Abstract
With the objective of increasing electronic death registration, Intermountain Healthcare and the Utah Office of Vital Records and Statistics have developed a system enabling death certification from within Intermountain’s electronic medical record (EMR), consisting of an EMR module and an HL7 interface. Comparison of post-intervention death certification at Intermountain Healthcare against a baseline study found a slight increase in the percentage of deaths certified electronically (73% pre vs. 77% post). Analysis of deaths certified using the EMR-module found that they were completed significantly sooner than those certified on paper or using the state’s web-based electronic death registration system (EDRS) (Mean time: Paper = 114.72 hours, EDRS = 81.84 hours, EMR = 43.92 hours; p < 0.0001). EMR-certified deaths also contained significantly more causes of deaths than either alternative method (Mean number of causes: Paper = 3.9 causes, EDRS = 4.0 causes, EMR = 5.5 causes; p < 0.0001).
Introduction
Death certificates are the primary source of death information throughout the United States. Each state maintains a central death registration system for deaths occurring in their state. As part of maintaining these registries, they institute systems to collect, validate, and archive death records. Frequently, funeral directors initiate the process of creating a new death certificate and then seek cause of death data from medical professionals, including physicians and medical examiners. A death certificate must be completed before a funeral director can proceed with the disposition (burial, cremation, etc.) of the decedent (deceased person).
Over recent years, a majority of state health departments have implemented web-based electronic death registration systems (EDRS) for the gathering and reporting of Death Certificate data.1 EDRS have several advantages over traditional paper-based systems. Electronic systems are more efficient than paper-based systems, producing higher quality data in a more timely manner.2 Paper-based systems require funeral directors to mail or hand-deliver partially completed death certificates to physician certifiers. Once completed, these paper death certificates need to be delivered, in person or by mail to local or state registrars for finalization, including typing the handwritten data into the state’s electronic death records. Electronic systems can reduce or eliminate travel costs incurred by funeral directors in tracking down physicians to complete a death certificate. It is also less likely that waiting for a physician to complete their portion of the certificate will cause delays in the disposition of a decedent. Further, entering data electronically reduces the risk of handwriting-related errors. Government registrars also save time and resources by not having to enter handwritten data into electronic databases.
In 2006, The Utah State Office of Vital Records & Statistics (OVRS) implemented and deployed an EDRS named the Electronic Death Entry Network (EDEN). Utah was the 13th state to deploy an EDRS. EDEN is available to funeral directors, physicians, and medical examiners, as well as health department officials via the World Wide Web. Using EDEN, they can enter and review data from anywhere with an Internet connection.
Problem
EDEN quickly gained nearly universal adoption among funeral directors, but was not as universally adopted among physicians. While nearly all of Utah’s funeral directors are registered users of the EDEN system, in 2010, only 591 of the nearly 5,000 Utah physicians were registered users of the EDEN system. As of March 2010, the funeral director’s portion of the death certificate was completed electronically in EDEN for virtually all death certificates. Conversely, the physician’s portion was being completed electronically for between 60% and 65% of death certificates.
It is not surprising that funeral directors have a higher EDRS adoption rate than physicians. Funeral directors have a vested interest in seeing an increase in the proportion of death certificates completed electronically. Most of the benefits gained by moving from paper death certificates to electronic death certificates accrue to funeral directors and government registrars. On the other hand, aside from the increased flexibility of being able to enter cause of death information without having to receive the paper copy, physicians do not have much to gain by switching to an electronic process. Completing a death certificate using the EDEN EDRS is more complicated for physicians than completing a paper death certificate. Physicians must set up an account on the EDRS in order to use EDEN, and then remember their login name and password in order to access it. The original EDEN user interface lacked clear instructions for novice users. All users, physicians and funeral directors alike were presented with the same screens for data entry, though each user type only needs to enter data into a subset of the available screens. It was not immediately clear to physicians how to complete their portion of the death record. From the physician’s perspective, completing a paper death certificate is much simpler. The confusion stemming from the extraneous (from the physician’s perspective) fields and screens in EDEN was one barrier to physician adoption of the EDEN EDRS.
