Abstract
Background:
Over the past 30 years, there has been a dramatic increase in the prevalence of childhood obesity and hypertension in the United States. The prevalence of these diagnoses among individuals participating in school-sanctioned sports has not been clearly defined.
Purpose:
To identify the prevalence of obesity and elevated blood pressure (BP) among student athletes and investigate associations between race, sex, type and number of sports played, and the prevalence of these diseases.
Study Design:
Cross-sectional study; Level of evidence, 3.
Methods:
Pre–sports participation medical examinations (N = 7705) performed between 2009 and 2013 were reviewed to identify the prevalence of obesity and elevated BP and examine relationships between the type of sports played, participation in multiple sports versus a single sport, and the athlete’s body weight and body mass index (BMI).
Results:
The prevalence of obesity was 23.5%. There was a significant association (P < .001) between the number of sports played by the student and BMI. The risk of obesity among single-sport athletes was more than 2-fold the risk (relative risk [RR], 2.13) compared with ≥3-sport athletes and 1.42 times greater compared with 2-sport athletes (RR, 1.42). The prevalence of elevated BP was 21.2%. There was a significant association (P < .001) between the number of sports played by the student and elevated BP. The risk of elevated BP among single-sport athletes was 1.59 times greater (RR, 1.59) than ≥3-sport athletes and 1.30 times greater compared with 2-sport athletes (RR, 1.30). Finally, obese students were 2.40 times more likely to have elevated BP compared with nonobese students (P < .001).
Conclusion:
The result of this study confirms the progressive nature of the obesity epidemic and identifies the contribution of obesity to the worsening cardiometabolic profiles in student athletes. The study also identifies that participation in multiple sports and running sports decreases the individual’s risk for obesity and hypertension.
Clinical Relevance:
The present study emphasizes the importance of screening for obesity and elevated blood pressure during the athlete’s preparticipation physical examination.
Keywords: obesity, hypertension, adolescent, student, athletes
According to the National Federation of State High School Associations (NFHS), almost 8 million student athletes participate in school-sanctioned sports each year.17 For many of today’s youth, sports provide an opportunity for developing social skills and healthy exercise habits. Furthermore, participation in school sports is associated with improved academic performance, self-esteem, and a reduction in high-risk behavior.6,15,16 As a prerequisite to participation, many students are required to undergo an annual preparticipation medical evaluation (PPE). The NFHS has acknowledged the importance of a preseason medical history and physical examination, and most state governments require athletes participating in state-funded sports to obtain documentation of their general fitness prior to involvement in a sports program.19 While obtaining “preseason medical clearance” may be considered standard practice, there remains a great deal of debate regarding the appropriate context, content, and expectation of health benefits to be obtained by the PPE. For some, this encounter may be viewed as a waiver of liability for sports participation; however, the PPE should be regarded as an opportunity to provide the athlete with a comprehensive examination and general health screening. This opportunity may be especially important in patient populations with limited access to primary medical care.
Over the past 30 years, there has been a dramatic increase in the prevalence of childhood obesity in the United States. A general trend for increasing prevalence of pediatric obesity can be observed among most patient populations; however, several studies have recognized a disproportionate risk among certain geographic and socioeconomic groups. Not only is the prevalence of childhood obesity increasing, but many of the comorbid conditions historically associated with adult-onset obesity, such as diabetes and hypertension, are also on the rise in this patient population.5,25,33 In the adolescent population, the diagnosis of obesity alone carries an increased risk for the development of early morbidity, cardiometabolic disease, osteoarthritis, and certain forms of cancer later in life.18,27 These alarming trends should be viewed as a significant health concern with widespread public health implications in the near future. The preparticipation encounter provides the sports medicine physician with an opportunity to identify patients at risk for adulthood obesity, who might otherwise have limited access to medical care. Also, since this unique medical encounter is associated with participation in sports, it may be an opportunity for the physician to influence the individual’s behavior positively by associating healthy diet and exercise habits with sports participation and performance.
Given the natural increases in body mass index (BMI) that occur with age, it is necessary to compare individuals using age- and sex-specific growth charts. The use of BMI to identify adolescents who are at an increased risk for adulthood obesity is well established in the medical literature.8,26,28,38 The Centers for Disease Control and Prevention (CDC) developed the CDC-2000 growth charts using representative surveys of US children and have categorized children and adolescents with a BMI ≥95th percentile as obese. These tables can be accurately used by health care providers to identify patients at risk for adulthood obesity and potentially influence the child’s health decisions early on in the development of disease.28
The prevalence of hypertension also appears to have increased during the obesity epidemic. Contemporary reports estimate the prevalence of hypertension among American children to be between 2% and 5%.28,30,36 While the US Preventative Services Task Force (USPSTF) has published evidence-based recommendations regarding screening and diagnosis of hypertension in children, there remains debate on the long-term impact of screening in this population.31,36 According to the American Academy of Pediatrics, routine blood pressure screening is an important component of the athlete’s physical examination, since elevated blood pressure represents one of the most common abnormal findings identified during the PPE.2 The purpose of this study was to identify the prevalence of obesity and elevated blood pressure in a population of Mississippi high school athletes and to examine the influence of sex, age, ethnicity, and details of sports participation on the prevalence of these diagnoses.
