Abstract
Background:
Scapular dyskinesis, or abnormal dynamic scapular control, is a condition that is commonly associated with shoulder pathology but is also present in asymptomatic individuals. Literature varies on whether it represents a cause or symptom of shoulder pathology, but it is believed to be a risk factor for further injury. Clinical identification focuses on visual observation and examination maneuvers. Treatment of altered scapular motion has been shown to improve shoulder symptoms. It is thought to be more common in overhead athletes due to their reliance on unilateral upper extremity function but the incidence within nonoverhead athletes is unknown.
Hypothesis:
Overhead athletes will have a greater prevalence of scapular dyskinesis when compared with nonoverhead athletes.
Study Design:
Systematic review; Level of evidence, 3.
Methods:
After PROSPERO registration, a systematic review was performed using PRISMA guidelines through the PubMed database looking for studies published before October 2014. All studies containing the search terms scapular, scapulothoracic, dyskinesis, dyskinesia, shoulder athlete, or overhead athlete were included. Studies that did not include prevalence data for scapular dyskinesis were excluded. Study methodological quality was evaluated using the modified Coleman methodology score. Descriptive statistics and 2-proportion 2-tailed z-tests were used to compare the reported prevalence of scapular dyskinesis between overhead and nonoverhead athletes.
Results:
Twelve studies were analyzed including 1401 athletes (1257 overhead and 144 nonoverhead; mean age, 24.4 ± 7.1 years; 78% men). All the studies were evidence level 2 (33%) or level 3 (67%). The reported prevalence of scapular dyskinesis was significantly (P < .0001) higher in overhead athletes (61%) compared with nonoverhead athletes (33%).
Conclusion:
Scapular dyskinesis was found to have a greater reported prevalence (61%) in overhead athletes compared with nonoverhead athletes (33%).
Clinical Relevance:
Prevalence data for scapular dyskinesis are scarce within the literature. Information on the reported prevalence, laterality, and association with the dominant extremity will allow for better allocation of diagnostic and therapeutic interventions. Recognition and treatment will help athletes to optimize functional performance and decrease the risk of further shoulder injury.
Keywords: scapula, scapular dyskinesis, scapular dyskinesia, overhead, athlete, shoulder, scapulohumeral rhythm, prevalence
Scapular dyskinesis, or alterations in dynamic scapular control, is present in as many as 67% to 100% of athletes with shoulder injuries.26 However, it is also present in many asymptomatic individuals.26 Alterations in scapular motion can be caused by fatigue, neurologic dysfunction (eg, long thoracic, accessory, or dorsal scapular nerve palsies), or inhibition by intra-articular glenohumeral or subacromial processes (eg, subacromial impingement, rotator cuff pathology, internal impingement, labral injury, glenohumeral instability, glenohumeral arthritis, and adhesive capsulitis).1,3,5,9,12,23–25,30,33 The association between scapular dyskinesis and shoulder pathology is uncertain—whether it represents a cause or effect of the pathology.2,9,22 Prior studies have shown altered scapular movements to be detrimental to shoulder function.6,31 Additionally, improvement or correction of abnormal scapular mechanics can decrease the symptoms associated with shoulder pathology (eg, full-thickness rotator cuff tears).6
Clinical identification of scapular dyskinesis is difficult and relies primarily on visual observation.31 Kibler et al10,13,14 described the most well-known classification technique, which has been subsequently modified to include weighted exercises, videotaping for further review by investigators, inclinometry, and tape measurements.7,28 Scapular dyskinesis is believed to be more common in overhead or throwing athletes due to their heavy reliance on unilateral upper extremity function.31 During throwing, the glenohumeral and scapular joint experience increased stress as they act as the “funnel” or bridge that transfers power from the lower extremities and trunk to the arm.3,8,10,11,22 Alterations in this transfer of power lead to increased stress on the glenohumeral and scapular-thoracic joints, thus increasing the theoretical risk of injury.3,30 However, there is scarce literature on the reported prevalence of scapular dyskinesis in both overhead and nonoverhead athletes.
Our goal was to perform a systematic review to identify and compare the reported prevalence of scapular dyskinesis in overhead and nonoverhead athletes. Our hypothesis was that overhead athletes would demonstrate a significantly greater reported prevalence of scapular dyskinesis when compared with nonoverhead athletes.
Methods
Identification and Selection of Literature
This systematic review was registered with the International Prospective Register of Systematic Reviews (PROSPERO) on September 10, 2014 (registration number, CRD42014010573). It was conducted and reported using the protocol described by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).20 The search was performed by 2 of the authors (M.B.B., J.D.H.) using the PubMed database between September 10 and 13, 2014, with the following search terms: “scapular dyskinesis OR scapular dyskinesia OR scapulothoracic dyskinesis OR scapulothoracic dyskinesia OR scapulohumeral rhythm OR Shoulder athlete OR overhead athlete.” All titles and abstracts from the search results were screened while identifying relevant articles by applying the inclusion and exclusion criteria (Figure 1). If an article met the criteria or if insufficient information was provided from the abstract to make a decision, the full-text was obtained.
Figure 1.