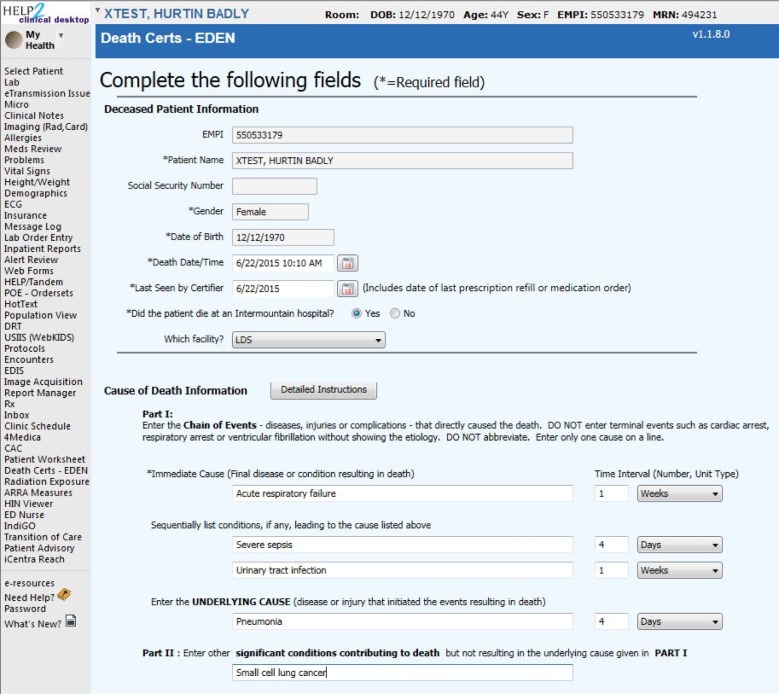
When a physician certifier chooses not to complete a death certificate electronically, the funeral director must “drop to paper” – print out the partially completed certificate and physically deliver it to the physician for completion (Figure 1). Utah state law requires that deaths be “certified” (cause of death information completed by a licensed provider) within 72 hours of a decedent’s death, and that the death be registered (meaning the death certificate has been fully completed), within 5 days of the time of death. During the first year and a half that EDEN was in operation, 61% of cause of death data entered electronically within the EDEN system was entered within 72 hours of the time of death. When the funeral director had to use the “drop to paper” option, only 34% were certified within 72 hours.
Figure 1.
Pre-intervention death certificate workflow. FD = Funeral Director. MD = Physician. LHD = Local Health Department.
Intermountain Healthcare (Intermountain) is a large integrated delivery network, centralized in the state of Utah, that provides care to approximately half the population of Utah.3 For death certification, Intermountain has seen EDRS adoption rates among its provider network similar to those seen statewide. During the period from January 2007 through October 2009, Intermountain physicians certified 39% of the 35,093 deaths registered in the state of Utah, 73% using the EDEN EDRS.
Many Intermountain physicians do use the EDEN EDRS for death registration. EDEN adoption rates are particularly high among physicians who complete a high number of death certificates. During the period examined, Intermountain physicians who completed an average of one or more death certificates per month used the EDEN system for 98% of the deaths they certified. This group of “high volume” death certifiers included only 3% of Intermountain physicians who completed at least one death certificate during that period, but accounted for 65% of all deaths certified by Intermountain physicians during that same period.
The vast majority of Intermountain physicians fell into the much larger group of “low volume” death certifiers, certifying less than one death per month on average. These physicians only used the EDEN system for 28% of the deaths that they certified. The large number of “low volume” certifiers collectively represents a “long tail” that accounted for 35% of death certificates completed by Intermountain physicians between January 2007 and October 2009, but only 13.5% of death certificates certified electronically (Table 1). Nearly three-fourths (74%) of the physicians who certified at least one death during the study period certified less than 1 death per year, and these “very low volume” certifiers were even less likely to use the EDEN system, completing only 12% of their death certificates electronically.
Table 1.
Use of EDRS by Intermountain physicians grouped by number of deaths certified per month; Baseline study – January 2007 to October 2009.
| Death certificates/month | % of all death certifiers | % of all death certificates | % certified electronically (EDEN EDRS) |
|---|---|---|---|
| <1 | 96.5% | 35.4% | 28.0% |
| 1–2 | 1.8% | 11.7% | 89.8% |
| 2–3 | 0.4% | 4.7% | 98.6% |
| 3–4 | 0.4% | 6.6% | 99.6% |
| 4–5 | 0.1% | 1.1% | 99.3% |
| >5 | 0.7% | 40.5% | 99.9% |
Solution
With the objective of increasing electronic death certification, OVRS applied for and received a grant from the Centers for Disease Control and Prevention (CDC) to implement an electronic cause of death interface between the EDEN system and the HELP2 electronic medical record (EMR) system in place at all Intermountain hospitals and clinics. Intermountain has a history of collaborating with the Utah Department of Health (UDOH), especially for electronic data exchanges.4–6 The development of this death certificate interface between Intermountain and UDOH is the first instance in the country of death certification done from within an EMR.
