Abstract
Despite growing use of patient-facing technologies such as patient portals to address information needs for outpatients, we understand little about how patients manage information and use information technologies in an inpatient context. Based on hospital observations and responses to an online questionnaire from previously hospitalized patients and caregivers, we describe information workspace that patients have available to them in the hospital and the information items that patients and caregivers rate as important and difficult to access or manage while hospitalized. We found that patients and caregivers desired information—such as the plan of care and the schedule of activities—that is difficult to access as needed in a hospital setting. Within this study, we describe the various tools and approaches that patients and caregivers use to help monitor their care as well as illuminate gaps in information needs not typically captured by traditional patient portals.
Introduction
Hospitals are complex, dynamic, and information rich environments, yet patients and family members experience many information challenges when they are in this environment. Most hospitals have large, diverse care teams that must coordinate rapidly changing health data among providers. In addition, the information about the patient changes fairly quickly and the source of information is fragmented across hospitalists, nurses, surgeons, and different specialist services. When providing that information to patients, clinicians convey much of that information verbally and often quite rapidly. Yet, research shows that patients forget almost immediately 40–80% of what was said during a medical consultation1. Further compounding the issue, patients in the hospital are often severely ill, anxious, and stressed, which further decreases their ability to receive and process that information.
Although we know that providing outpatients with electronic information about their care can significantly improve their satisfaction with their care experience2, we know little of patient and family information needs in an inpatient context. Moreover, new initiatives to expand the role of patient portals and the pervasive presence of smart phones, tablets, and other electronic devices suggest a future where patients and families will be able to leverage real-time access to their care information while in the hospital. To explore this information space, we conducted in-hospital observations of patient-provider communication and used an online questionnaire to collect details about the experiences of patients and families. We provide a summary of the difficulty that patients and their caregivers face in obtaining and managing information while they are in the hospital and highlight information needs that are not typically a part of ambulatory patient portals. Our analysis illuminates opportunities to transform the hospital environment into an information workspace that supports greater patient and family engagement.
Background
The hospital environment creates unique challenges for patients and caregivers who are trying to access, manage and understand information about their care. We review related work that either examined the needs of patients and families in the hospital or analyzed the provision of patient-centered electronic access to medical record data.
Prior research has shown that patients perform extensive work to manage their health in the clinic3 as well as throughout their everyday lives4–6. In particular, the research suggests that patients and families are often engaged in background work, where “the workers themselves are quite visible, yet the work they perform is invisible or relegated to a background of expectation”7. In an inpatient context, patients and caregivers engage in activities to understand, organize, and manage information related to their care that is poorly understand and less visible to their care teams. Although new technologies exist to help outpatients with their work, within the hospital, patient access to information about their care is traditionally limited to verbal dialogue and occasionally to standardized, printed materials. The predominant non-verbal tool used to communicate with patients is the whiteboard, which is often used to provide information such as nurse and provider names, family contact information, and occasionally discharge expectations. Nonetheless, Marilyn Tan and colleagues found that whiteboards improved patient awareness of their care team and the goals for their care8. However, differences in use between different care providers and the difficulty in keeping the information up-to-date has constrained the effectiveness of whiteboards9. Moreover, whiteboards are tools primarily managed by nurses and their design reflects a provider-managed view of determining what patients should know.
Skeels and Tan posited that technology could help patients learn about their health and care while filling the significant amount of idle time that they experience during their stay10. Through inpatient interviews, the authors found that patients desired greater awareness of what was currently going on in relation to their care and more powerful and nuanced ways of communicating with their care team, families, and wider social network. In a pilot study by Weiland, et al., the authors demonstrated increased patient satisfaction and involvement in their care when cystic fibrosis patients were given a personalized schedule of their care11. Simply having enhanced information about the process of care delivery in the hospital improves the patient experience. A systematic review from Prey, et al. further highlights the value of technology to support patient engagement in an inpatient setting, but also acknowledges that this space is still in its infancy12. Prey and colleagues also conducted a field study where hospitalized patients were given printed copies of their raw medical record data—lab results, physician progress and consult notes, radiology reports, medication administration records—and found that even if patients did not understand all of the technical terms, they felt more informed and were able to “fact check” the information13. Patient-facing technologies in the inpatient environment can improve patient awareness and management of information about their care activities.
In an ambulatory and outpatient context, health systems increasingly give patients access to their medical information through patient portals. Although evidence of their impact is still lacking14, patient portals facilitate information exchange between patients and their providers and represent a larger movement to support patients in being more active participants in their care. The Open Notes project illustrates an enhanced approach to the traditional patient portal. Instead of providing a summary view of patient data and notes, Open Notes allows patients to have immediate access to the raw clinical notes created by providers as well as unfiltered access to imaging and laboratory data. In a pilot study of 19,000 patients across three institutions, most patients took time to log in and read their notes, and 99% indicated that they wanted to continue having access to their notes online15. Increasingly, these types of tools show promise for supporting patients to identify medical record errors16 and thereby mitigate possible safety risk, but their evaluation has centered primarily in environments outside the hospital.
