Abstract
This study entailed a cross-examination of oxidant/antioxidant balance, high-density lipoprotein (HDL)-linked paraoxonase 1 (PON1) phenotypes, and levels of serum routine lipids among patients with normal tension glaucoma (NTG) or pseudoexfoliative glaucoma (PEXG) compared with healthy control groups. We aimed to investigate the links between oxidative stress (OS), HDL-related antioxidant enzyme activities and dyslipidemia in distinct subtypes of glaucoma. The study included 32 patients with NTG, 31 patients with PEXG, and 40 control subjects. Levels of PON1 and arylesterase enzymatic activity, total oxidant status (TOS), and total antioxidant status were measured by spectrophotometry and OS indexes (OSI) were calculated. The phenotype distribution of PON1 was determined using the dual substrate method. Blood serum levels of HDL, low-density lipoprotein, total cholesterol (TC), and triglyceride (TG) were measured. The TOS and OSI values in the NTG group were significantly higher compared with the other groups (both p < 0.01). The phenotype distribution found in the glaucoma and control groups were NTG: QQ, 59.4%; QR, 37.5%; RR, 3.1%; PEXG: QQ, 45.1%; QR, 48.4%; RR, 6.5%; and in the control group: QQ, 42.5%; QR, 50.0%; RR, 7.5%. Serum TC levels were significantly higher than the control in both NTG and PEXG groups, whereas TG was significantly higher in NTG only (p < 0.01 and p < 0.02, respectively). Hyperlipidemia, OS and variations in phenotype distribution of PON1 may play a role in the pathogenesis of different types of glaucoma.
KEY WORDS: Oxidative stress, paraoxonase, high-density lipoprotein, hyperlipidemia, normal tension glaucoma, pseudoexfoliative glaucoma, paraoxonase 1 phenotype
INTRODUCTION
Glaucoma is a continuous optic neuropathy, commonly caused by elevated intraocular pressure (IOP) levels due to resistance to aqueous humor drainage through the trabecular meshwork (TM) and Schlemm’s canal [1]. Primary open-angle glaucoma (POAG) is chronic and painless and often has no symptoms until the disease has progressed significantly. The underlying biological cause of open-angle glaucoma remains unclear [2]. Most notably, endothelium of the TM behaves like vascular endothelium. Recent studies have identified increasing similarities between blockage of the TM and endothelial dysfunction (e.g., atherosclerosis) [3,4].
Even though high IOP has been found to be the most common risk factor for glaucoma, in normal tension glaucoma (NTG), a subtype of POAG, the IOP of afflicted patients remains within normal limits. Little is known about the pathophysiologic mechanism of NTG [5]. Various systemic factors, such as dyslipidemia and oxidative stress (OS), are believed to trigger and increase the severity of the disorder [6,7]. Pseudoexfoliation glaucoma (PEXG) is also associated with OS, in which abnormal extracellular fibrillar material is accumulated in the eye, obstructing humor drainage [8]. PEX syndrome (PEX) is, in fact, an age-related systemic disorder of the extracellular matrix, also observed in the vascular system and various organs [9-13].
The human serum paraoxonase 1 (PON1) refers to a high-density lipoprotein (HDL)-linked A-esterase glycoenzyme that increases the antioxidant and anti-atherosclerotic potential of HDL [14]. PON1 is a promiscuous enzyme capable of hydrolyzing oxidized HDL, low-density lipoprotein (LDL) and other lipids, various esters, and other chemicals [15]. Expression of human PON1 in mouse models of atherosclerosis have been shown to reduce circulating oxidized LDL, macrophage OS, and foam cell formation, and normalize endothelial function, thus retarding atherosclerosis [16,17]. Significantly, low PON1 activity is associated with dysfunctional HDL [18].
Polymorphisms of the PON1 gene have been shown to be capable of affecting the performance of PON1 [19,20]. In terms of enzymatic activity, human serum PON1 is present in two main polymorphic forms varying at amino acid position 192, namely Q192 (glutamine, wild-type) and R192 (arginine, variant). Importantly, the polymorphic characteristics of PON1 depend on the substrate. The Q alloenzyme is less efficient in hydrolyzing paraoxon but more efficient toward oxidized lipoproteins than the R alloenzyme [21]. By dividing the PON activity by the arylesterase (ARE) activity of serum PON1 (double substrate method), three phenotypes were defined, namely QQ, QR, and RR [22]. Interestingly, the PON1 genotypes of individuals do not precisely correspond to these phenotypes, indicating that factors other than polymorphism contribute to the PON1 profile. Therefore, PON1 activity is regarded as a more suitable indicator of disease compared to genotyping alone [23,24].