This system, that allows deaths to be certified from the EMR, consists of two key components: an EMR module that allows physician users to input the required cause of death data for death certification, and an HL7 interface that allows these data to be transmitted from the EMR to OVRS. Both of these components were developed following significant discussion and collaboration between technical, clinical, and administrative personnel at Intermountain and OVRS, as well as input from the Utah Funeral Directors Association.
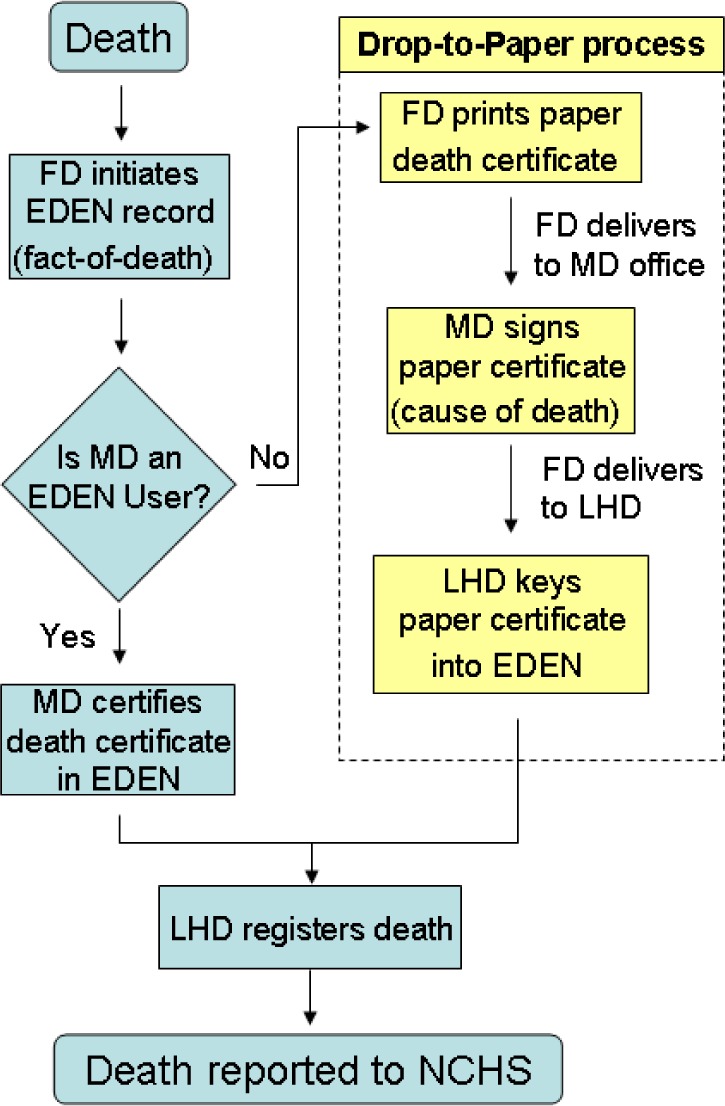
The user-facing EMR module was designed in a manner consistent with National Center for Health Statistics (NCHS) standards.7 The module allows providers to enter cause of death data for a decedent without needing to directly access the EDEN system, eliminating the need for them to remember a separate login and password. As this module was built specifically to be used by physician certifiers, it only includes data fields for the physician’s portion of the death certificate, eliminating some of the confusion physicians had experienced when using OVRS’s EDEN EDRS. (Figure 2)
Figure 2.
Demographics and Cause of Death sections of EMR-based death certificate module
In addition to simplifying and streamlining the physician certifiers’ data entry process, the new EMR module provides users with access to detailed instructions, produced by the CDC, for properly completing the cause of death section of the death certificate,8 to support especially those physicians who only certify deaths infrequently. Because the module is integrated into the EMR, it is able to automatically populate required demographic fields, including name, date of birth, gender, and social security number. Stored certifier user data is also automatically entered into the required fields for certifier name, license number, and mailing address. Another advantage of completing a death certificate from within the EMR is that certifiers can easily switch back and forth between the death certificate module and other portions of the decedent’s medical record (progress notes, laboratory data, medication history, etc.) to gather relevant data for completing the cause of death portion of the death certificate.
In order to transmit the cause of death data from Intermountain to OVRS, an HL7 interface for cause of death data was created. This HL7 interface supports three distinct types of messages: (1) an ADT^A04 (Patient registration) message is used when sending a new cause of death record to OVRS, (2) an ADT^A08 (Update patient information) message is used to send an update to an already submitted records, and (3) an ADT^A23 (Delete patient encounter) message is used to notify OVRS that a record was submitted in error and should be deleted. Delete messages do not trigger an automatic deletion of a record, as it was determined that personnel at OVRS would like to manually follow up on those instances before a cause of death record is deleted.