Methods
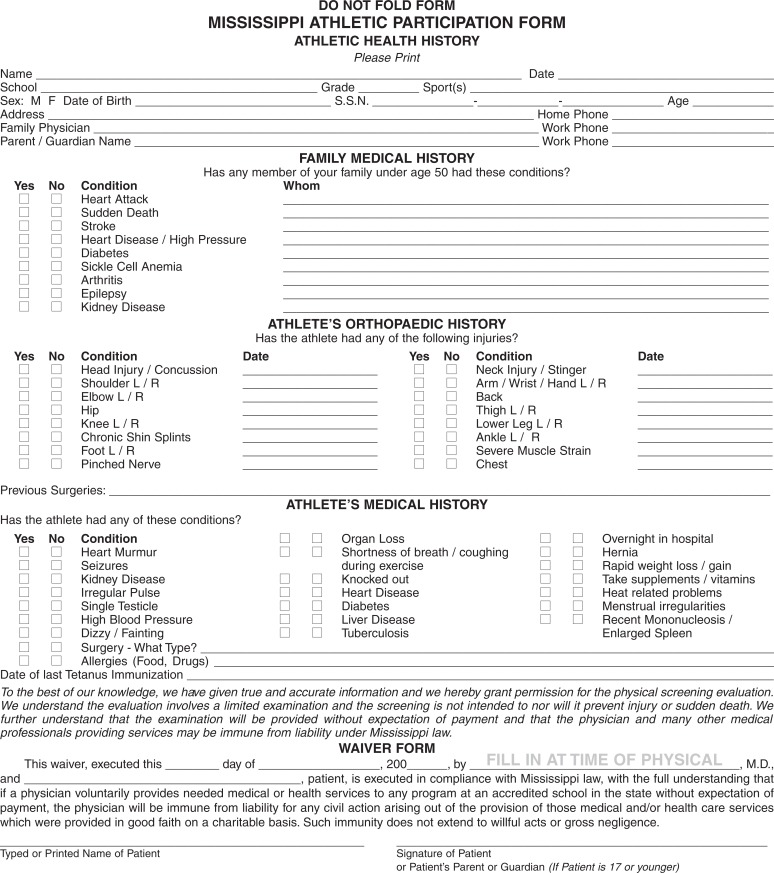
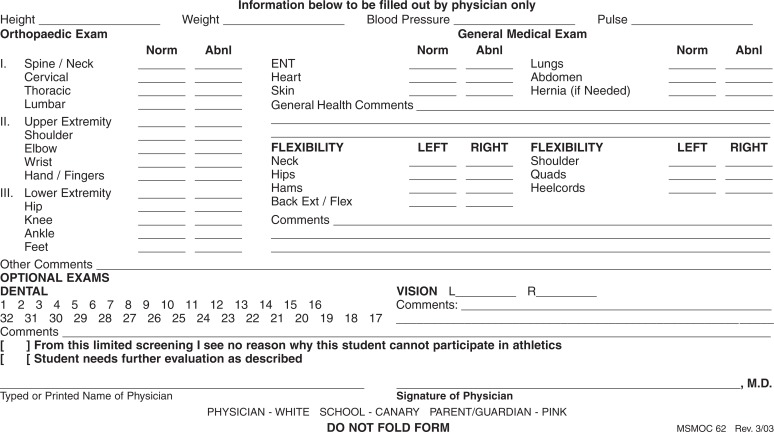
Between 2009 and 2013, PPEs were performed by a team of physicians from the Mississippi Sports Medicine and Orthopaedic Center (MSMOC) in Jackson, Mississippi. All encounters were performed by moving athletes through a coordinated medical team of providers, which included primary care physicians, orthopaedic surgeons, cardiologists, athletic trainers, registered nurses, and medical assistants. The student population was composed of athletes attending schools located in metropolitan or suburban areas of Jackson, Mississippi, who wished to participate in a school-sanctioned sport. These PPEs were utilized by 146 different high school athletic programs during the study period. All medical care was provided to the athletes free of charge by the sponsoring institution (MSMOC). The examinations were documented and completed using a standardized form. This comprehensive screening form was developed by the sponsoring institution (MSMOC) and includes pertinent patient history and physical examination components endorsed by the American Academy of Pediatrics and Preparticipation Physical Evaluation Working Group (see the Appendix). Furthermore, this form has been acknowledged by Mississippi state officials and is currently used as the standard preparticipation physical examination by the State of Mississippi High School Athletic Association.17 Informed consent for the examination was obtained from each patient’s legal guardian, and the study was approved by the sponsoring institution’s internal review board.
Inclusion criteria for the study included high school athletes aged 14 to 18 years and a first-time encounter with the individual student. Exclusion criteria included incomplete demographic data including date of birth, sex, and race or a physiologically implausible physical examination data value. Age was calculated in months from date of birth to date of PPE. Sex and ethnicity were self-described. Ethnic categories included white, African American, Asian, and Hispanic. Weight (kg) and height (m) were measured using a calibrated professional medical scale, and BMI was calculated (kg/m2). Athletes were assigned into BMI percentiles, which were based on the most current age and sex normative anthropometric reference data available from the CDC. Using BMI percentiles, individuals were grouped into 3 categories: normal weight (≤85th percentile), overweight (>85th and <95th percentile), or obese (≥95th percentile). For statistical analysis, sex, ethnicity, sport, and number of sports played were examined as individual predictors of obesity status.