Although easier, measuring concentrations of individual oxidants and antioxidants in serum is not a practical approach. The oxidant and antioxidant potential of a biological specimen should be calculated in total to be physiologically meaningful. The studies demonstrating higher levels of serum systemic OS in POAG and PEXG patients cited above may not be sufficiently comprehensive in that they included different OS markers, analyzed only one glaucoma type or unclassified mixed types of glaucoma in the case group, and/or analyzed either the pro-oxidant or antioxidant status only. This study aims to analyze serum total oxidant and antioxidant potentials in NTG and PEXG patients separately. Furthermore, phenotypic distribution of PON1 among NTG patients is determined by the double substrate method for the first time.
MATERIALS AND METHODS
Subjects
This case-control study included 32 patients with NTG, 31 patients with PEXG and 40 control subjects. The study was approved by the local ethics committee of the hospital and was carried out in accordance with the principles of the Declaration of Helsinki. All groups involved in the study underwent a thorough ophthalmological investigation. Corrected Snellen chart visual acuity tests, slit-lamp microscope investigation for the anterior and posterior segments, gonioscopic testing, and IOP measurements with Goldmann applanation tonometry and with corneal thickness were performed.
Patients with an IOP of 21 mmHg or lower, displaying glaucomatous changes in the optic disc (atrophy, neuroretinal rim loss and peripapillary hemorrhage) and in the visual field were diagnosed as having NTG. PEX was diagnosed by slit-lamp microscope investigation following mydriasis, provided that typical presence of a pseudoexfoliation component was found on the anterior lens capsule or the pupillary border. A diagnosis of PEXG was given if the results for the anterior segment of the pseudoexfoliative component showed an IOP exceeding 21 mmHg without typical optic nerve head changes or visual field effects. Patients of matching ages with an IOP of ≤21 mmHg that had normal optical appearances with non-visual effects were classified as control subjects.
Dilated fundus investigation was made with a 90-dioptre lens, and all fundus parameters were examined through spectral domain optical coherence tomography (SD-OCT) using the Cirrus high-definition-OCT device. SD-OCT was performed following three different protocols. The initial protocol entailed the macular cube 512 × 128, in which the macula was classified into nine areas according to retinal thickness, coupled with the measuring of ganglion cell-inner plexiform layer thickness in each area. The second protocol involved the optic disc cube for each of the four quadrants (upper, lower, nasal and temporal), in which the peripapillary retinal nerve fiber layer thickness was determined. The third protocol entailed the assessment of the optic disc region, optic rim region, optic cup region, vertical and horizontal disc or cup ratio, and the parametric symmetry of both discs. The Octopus 900 perimeter was used for the visual field test with a 30° white stimulant. The visual field evaluation was done by using the mean deviation of the decibel values.
Detailed medical histories were also obtained from each patient. Those with other ocular diseases (such as diabetic retinopathy, age-related maculopathy, and uveitis), kidney diseases and any central nervous system diseases that might interfere with the visual field test were excluded from this study. All subjects were asked whether they smoked or took specific medication (including non-steroidal anti-inflammatory drugs, supplemental vitamin C and/or vitamin E, and diuretics); those that answered in the affirmative were excluded from the study.
All of the study subjects were selected and designated into groups by an ophthalmologist while subsequent laboratory tests were performed by a biochemist who was not informed of the groupings to achieve single-blind assessment.
Measurement of PON1 and ARE enzyme activities in serum
PON1 and ARE enzyme activities were measured using commercially available kits (Relassay®, Gaziantep/Turkey). The fully automated PON1 activity measurement method consists of two different sequential reagents; the first reagent is an appropriate Tris buffer containing calcium ions, which is a cofactor of PON1 enzyme. A linear increase in the absorbance of p-nitrophenol, produced from paraoxon, is followed in a kinetic measurement mode. The non-enzymatic hydrolysis of paraoxon was subtracted from the total rate of hydrolysis. The molar absorptivity of p-nitrophenol is 1829 m2/mol and 1 U of PON1 activity is equal to 1 mol of paraoxon hydrolyzed per liter per minute at 37°C [25].