The initial HL7 messages were a version 2.4 format agreed upon by engineers at OVRS and Intermountain. As this project grew in national prominence, leaders at the National Center for Vital and Health Statistics (NCVHS) proposed that a standard HL7 message format be developed for use in sending death certificate records from EMRs to electronic vital records registration systems. That proposal led to the development of an HL7 draft standard for trial use that uses HL7 version 2.5.1 messages.9 Engineers at Intermountain and UDOH OVRS helped to define and vet this standard, and have updated our interface from the original version 2.4 messages to the new standard.
Once these data have been received, they are merged with the funeral director’s portion of the death certificate that continues to be entered into OVRS’s EDEN system. The demographic data in the physician’s portion of the record are compared against records created in EDEN by funeral directors. These demographic data include decedent name, social security number (if applicable), date of birth, gender, and date of death. If a match is found, the two records are merged. In the event of a non-perfect demographic match, records can be reviewed and a merge can be manually triggered by administrative staff at OVRS. OVRS staff report that approximately 40% of the records merge automatically, with the remaining 60% requiring the manual review step.
In addition to transmitting cause of death data to OVRS, Intermountain also stores a copy of the cause of death in the Intermountain Clinical Data Repository (CDR), fulfilling the Meaningful Use Core Measures requirement to record the “Date and preliminary cause of death in the event of mortality in the eligible hospital or CAH.”10
The new workflow associated with the EMR-based death certificate module is as follows: When a death occurs, the funeral director and physician can both complete their portions of the record independently and asynchronously, the funeral director using the EDEN EDRS, and the physician using the EMR module. When the funeral director has completed their portion of the record in EDEN, they can check to see if a physician has already completed their portion. If they have not, they contact the physician by telephone or e-mail as before. With the convenience of completing death certificates from within the EMR, some physicians routinely complete their portion of death certificates even before receiving notification from a funeral home. In that scenario, the funeral director now does not need to contact them, and can wait for the two portions of the record to be matched and merged. (Figure 3)
Figure 3.
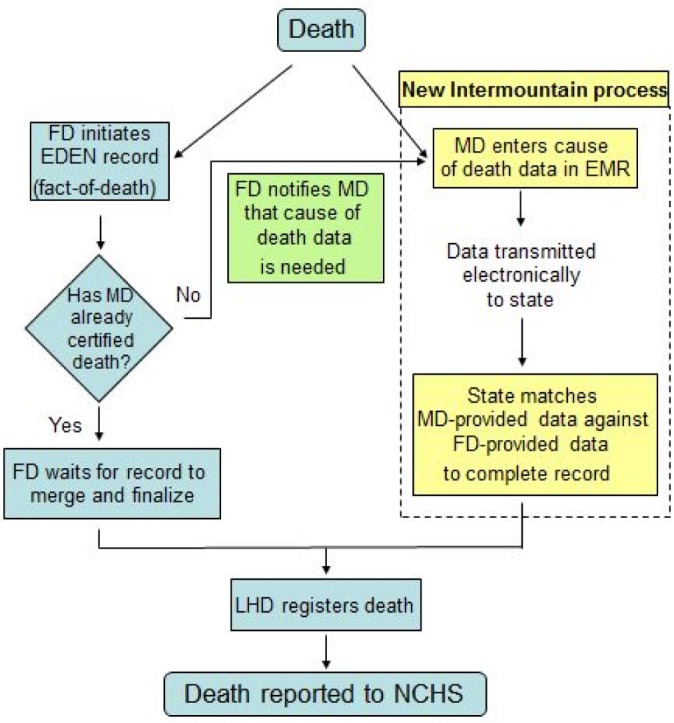
Post-intervention death certificate workflow with electronic interface from Intermountain EMR to EDEN EDRS. FD = Funeral Director. MD = Physician. LHD = Local Health Department.
Despite being fully developed by 2010, due to competing information systems priorities at Intermountain, the death certificate module in Intermountain’s HELP2 EMR only went into pilot production in March of 2011with pilot users at both inpatient and outpatient sites, and was not available broadly throughout Intermountain Healthcare until July 2013.
Methods
With the module finally available to most Intermountain physicians, we wanted to assess the impact of being able to complete death certificates from within the EMR. Data was gathered for all deaths occurring in 2014 that were registered in the state of Utah, and compared them against the baseline data for deaths occurring between January 2007 and October 2009.