Other researchers have sought to enhance access to information for hospitalized patients by migrating the patient portal concept to the inpatient environment17. Although limited to the emergency room environment, Wilcox and colleagues proposed a patient-facing, electronic, in-room display that would facilitate within-visit information sharing, encourage post-visit sharing and archiving, and serve as a useful memory aid as well as reference of the care delivered18. They further explored the value of providing information from the medical record to give patients insight into the background activities performed by health care staff that is normally invisible to the patient19. The same research group used the findings from this study to pilot a mobile-based process of care summary20. Researchers have also explored a tablet computer interface to either provide access to patient portal information or deliver educational content21,22. They found that patient awareness of their medication administration helped the patients assess their overall progress and health status23. Overall, this early work suggests that creating tools to provide automated summary information for patients is feasible and highly desired by patients and families.
As patient portals become pervasive, patients are likely to have information about their health care available electronically, even in the hospital. These related studies make a case for the role that technology can play in sharing care activities (1) to promote useful awareness among patients, (2) to support decision-making, and (3) to improve patient-provider communication. However, we do not know whether a traditional patient portal designed for long-term, ambulatory use will meet the needs of inpatients. To understand the unique information needs in an inpatient setting, we explore the information work currently being done by patients and families while they are in the hospital.
Methods
We used two methods to explore the information needs of hospitalized patients: (1) observations of patient-provider interaction points conducted at two hospital facilities; and (2) an online questionnaire completed by patients previously hospitalized and by family members or other caregivers that took care of a hospitalized patient. This work was approved by the authors’ institutional review board.
Observation Study
We conducted 118 hours of observations at a children’s hospital (Site 1) and an adult tertiary care hospital facility (Site 2). The observations occurred at different interaction points with patients: physician and multi-disciplinary rounding, discharge, care conferences, physical and occupational therapy sessions, as well as ad hoc exchanges among patients and the nursing staff. The observation findings were primarily based on open field notes and sketches of the patients’ environments. Our data reflects the perspective of care providers during their shift work, including hospitalist attending physicians, residents, specialist physicians, physical therapists, and direct nursing staff. In addition, we conducted in-room observations to observe communication and information flow from the patient’s perspective. Overall, we observed communication interactions with more than 50 individual patients. The observation notes were analyzed for factors that promoted patient information access, barriers that inhibited patient interaction during a hospital stay, and types of information managed by healthcare providers, patients, and caregivers. Our research team met regularly to review observation findings to identify preliminary themes and evaluate the extent of coverage of patient-provider communication during inpatient care.
Online Questionnaire
We also created an online questionnaire that asked participants about a prior hospital experience. Participants were recruited using convenience and snowball sampling through postings on social media sites, mailing lists, and website announcements. The questionnaire included topics across three areas: (1) importance and difficulty of receiving different types of information in the hospital, (2) approaches to managing information in the hospital, and (3) attitudes about care involvement and patient-provider communication. We received completed responses from 157 individuals from across the US and Canada who identified as being either a patient or a caregiver (e.g. family member) of a patient during a past hospitalization. We analyzed structured data from the questionnaire using descriptive summaries to identify general trends and patterns. Using an open coding technique and card sorting process24, we evaluated free text responses for related concepts and themes.
Sample population
Of 157 questionnaire responses, 61% self-identified as former patients and the remaining 39% identified as a caregiver who supported a patient during his or her hospitalization. Within the caregiver group, approximately 33% indicated they were a spouse of the hospitalized patient, 21% were parents, 21% were adult children caring for a parent in the hospital, and the remaining 25% were relatives or friends. The majority of the participants were female (75%) and ranged in age from 18 to 79. Fifty-eight percent indicated they were between the ages of 40 and 59. Respondents predominantly identified as white or Caucasian (87%). In addition, the survey participants tended to be highly educated, with 58% indicating that they have achieved some level of post-graduate education.
Forty percent (n=63) of the respondents had experienced a hospitalization within 12 months from the time they submitted the questionnaire, 23% were in the hospital between 1 and 3 years ago, and another 19% within 3 to 5 years. The reasons for the hospital admission were diverse. Many described an acute injury, while others mentioned pregnancy and various surgical procedures. Moreover, 33% of the participants described a hospital stay that lasted more than 7 days, another 29% were in the hospital between 2 and 4 days, 18% for 5 to 7 days, and the remaining 19% were hospitalized for 1 day or less. The majority of caregivers (84%) visited the patient in the hospital daily.