Phenyl acetate was used as a substrate to measure ARE activity. PON1, present in the sample, hydrolyses phenyl acetate to its products, phenol, and acetic acid. The produced phenol is colorimetrically measured via oxidative coupling with 4-aminoantipyrine and potassium ferricyanide. Non-enzymatic hydrolysis of phenyl acetate was then subtracted from the total rate of hydrolysis. The molar absorptivity of the colored complex is 400 m2/mol and 1 U of ARE activity is equal to 1 mmol of phenyl acetate hydrolyzed per liter per minute at 37°C [26]. Double-distilled water (ddH2O) was used as a negative control during spectrometry.
PON1 phenotype distribution
The genetic polymorphism Q192R is responsible for three phenotypes: QQ, QR, and RR for low, intermediate and high PON1 activity, respectively. The phenotypic distribution of PON1 was determined using the dual substrate method. The ratio of paraoxon hydrolysis in the presence of 1 mol/L NaCl (salt stimulated PON1 [stPON1]) to phenyl acetate hydrolysis was used to assign individuals to one of the phenotypes [25]. The ratio provided by dividing salt-stimulated PON1 by ARE enzyme activity demonstrated a trimodal PON1 phenotype distribution in the whole study population. Accordingly, the cut-off values for assigning a participant to a phenotype were <2.0 for QQ, 2.0-5.0 for QR and >5.0 for RR (Figure 1).
FIGURE 1.
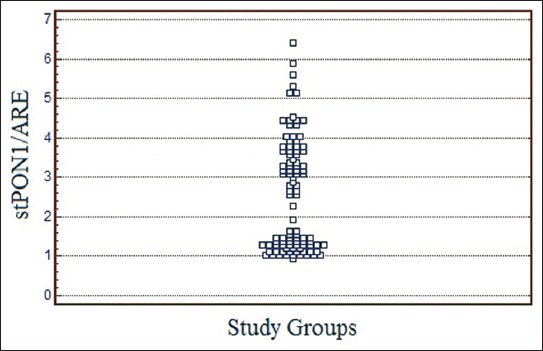
Distribution of paraoxonase 1 (PON1) phenotype in whole study group. Each square represents one subject. The y axis represents the enzyme activity ratio used for assigning PON1 phenotype groups. The cut-off values for assigning a subject to a phenotype are <2.0 for QQ, 2.0 to 5.0 for QR and >5.0 for RR. PON1: High-density lipoprotein-linked paraoxonase 1; stPON1: Salt-stimulated PON1 activity; ARE: Arylesterase.
Measurement of serum total oxidant status (TOS)
Serum TOS levels were analyzed by using a novel automated colorimetric measurement method developed by Erel [27]. In this method, oxidants in the sample oxidize the ferrous ion-chelator complex to a ferric ion which makes a colored complex with a chromogen in an acidic medium. The color intensity, which can be measured spectrophotometrically, is related to the total amount of oxidant molecules present in the sample. The results are expressed in terms of micromoles of hydrogen peroxide equivalent per liter (μmol H2O2 equivalent/L) ddH2O was used as a negative control during spectrometry.
Measurement of serum total antioxidant status (TAS)
Serum TAS levels were analyzed by using a novel automated colorimetric measurement method developed by Erel [28]. In this method, antioxidants in the sample reduce dark blue-green colored 2,2’-azino-bis (3-ethylbenzthiazoline-6-sulphonic acid) (ABTS) radical to colorless reduced ABTS form. The change of absorbance at 660 nm is related with the total antioxidant level of the sample. This method determines the anti-oxidative effect of the sample against the potent free radical reactions initiated by the produced hydroxyl radical. The results are expressed as micromoles of Trolox equivalent per liter (μmol Trolox equivalent/L) ddH2O was used as negative control during spectrometry.
OS index (OSI)
The percentage ratio of TOS level to TAS level was suggested as OSI [29]. The OSI value was calculated according to the following formula: OSI (arbitrary unit) = TOS (micromolar hydrogen peroxide equivalent per liter)/TAS (micromolar Trolox equivalent per liter).