As the EMR-based death certificate tool was only available to physicians affiliated or employed by Intermountain, we limited the analysis of these data to those providers. Presence of a certifier’s license number in Intermountain’s master service provider registry numbers was used as an indicator of whether or not a physician certifier would have been likely to have had access to the EMR-based death certificate module. Each death was classified according to the method by which it was certified, whether it was certified on paper (“Paper”), via direct use of the EDEN EDRS (“EDEN”), or by using the EMR death certificate module and associated HL7 interface (“EMR”).
We wanted to know whether the introduction of the EMR death certificate module would increase of the proportion of deaths certified electronically at Intermountain, and whether it would increase the percentage of “low volume” certifiers certifying deaths electronically, or simply result in certifiers who were already certifying deaths electronically switching from one electronic method (the EDEN EDRS) to another (the EMR-based death certificate module). To assess the impact of the EMR death certificate module on “low volume” certifiers, we looked at the proportion of deaths certified by each method within certifiers groups stratified by the number of deaths they certified in 2014.
To assess the impact of the EMR death certificate module on the “timeliness” of death certification and registration, we calculated what percentage of deaths certified by each method of death certification (“Paper”, “EDEN”, and “EMR”) was certified within 72 hours of the recorded time of death, together with average time of certification for each method. We also calculated the percentage of deaths certified by each of the three methods that was fully registered within the 5 days allowed under state statute, together with the average time of registration for records in each category.
Additionally, to assess whether having the death certificate certified from within the decedent’s medical record (in the EMR) aided certifiers in more completely describing the cause of death, we calculated the average number of ICD-10 codes assigned to each category of death certificates by coders at the National Center for Health Statistics (NCHS).
Results
In 2014, 17,267 deaths were registered with the Utah Department of Health’s Office of Vital Records and Statistics. Of these, 13,249 (77%) were certified by 1537 providers whose license numbers were in Intermountain Healthcare’s service provider registry. Of these 13,249 deaths, 3,051 (23.0%) were certified by 971 certifiers using the “drop-to-paper” method and 10,198 (77.0%) were certified electronically by 675 certifiers, either by using the EDEN EDRS system directly, or by using the EMR-based death certificate module. The77% certified electronically represents a statistically significant increase over the 73% done electronically in the period from January 2007 to October 2009 (p < 0.001, student’s t test). Of the 10,198 deaths certified electronically, 751 were completed by 181 certifiers using the EMR-based death certificate module, 7.4% of electronically-certified deaths, and 5.7% of all Intermountain-certified deaths in 2014.
Stratifying certifiers by the average number of deaths they certified each month (Table 2), we found that the increased proportion of records certified electronically in 2014 was almost entirely due to a nearly 20% increase in the proportion of records certified electronically by the “low volume” certifiers (those certifying less than 1 death per month). This increase included a 9.5% increase in deaths certified in the EDEN EDRS system, and 10% of deaths certified by this group of certifiers being certified using the now available EMR-based death certificate module. The majority of deaths certified by higher volume certifiers continued to be done electronically, though not quite at the near universal rate seen in the baseline analysis.
Table 2.
Comparison of death certification methods used, stratified by the frequency of deaths certified, for baseline (2007–2009) and post-intervention (2014) periods.
| Total Certifiers | Deaths Certified | % of all deaths | Paper | EDRS | EMR | ||
|---|---|---|---|---|---|---|---|
| <1 death/month | 2007–2009 | 1790 | 4840 | 35.4% | 72.0% | 28.0% | – |
| 2014 | 1315 | 3901 | 29.4% | 52.5% | 37.5% | 10.0% | |
| 1–2 deaths/month | 2007–2009 | 34 | 1603 | 11.7% | 10.2% | 89.8% | – |
| 2014 | 105 | 1770 | 13.4% | 26.3% | 66.1% | 7.6% | |
| 2–3 deaths/month | 2007–2009 | 8 | 644 | 4.7% | 1.4% | 98.6% | – |
| 2014 | 42 | 1187 | 9.0% | 10.5% | 76.8% | 12.8% | |
| 3–4 deaths/month | 2007–2009 | 8 | 907 | 6.6% | 0.4% | 99.6% | – |
| 2014 | 20 | 821 | 6.2% | 13.5% | 79.1% | 7.4% | |
| 4–5 deaths/month | 2007–2009 | 1 | 148 | 1.1% | 0.7% | 99.3% | – |
| 2014 | 17 | 887 | 6.7% | 19.1% | 80.4% | 0.6% | |
| >5 deaths/month | 2007–2009 | 13 | 5546 | 40.5% | 0.1% | 99.9% | – |
| 2014 | 38 | 4683 | 35.4% | 2.8% | 97.0% | 0.2% | |
| Cumulative totals | 2007–2009 | 1854 | 13688 | 100% | 26.8% | 73.2% | – |
| 2014 | 1537 | 13249 | 100% | 23.0% | 71.3% | 5.7% |
On average, deaths certified on paper took 4.78 days from the time of death until the time of certification, with 35.5% being certified within the state-mandated 72 hours. Deaths certified via the EDEN EDRS took an average of 3.41 days, with 56.6% certified within 72 hours of death. Deaths certified via the EMR-based death certificate module took an average of 1.83 days, with 77.5% certified within 72 hours of death. (Table 3)
Table 3.