All blood pressure measurements were done using an automated blood pressure cuff in the nondominant extremity by a registered nurse or medical assistant. Given the large population size of this study, automated oscillometric blood pressure measurements were utilized for general screening purposes.7 Individuals with a systolic pressure >120 mm Hg or diastolic pressure >80 mm Hg were referred for manual blood pressure measurements using a mercury sphygmomanometer for 3 consecutive measurements separated by 5 minutes of rest.32 The average of the 3 readings was used to represent the final blood pressure value. Blood pressure percentiles were calculated based on the most current normative anthropometric reference data available from the CDC. Using blood pressure percentiles, individuals were grouped into 2 categories: elevated blood pressure (≥95th percentile) or not elevated (<95th percentile). Definitive diagnosis of hypertension in pediatric populations requires longitudinal blood pressure tracking, and since these examinations represented a single encounter used for screening purposes and sports participation clearance, a definitive diagnosis of hypertension was not made at the time of the patient encounter. Last, students were classified by sport and as either having requested clearance to participate in 1 sport, 2 sports, or ≥3 sports.
Descriptive statistics are presented as means, standard deviations, and percentages. The chi-square test was used to test for associations between the 3 classifications of BMI and number of sports categories. Unadjusted relative risk (RR) and 95% CIs were calculated for individual predictors of obesity status (obesity vs normal/overweight) and elevated blood pressure. For adjusted estimates of relative risks, a binomial regression with a log link function was used. For inferential analyses including race, Hispanics and Asians were excluded because of inadequate sample size. A P value of .05 was used to determine statistical significance.
Results
During the study period, 19,176 PPEs were documented. There were 9183 students who met the inclusion criteria as a first-time encounter within the target age range. There were 1478 students who met the exclusion criteria, leaving 7705 examinations for the final analysis (Table 1). The primary reason for exclusion was patients reporting only their age and not their date of birth. Date of birth is required for BMI percentage categorization. During the study period, 169 (2.2%) students were not cleared for sports participation at the time of their initial encounter. The mean age of the sample was 15.5 years, with 69.4% being male. Based on self-reported ethnicity, blacks represented 66.4% and whites represented 31.9% of the study population. The mean BMI was 24.9 kg/m2. Based on BMI classification, the prevalence of obesity was 23.5%; 20.3% of students were overweight and 56.2% were normal weight. The prevalence of morbid obesity (BMI ≥99th percentile) was 3.5%. The most frequently cited sports participation were football (46.5%), basketball (28.4%), track and field (13.7%), and baseball (9.4%); 913 students did not endorse a sport for participation. The remaining students indicated that they participated in 1 sport (n = 4686, 69.0%), 2 sports (n = 1548, 22.8%), or ≥3 sports (n = 558, 8.2%). The prevalence of obesity and elevated blood pressure among athletes participating in a single sport is demonstrated in Table 2. The prevalence of student athletes with the combined diagnosis of obesity and elevated blood pressure was 9% (n = 697). The mean systolic and diastolic blood pressure measurements were 122.7 and 69.6 mm Hg, respectively. The prevalence of elevated blood pressure (blood pressure ≥95th percentile) was 21.2%.
TABLE 1.
Demographic and Clinical Variables for Students in Pre–Sports Participation Physicals (N = 7705)a
| Age, y, mean ± SD | 15.5 ± 1.17 |
|---|---|
| Age, y, n (%) | |
| 14 | 2109 (27.4) |
| 15 | 1993 (25.9) |
| 16 | 1976 (25.6) |
| 17 | 1297 (16.8) |
| 18 | 330 (4.3) |
| Sex, male/female, % | 69.4/30.6 |
| Ethnicity, n (%) | |
| Black | 5119 (66.4) |
| White | 2257 (31.9) |
| Hispanic | 90 (1.2) |
| Asian | 39 (0.5) |
| Anthropometric measures | |
| Height, cm, mean ± SD | 171.7 ± 11.1 |
| Weight, kg, mean ± SD | 74.4 ± 19.9 |
| BMI, kg/m2, mean ± SD | 24.9 ± 6.0 |
| Normal, % | 56.2 |
| Overweight, % | 20.3 |
| Obese, % | 23.5 |
| Hemodynamic measures | |
| Systolic BP, mm Hg, mean ± SD | 122.7 ± 13.1 |
| Diastolic BP, mm Hg, mean ± SD | 69.6 ± 9.4 |
| <90th percentile, % | 66.5 |
| 90th-94th percentile, % | 12.2 |
| ≥95th percentile, % | 21.2 |
| Physical examination by sport, n (%)b | |
| Football | 3585 (46.5) |
| Basketball | 2191 (28.4) |
| Track and field | 1057 (13.7) |
| Baseball | 727 (9.4) |
| Soccer | 627 (8.1) |
| Softball | 360 (4.7) |
| Cheerleading | 356 (4.6) |
| Cross country | 205 (2.7) |
| Tennis | 190 (2.5) |
| Volleyball | 80 (1.0) |
| Golf | 58 (0.8) |
| Swimming | 26 (0.3) |
| Lacrosse | 2 (<0.1) |
| Wrestling | 1 (<0.1) |
| None | 913 (11.8) |
aBMI, body mass index; BP, blood pressure.
bPercentages total to greater than 100% due to multisport athletes.