Results
Using mixed methods of an online questionnaire and in-hospital observations, we determined that patients and caregivers performed extensive background work to manage their information needs. To frame the context in which these stakeholders work, we begin with an overview of the patients room environment, characterized as an information workspace3. We follow these observations with an exploration of the patient’s experience receiving information based on provider workflow. By understanding the current state of information dissemination, we proceed to discuss the information gaps that patients and caregivers identified in the online questionnaire. The survey findings motivate our final observations regarding patient and caregiver work in using different tools to track information about their health.
The information workspace of a patient room
The patient’s hospital room serves as the primary focal point for information transfer among patients, caregivers, and clinical care providers. Typically, the design of the hospital room focuses on aesthetics, space for visitors, accessibility needs, support for monitoring equipment to address issues like risk of falling, noise25, and general patient satisfaction26. During our observations of patient, family, and care provider interactions in this environment, we found that different surfaces and spaces within the environment served as a means to organize, manage, and communicate care information. The design of the patient room in terms of how well the space supports information transfer is especially important considering the amount of idle time patients and caregivers experience while in the hospital.
Within the hospital rooms, we observed that patients have access to a variety of displays (Figure 1). TVs have the ability to display educational content, although that content is often standardized, rather than personalized to a patient’s situation; thus, the devices are primarily used for entertainment. Whiteboards provide a pseudo-dynamic space for patients to receive personalized information. They often have a structured layout with defined content areas for provider names, diet orders, frequency of vitals, and family contact information. Occasionally, pre-printed posters were used to display structured pathways that outlined the recovery from common surgeries like knee joint replacement. Importantly, the pathway diagrams were actionable, goal-oriented displays to assist patients in understanding the steps required before they could leave the hospital. We also observed temporary pieces of information taped above a bed or near the whiteboard that displayed instructions for nurses about patient-specific issues, such as not drawing blood from a particular arm. The displays that we observed were visible to patients and provided awareness about their care team, discharge criteria, and general care activities; however, the clinical care team primarily managed them.
Figure 1.
(a) A typical empty patient room at our study sites. (b) When the room was occupied, nearby surfaces were cluttered, leaving limited space for patients’ devices. Papers with information about their medical condition were often stacked by the window, and the whiteboard was located across the room from the bed.
Although hospital rooms have a variety of displays and surfaces to convey information to patients, we also observed challenges in being able to use these surfaces from the patient perspective. Patients had access to limited flat surface space and in-room computers frequently used by nurses were often positioned away from the bedside. We observed that the surface most accessible to the patient—a mobile tray table—was often covered with food, liquid containers, and trash that accumulate over the course of their stay. As a result, printed educational materials, notebooks, and the patients’ devices were often pushed into stacks in the corners of the room. Others described challenges with information scattered throughout a room: “Most of it I scrawled it on the back of some pamphlets that came out of a box of dressings because I didn’t have any paper. They did have a whiteboard in my room so I could keep track of some of it there, but some of it was embarrassing and I didn’t want it available to be read by anyone who walked in the room” (10466299). The whiteboard was rarely used by patients despite having a place for patient and family input. One caregiver described trying to use a whiteboard, “only later did we find out that it was only for staff and not for our questions for the doctor” (10276700). In our observations, many whiteboards were out of date and the information displayed was limited—typically listing only the names of care providers.
From the patient and caregiver perspective, visibility and access to information within the patient room was a challenging experience overall. To some extent, the shift to electronic systems compounds this problem because the “EMR eliminates ready review of what has been administered and when, etc. We learned to try and build good relationships with staff and were so happy when we had nursing staff that were kind, informative” (12878449). Rather than just review a paper medical chart at the bedside, the patient and their family had to develop a good relationship with their nurses to stay up-to-date on care activities. Ultimately, patient room design appeared to support provider information dissemination primarily and less so the patient’s ability to utilize objects and surfaces in the room as a workspace for accessing and managing information for his or her particular needs.
Staying informed through verbal dialogue: provider-centered access to information
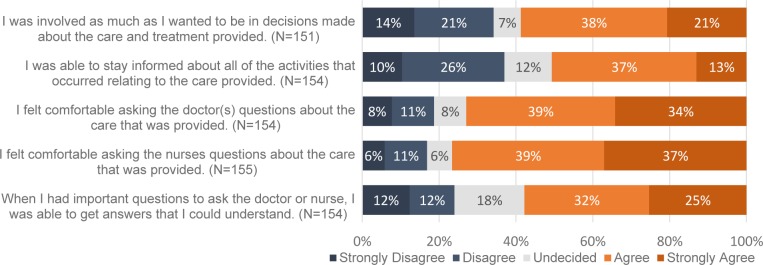
Not only are information displays in patient rooms set up primarily for provider use, but the way patients engage with information about their care is often through verbal dialogue driven by staff workflows. During rounding and other patient-provider interactions, we observed different challenges that can hinder patient and families ability to learn up-to-date information about their care. With the exception of using the call button, patients and caregivers often have to wait around for a provider to stop by in order to obtain updates about their care. Even within information exchanges like rounding and bedside handoffs, we observed providers referring to patients in the third person rather than directly engaging them in the conversation. The children’s hospital study site had instituted large, multidisciplinary rounds where more than a dozen providers crowded at the patient’s door and bedside. This large group creates an intimidating environment for young patients and caregivers to effectively communicate with their principal care team and to be involved in their care. Relatedly, participants in the survey were split in their agreement about being involved in decision-making (Figure 2). Fifty-nine percent agreed or strongly agreed, while 35% disagreed or strongly disagreed that they were as involved as they wanted to be. Over a third (37%) of those surveyed disagreed with the statement, “I was able to stay informed about all of the activities that occurred relating to the care provided”. Patients and caregivers appear to be very interested in being involved and staying informed but still experience communication barriers that inhibit their participation.