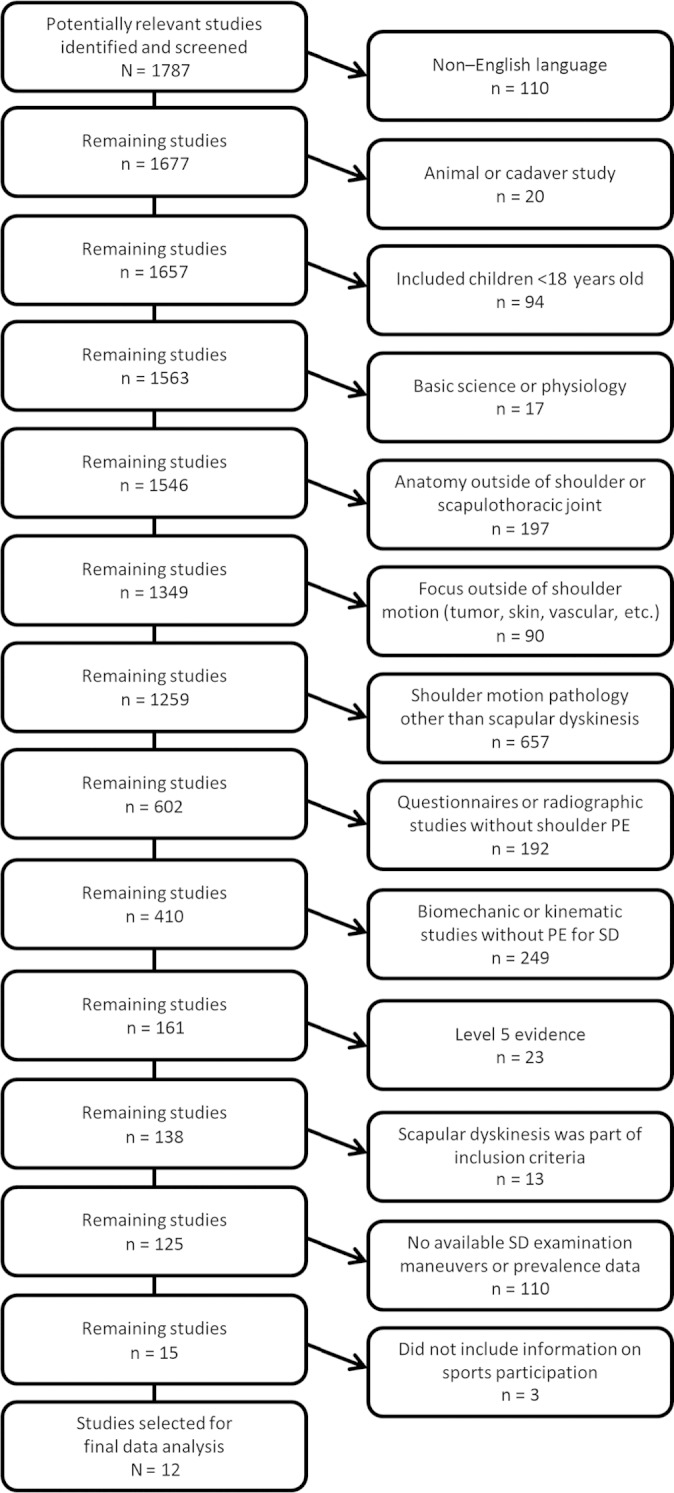
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flowchart illustrating application of exclusion criteria to determine the final number of studies analyzed in this systematic review. PE, physical examination; SD, scapular dyskinesis.
Selection Criteria
An article was included in the final analysis if it met the inclusion criteria of a clinical study reporting the prevalence of scapular dyskinesis in athletes (Figure 1). Articles were excluded if they: (1) were not written in the English language, (2) were animal or cadaver (rather than human) studies, (3) involved children younger than 18 years, (4) focused on basic science or physiology (rather than clinical parameters), (5) focused on anatomic regions outside of the shoulder or scapulothoracic articulation (hand, wrist, elbow, spine, lower extremities, etc), (6) focused on processes outside of shoulder motion (tumors, skin, vascular, etc), (7) focused on questionnaires or radiographic studies without patient examination, (8) were biomechanic or kinematic studies that lacked physical examination specifically for scapular dyskinesis, (9) discussed scapular dyskinesis only briefly without clinical measures, (10) constituted level 5 evidence, (11) included only patients with scapular dyskinesis prohibiting prevalence calculations, (12) focused on scapular dyskinesis and utilized clinical examination but did not contain prevalence or incidence data, or (13) did not include information on athletic participation.
Quality Assessment/Data Extraction
Each article was independently assessed by the 2 authors (M.B.B., J.D.H.) without blinding for each article’s identifiers, such as author names, institutions, journals, and so on. Each reviewer computed an individual modified Coleman methodology scores (MCMS) for each article. This scoring system involves 15 components for a scaled total of 96 points, but, due to the nature of the included diagnostic studies, we further modified it to remove (1) outcome assessment (0-6 points), (2) cointerventions (0-6 points), (3) description of rehabilitation protocol (0-4 points), (4) clinical effect measurement (0-6 points), and (5) number of patients to treat (0-4 points), as these subcategories did not apply to these diagnostic studies (Table 1). This left a total maximum score of 70 points. MCMS scores were reported both as a raw score and percentage.
TABLE 1.