TABLE 2.
Prevalence of Obesity, Elevated Blood Pressure, and Combined Obesity and Elevated Blood Pressure Among Single-Sport Athletes
| Sport | n | Body Mass Index, % | Elevated Blood Pressure, % | Combined Obesity + Elevated Blood Pressure, %a | ||
|---|---|---|---|---|---|---|
| Normal | Overweight | Obese | ||||
| Football | 2307 | 38.2 | 22.3 | 39.4 | 28.4 | 16.2+ |
| Softball | 148 | 49.3 | 25.7 | 25.0 | 15.5 | 6.1 |
| Golf | 16 | 62.5 | 12.5 | 25.0 | 0.0 | 0.0 |
| Cheerleading | 253 | 64.8 | 19.8 | 15.4 | 17.0 | 5.9 |
| Baseball | 180 | 64.4 | 20.6 | 15.0 | 27.3 | 7.8 |
| Volleyball | 35 | 68.6 | 17.1 | 14.3 | 20.0 | 11.4 |
| Basketball | 1121 | 68.9 | 17.2 | 13.9 | 17.4 | 5.0– |
| Soccer | 298 | 70.1 | 19.8 | 10.1 | 16.4 | 2.3– |
| Track and field | 163 | 80.4 | 12.9 | 6.7 | 19.6 | 1.2– |
| Tennis | 59 | 66.1 | 25.4 | 8.5 | 20.3 | 3.4 |
| Cross country | 53 | 90.6 | 5.7 | 3.8 | 11.3 | 3.8 |
| Swimming | 11 | 72.7 | 18.2 | 9.1 | 36.4 | 0.0 |
aFor single-sport athletes, “+” indicates a statistically significant increase in prevalence and “–” indicates a statistically significant decrease in prevalence of combined obesity and elevated blood pressure in the sport category compared with athletes in other categories. For example, single-sport football players had a statistically significant increase in prevalence of combined obesity and elevated blood pressure compared with single-sport athletes in other sports.
Regarding individual predictors of obesity, there was a significant chi-square association (P < .001) between the number of sports played by the student and their BMI classification, with obesity rates decreasing as the number of sports played increased (Table 3). The prevalence of obesity among single-sport athletes was 26.4% compared with a prevalence of 18.9% and 12.5% for 2- and ≥3-sport athletes, respectively. Relative risks for obesity are shown in Table 4. Males had a significantly (P < .001) increased risk (RR, 1.49) of obesity compared with females. We failed to find significant associations between race and obesity, unadjusted or adjusted. The risk of obesity among single-sport athletes was 2.13 times the risk for ≥3-sport athletes and 1.42 times greater than the risk for 2-sport athletes. Further detail on the relative risks for obesity is reported in Table 4. Adjusting for race and number of sports played, males were statistically 1.71 times more likely to be obese compared with females. Adjusting for sex and race, single-sport athletes were 1.40 and 2.17 times more likely to be obese compared with 2- and ≥3-sport athletes, respectively.
TABLE 3.
Distribution of BMI and Blood Pressure Categories by Number of Sports Participationa
| 1 Sport | 2 Sports | ≥3 Sports | |
|---|---|---|---|
| BMI | |||
| Normal | 2506 (53.5) | 945 (61.0) | 363 (65.1) |
| Overweight | 942 (20.1) | 311 (20.1) | 125 (22.4) |
| Obese | 1238 (26.4) | 292 (18.9) | 70 (12.5) |
| Blood pressureb | |||
| Normal | 3603 (76.9) | 1275 (82.4) | 476 (85.3) |
| Elevated | 1083 (23.1) | 273 (17.6) | 82 (14.7) |
aData are presented as n (%). BMI, body mass index.
bP < .001.
TABLE 4.
Risk Factors for Obesity and Elevated Blood Pressurea
| Relative Risk (95% CI) | ||
|---|---|---|
| Unadjusted | Adjusted | |
| Obesity vs normal and overweight | ||
| Sex, male (vs female) | 1.49 (1.35-1.65) | 1.71 (1.52-1.92) |
| Race, black (vs white) | 1.01 (.93-1.10) | 0.95 (.87-1.04) |
| 1 sport (vs ≥3 sports) | 2.13 (1.70-2.67) | 2.17 (1.73-2.71) |
| 1 sport (vs 2 sports) | 1.42 (1.26-1.59) | 1.40 (1.26-1.58) |
| Elevated Blood Pressure | ||
| Sex, male (vs female) | 1.28 (1.15-1.41) | 1.24 (1.10-1.38) |
| Race, black (vs white) | 1.23 (1.11-1.35) | 1.20 (1.09-1.33) |
| 1 sport (vs ≥3 sports) | 1.59 (1.29-1.95) | 1.27 (1.09-1.64) |
| 1 sport (vs 2 sports) | 1.30 (1.15-1.47) | 1.17 (1.04-1.32) |
| Obese (vs normal and overweight) | 2.40 (2.11-2.61) | 2.33 (2.13-2.55) |
aP < .005 for all values except race comparison for obesity.