Figure 2.
Patient and caregiver attitudes about their involvement and communication during a hospitalization. Respondents expressed greater disagreement with statements relating to their involvement and staying informed.
We also observed providers employ strategies to mitigate some of the communication challenges and help to engage patients. While observing a patient being admitted at the children’s hospital site, the admitting staff member finished talking to the parent, turned to the child patient, and told him she would need to hear from him if he felt better or worse as they treat him. She told him he was a “full partner” in this. Moreover, physicians would utilize their mobile computers or print out materials to share radiology images at the bedside. During one observation, a patient did not understand the reason why he was having difficulty swallowing food. The physician brought a computer with a large screen over to the bedside and showed the patient along with the patient’s family the latest CT scan. Not only the patient, but the patient’s entire family crowded around the display and engaged in collaborative question and answer dialogue as the physician explained his interpretation of the data. Patients and families experienced successful information exchange when their providers utilized a partnership model to collaboratively explore medical record data. Based on the experiences of survey respondents and our observations, we found that effective tool use and collaborative dialogue helped to address some of the communication challenges created by provider workflows.
Gaps in information needs: prioritization of workflow and care activity data
Traditionally, patients access information in the hospital through verbal interactions with care providers and occasionally through standardized, printed content. We elicited a number of information needs prioritized by patients and observed patient-driven approaches to informal information exchange with peers in the hospital.
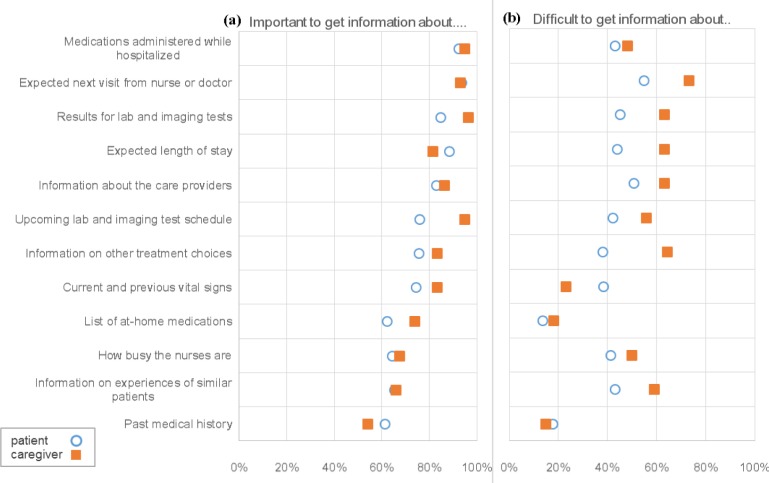
Survey respondents identified the top three most important pieces of information that they wanted to receive during their hospital stay as: (1) medications administered, (2) the expected next visit from a nurse or doctor, and (3) lab and imaging results (Figure 3). Being able to access information on past medical history and at-home medications was less important than the other items listed in the questionnaire. Overall, respondents tended to rate information about care process activities as most important. For example, information about the “expected next visit from a nurse or doctor,” was highly rated by participants and serves as a key communication point for patients to get updates. However, this information is also difficult for hospitals to provide because of unanticipated changes in physician schedules. When asked about challenges in accessing information, more than 50% of survey participants marked the expected next visit from their provider, information about their care team, and information about patients that have experienced similar health situations as somewhat difficult or very difficult to access. As one caregiver respondent described, “We spent a lot of time sitting around waiting for the doctors. Then we would go to the bathroom or to get food, and come back and they would have been there without speaking with any of us. We would have to wait another day to ask our questions or share information or observations” (10264109).
Figure 3.
Within the questionnaire, percentage of Caregivers (orange square) and Patients (blue circle) that evaluated accessing different types of information while in the hospital as “somewhat important” or “important”, shown on the left (a) and “somewhat difficult” or “very difficult”, shown on the right (b).