Routine parameters
The levels of triglycerides (TG), total cholesterol (TC), HDL cholesterol and LDL cholesterol were determined by using commercially available assay kits (Abbott, Illinois/USA) with an autoanalyzer (Architect® c16000, Abbott Diagnostics, Illinois/USA).
Statistical analysis
Statistical analyses were performed using the statistical software MedCalc®, version 11.5.1.0 (MedCalc Software, Ostend/Belgium). Kolmogorov–Smirnov test was used to determine normality of data distribution. In normally distributed groups, the results were presented with mean and standard deviation. The significance of the differences between groups was determined by the Student’s unpaired t-test for normal distributions, and by the Mann–Whitney U-test in abnormal distributions. The significance of the association between categorical variables was evaluated by using Chi-square test. Differences with p < 0.05 were accepted as significant.
RESULTS
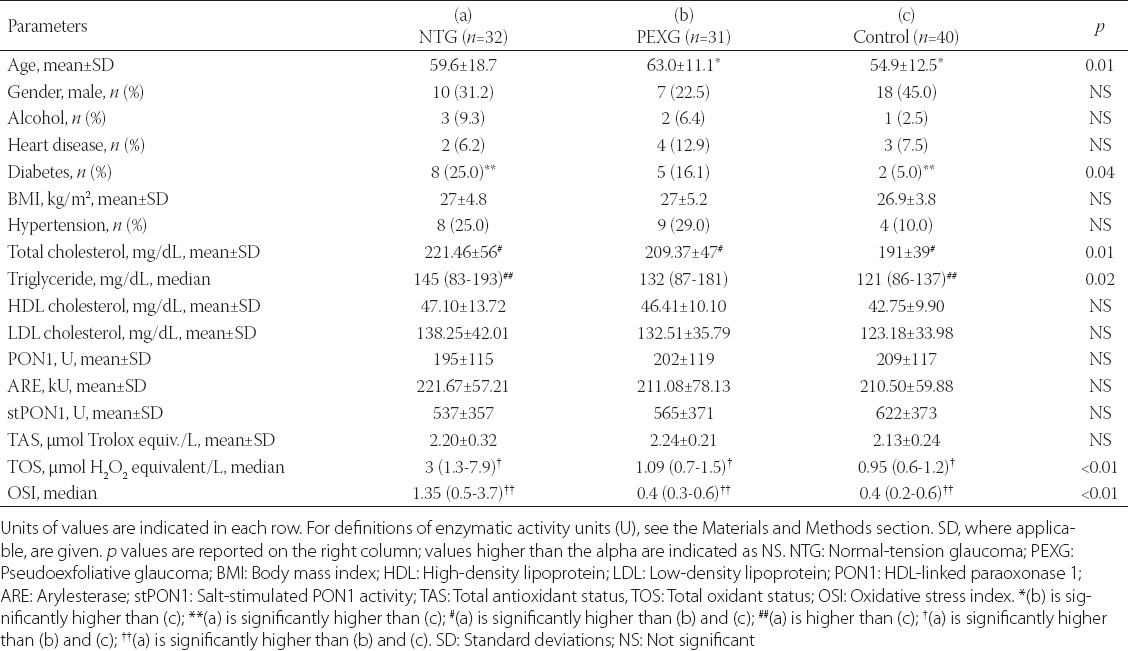
Demographic and blood serum parameters of glaucoma patients (NTG and PEXG) and healthy controls, collected by patient history and biochemical analysis, are given in Table 1. The gender, smoking and alcohol consumption status, heart disease and hypertension frequency, and body mass index, of the glaucoma patients and control subjects were similar. Lipid parameters showed variation; TC levels were significantly higher in the NTG group compared to the PEXG group and controls (p = 0.01), and TG levels were significantly higher in NTG patients compared with the control group (p = 0.002). The PEXG patients were significantly older than those in the other groups (p = 0.01) as expected, since the disorder is age-related. Diabetes was more prevalent in patients with NTG compared with the control subjects (p = 0.04). There was no indicative variation between the patients with glaucoma and control subjects in terms of PON1, ARE, stPON1, or TAS levels. However, the oxidant parameters (TOS and OSI) were significantly higher in the NTG group compared to the other two (p < 0.01 for both).