Regarding the individual predictors for elevated blood pressure, there was a significant chi-square association (P < .001) between the number of sports played by the student and elevated blood pressure (blood pressure ≥95th percentile for age and sex), with the prevalence of individuals with elevated blood pressure decreasing as the number of sports played increased (see Table 3). The prevalence of elevated blood pressure among single-sport athletes was 23.1% compared with a prevalence of 17.6% and 14.7% for 2- and ≥3-sport athletes, respectively. Further detail on the relative risks for elevated blood pressure is reported in Table 4. Males were 1.28 times more likely to have elevated blood pressure compared with females. Adjusting for race and number of sports played, males were 1.24 times more likely to have elevated blood pressure than females. There was a significant association between race and elevated blood pressure (P < .001), with blacks being 1.23 times more likely to have elevated blood pressure compared with whites. There was a significant association between elevated blood pressure status and number of sports played. The risk of elevated blood pressure among single-sport athletes was more than 1.59 times greater than athletes participating in ≥3 sports and 1.30 times greater compared with 2-sport athletes. There was also a significant association between elevated blood pressure and obesity status. Obese students were 2.40 times more likely to have elevated blood pressure compared with nonobese students.
Discussion
There are several limitations to this study. First, the authors recognize that the results of this study may not be representative of the general population of high school student athletes in the United States. In the current study, 66.4% of athletes examined were black and 31.9% were white. Also, football (29.9%) and basketball (14.5%) made up nearly 45% of the athletes examined. Since lower income athletes may be more inclined to participate in a free PPE and higher income athletes may have greater access to a primary care medical provider, it is possible a selection bias resulted in disproportionate representation from lower socioeconomic groups, which are at a higher risk for obesity and hypertension.13,35
Although the prevalence of childhood obesity has now reached epidemic proportions, it remains a difficult condition for many providers to identify and manage. In a study by O’Brien et al20 on pediatric patients presenting for routine health screenings, only 53% of obese patients were formally diagnosed as obese in their medical record. Among the patients diagnosed with obesity, only 33% of the medical records contained recommendations for lifestyle and activity modification.11 Given these findings, it is important for sports medicine providers to recognize that obesity may be easily overlooked during the PPE, and that screening and treatment recommendations frequently lacked adherence to the American Academy of Pediatrics’ guidelines for management.11 The American Academy of Pediatrics recommends diet and exercise as the first line of intervention for management of obesity and hypertension in pediatric patients.11 For many of today’s youth, sports participation is important in mental and physical development, and given the motivation to participate in sports, the athlete’s PPE provides the team physician with a unique opportunity to influence the patient’s general health decisions.
To our knowledge, this is one of the largest studies to report the prevalence of obesity and hypertension in a population of otherwise healthy athletes and the only study to examine the details of sports participation as a predictor of obesity and elevated blood pressure. In 2007, the National Survey of Children’s Health (NSCH) examined the general population of adolescents in the state of Mississippi. Using BMI, they reported a prevalence of overweight and obese individuals to be 22.6% and 21.9%, respectively.29 In this study, we found the prevalence of overweight and obese participants to be 20.3% and 23.5%, respectively. Our current study of student athletes demonstrates a strikingly similar prevalence of obese BMIs, which may be surprising considering that our patient population consisted of only athletes. This finding should be especially concerning for public health officials and policy makers, since several studies have identified elevated BMI in adolescents as perhaps the greatest predictor of long-term morbidity and mortality associated with cardiovascular disease.1,14,31,37
As noted previously, this study utilized sex- and age-specific BMI percentiles to define individuals as obese. Since BMI does not differentiate between lean body mass and excessive body fat—a distinction particularly relevant to our population of student athletes—one important feature of the current study design was critical examination of the available literature supporting utilization of BMI as a surrogate for excessive body fat composition in pediatric patients. When examining BMI as a screening tool for obesity, it is also important to recognize the difference between using BMI to classify individuals as overweight versus obese. As the individual’s BMI percentile increases above the 95% it becomes much less likely that the increase is secondary to lean body mass.23 Furthermore, obesity defined as BMI >95% is the established gold standard for identification of individuals at long-term risk for adulthood obesity and is known to track well in older populations of adolescents who are near or beyond sexual maturity, which made up our patient population. In a study by Whitlock et al,38 the authors demonstrated that the probability of obesity in adulthood is >50% among adolescents older than 13 years with a BMI value above the 95%. All individuals in our patient population were older than 13 years. Further, the distribution of our athletes as overweight and obese is strikingly similar to previously benchmarked values for the general adolescent population in the state of Mississippi. The results of our study identify an association between BMI >95% and elevated blood pressure; however, further study is warranted regarding long-term risk for development of cardiovascular disease associated with obesity and hypertension in the young athletes.
