for nurses’ use to date, the approach described may be useful in two ways: 1) it may facilitate interactions between a nursing informatician (on behalf of nurse users) and a developer to implement a computer system that nurses prefer; and 2) it may enable the maintenance of a model of a computer system that is easily modified for upgrades.
Limitations
The study findings have limited generalizability because the 1) UML modeling process was tested with only one guideline; 2) accuracy and completeness of translation of UML should be compared with those of other guideline modeling approaches (i.e. GLIF) and 3) the web-based medication management system was not tested with real patients’ data. Future research is necessary to develop decision support systems by following steps in this study with different guidelines and to test this system in community or public health nursing practice.
Acknowledgments
Authors acknowledge support for this study by the University of Wisconsin College of Nursing Harriet H. Werely Award and the International Council of Nurses.
References
- 1.Choi J, Currie L, Wang D, Bakken S. Encoding a clinical practice guideline using guideline interchange format: A case study of a depression screening and management guideline. International Journal of Medical Informatics. 2007;76S:S302–S307. doi: 10.1016/j.ijmedinf.2007.05.011. [DOI] [PubMed] [Google Scholar]
- 2.Peleg M, Shachak A, Wang D, Karnieli E. Using multi-perspective methodologies to study users’ interactions with the prototype front end of a guideline-based decision support system for diabetic foor care. International Journal of Medical Informatics. 2009;78:482–493. doi: 10.1016/j.ijmedinf.2009.02.008. [DOI] [PubMed] [Google Scholar]
- 3.CMS EHR Incentive Programs. 2015. [Accessed March 5, 2015]. https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/index.html?redirect=/EHRIncentivePrograms/30_Meaningful_Use.asp.
- 4.Anderson J, Willson P. Clinical Decision Support Systems in Nursing: Synthesis of the Science for Evidence-Based Practice. Computers, Informatics, Nursing. 2008;26(3):151–158. doi: 10.1097/01.NCN.0000304783.72811.8e. [DOI] [PubMed] [Google Scholar]
- 5.Bakken S, Currie LM, Lee NJ, Roberts WD, Collins SA, Cimino JJ. Integrating evidence into clinical information systems for nursing decision support. Int J Med Inform. 2008 Jun;77(6):413–420. doi: 10.1016/j.ijmedinf.2007.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Clercq PD, Kaiser K, Hasman A. Computer-interpretable Guideline Formalisms. Studies in Health Technology and Informatics. 2008;139:22–43. [PMC free article] [PubMed] [Google Scholar]
- 7.Peleg M. Computer-interpretable clinical guidelines: a methodological review. J Biomed Inform. 2013 Aug;46(4):744–763. doi: 10.1016/j.jbi.2013.06.009. [DOI] [PubMed] [Google Scholar]
- 8.Kamsu-Foguem B, Tchuenté-Foguem G, Foguem C. Using conceptual graphs for clinical guidelines representation and knowledge visualization. Information Systems Frontiers. 2012;16(4):571–589. [Google Scholar]
- 9.Aggarwal V. The Application of the Unified Modeling Language in Object-Oriented Analsys of Healthcare Information Systems. Journal of Medical Systems. 2002;26(5):383–397. doi: 10.1023/a:1016449031753. [DOI] [PubMed] [Google Scholar]
- 10.Ahmadian L, van Engen-Verheul M, Bakhshi-Raiez F, Peek N, Cornet R, de Keizer NF. The role of standardized data and terminological systems in computerized clinical decision support systems: literature review and survey. Int J Med Inform. 2011 Feb;80(2):81–93. doi: 10.1016/j.ijmedinf.2010.11.006. [DOI] [PubMed] [Google Scholar]
- 11.Kawamoto K, Del Fiol G, Lobach D, Jenders A. Standards for Scalable Clinical Decision Support: Need, Current and Emerging Standards, Gaps, and Proposal for Progress. The Open Medical Informatics Journal. 2010;4:235–244. doi: 10.2174/1874431101004010235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.OMG Introduction to OMG’s Unified Modeling Language™ (UML) 2013. [Accessed September, 2013]. http://www.omg.org/gettingstarted/what_is_uml.htm.
- 13.Booch G, Rumbaugh J, Jacobson I. The Unified Modeling Language User Guide. 6th. Reading, Massachusetts: Addison Wesley Longman Inc; 1999. [Google Scholar]
- 14.Coenen A. The International Classification for Nursing Practice (ICNP®) Programme: Advancing a Unifying Framework for Nursing. Online Journal of Issues in Nursing. 2003 Apr 3; [Google Scholar]
- 15.ICN International Classification for Nursing Practice (ICNP®) 2013. [Accessed March, 9, 2015]. http://www.icn.ch/what-we-do/international-classification-for-nursing-practice-icnpr/
- 16.Lewis A. Non-compliances: a $100 billion problem. The Remington Report. 1997 [Google Scholar]
- 17.Swanlund SL, Scherck KA, Metcalfe SA, Jesek-Hale SR. Keys to successful self-management of medications. Nursing science quarterly. 2008;21(3):238–246. doi: 10.1177/0894318408319276. [DOI] [PubMed] [Google Scholar]
- 18.Bowles KH, Dykes P, Demiris G. The use of health information technology to improve care and outcomes for older adults. Research in gerontological nursing. 2015 Jan-Feb;8(1):5–10. doi: 10.3928/19404921-20121222-01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Delaney C, Apostolidis B, Bartos S, Robbins R, Young AK. Pilot Testing of the Home Care Education, Assessment, Remote-Monitoring, and Therapeutic Activities Intervention. Home Health Care Management & Practice. 2014;26(4):205–216. [Google Scholar]
- 20.Kim SS, Kim EJ, Cheon JY, Chung SK, Moon S, Moon KH. The effectiveness of home-based individual tele-care intervention for stroke caregivers in South Korea. International Nursing Review. 2012;59:369–375. doi: 10.1111/j.1466-7657.2011.00967.x. [DOI] [PubMed] [Google Scholar]
- 21.CHAMP . Medication Management. VNSNY Center for Home Care Policy & Research; 2009. [Google Scholar]
- 22.Budnitz DS, Shehab N, Kegler SR, Richards CL. Medication Use Leading to Emergency Department Visits for Adverse Drug Events in Older Adults. Annals of Internal Medicine. 2007;147:755–765. doi: 10.7326/0003-4819-147-11-200712040-00006. [DOI] [PubMed] [Google Scholar]
- 23.Marek DK, Antle L. Medication Management of the Comminuty-Dwelling Older Adults. In: Hughes R, editor. Patient Safety and Quality: An Evidence-Based handbook for Nurses. Vol. 1. Rockville, MD: Agency for Healthcare Research and Qaulity; 2008. [PubMed] [Google Scholar]
- 24.Ambler S. Agile Modeling (AM) Home Page Effective Practices for Modeling and Documentation. 2013. [Accessed September, 2013]. http://www.agilemodeling.com/style/activityDiagram.htm.
- 25.Cormen TH, Leiserson CE, Rivest RL, Stein C. Introduction to Algorithms. 3rd. Cambridge, Massachusetts: The MIT Press; 2009. [Google Scholar]
- 26.IEEE . IEEE recommended practice for software requirements specifications. New York, NY: Institute of Electrical and Electronics Engineers; 1998. [Google Scholar]
- 27.Choi J, Choi JE. Representing Nursing Guideline with Unified Modeling Language to Facilitate Development of a Computer System: A Case Study. Studies in Health Technology and Informatics. 2014;201:181–187. [PubMed] [Google Scholar]