Another notable item from the questionnaire was that 66% of patients and caregivers ranked information about the experiences of similar patients as either important or somewhat important. Despite being ranked less important than other items in the questionnaire, our observations of instances where patients engaged with their peers in informal, social interactions demonstrated the potential value of this type of information. For example, we observed one patient engaging in a physical therapy (PT) session as part of her recovery from a double-knee replacement surgery. These PT sessions often took place in a dedicated gym-like space where multiple patients and physical therapists are present. Our observed patient expressed a lot of uncertainty and doubt about her ability to climb a set of stairs but her attitude shifted after watching another patient complete the activity immediately before her and found out they both had the same type of surgery on the same day. Seeing another patient with a similar condition successfully perform the exercise, the patient appeared more confident at attempting the stair climb and succeeded in completing the activity. We also observed patients exchanging information with neighboring patients while walking around their hospital floor. Although these interactions were limited and not explicitly supported by clinicians, we observed patients providing social support and occasionally sharing information about their care experiences.
The patients and caregivers in our online questionnaire prioritized activity data—actions that have happened recently like medication administration, future plans related to scheduled tests and provider visits—when asked what information was most important. Patients also obtained valuable support through social interactions. These types of information needs indicate a desire for data about the background work of care providers and other patients.
Patient and caregiver information work
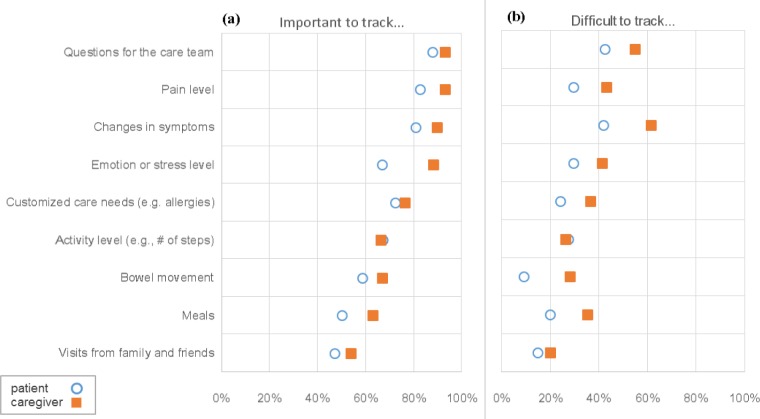
Based on observations and questionnaire results, patients and caregivers demonstrated active work to manage information about the care provided to them. When asked about items that they might track while in the hospital (Figure 4), survey respondents indicated that preparing questions for the care team was most important to them (90%). As one caregiver explained in the questionnaire, despite having “a robust care team…making sure we had a way to capture and communication our questions was essential” (10276700). However, their perspective on the challenge of keeping track of questions was more mixed; 47% indicated that it was either somewhat or very difficult to track. Keeping track of changes in symptoms, another item rated as important, was the most challenging item across the two groups to manage (50%). Other items, such as bowel movements or visits from family and friends, were marked as easier to track, but were less important. Overall, the importance of the items listed in Figure 4 suggests that patients and caregivers value the concept of tracking information about their personal health and care.
Figure 4.
Within the questionnaire, percentage of Caregivers (orange square) and Patients (blue circle) that evaluated tracking different types of information while in the hospital as “somewhat important” or “ important”, shown on the left (a) and “somewhat difficult” or “very difficult” on the right (b).
In the survey, participants listed diverse reasons for choosing to track information during their stay. The most cited reason was to help prepare and manage questions for the next visit from their health care provider. One participant prepared captured written notes, “So we wouldn’t forget our questions for the doctors, and so different members of the family could share information with each other or with the doctor or nurse when they arrived. We were never clear on when [the doctors and nurses] were coming by” (10264109). Others cited monitoring care quality as a reason for tracking. For one respondent, “The main reason I kept track was because of an error during surgery. So I knew I needed to keep a log because I wouldn’t remember all the events” (11740791). Another caregiver explained how, “We wrote down “in’s and outs” (nutritional intake and output) ourselves and then gave to the nurse at end of shift” because this “significantly increased accuracy for us to track the info ourselves” (10260629). Based on a prior event or because they believed their input was the most accurate source of data, patients and caregivers would actively record and share information with their care team.
The tools and methods used by patients and caregivers to track information about their health care varied widely. Of the respondents that stated they tracked information, almost half (49%) of these respondents used written notebooks or electronic data capture—often with a mobile phone—to document their care activities (Table 1). Some participants (18%) would keep track of things in the hospital through verbal interactions with their care team. These check-ins served as a way to reinforce what information needed to be remembered. For 5% of the respondents, they described relying on their caregivers to keep track of things for them. However, a substantial number of participants relied on their memory to keep track of things (19%). During our observations, even though many patients had a smartphone or similar device available to them, few used these devices to manage information related to their care. They served primarily as entertainment or external communication devices. We noticed that many of these devices were placed on a surface out of reach from the bedside or piled under papers and other items accumulated during the stay. The children’s hospital would actually provide patients with a tablet device during their stay, but even this was often pushed to corners of the room. Patients also had to cope with physical limitations because, “with IVs in your arm and/or hand, it was difficult to write or type” (10269740). Patients and caregivers experienced difficulty using different tracking tools because of the unique constraints related to their health maintenance and the physical space of the patient rooms. The usability of the various tools also affected their ability to capture information for tracking purposes and manage information for communicating with their care team.