Another interesting finding was the prevalence of elevated blood pressure among our population of athletes. It is important to recognize that our diagnosis of elevated blood pressure on the athlete’s initial screening does not represent a definitive diagnosis of hypertension. The number of patients with elevated blood pressure in our study population is alarming; however, similarly high prevalences have been reported in some adolescent populations. In a recent study by Lo et al11 examining the prevalence of hypertension in extremely obese adolescents, the authors reported a 24.2% prevalence of elevated blood pressure during the initial screening. In a school-based screening study from the metropolitan Houston, Texas area, the prevalence of elevated blood pressure screenings on initial screening was found to vary based on race, with the be highest blood pressure values reported in Hispanics (25%), followed by whites (18%), blacks (17%), and Asians (16%).37 In a study of predominantly black minority students, Jago et al10 reported a 23.9% prevalence of elevated blood pressure in a population of eighth grade adolescents. The present study demonstrated similar trends, with elevated blood pressure at initial encounter occurring in 21.4% of high school athletes. An end diagnosis of primary hypertension in pediatric patients requires longitudinal blood pressure tracking or multiple measurements separated by significant time intervals. Definitive diagnosis of hypertension is not a goal or realistic expectation of the PPE for student athletes. Rather, sports medicine providers should work to accurately identify athletes at risk for hypertension and encourage close follow-up with their primary medical providers or medical home.
In the current study, risk factors associated with elevated blood pressure included male sex, obesity, black race, and single-sport athletes. While there is a general consensus that ethnicity is an independent determinant of hypertension risk in adult populations, studies examining this association in pediatric populations have yielded conflicting results.3,17,22,37 In a longitudinal study of adolescent patients over a 10-year period, Dekkers et al3 found that ethnicity was a risk factor for higher systolic and diastolic blood pressure when controlling for growth, sex, adiposity, and socioeconomic status. Conversely, in a study by Sorof et al30 that tracked patients with elevated blood pressure to an end diagnosis of hypertension, the association of ethnicity with elevated blood pressure readings present on their initial screening did not persist after 3 sets of screening measurements. The authors concluded that ethnicity was not an independent determinant of hypertension among individuals within their patient population and highlighted the importance of longitudinal follow-up for obese patients identified as at-risk for hypertension. While our study demonstrated an association between ethnicity and elevated blood pressure, our results represent a first-time encounter and screening for elevated blood pressure, not a definitive diagnosis of hypertension. Longitudinal analysis of our results would be necessary to demonstrate whether this association would persist.
There is debate regarding the long-term health benefits of screening for hypertension in children and adolescents. Screening for hypertension in the ambulatory setting can be laborious, and studies have identified that formal hypertension screening may occur in as few as 35% of pediatric ambulatory visits.14 In a report prepared for the US Preventative Service Task Force regarding blood pressure screening in children, Thompson et al34 concluded that there is no direct evidence that screening for hypertension in children and adolescents reduces the morbidity of disease in adulthood. Screening, however, is recommended for adult populations.14,22 Given the silent nature of hypertension as a disease process, early recognition and management may be the best means of preventing long-term disease morbidity, and therefore, the principles of early diagnosis and preventative management may provide the best means of minimizing long-term morbidity and mortality. Based on our findings, we recommend a standardized approach and routine blood pressure monitoring as an important part of the athlete’s preparticipation physical examination.
Perhaps the most significant finding in our current study is the influence of type and number of sports on the individual’s BMI and blood pressure. As the number of sports reported increased, there was a uniform decrease in the prevalence of obesity, with single-sport athletes being 1.40 and 2.17 times more likely to be obese than 2-sport and ≥3-sport athletes, respectively. Similarly, single-sport athletes were 1.17 and 1.27 times more likely to have elevated blood pressure compared with 2-sport and ≥3-sport athletes, respectively. Recently, there has been increased interest in the prevention of overuse injuries associated with pediatric sports participation.4,9,12 While our study did not differentiate between single-sport, single-season athletes and individuals participating in a single sport on a year-round basis, previous studies have linked year-round participation in a single sport to an increased risk of overuse injury. In addition to the prevention of overuse injury, the results of the current study identify additional general health benefits that may be gained from a diversified year-round approach to sports participation such as a decreased risk for obesity and elevated blood pressure.
It is equally important to note that our study identified certain sports associated with a higher prevalence of obesity. In our patient population, 29.9% of athletes reported participation in football and 15.4% reported participation in basketball. It is not our opinion that these findings should discourage participation in specific sports but rather to highlight the benefits of multiple sports participation. In our methodology, we identified individuals as multisport athletes or single-sport participants for data analysis, believing that this information would provide practitioners with the most accurate tools for risk assessment of their patient populations. In our population, multisport participants were at lower risk for obesity even if they participated in a sport associated with increased BMI. It should be noted that the nature of certain sports—or even positions—may lead to selection bias. Individuals with higher BMIs may be more likely to participate in specific sports or positions. For example, higher BMI body types may excel in sports like football and at positions like offensive and defensive line, while leaner body mass individuals be more suitable for positions like wide receiver or cornerback and be more inclined to participate in other endurance sports. Parents and coaches should be aware of the long-term health risks associated with obesity and encourage athletes to maintain a healthy body weight, especially athletes who participate in sports or positions that may favor or reward athletes with higher BMIs. The prevalence of obesity was significantly lower in individuals who participated in running and endurance sports, and consequently, parents and coaches should consider the benefits of physical education programs emphasizing multisport and endurance sport participation while the athletes are at a younger age.