Modified Coleman Methodology Scoring Used in This Studya
| Category | No. of Points | Category | No. of Points |
|---|---|---|---|
| 1. Inclusion criteria | 6. (continued) | ||
| Not described | 0 | Medium-term (6-24 mo) | |
| Described without percentages given | 3 | Patient retention <80% | 2 |
| Enrollment rate <80% | 6 | Patient retention 80%-90% | 4 |
| Enrollment rate >80% | 9 | Patient retention >90% | 6 |
| 2. Power | Long-term (>24 mo) | ||
| Not reported | 0 | Patient retention <80% | 4 |
| >80%, methods not described | 3 | Patient retention 80%-90% | 6 |
| >80%, methods described | 6 | Patient retention >90% | 8 |
| 3. Alpha error | 7. Patient analysis | ||
| Not reported | 0 | Incomplete | 0 |
| <0.05 | 3 | Complete | 3 |
| <0.01 | 6 | Complete and intention-to-treat | 6 |
| 4. Sample size | 8. Blinding | ||
| Not stated or <20 | 0 | None | 0 |
| 20-40 | 3 | Single | 2 |
| 41-60 | 6 | Double | 4 |
| >60 | 9 | Triple | 6 |
| 5. Randomization | 9. Treatment description | ||
| Not randomized | 0 | None | 0 |
| Modified/partial | Fair | 3 | |
| Not blinded | 2 | Adequate | 6 |
| Blinded | 4 | 10. Group comparability | |
| Complete | Not comparable | 0 | |
| Not blinded | 6 | Partially comparable | 3 |
| Blinded | 8 | Comparable | 6 |
| 6. Follow-up | 11. Similarity in treatment/cointerventions (0-6 points)b | ||
| Short-term (<6 mo) | 12. Outcome assessments (0-6 points)b | ||
| Patient retention <80% | 0 | 13. Description of rehabilitation protocol (0-4 points)b | |
| Patient retention 80%-90% | 2 | 14. Clinical effect measurement (0-6 points)b | |
| Patient retention >90% | 4 | 15. Number of patients to treat (0-4 points)b |
aAdapted from Cowan et al.4
bThese 5 categories were excluded from analysis (see Methods).
Data were extracted from each article, including journal, publication date, title, authors, conflict of interest reporting, study design, blinding, randomization, power, alpha error, study purpose, patient analysis type, year of patient examination, country of origin, source of subjects, inclusion criteria, exclusion criteria, number of eligible patients, number of enrolled patients, clinical follow-up, level of athletic participation, type of sports participation, number with shoulder pain at baseline, shoulder diagnoses, shoulder surgeries, patient age, sex, hand dominance, group comparability, examination techniques, definition of scapular dyskinesis, adequacy of examination description, and number of examiners.
Overhead sports were defined by performing a separate search utilizing the PubMed database and the search terms “((Overhead) AND Athlete) AND Sport.” The first 100 results were reviewed for definitions of an overhead athlete. From these 100 articles, 18 sports were defined as “overhead,” including baseball, volleyball, tennis, softball, water polo, handball, swimming, field events (including javelin throwing, shot put, discus, pole vaulting), badminton, basketball, squash, racquetball, gymnastics, football (quarterback only), soccer (goalkeeper only), wheelchair basketball, lacrosse, and golf. Wheelchair basketball, golf, and lacrosse were only referred to as overhead in 1 article each. The authors unanimously agreed, based on the lack of sustained and vigorous activity above the level of the shoulder, that lacrosse and golf should be defined as nonoverhead sports. Although wheelchair basketball was only discussed in 1 article, basketball was listed in 5 articles. Due to this and the shoulder position necessary to dribble and shoot a ball from a wheelchair, the authors have designated it as an overhead sport. By exclusion, all other sports identified by our search were considered nonoverhead, including amputee soccer, disabled table tennis, table tennis, diving, bowling, archery, and rugby.
Data Analysis
Studies were included as “overhead” for the overall analysis if ≥80% of the athletes they included participated in overhead sports. Two studies, one by Park et al23 and the second by Clarsen et al,2 did not include overall prevalence data of scapular dyskinesis. Clarsen et al2 separated the prevalence data into those who exhibited dyskinesis during shoulder flexion or shoulder scaption (defined as shoulder abduction in the scapular plan or 30° anterior to the coronal plane). Only the scaption value was used for the overall calculation. Park et al23 reported the data by number of shoulders with dyskinesis rather than by the number of patients. For the overall calculation, the average of the maximum (patients were assumed to have only 1 shoulder involved) and minimum (patients were assumed to have 2 shoulders involved) number of patients was used. All reported and calculated values are listed in Table 2. Continuous variable data were reported as means and standard deviations. Means and standard deviations were calculated for all subject and shoulder parameters. Categorical variable data were reported as frequency with percentages.
TABLE 2.