Comparison of timeliness of certification (completion of the physician’s portion of the record) and registration (full completion of the record), as grouped by method of certification. *= p-values calculated using student’s t test.
| Paper | EDRS | EMR | p-value* (Paper vs. EDRS) | p-value* (EDRS vs. EMR) | |
|---|---|---|---|---|---|
| Average hours from death to certification | 114.72 | 81.84 | 43.92 | <0.0001 | <0.0001 |
| Percentage certified within 72 hours | 35.5% | 56.6% | 77.5% | ||
| Average days from death to registration | 5.38 | 4.55 | 4.18 | <0.0001 | 0.0086 |
| Percentage registered within 5 days | 58.5% | 68.6% | 74.7% |
Death registration (full completion of the death certificate) for deaths certified on paper took an average of 5.38 days, with 58.5% being fully registered within the 5 days specified by state law. Deaths certified in the EDEN EDRS were registered, on average, 4.55 days after the death, with 68.6% being registered within the mandated 5 day period. Deaths certified in the EMR-based death certificate module were registered in an average of 4.18 days from the time of death, with 74.7% being fully registered within 5 days. Deaths certified via the EMR-based death certificate module were certified significantly sooner than those done using the EDEN EDRS (p < 0.0001, student’s t test). Deaths certified in the EMR were also registered significantly sooner than those certified using the EDEN EDRS (p = 0.0086, student’s t test). (Table 3)
The average number of ICD-10 coded causes of death assigned by NCHS coders to deaths certified on paper was 3.9. The average number of coded causes of death assigned to deaths certified via the EDEN EDRS was 4.0. The average number of coded causes of death assigned to deaths certified using the EMR-based death certificate module was 5.5. The difference between number of coded causes of death for the paper-certified and EDRS-certified deaths was not statistically significant (p = 0.2049, student’s t test), but the difference between the number of coded causes of death for the EMR-certified deaths was significantly higher than both paper-certified deaths (p < 0.0001, student’s t test) and EDRS-certified deaths (p < 0.0001, student’s t test).
Discussion
In the period between 2009 and 2014, the percentage of deaths certified electronically at Intermountain Healthcare increased from 73% to 77%. This increase was statistically significant, but relatively modest in size, still requiring funeral homes to hand deliver nearly 1 of every 4 death certificates to physicians for certification.
The increase in the overall percentage of deaths certified electronically corresponds with increased electronic certification among certifiers who certified less than 1 death certificate per month. All other strata actually saw a decrease in the percentage of deaths certified electronically, as compared with the baseline study, but because the “low volume” certifiers certify such a large percentage of deaths, the increase in electronic certification in that stratum of certification was enough to increase the overall percentage of deaths certified electronically.
The introduction of a death certificate module within Intermountain’s HELP2 EMR may have contributed a small amount to that increase, especially considering that the increased percentage of deaths certified electronically by “low volume” certifiers was shared about equally between the state’s EDRS and Intermountain’s EMR-based module. However, to date, adoption of the EMR-based death certificate module by Intermountain physicians has been relatively low. Only about 12% of Intermountain certifiers used the EMR-based module to complete at least one death certificate.
We examined the mode of death certification in frequency-based strata because of our hypothesis that the EMR-based module might be more user-friendly for providers who only certify death rarely. However, in light of the fact that the number of providers in most of the frequency-based strata changed significantly between the times of the two samples, it is difficult to attribute much of the changes between the sample periods to changes in behavior by individual providers. In the post-implementation sample, all but the lowest volume stratum had many more certifiers than in the pre-implementation sample, so changes in mode of certification in each stratum are more likely to have come from the behavior of different physicians being in those strata than to have come from a change in behavior by individual physicians. For example, in the “high volume” stratum, the percentage of deaths certified on paper increased from 0.1% to 2.8%, but the number of certifiers increased from 13 to 38. It seems more likely that the increase of paper-based certification is due to a few more physicians who typically certify deaths on paper certifying more than five deaths per month in 2014, than it is due to physicians who previously certified deaths electronically switching back to certifying them on paper.