The results of the current study confirm the progressive nature of the obesity epidemic, which may disproportionately affect individuals living in the southeastern United States.21 While the results of our study may not be generalized to other geographic regions of the United States, this study highlights the contribution of obesity to the worsening cardio metabolic profiles in our population of adolescent athletes, with obese athletes having a 2.33-fold increase in risk for elevated blood pressure. All participants in this study were involved in some form of school-sponsored sport, an activity that presents the individual with routine physical exercise during the season of participation. The CDC recommends that individuals aged 6 to 17 years participate in a minimum of 60 minutes of moderate intensity aerobic activity daily and muscle and bone strengthening exercises at least 3 days per week.24 Our study points out that not all forms of exercise are equal when it comes to examining an individual’s long-term risk for obesity. Finally, this study demonstrates the vital role that many orthopaedic surgeons and sports medicine physicians can play in providing general health-screening examinations and health education to thousands of student athletes each year.
Appendix
Mississippi High School Athletic Association Standardized Preparticipation Physical Examination Form
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: This study was sponsored by the Arthroscopy Association of North America (AANA), which provided reimbursement for travel expenses associated with manuscript presentation at the fall 2014 AANA meeting.
References
- 1. Berenson GS; Bogalusa Heart Study Investigators. Bogalusa Heart Study: a long-term community study of a rural biracial (Black/White) population. Am J Med Sci. 2001;322:293–300. [PubMed] [Google Scholar]
- 2. Bernhardt D, Roberts WO; American Academy of Family Physicians, & American Academy of Pediatrics. PPE: Preparticipation Physical Evaluation. 4th ed Elk Grove Village, IL: American Academy of Pediatrics; 2010. [Google Scholar]
- 3. Dekkers JC, Snieder H, Van Den Oord EJ, Treiber FA. Moderators of blood pressure development from childhood to adulthood: a 10-year longitudinal study. J Pediatr. 2002;141:770–779. [DOI] [PubMed] [Google Scholar]
- 4. DiFiori JP, Benjamin HJ, Brenner J, et al. Overuse injuries and burnout in youth sports: a position statement from the American Medical Society for Sports Medicine. Clin J Sport Med. 2014;24:3–20. [DOI] [PubMed] [Google Scholar]
- 5. Din-Dzietham R, Liu Y, Bielo MV, Shamsa F. High blood pressure trends in children and adolescents in national surveys, 1963 to 2002. Circulation. 2007;116:1488–1496. [DOI] [PubMed] [Google Scholar]
- 6. Fox CK, Barr-Anderson D, Neumark-Sztainer D, Wall M. Physical activity and sports team participation: associations with academic outcomes in middle school and high school students. J Sch Health. 2010;80:31–37. [DOI] [PubMed] [Google Scholar]
- 7. Fishman PA, Anderson ML, Cook AJ, et al. Accuracy of blood pressure measurements reported in an electronic medical record during routine primary care visits. J Clin Hypertens (Greenwich). 2011;13:821–828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hammer LD, Kraemer HC, Wilson DM, Ritter PL, Dornbusch SM. Standardized percentile curves of body-mass index for children and adolescents. Am J Dis Child. 1991;145:259–263. [DOI] [PubMed] [Google Scholar]
- 9. Hill DE, Andrews JR. Stopping sports injuries in young athletes. Clin Sports Med. 2011;30:841–849. [DOI] [PubMed] [Google Scholar]
- 10. Jago R, Harrell JS, McMurray RG, Edelstein S, El Ghormli L, Bassin S. Prevalence of abnormal lipid and blood pressure values among an ethnically diverse population of eighth-grade adolescents and screening implications. Pediatrics. 2006;117:2065–2073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lo JC, Chandra M, Sinaiko A, et al. Severe obesity in children: prevalence, persistence and relation to hypertension. Int J Pediatr Endocrinol. 2014;2014:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lykissas MG, Eismann EA, Parikh SN. Trends in pediatric sports-related and recreation-related Injuries in the United States in the last decade. J Pediatr Orthop. 2013;33:803–810. [DOI] [PubMed] [Google Scholar]
- 13. Lynch BA, Finney Rutten LJ, Jacobson RM, et al. Health care utilization by body mass index in a pediatric population. Acad Pediatr. 2015;15:644–650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Maison P, Byrne CD, Hales CN, Day NE, Wareham NJ. Do different dimensions of the metabolic syndrome change together over time? Evidence supporting obesity as the central feature. Diabetes Care. 2001;24:1758–1763. [DOI] [PubMed] [Google Scholar]
- 15. Miller KE, Sabo DF, Farrell MP, Barnes GM, Melnick MJ. Athletic participation and sexual behavior in adolescents: the different worlds of boys and girls. J Health Soc Behav. 1998;39:108–123. [PubMed] [Google Scholar]
- 16. Miller KE, Sabo DF, Farrell MP, Barnes GM, Melnick MJ. Sports, sexual behavior, contraceptive use, and pregnancy among female and male high school students: testing cultural resource theory. Sociol Sport J. 1999;16:366–387. [DOI] [PubMed] [Google Scholar]
- 17. Mississippi athletic participation form. Retrieved from http://www.misshsaa.com/LinkClick.aspx?fileticket=gUiK2gP1fbw=. Accessed October 15, 2015.