Clinical Outcomes From the Included Studies
| Article | No. of Subjects | Identification Technique | Sports | Category | Prevalence of Scapular Dyskinesis, n (%) |
|---|---|---|---|---|---|
| Clarsen et al2 | 203 | Visual observation | Handball | Overhead | Abduction: 49/203 (24) Flexion: 100/203 (62) |
| Aytar et al1 | 63 | Lateral scapular slide test | Wheelchair basketball | Overhead | 17/22 (77) |
| Disabled table tennis, amputee soccer | Nonoverhead | 15/41 (37) | |||
| Park et al24 | 165 Overhead ≥80% (80%)a | Visual observation | Baseball, swimming, javelin throwing, handball, basketball, golf, table tennis, diving, bowling, archery, “occasional sporting activity” | Overhead | 145/165 (88) |
| Struyf et al30 | 113 | Visual observation | Volleyball, badminton, tennis, baseball, handball | Overhead | 37/113 (28) |
| Park et al23 | 89 Overhead ≥80% (93%)a | Visual observation | Baseball, volleyball, swimming, badminton, golf, “occasional sporting activity” | Overhead | 122/178 shoulders Maximum: 89/89 patients (100) Minimum: 61/89 patients (69) Average: 75/89 patients (84) |
| Tate et al32 | 67 | Visual observation | Swimming | Overhead | 32/67 (48) |
| Kawasaki et al8 | 103 | Visual observation | Rugby | Nonoverhead | 33/103 (32) |
| Madsen et al17 | 78 | Visual observation | Swimming | Overhead | 0/78 (0) |
| Merolla et al19 | 31 | Visual observation | Volleyball | Overhead | 31/31 (100) |
| Reeser et al27 | 276 | Visual observation | Volleyball | Overhead | 158/276 (57) |
| McClure et al18 | 142 | Visual observation | Water polo, swimming, baseball, softball, volleyball, tennis | Overhead | 89/142 (63) |
| Koslow et al16 | 71 | Lateral scapular slide test | Basketball, baseball, tennis, volleyball | Overhead | 52/71 (73) |
aArticles with mixed overhead and nonoverhead athletes (without reporting separate results) were designated as overhead if ≥80% of the athletes were classified as overhead athletes.
bClarsen et al2 reported results when tested in flexion and in abduction separately. Both are reported, but only prevalence in abduction was included in the overall analysis.
cPark et al23 reported the prevalence in shoulders, rather than by patients. The average of the maximum (patients were assumed to have only 1 shoulder involved) and minimum (patients were assumed to have 2 shoulders involved) number of patients with the number of affected shoulders was used for overall analysis.
Results
Using the PubMed database and the search criteria discussed above, 1787 articles were available for review. Of these, 1492 were excluded based solely on the abstract. The remaining 295 articles were obtained and reviewed. After exclusion of 283 articles, there were 12 articles left that included prevalence data on scapular dyskinesis in overhead or nonoverhead athletes (Figure 1). Of these 12 studies, all were either level 2 (33%) or level 3 (67%) evidence (Table 3). Fifty-eight percent of studies (7/12 studies) denied the presence of any financial conflict of interest. Financial conflict of interest was unreported in the remaining 42% of studies. Most of the studies were performed in the United States (4 studies, 33%), Asia (3 studies, 25%), Europe (2 studies, 17%), or Scandinavia (2 studies, 17%). The overall mean MCMS was 38% (26.8 ± 5.4 of 70 points), which represents a poor rating. The 3 highest scoring MCMS items were sample size, patient analysis, and description of treatment. The 4 lowest scoring MCMS items were randomization, power, follow-up, and blinding.
TABLE 3.
Demographic Information for the Included Studies (N = 12)a
| Variable | n (%) |
|---|---|
| Level of evidence (by CEBM criteria) | |
| Level 1 | 0 (0) |
| Level 2 | 4 (33) |
| Level 3 | 8 (67) |
| Level 4 | 0 (0) |
| Financial conflict of interest | |
| Yes | 0 (0) |
| No | 7 (58) |
| Not reported | 5 (42) |
| Country of study origin | |
| United States | 4 (33) |
| Europe (Belgium, Italy) | 2 (17) |
| Asia (Japan, South Korea) | 3 (25) |
| Scandinavia (Norway, Denmark) | 2 (17) |
| Turkey | 1 (8) |
| Journal of publication | |
| Br J Sports Med | 1 (8) |
| Prosthet Orthot Int | 1 (8) |
| J Shoulder Elbow Surg | 4 (33) |
| Int J Sports Med | 1 (8) |
| J Athl Train | 2 (17) |
| Clin J Sport Med | 1 (8) |
| PM R | 1 (8) |
| J Orthop Sports Phys Ther | 1 (8) |
| Dates of subject enrollment | 2006-2011 |
| Modified Coleman methodology score, adjusted, % (mean ± SD)b | 38 ± 7.8 |
aCEBM, Centre for Evidence-Based Medicine.
bTo accurately represent the study quality, the Coleman methodology score was reported as a percentage (26.8 ± 5.4 divided by 70).
Within these 12 studies, 1401 subjects were available for analysis, with a mean age of 24.4 ± 7.1 years (Table 4). Of the 11 studies that reported subject sex, 78% were men and 22% were women.1,2,8,16–19,23,24,27,30 Prior authors have noted that the dominant extremity often exhibits accentuated dyskinetic findings attributed to overuse, injury, muscle asymmetry, and differences in range of motion.2,10,31 Most studies1,2,8,19,23,24,27,30 reported the hand dominance of the subjects, but only 2 studies8,18 reported the laterality (ie, left or right) of the dyskinetic extremity without reporting dominance while another 2 studies2,30 reported whether the dominant extremity was affected without reporting laterality. Kawasaki et al8 found a greater rate of dyskinesis in the right upper extremity (21% vs 13%) and commented that the “right … was often … the side of dominancy.” McClure et al18 found a greater rate in the left extremity (37% vs 26% in the right extremity), with 23% of subjects affected bilaterally with no mention of dominance. Clarsen et al2 and Struyf et al30 did not comment on laterality but reported the dominant extremity was affected in 24% and 29% of subjects, respectively.