Table 1.
Methods and rationale for tracking in the hospital coded from free-text survey responses (n=74).
| Tracking Method | % | Survey participant categories for motivation for tracking |
|---|---|---|
| Written logs and notes | 49% | Being an active participant; Monitoring care quality; Being in the know; Improving communication with staff; Personal accounting; Concerns about safety; Coping with health challenges (e.g. cognitive state); Provider requested; Dealing with too many different events occurring |
| Memory | 19% | Being an active participant; Monitoring care quality; Being in the know; Planning ahead; Being prepared for Q&A with staff; Sharing; Monitoring progress/recovery |
| Verbal reinforcement | 18% | Being an active participant; Monitoring care quality; Being in the know; Personal accounting; Provider requested tracking; Sharing; Post-hospital planning; Getting status updates |
| Electronic devices | 14% | Being in the know; Personal accounting; Being prepared for Q&A with staff; Medication monitoring; Concerns about safety, Sharing |
| Reliance on Caregiver | 5% | Monitoring care quality; Concerns about safety; Coping with health challenges (e.g. cognitive state); Improving communication with staff; Pain management |
Discussion
Through our observations and questionnaire, we found that patients often experience an information-poor environment outside of conversations with their care team. Our data illuminates patient barriers in using their hospital room as an information workspace, the difficulties that they experience in obtaining information outside of provider workflows, and their desire for information not normally displayed in the EMR or through patient portals.
Patient rooms reflect a provider-centered information workspace, despite being equipped to convey information to the patient through electronic interfaces and physical wall displays like whiteboards. For whiteboards in particular, we noticed incomplete and inconsistent usage throughout our observations that further reinforced the difficulties that patients experience in obtaining up-to-date information. Despite these challenges, the whiteboards and other displays occasionally served as useful places for physicians to diagram procedures or use visuals to help explain the patient’s condition and progress. The frequent presence of patient tools like smartphones and tablets suggest an opportunity to help patients organize all of the information collected over the course of a stay. Yet, these surfaces are frequently obscured by other objects or relegated to corners of the room away from the patient.
Within this physical environment, we found that the flow of communication is typically driven by provider workflows like rounding. Patients and caregivers experience communication challenges in this context because of the difficulty in being able to prepare for a visit that can occur at any moment. These interactions are also difficult because the information exchange is almost completely verbal and often time-constrained by the providers’ rounding schedules. In some instances, we observed providers enhance their approach to patient engagement by using collaborative behavior and electronic displays to discuss medical record data alongside the patients and caregivers. Increasing the use of visual tools at the patient’s bedside has the potential to enhance patient and caregiver participation in their care.
Finally, patients and caregivers expressed a variety of information and tracking needs related to their difficulty with managing their health information in the hospital. This extra patient and caregiver work was often motivated by concerns about care quality and wanting to stay informed when dealing with the care complexity of an inpatient environment. Accordingly, patients and caregivers indicated that information about their care team as being one of the most important and challenging pieces of information to manage. Our findings about tracking needs suggest that existing patient room displays and provider-driven information dissemination do not adequately support the patients’ and caregivers’ ability to use tools in their rooms and maintain awareness about their care activities. Moreover, the informal social interactions that we observed demonstrate that patients can obtain value through experiences of others. Reimagining the information workspace of a hospitalized patient should consider these needs and support opportunities for patient-driven care provider and peer interaction.
Addressing Information Needs
Providing enhanced access to information during a hospitalization can reduce the cognitive load for patients and improve common ground between the patient and their care team. The order that information is presented, modality, perceived importance, and health context can all have important impacts on the patient’s likelihood of remembering information. Something like a printed or electronic summary of the plan of care—upcoming activities, discharge goals, provider visit times, and other items highlighted by our questionnaire participants—creates an opportunity for patients to process activities related to their care on their own time. They can then reassess situations with their care providers to ensure their expectations match with the documented plan of care.