TABLE 1.
Demographic and blood serum parameters of glaucoma patients (NTG and PEXG) and healthy controls
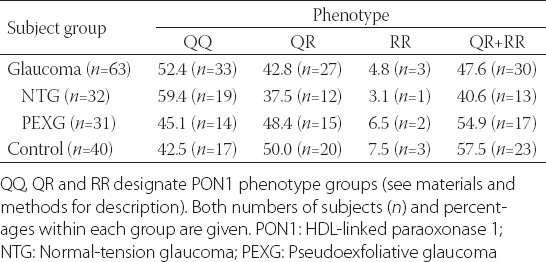
The phenotypic distribution of PON1 activity in the study group is shown in Figure 1. Distribution in the NTG and PEXG groups as well as the healthy controls is given in Table 2. The QQ (low activity) phenotype appeared more dominant in the NTG group compared to the PEXG and control groups, but the difference was not significant.
TABLE 2.
Phenotypic distribution of PON1 activity in glaucoma patients (cumulative, NTG and PEXG) and healthy controls
DISCUSSION
In its late stage, glaucoma is a neurodegenerative disorder, in which loss of retinal ganglion cells leads to blindness. On the other hand, deterioration of TM structure and function is prevalent in open-angle glaucoma. Considering the similarities between TM and vascular endothelium, POAG may be perceived as a vascular disorder [3,4]. In agreement, dyslipidemia, coronary arterial disease, and vascular malfunction are comorbid with glaucoma. PEXG is also manifested secondary to a systemic disorder, PEX, which affects the extracellular matrix. Interestingly, even though the two subtypes of glaucoma are caused by different mechanisms, OS is associated with both. In our study, we aimed to explore this phenomenon by comparing parameters related to oxidative balance in NTG and PEXG.
The oxidant/antioxidant parameters in PEX and PEXG patients has been studied extensively and OS markers were found to have risen, while antioxidants have diminished, resulting in an oxidative balance in favor of oxidants [9-13]. There are fewer studies on NTG, but an increase in OS has been associated with it nonetheless [6,7]. We were able to find only one paper comparing PEXG and NTG directly in this frame. Tanito et al. have found no significant difference in the biological antioxidant capacity or levels of reactive oxygen metabolites and sulfhydryl groups (an estimate of total thiol groups) in serum between PEXG and NTG patients [12]. In contrast, our analysis has shown that TOS and OSI values in the NTG group were significantly higher than those in PEXG and control groups. This variation might indicate that the etiopathogenesis of NTG and PEXG might differ in relation to OS. It must be noted that the cited study was carried out in Japan, while our subjects were of Caucasian background.
PON1 is a key element of HDL function in terms of lipid metabolism and OS/damage, in addition to its antithrombotic and anti-atherogenic characteristics [15,20]. The role of PON1 in various systemic diseases is established in the literature, but its relation to glaucoma is not yet determined. Considering the link between OS and glaucoma, HDL and PON1 are factors of interest for research. HDL containing the PON1 R alloenzyme has been shown to be less effective in protecting LDL from oxidation than the Q alloenzyme [30]. There are three studies that have investigated into this phenomenon. The first two performed genotype analysis in Asian populations, one of which identified significantly higher R192 frequency in POAG patients compared to healthy controls [31]. The other, in contrast, has failed to find any statistically meaningful allelic distribution of the Q192R polymorphism between POAG, NTG or control groups [32]. Interestingly, the same study has established a positive regression between IOP levels and carrying the R192 allele (one or two copies) for both glaucoma patients and healthy controls. The third such paper has determined the PON1 phenotypes of subjects instead of genotyping, which is considered the better criterion of the two (see introduction). Demirogen et al. have shown that the incidence of people exhibiting RR phenotype was higher in PEX patients compared to the control group, but the difference was not significant for PEXG patients [13]. Our analysis, which was performed on Caucasian subjects like the study last referred to, has not identified any statistically significant variation within PON1 phenotypes of PEXG, NTG and control groups, although a slight increase in QQ phenotype was present in NTG patients. One should note that the distribution of PON1 alleles, as well as IOP levels of glaucomatous eyes varies greatly between Asian and Caucasian populations, further complicating any conclusions to be drawn [32]. More research is needed to elucidate the role of PON1 function regarding glaucoma. It is not beyond reason to assume that PON1 function is clinically important, yet difficult to prove statistically.