TABLE 4.
Demographic Information for the Patients Within the Included Studiesa
| Variable | Overhead Athletes (n = 1257 Patients) | Nonoverhead Athletes (n = 144 Patients) |
|---|---|---|
| Patient sex | ||
| Male | 899 (72) | 136 (94) |
| Female | 291 (23) | 8 (6) |
| Not reported | 67 (5) | 0 (0) |
| Hand dominance | ||
| Right | 490 (39) | 99 (69) |
| Left | 111 (9) | 4 (3) |
| Not reported | 656 (52) | 41 (29) |
| Patient age, y, mean ± SD | 24.3 ± 7.9 | 24.8 ± 0.2 |
aData are reported as n (%) unless otherwise indicated.
Clinical identification methods for scapular dyskinesis varied considerably among these 12 studies (Table 5). Most of these studies (10/12) used visual observation, either live‡ and/or by video review,18 to identify scapular dyskinesis. Each subject was asked to perform repetitive shoulder movements known to demonstrate scapular dyskinesis if present, such as shoulder flexion, shoulder abduction (in the coronal plane), or scaption (shoulder abduction in the plane of the scapula or 30° anterior to the coronal plane), but the combinations of these 3 movements utilized and the number of repetitions differed between studies (Table 5). The examiner observed the subject from behind to identify “premature or excessive scapular elevation or protraction, nonsmooth or stuttering motion during arm elevation or lowering, or rapid downward rotation during arm lowering.”11,18 Four studies1,16,17,30 reported whether dyskinesis was present; 3 studies2,18,32 categorized dyskinesis as absent, subtle, or obvious; and 5 studies8,19,23,24,27 used the Kibler classification for the pattern of dyskinesis.14 Half of the studies (6/12) used weights during shoulder movements to exacerbate subtle differences in scapular rhythm.2,8,18,23,24,32 Of the studies using weights, 4 studies18,23,24,32 adjusted the amount of weight used based on the subjects’ body weight (with 3 different regimens), while 2 studies2,8 used the same weight for all subjects regardless of body weight. Four studies1,16,27,30 used variants of the lateral scapular slide test. During this test, the scapula is examined with the shoulder in 3 different positions: (1) with the arms relaxed at the subjects’ sides, (2) with the subjects’ hands placed on their ipsilateral hips with thumbs posterior and fingers anterior (ie, shoulder abducted to approximately 45° and internally rotated), and (3) with their shoulders abducted to 90°. For position 3, 1 study30 used neutral shoulder rotation (ie, thumbs up), while the other 3 studies1,16,27 used maximal shoulder internal rotation (ie, thumbs down). Two studies27,31 utilized these positions for visual classification, while another 2 studies1,16 performed the actual measurements. In these latter 2 studies, the distance between the inferior angle of the scapula and the closest thoracic spinous process was measured, as was initially described by Kibler et al.15 If this distance was greater than 1.5 cm in any position, the subject was deemed to have scapular dyskinesis.1,16
TABLE 5.
Clinical Identification Techniques Used by These 12 Studies for Scapular Dyskinesisa
| Study | Classification of Findings | Technique Used | Videotape Analysis? | Weight Used? | |
|---|---|---|---|---|---|
| Visual Observation | Measurement | ||||
| Clarsen et al2 | Normal, subtle dyskinesis, and obvious dyskinesis | Live observation: 5 repetitions of shoulder flexion, 5 repetitions of shoulder abduction | Yes | Yes, 5 kg | |
| Aytar et al1 | Normal and dyskinesis | LSSTb | No | No | |
| Park et al24 | Kibler classification (type I-IV) | Live observation: 10 repetitions of shoulder flexion, 10 repetitions of shoulder scaption | Yes | Yes, adjusted by body weight | |
| Struyf et al30 | Normal and dyskinesis | Live observation in 3 LSST positionsb: 3 repetitions of shoulder abduction | No | No | |
| Park et al23 | Kibler classification (type I-IV) | Live observation: 10 repetitions of shoulder flexion, 10 repetitions of shoulder scaption | Yes | Yes, adjusted by body weight | |
| Tate et al32 | Normal, subtle dyskinesis, and obvious dyskinesis | Live observation: 5 repetitions of shoulder flexion, 5 repetitions of shoulder abduction | No | Yes, adjusted by body weight | |
| Kawasaki et al8 | Kibler classification (type I-IV) | Live observation: 5 repetitions of shoulder flexion, 5 repetitions of shoulder scaption | Yes | Yes, 3 kg | |
| Madsen et al17 | Normal and dyskinesis | Live observation: 3 repetitions of shoulder scaption, 3 repetitions of wall push-up | No | No | |
| Merolla et al19 | Kibler classification (type I-IV) | Live observation: arm at side, elbow flexed to 90° | No | No | |
| Reeser et al27 | Kibler classification (type I-IV) | Live observation in 3 LSST positionsb | No | No | |
| McClure et al18 | Normal, subtle dyskinesis, and obvious dyskinesis | Video observation: 5 repetitions of shoulder flexion, 5 repetitions of shoulder abduction | Yes | Yes, adjusted by body weight | |
| Koslow et al16 | Normal and dyskinesis | LSSTb | No | No | |
aabduct, abduction; flex, flexion; LSST, lateral scapular slide test; scapt, scaption (elevation in the plane of scapular or 30° anterior to the coronal plane).
bThe 3 positions utilized for the LSST are described within the Results section.