Hospitals are increasingly migrating their outpatient portal into the hospital environment as one approach to addressing the problem of patient access to information about their care. This is a positive first step, but our observations and questionnaire data show that a traditional portal doesn’t address most important information needs identified by participants, such as being able to know the plan of care and when to expect the next provider visit. The interest in information about care activities suggests that an inpatient-specific portal should reflect the dynamic nature of hospital care. There is an opportunity to capture the metadata contained within order sets and to explore approaches to communicating expectations for uncertain events like when the physician will be visiting the patient next. Leveraging the process of care data embedded in the electronic medical record provides an opportunity to reconsider the patient portal as a mechanism for maintaining awareness of changes and updates in a dynamic hospital environment.
Addressing Information Work
The patients and their caregivers that participated in our questionnaire developed various strategies for coping with the information communicated verbally in the hospital. In particular, even though our respondents stated that they felt comfortable with asking their care providers questions and rated keeping track of questions as the most important activity that they could do, they also stated that keeping track of changes was one of the most challenging activities during their hospitalization experiences. This relates to our observation data showing that patients face barriers to using tracking tools. In part, this is due to constraints created by the physical environment. We often observed tracking tools such as smartphone devices, notebooks, and even pieces of paper were relegated to areas of the room distant from the patient’s bedside. Even tablets, which are increasingly used to provide access to patient portals and health records, were often out of reach of the patient. The only tool consistently at the patient’s side was the call button which can alert a nurse if the patient has a question but lacks the ability to track information. Moreover, patients and caregivers in the survey expressed how they are able to track certain types of information about themselves more accurately than the care team that may not always be present in their room. Current conceptualizations of the patient portal typically do not address tracking needs. In fact, patients and caregivers are using tools when they are available and cite the lack of resources as a major barrier to being able to manage the large amount of information and activity occurring during a hospitalization.
Limitations
Our qualitative, ethnographic approach to studying the patient experience has several limitations, including that the questionnaire sample skews toward a well-educated demographic. However, even within this group, both patients and caregivers experienced challenges with obtaining access to key information about their care. Ultimately, the questionnaire is not intended to be a representative population sample, but instead provide a means to explore a broad range of patient and caregiver experiences across the US. We integrated the questionnaire findings with observation data from two independent hospital environments help to strengthen the validity of our findings.
Conclusion
The findings of our online questionnaire paired with inpatient observations show that inpatients face many information and communication challenges during their hospital stay. Analyzing the patient’s room as an information workspace in the hospital illustrated challenges and opportunities for tools and displays that can enhance patient interaction with their care information. Moreover, when we consider the patient portal functionality that is typically used in an outpatient setting as a strategy to mitigate some of these challenges, we found that inpatients need additional support within the hospital context. In particular, patients and caregivers highly desired yet found it quite challenging to obtain the patient’s plan of care for each day. In addition, most patients wanted to track key aspects of their experience. Neither of these important functionalities are available in patient portals but often exist as metadata within the patient’s medical record. Our work highlights these important needs and suggests new functionality that emerging inpatient information systems need to support. This type of new functionality has the potential to transform inpatient care by empowering these patients and caregivers with the information they need to have a satisfying care experience.
Acknowledgments
This project was supported by grant #1R01HS022894 from the Agency for Healthcare Research and Quality (AHRQ).
References
- 1.Kessels RPC. Patients’ memory for medical information. J R Soc Med. 2003 May;96(5):219–22. doi: 10.1258/jrsm.96.5.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Delbanco T, Walker J, Bell SK, Darer JD, Elmore JG, Farag N, et al. Inviting patients to read their doctors’ notes: A quasi-experimental study and a look ahead. Ann Intern Med. 2012;157:461–70. doi: 10.7326/0003-4819-157-7-201210020-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Unruh KT, Skeels M, Civan-Hartzler A, Pratt W. Proc ACM. New York: ACM Press; 2010. Transforming Clinic Environments into Information Workspaces for Patients; pp. 183–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pratt W, Unruh KT, Civan A, Skeels MM. Personal health information management. Commun ACM. 2006;49(1):51–5. Available from: http://cacm.acm.org/magazines/2006/1/6036/fulltext. [Google Scholar]