In each of the frequency-based strata, the EDEN EDRS was used more frequently for death certification than the EMR-based module. The EMR-based module was used most frequently by certifiers completing 4 or fewer death certificates each month. In the “high volume” stratum, certifiers used the EDEN EDRS almost exclusively when certifying deaths electronically. The “high volume” certifiers were already certifying nearly all of their deaths using the EDRS prior to the implementation of the EMR-based option, and perhaps the benefits of the EDRS outweigh those of the EMR-based option for high volume certifiers.
The web-based EDEN system can be used anywhere that a browser is available, while the EMR-based death certificate module requires the installation of a bit of software on each computer where it is to be used. This generally limits use of the EMR-based module to only those computers in Intermountain hospitals and clinics. Additionally, during the time this study was done, OVRS introduced a physician-specific portal for the EDEN system (EDEN MD) that simplifies and streamlines the physician’s part of the process, a significant improvement over the original EDEN system. Additionally, use of the EMR death certificate module has not been mandated at Intermountain, and while most physician certifiers have access it, they may not be aware of its availability. Going forward, efforts could be made to advertise the module’s existence, highlighting some of its conveniences. The small, but not insignificant, rate of the module’s use among low volume certifiers shows some promise that further growth could be seen among that group.
It should not be surprising that deaths certified electronically are both certified and registered significantly sooner than deaths certified on paper, but it is interesting that deaths certified using the EMR-based module are certified and registered significantly sooner than those completed using the state’s web-based EDRS. While it is possible that the early adopters of the EMR-based module are inherently more likely to complete deaths sooner than other certifiers, there are several factors that contribute to the increased timeliness of the EMR-certified deaths. First, the certifiers use the EMR regularly as part of their daily medical practice, and often complete other clinical notes related to a patient’s death. A physician completing other clinical documentation on a patient death can simply click over to the death certificate module and certify the death as well. Additionally, certifiers using the EDRS must first wait for a funeral home to begin a death record and then notify them that it is ready for them to certify. This notification may not come at a time when it is convenient for the certifier to log into the EDRS and complete the record, increasing the length of time before the death is certified and ultimately registered.
In addition to being completed significantly sooner than EDRS-certified deaths, the EMR-certified deaths contained significantly more information, as represented by the number of causes of death reported, than either EDRS-certified or paper-certified deaths. Certifiers using the EMR-based module can click back and forth between the death certificate module, and other EMR modules, including clinical notes, lab results, vital signs, etc. One physician reported that, when completing a death certificate within the EMR, he often reviews a patient’s history & physical (H&P) note, and the death summary note to better understand the chain of events leading up to a patient’s death. Further analysis is needed to determine whether the increased number of causes of death in the EMR-certified records can be attributed to having convenient access to the decedent’s medical record, but it seems likely that this would at least contribute to the increase in information reported.
It should be noted that this was not a randomized trial of the EMR-based death certificate module, and physician certifiers were at liberty to use or not use the module as they chose, so there is a possibility of selection bias. It may be that those physicians who choose to use the EMR-based module over the state’s EDRS or paper are more likely than other physicians to complete their death certificates quickly, and include more causes of death.
As mentioned above, one outcome of this work has been the creation of an HL7 Draft Standard for Trial Use for death reporting, specifically designed for the transmission of death certification records from an EMR to an EDRS. That standard has been implemented in the interface between Intermountain Healthcare and the Utah Department of Health’s Office of Vital Records and Statistics. Intermountain is currently transitioning from a set of home-grown EMR applications to a widely used commercially-vended EMR system. As part of that transition, the vender has added a form for death certification to their EMR. This EMR is now in place at a few facilities, and records entered into its death certificate form are subsequently formatted using the HL7 Draft Standard and transmitted to the EDEN EDRS, using the same interface used for death certifications coming from the HELP2 EMR. Other customers of this commercial EMR could potentially use this same death certificate form and message format to send death record electronically to a government-run EDRS. While Utah’s EDEN system is currently the only EDRS supporting this standard, its implementation in one of the more widely used commercial EMR means that other healthcare organizations that use that EMR could potentially begin certification of deaths from within an EMR. These steps open the door to the standard’s implementation in other EDRS, and the possibility of more widespread EMR-based death certification.