Most of the subjects met our definition of “overhead athletes” (1257 subjects, 90%) compared with “nonoverhead athletes” (144 subjects, 10%). The most common sports among overhead athletes were volleyball (30%), baseball (18%), handball (18%), and swimming (14%) (Figure 2). The most common sports for nonoverhead athletes were rugby (66%), disabled table tennis (15%), and amputee soccer (13%). Overall, the reported prevalence of scapular dyskinesis was 54.5% in overhead athletes and 33.3% in nonoverhead athletes (Table 6).
Figure 2.
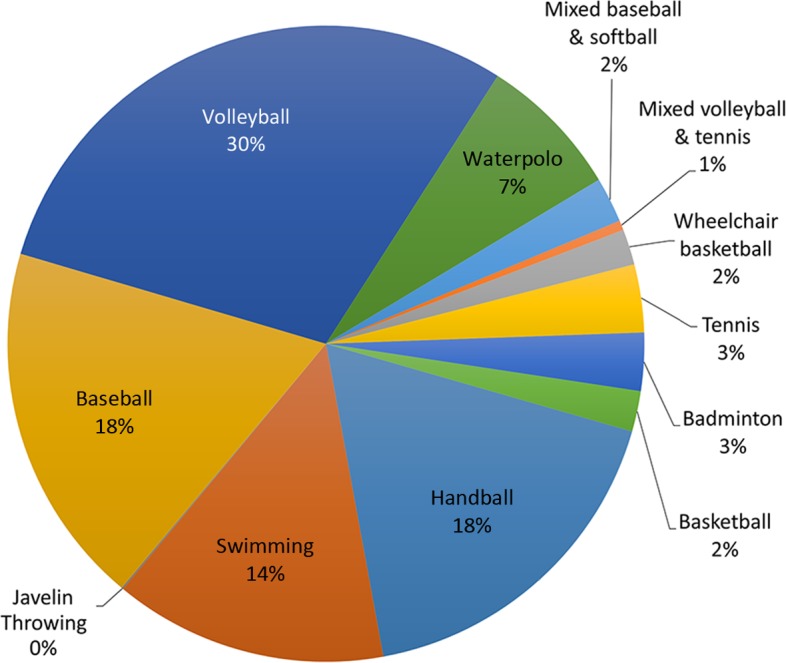
Pie chart showing an overview of the sport participation in the overhead athlete population.
TABLE 6.
Overall Reported Prevalence of Scapula Dyskinesis in Overhead and Nonoverhead Athletes
| Overhead Athletes | Nonoverhead Athletes | |
|---|---|---|
| Total patients, n | 1257 | 144 |
| Prevalence of scapular dyskinesis, % | 54.5 | 33.3 |
Discussion
The purpose of this systematic review was to identify and compare the reported prevalence of scapular dyskinesis in overhead and nonoverhead athletes. The authors hypothesized that overhead athletes would demonstrate a significantly greater reported prevalence of scapular dyskinesis compared with nonoverhead athletes due to increased forces and stress on the shoulder.30,31 Overhead athletes did have a greater reported prevalence of scapular dyskinesis (61%) compared with nonoverhead athletes (33%); however, the reported prevalence of scapular dyskinesis in nonoverhead athletes was higher than the authors expected.
Identifying scapular dyskinesis allows for early therapeutic intervention, which has been shown to improve shoulder symptoms, shoulder function, and theoretically decrease the risk of further shoulder injury.6,31 Kibler and Sciascia11 introduced a classification system for scapular dyskinesis based on visual observation, which has become the gold standard. The majority of studies included in this systematic review utilized visual observation of abnormal scapular rhythm to identify scapular dyskinesis.§ Unfortunately, this technique has shown only moderate specificity and sensitivity, which are limited by the reliance on subjective interpretation and the examiners’ level of experience.14,31 In light of this, modifications to this technique by adding arm weights to exacerbate subtle dyskinesis and simplifying the classification system to identify only whether dyskinesis is present have been used to increase reliability.2,8,27,30 Additionally, other identification methods have been investigated that allow objective quantification of scapular motion using 3-dimensional kinematics with skin surface markers placed over bone landmarks in combination with motion capture devices. However, the use of kinematics is limited by cost, the need for technical experience and equipment, lack of control values, movement of the overlying skin in combination with the scapula’s depth below the overlying musculature, and the complexity of 3-dimensional scapular motion, where measurements must take into account 3 rotational and 2 translational movements.5,10,23,28,29 Kinematic accuracy could be improved by attaching the probes directly to the scapula, but this would be invasive and is not feasible for human clinical studies.30 Park et al23,24 have investigated 3-dimensional wing computed tomography, which has shown promise in identifying scapular angulation and translation but requires significant radiation exposure. Due to the limitations of these newer techniques, clinical examination remains the gold standard for identifying scapular dyskinesis.4,8,20,21,26,27
This study has limitations, including, most notably, the level of evidence of the included studies, which represent level 2 (33%) or level 3 (67%) evidence. Although level 1 through 4 studies were within the inclusion criteria, no level 1 or level 4 study passed inclusion criteria. Selection bias was limited by the inclusive nature of our search, as level 5 studies were the only level of evidence excluded. However, a number of the included studies had some type of bias. Almost half (42%) of these studies failed to report their conflict of interest, which could contribute to selection bias. Measurement bias was present due to the difference in patient demographics between each study and the difference in clinical identification or measurement techniques utilized in the detection of scapular dyskinesis. Most (n = 10) of the studies used some variant of visual observation with or without video recording, while 4 studies used a variation of the lateral scapular slide test with measurement between the medial scapular border and the thoracic spine. Due to the data reporting in the included studies, it is not possible to determine whether the extremity affected by scapular dyskinesis was the dominant extremity, nondominant extremity, or both in all athletes. Overhead athletes, especially in unilateral sports (ie, baseball pitchers), commonly have hemihypertrophy in the dominant extremity and may have shown an inflated prevalence when looking only at the dominant extremity.11,31 This physical asymmetry may confound the ability of the investigators in these studies to accurately identify shoulders with normal or dyskinetic patterns of movement. Investigators were not blinded to each articles’ identifying features (eg, authors, institution, journal, sponsorship, etc), which could contribute to bias. However, Morissette et al21 showed an insignificant difference between blinded and unblended systematic reviews. There was a significant difference between the sex and hand dominance of patients between the overhead and nonoverhead groups; however, there was no significant difference in age (see Table 4). Publication bias is present, as publications in non-English languages and unpublished English language studies were excluded.