- 5.Moen A, Brennan PF. Health@Home: the work of health information management in the household (HIMH): implications for consumer health informatics (CHI) innovations. JAMIA. 2005;12(6):648–56. doi: 10.1197/jamia.M1758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Klasnja P, Civan-Hartzler A, Unruh KT, Pratt W. Blowing in the Wind: Unanchored Patient Information Work During Cancer Care Proc ACM CHI ’10. Atlanta, GA: ACM Press; 2010. pp. 1361–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Star SL, Strauss A. Layers of Silence, Arenas of Voice : The Ecology of Visible and Invisible Work. Comput Support Coop Work. 1999;8(1995):9–30. [Google Scholar]
- 8.Tan M, Hooper Evans K, Braddock CH, Shieh L. Patient whiteboards to improve patient-centred care in the hospital. Postgrad Med J. 2013;89(1056):604–9. doi: 10.1136/postgradmedj-2012-131296. [DOI] [PubMed] [Google Scholar]
- 9.Sehgal NL, Green A, Vidyarthi AR, Blegen Ma, Wachter RM. Patient whiteboards as a communication tool in the hospital setting: a survey of practices and recommendations. J Hosp Med. 2010;5(4):234–9. doi: 10.1002/jhm.638. [DOI] [PubMed] [Google Scholar]
- 10.Skeels M, Tan DS. Identifying opportunities for inpatient-centric technology; Proc ACM IHI ’10; New York, New York, USA: ACM Press; 2010. p. 580. [Google Scholar]
- 11.Weiland J, Schoettker PJ, Byczkowski T, Britto MT, Pandzik G, Kotagal UR. Individualized daily schedules for hospitalized adolescents with cystic fibrosis. J Pediatr Health Care. 2003;17(6):284–9. doi: 10.1016/s0891-5245(03)00109-3. [DOI] [PubMed] [Google Scholar]
- 12.Prey JE, Woollen J, Wilcox L, Sackeim AD, Hripcsak G, Bakken S, et al. Patient engagement in the inpatient setting: a systematic review. J Am Med Inform Assoc. 2014;21:742–50. doi: 10.1136/amiajnl-2013-002141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Prey JE, Restaino S, Vawdrey DK. AMIA Annu Symp Proc. Washington, DC; 2014. 2014. Providing Hospital Patients with Access to Their Medical Records; pp. 1884–93. [PMC free article] [PubMed] [Google Scholar]
- 14.Goldzweig CL, Orshansky G, Paige NM, Towfigh AA, Haggstrom DA, Miake-Lye I, et al. Electronic patient portals: Evidence on health outcomes, satisfaction, efficiency, and attitudes. Ann Intern Med. 2013;159(10):677–87. doi: 10.7326/0003-4819-159-10-201311190-00006. [DOI] [PubMed] [Google Scholar]
- 15.Walker J, Meltsner M, Delbanco T. US experience with doctors and patients sharing clinical notes. Bmj. 2015 Feb;350:g7785–g7785. doi: 10.1136/bmj.g7785. [DOI] [PubMed] [Google Scholar]
- 16.Hanauer Da, Preib R, Zheng K, Choi SW. Patient-initiated electronic health record amendment requests. J Am Med Inform Assoc. 2014;(2):1–10. doi: 10.1136/amiajnl-2013-002574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pell JM, Mancuso M, Limon S, Oman K, Lin C-T. Patient Access to Electronic Health Records During Hospitalization. JAMA Intern Med. 2015;2(14):2–4. doi: 10.1001/jamainternmed.2015.121. [DOI] [PubMed] [Google Scholar]
- 18.Wilcox L, Morris D, Tan D, Gatewood J. Designing patient-centric information displays for hospitals. In: Anttiroiko A-V, Mälkiä M, editors. Proc ACM CHI ’10; New York: ACM Press; 2010. p. 2123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wilcox L, Morris D, Tan D. Characterizing patient-friendly micro-explanationsof medical events; Proc ACM CHI ’11; New York: ACM Press; 2011. pp. 29–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pfeifer Vardoulakis L, Karlson A, Morris D, Smith G, Gatewood J, Tan D. Using mobile phones to present medical information to hospital patients; Proc ACM CHI ’12; New York: ACM Press; 2012. p. 1411. [Google Scholar]
- 21.Vawdrey DK, Wilcox LG, Collins SA, Bakken S, Feiner S, Boyer A, et al. A tablet computer application for patients to participate in their hospital care; AMIA Annu Symp Proc 2011; Washington DC. 2011. pp. 1428–35. [PMC free article] [PubMed] [Google Scholar]
- 22.Greysen SR, Khanna RR, Jacolbia R, Lee HM, Auerbach AD. Tablet computers for hospitalized patients: A pilot study to improve inpatient engagement. J Hosp Med. 2014 Feb 13;9:1–4. doi: 10.1002/jhm.2169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wilcox L, Feiner S, Liu A, Restaino S, Collins S, Vawdrey D. Designing inpatient technology to meet the medication information needs of cardiology patients; Proc ACM IHI ’12; New York: ACM Press; 2012. p. 831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Martin B, Hanington BM. Universal methods of design: 100 ways to research complex problems, develop innovative ideas, and design effective solutions. Rockport Publishers; 2012. [Google Scholar]
- 25.Cabrera IN, Lee MH. Reducing noise pollution in the hospital setting by establishing a department of sound: a survey of recent research on the effects of noise and music in health care. Prev Med (Baltim) 2000;30:339–45. doi: 10.1006/pmed.2000.0638. [DOI] [PubMed] [Google Scholar]
- 26.Harris PB, McBride G, Ross C, Curtis L. A place to heal: Environmental sources of satisfaction among hospital patients. J Appl Soc Psychol. 2002;32:1276–99. [Google Scholar]