- 18. Must A, Jacques PF, Dallal GE, Bajema CJ, Dietz WH. Long-term morbidity and mortality of overweight adolescents. A follow-up of the Harvard Growth Study of 1922 to 1935. N Engl J Med. 1992;327:1350–1355. [DOI] [PubMed] [Google Scholar]
- 19. NFHS (National Federation of State High School Associations). http://www.nfhs.org/. Accessed October 15, 2015.
- 20. O’Brien SH, Holubkov R, Reis EC. Identification, evaluation, and management of obesity in an academic primary care center. Pediatrics. 2004;114:e154–e159. [DOI] [PubMed] [Google Scholar]
- 21. Ogden CL, Flegal KM, Carroll MD, Johnson CL. Prevalence and trends in overweight among US children and adolescents, 1999-2000. JAMA. 2002;288:1728–1732. [DOI] [PubMed] [Google Scholar]
- 22. Ostchega Y, Dillon CF, Hughes JP, Carroll M, Yoon S. Trends in hypertension prevalence, awareness, treatment, and control in older U.S. adults: data from the National Health and Nutrition Examination Survey 1988 to 2004. J Am Geriatr Soc. 2007;55:1056–1065. [DOI] [PubMed] [Google Scholar]
- 23. Pan WH, Yeh WT. How to define obesity? Evidence-based multiple action points for public awareness, screening, and treatment: an extension of Asian-Pacific recommendations. Asia Pac J Clin Nutr. 2008;17:370–374. [PubMed] [Google Scholar]
- 24. Products—Health United States—Child and Adolescent Health. Table 60 adolescent obesity. http://www.cdc.gov/nchs/hus/child.htm. Accessed October 15, 2015.
- 25. Robinson RF, Batisky DL, Hayes JR, Nahata MC, Mahan JD. Body mass index in primary and secondary pediatric hypertension. Pediatr Nephrol. 2004;19:1379–1384. [DOI] [PubMed] [Google Scholar]
- 26. Rosner B, Prineas R, Daniels SR, Loggie J. Blood pressure differences between blacks and whites in relation to body size among US children and adolescents. Am J Epidemiol. 2000;151:1007–1019. [DOI] [PubMed] [Google Scholar]
- 27. Saydah S, Bullard KM, Imperatore G, Geiss L, Gregg EW. Cardiometabolic risk factors among US adolescents and young adults and risk of early mortality. Pediatrics. 2013;131:e679–e686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Shapiro DJ, Hersh AL, Cabana MD, Sutherland SM, Patel AI. Hypertension screening during ambulatory pediatric visits in the United States, 2000-2009. Pediatrics. 2012;130:604–610. [DOI] [PubMed] [Google Scholar]
- 29. Singh GK, Kogan MD, van Dyck PC. Changes in state-specific childhood obesity and overweight prevalence in the United States from 2003 to 2007. Arch Pediatr Adolesc Med. 2010;164:598–607. [DOI] [PubMed] [Google Scholar]
- 30. Sorof JM, Lai D, Turner J, Poffenbarger T, Portman RJ. Overweight, ethnicity, and the prevalence of hypertension in school-aged children. Pediatrics. 2004;113:475–482. [DOI] [PubMed] [Google Scholar]
- 31. Srinivasan SR, Bao W, Wattigney WA, Berenson GS. Adolescent overweight is associated with adult overweight and related multiple cardiovascular risk factors: the Bogalusa Heart Study. Metabolism. 1996;45:235–240. [DOI] [PubMed] [Google Scholar]
- 32. Stergiou GS, Nasothimiou E, Giovas P, Kapoyiannis A, Vazeou A. Diagnosis of hypertension in children and adolescents based on home versus ambulatory blood pressure monitoring. J Hypertens. 2008;26:1556–1562. [DOI] [PubMed] [Google Scholar]
- 33. Sun SS, Grave GD, Siervogel RM, Pickoff AA, Arslanian SS, Daniels SR. Systolic blood pressure in childhood predicts hypertension and metabolic syndrome later in life. Pediatrics. 2007;119:237–246. [DOI] [PubMed] [Google Scholar]
- 34. Thompson M, Dana T, Bougatsos C, Blazina I, Norris SL. Screening for hypertension in children and adolescents to prevent cardiovascular disease. Pediatrics. 2013;131:490–525. [DOI] [PubMed] [Google Scholar]
- 35. Tonetti L, Fabbri M, Filardi M, Martoni M, Batale V. The association between higher body mass index and poor school performance in high school students [published online October 21, 2015]. Pediatr Obes. doi:10.1111/ijpo.12075. [DOI] [PubMed] [Google Scholar]
- 36. U.S. Preventive Services Task Force. Screening for high blood pressure: U.S. Preventive Services Task Force reaffirmation recommendation statement. Ann Intern Med. 2007;147:783–786. [DOI] [PubMed] [Google Scholar]
- 37. Wattigney WA, Webber LS, Srinivasan SR, Berenson GS. The emergence of clinically abnormal levels of cardiovascular disease risk factor variables among young adults: the Bogalusa Heart Study. Prev Med. 1995;24:617–626. [DOI] [PubMed] [Google Scholar]
- 38. Whitlock EP, Williams SB, Gold R, Smith PR, Shipman SA. Screening and interventions for childhood overweight: a summary of evidence for the US Preventive Services Task Force. Pediatrics. 2005;116:e125–e144. [DOI] [PubMed] [Google Scholar]