During this literature search, we noticed a paucity of high-quality research dedicated to scapular dyskinesis, with no level 1 evidence. In addition, we were unable to locate any studies reporting an overall prevalence of scapular dyskinesis in either overhead athletes or nonoverhead athletes. Available studies used a wide variety of techniques to identify scapular dyskinesis, with few studies using identical techniques. Additionally, the majority did not correlate their findings with laterality, bilaterality, or hand dominance, which is especially important in overhead athletes. Overhead athletes have a greater prevalence of reported scapular dyskinesis compared with nonoverhead athletes. Scapular dyskinesis was found to be present in 61% of overhead athletes and 33% of nonoverhead athletes. These represent areas within the literature that are lacking and would benefit from additional study to allow optimization of athletic function and performance.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
References
- 1. Aytar A, Zeybek A, Pekyavas NO, Tigli AA, Ergun N. Scapular resting position, shoulder pain and function in disabled athletes. Prosthet Orthot Int. 2015;39:390–396. [DOI] [PubMed] [Google Scholar]
- 2. Clarsen B, Bahr R, Andersson SH, Munk R, Myklebust G. Reduced glenohumeral rotation, external rotation weakness and scapular dyskinesis are risk factors for shoulder injuries among elite male handball players: a prospective cohort study. Br J Sports Med. 2014;48:1327–1333. [DOI] [PubMed] [Google Scholar]
- 3. Cools AM, Struyf F, De Mey K, Maenhout A, Castelein B, Cagnie B. Rehabilitation of scapular dyskinesis: from the office worker to the elite overhead athlete. Br J Sports Med. 2014;48:692–697. [DOI] [PubMed] [Google Scholar]
- 4. Cowan J, Lozano-Calderon S, Ring D. Quality of prospective controlled randomized trials. Analysis of trials of treatment for lateral epicondylitis as an example. J Bone Joint Surg Am. 2007;89:1693–1699. [DOI] [PubMed] [Google Scholar]
- 5. Giphart JE, Brunkhorst JP, Horn NH, Shelburne KB, Torry MR, Millett PJ. Effect of plane of arm elevation on glenohumeral kinematics: a normative biplane fluoroscopy study. J Bone Joint Surg Am. 2013;95:238–245. [DOI] [PubMed] [Google Scholar]
- 6. Harris JD, Pedroza A, Jones GL; MOON (Multicenter Orthopedic Outcomes Network) Shoulder Group. Predictors of pain and function in patients with symptomatic, atraumatic full-thickness rotator cuff tears: a time-zero analysis of a prospective patient cohort enrolled in a structured physical therapy program. Am J Sports Med. 2012;40:359–366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hong J, Barnes MJ, Leddon CE, Van Ryssegem G, Alamar B. Reliability of the sitting hand press-up test for identifying and quantifying the level of scapular medial border posterior displacement in overhead athletes. Int J Sports Phys Ther. 2011;6:306–311. [PMC free article] [PubMed] [Google Scholar]
- 8. Kawasaki T, Yamakawa J, Kaketa T, Kobayashi H, Kaneko K. Does scapular dyskinesis affect top rugby players during a game season? J Shoulder Elbow Surg. 2012;21:709–714. [DOI] [PubMed] [Google Scholar]
- 9. Kibler WB. The role of the scapula in athletic shoulder function. Am J Sports Med. 1998;26:325–337. [DOI] [PubMed] [Google Scholar]
- 10. Kibler WB, Ludewig PM, McClure PW, Michener LA, Bak K, Sciascia AD. Clinical implications of scapular dyskinesis in shoulder injury: the 2013 consensus statement from the ‘Scapular Summit’. Br J Sports Med. 2013;47:877–885. [DOI] [PubMed] [Google Scholar]
- 11. Kibler WB, Sciascia A. Current concepts: scapular dyskinesis. Br J Sports Med. 2010;44:300–305. [DOI] [PubMed] [Google Scholar]
- 12. Kibler WB, Sciascia A, Uhl T. Medial scapular muscle detachment: clinical presentation and surgical treatment. J Shoulder Elbow Surg. 2014;23:58–67. [DOI] [PubMed] [Google Scholar]
- 13. Kibler WB, Thomas SJ. Pathomechanics of the throwing shoulder. Sports Med Arthrosc. 2012;20:22–29. [DOI] [PubMed] [Google Scholar]