Future Directions
Going forward, there are a variety of enhancements that could be made to the EMR-based death certificate module to increase its utility. Plans for future versions of the module include presenting relevant data (labs, progress notes, etc.) to the end user within the module itself, eliminating the need for switching between modules. There continue to be concerns about the accuracy of death certificates11, 12, and another possible enhancement to the EMR-based module would be to develop decision support logic that uses existing patient data to make suggestions of conditions that ought to be considered among the causes of death. Additionally, enhancements to the communication aspect of this system could be made, including supporting the capability of funeral directors to trigger death certificate requests to Intermountain physicians via the EMR’s secure internal messaging system.
Conclusions
The partnership between Intermountain Healthcare and the Utah Office of Vital Records and Statistics succeeded in implementing the first ever EMR-EDRS interface for electronic death certification. To date, the EMR-based death certificate module has had limited adoption among Intermountain certifiers, primarily among users certifying 4 or fewer deaths per month. Still, it may have had a modest impact on the significant increase in electronic death certification at Intermountain Healthcare. Deaths certified using this module were completed significantly sooner than deaths certified using the state’s electronic death registration system, and included significant more causes of death, so there is strong incentive to work to increase the use of this method, both within Intermountain Healthcare, and at other sites in Utah, and in other states.
References
- 1.National Association for Public Health Statistics and Information Systems Electronic Death Registration Systems, By Jurisdiction. [Accessed: 24 Feb 2015]. Available from: https://naphsis-web.sharepoint.com/about/Documents/EDRSDevelopmentMapNov2014pptx.
- 2.National Association for Public Health Statistics and Information Systems Electronic Death Registration Systems Overview Presentation. [Accessed: 24 Feb 2015]. Available from: https://naphsis-web.sharepoint.com/about/Documents/Pan_Flu_Conference_Call.ppt.
- 3.Clayton PD, Narus SP, Huff SM, et al. Building a comprehensive clinical information system from components. The approach at Intermountain Health Care. Methods Inf Med. 2003;42(1):1–7. [PubMed] [Google Scholar]
- 4.Kfoury AG, French TK, Horne BD, et al. Incremental survival benefit with adherence to standardized heart failure core measures: a performance evaluation study of 2958 patients. J Card Fail. 2008 Mar;14(2):95–102. doi: 10.1016/j.cardfail.2007.10.011. [DOI] [PubMed] [Google Scholar]
- 5.Lappe JM, Muhlestein JB, Lappe DL, et al. Improvements in 1-year cardiovascular clinical outcomes associated with a hospital-based discharge medication program. Ann Intern Med. 2004 Sep 21;141(6):446–53. doi: 10.7326/0003-4819-141-6-200409210-00010. [DOI] [PubMed] [Google Scholar]
- 6.Rajeev D, Staes CJ, Evans RS, et al. Development of an electronic public health case report using HL7 v2.5 to meet public health needs. J Am Med Inform Assoc. Jan-Feb;17(1):34–41. doi: 10.1197/jamia.M3299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National Center for Health Statistics Specifications for Collecting and Editing the United States Standard Certificates of Birth and Death – 2003 Revision. [Accessed: 24 Feb 2015]. Available from: http://www.cdc.gov/nchs/data/dvs/Guidelinesbirthspecs1101acc.pdf.
- 8.Centers for Disease Control and Prevention Instructions for Completing the Cause-of-Death Section of the Death Certificate. [Accessed: 24 Feb 2015]. Available from: http://cdc.gov/nchs/data/dvs/blue_form.pdf.
- 9.Health Level Seven International HL7 Version 2.5.1 Implementation Guide: Vital Records Death Reporting, Release 1 (US Realm), DSTU Release 1.1. [Accessed: 24 Feb 2015]. Available from: http://www.hl7.org/implement/standards/product_brief.cfm?product_id=209.
- 10.Centers for Medicaid and Medicare Services Eligible Hospital and Critical Access Hospital Meaningful Use Core Measures, Measure 6 of 11, Stage 1(2014 Definition) [Accessed: 24 Feb 2015]. Available from: http://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/downloads/6_Record_Demographics.pdf.
- 11.Ives DG, Samuel P, Psaty BM, Kuller LH. Agreement between nosologist and cardiovascular health study review of deaths: implications of coding differences. J Am Geriatr Soc. 2009 Jan;57(1):133–9. doi: 10.1111/j.1532-5415.2008.02056.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ravakhah K. Death certificates are not reliable: revivification of the autopsy. South Med J. 2006 Jul;99(7):728–33. doi: 10.1097/01.smj.0000224337.77074.57. [DOI] [PubMed] [Google Scholar]