- 14. Kibler WB, Uhl TL, Maddux JW, Brooks PV, Zeller B, McMullen J. Qualitative clinical evaluation of scapular dysfunction: a reliability study. J Shoulder Elbow Surg. 2002;11:550–556. [DOI] [PubMed] [Google Scholar]
- 15. Kibler WB, Wilkes T, Sciascia A. Mechanics and pathomechanics in the overhead athlete. Clin Sports Med. 2013;32:637–651. [DOI] [PubMed] [Google Scholar]
- 16. Koslow PA, Prosser LA, Strony GA, Suchecki SL, Mattingly GE. Specificity of the lateral scapular slide test in asymptomatic competitive athletes. J Orthop Sports Phys Ther. 2003;33:331–336. [DOI] [PubMed] [Google Scholar]
- 17. Madsen PH, Bak K, Jensen S, Welter U. Training induces scapular dyskinesis in pain-free competitive swimmers: a reliability and observational study. Clin J Sport Med. 2011;21:109–113. [DOI] [PubMed] [Google Scholar]
- 18. McClure P, Tate AR, Kareha S, Irwin D, Zlupko E. A clinical method for identifying scapular dyskinesis, part 1: reliability. J Athl Train. 2009;44:160–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Merolla G, De Santis E, Sperling JW, Campi F, Paladini P, Porcellini G. Infraspinatus strength assessment before and after scapular muscles rehabilitation in professional volleyball players with scapular dyskinesis. J Shoulder Elbow Surg. 2010;19:1256–1264. [DOI] [PubMed] [Google Scholar]
- 20. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8:336–341. [DOI] [PubMed] [Google Scholar]
- 21. Morissette K, Tricco AC, Horsley T, Chen MH, Moher D. Blinded versus unblinded assessments of risk of bias in studies included in a systematic review. Cochrane Database Syst Rev. 2011;9:MR000025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Myers JB, Oyama S, Hibberd EE. Scapular dysfunction in high school baseball players sustaining throwing-related upper extremity injury: a prospective study. J Shoulder Elbow Surg. 2013;22:1154–1159. [DOI] [PubMed] [Google Scholar]
- 23. Park JY, Hwang JT, Kim KM, Makkar D, Moon SG, Han KJ. How to assess scapular dyskinesis precisely: 3-dimensional wing computer tomography—a new diagnostic modality. J Shoulder Elbow Surg. 2013;22:1084–1091. [DOI] [PubMed] [Google Scholar]
- 24. Park JY, Hwang JT, Oh KS, Kim SJ, Kim NR, Cha MJ. Revisit to scapular dyskinesis: three-dimensional wing computed tomography in prone position. J Shoulder Elbow Surg. 2014;23:821–828. [DOI] [PubMed] [Google Scholar]
- 25. Pizzari T, Wickham J, Balster S, Ganderton C, Watson L. Modifying a shrug exercise can facilitate the upward rotator muscles of the scapula. Clin Biomech (Bristol, Avon). 2014;29:201–205. [DOI] [PubMed] [Google Scholar]
- 26. Pluim BM. Scapular dyskinesis: practical applications. Br J Sports Med. 2013;47:875–876. [DOI] [PubMed] [Google Scholar]
- 27. Reeser JC, Joy EA, Porucznik CA, Berg RL, Colliver EB, Willick SE. Risk factors for volleyball-related shoulder pain and dysfunction. PM R. 2010;2:27–36. [DOI] [PubMed] [Google Scholar]
- 28. Ribeiro A, Pascoal AG. Resting scapular posture in healthy overhead throwing athletes. Man Ther. 2013;18:547–550. [DOI] [PubMed] [Google Scholar]
- 29. Scibek JS, Carcia CR. Assessment of scapulohumeral rhythm for scapular plane shoulder elevation using a modified digital inclinometer. World J Orthop. 2012;3(6):87–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Struyf F, Nijs J, Meeus M, et al. Does scapular positioning predict shoulder pain in recreational overhead athletes? Int J Sports Med. 2014;35:75–82. [DOI] [PubMed] [Google Scholar]
- 31. Struyf F, Nijs J, Mottram S, Roussel NA, Cools AM, Meeusen R. Clinical assessment of the scapula: a review of the literature. Br J Sports Med. 2014;48:883–890. [DOI] [PubMed] [Google Scholar]
- 32. Tate A, Turner GN, Knab SE, Jorgensen C, Strittmatter A, Michener LA. Risk factors associated with shoulder pain and disability across the lifespan of competitive swimmers. J Athl Train. 2012;47:149–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Williams JG, Laudner KG, McLoda T. The acute effects of two passive stretch maneuvers on pectoralis minor length and scapular kinematics among collegiate swimmers. Int J Sports Phys Ther. 2013;8:25–33. [PMC free article] [PubMed] [Google Scholar]