Parallel to inconstant PON1 activity, the significance of HDL lies in its quality, rather than quantity. HDL is a dynamic complex with over 200 known associated proteins and embodies vast functional heterogeneity, leading to the introduction of the “HDL functionality” concept [19,33,34]. Having presumed glaucoma a vascular disorder, one should investigate the role of dyslipidemia in its etiopathogenesis. Indeed, there is research showing increased levels of TC, TG and LDL, and decreased HDL in POAG and NTG patients [35-37]. Furthermore, one population analysis has linked dyslipidemia with increased IOP in people not receiving glaucoma treatment, suggesting that hyperlipidemia may play a role in the onset of glaucoma [38]. In this study, we have found higher levels of TC in glaucoma patients and TG in NTG patients only, compared to healthy controls. Signs of hyperlipidemia were more evident in the NTG group and were accompanied by higher TOS and OSI values. Hyperlipidemia is known to cause OS due to elevated levels of ROS, indicating that the observed status in NTG patients may be systemic.
We hypothesize that a causal relationship may exist between NTG and hyperlipidemia-related pathologies, which may be explained by systemic OS and dysregulation of the optic neuronal cellular stress response. The high rates of TC and TG among patients with NTG could be attributed to vascular endothelial malfunction. Importantly, research suggests that statins could offer some protection against glaucoma [39,40]. These findings suggest not only that treatment for hyperlipidemia may be effective against glaucoma, but also that routine serum lipid tests may be used to predict glaucoma.
CONCLUSION
Our results suggest that hyperlipidemia may be associated with glaucoma. Further research is needed to elucidate if this association is causative for glaucoma onset.
DECLARATION OF INTERESTS
The authors declare no conflict of interest.
REFERENCES
- [1].Casson RJ, Chidlow G, Wood JP, Crowston JG, Goldberg I. Definition of glaucoma:Clinical and experimental concepts. Clin Experiment Ophthalmol. 2012;40(4):341–9. doi: 10.1111/j.1442-9071.2012.02773.x. http://dx.doi.org/10.1111/j.1442-9071.2012.02773.x . [DOI] [PubMed] [Google Scholar]
- [2].Weinreb RN, Aung T, Medeiros FA. The pathophysiology and treatment of glaucoma:A review. JAMA. 2014;311(18):1901–11. doi: 10.1001/jama.2014.3192. http://dx.doi.org/10.1001/jama.2014.3192 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Saccà SC, Centofanti M, Izzotti A. New proteins as vascular biomarkers in primary open angle glaucomatous aqueous humor. Invest Ophthalmol Vis Sci. 2012;53(7):4242–53. doi: 10.1167/iovs.11-8902. http://dx.doi.org/10.1167/iovs.11-8902 . [DOI] [PubMed] [Google Scholar]
- [4].Saccà SC, Pulliero A, Izzotti A. The dysfunction of the trabecular meshwork during glaucoma course. J Cell Physiol. 2015;230(3):510–25. doi: 10.1002/jcp.24826. http://dx.doi.org/10.1002/jcp.24826 . [DOI] [PubMed] [Google Scholar]
- [5].Mi XS, Yuan TF, So KF. The current research status of normal tension glaucoma. Clin Interv Aging. 2014;9:1563–71. doi: 10.2147/CIA.S67263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Pinazo-Durán MD, Gallego-Pinazo R, García-Medina JJ, Zanón-Moreno V, Nucci C, Dolz-Marco R, et al. Oxidative stress and its downstream signaling in aging eyes. Clin Interv Aging. 2014;9:637–52. doi: 10.2147/CIA.S52662. http://dx.doi.org/10.2147/CIA.S52662 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Nitta E, Hirooka K, Tenkumo K, Fujita T, Nishiyama A, Nakamura T, et al. Aldosterone:A mediator of retinal ganglion cell death and the potential role in the pathogenesis in normal-tension glaucoma. Cell Death Dis. 2013;4:e711. doi: 10.1038/cddis.2013.240. http://dx.doi.org/10.1038/cddis.2013.240 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Schlötzer-Schrehardt U, Naumann GO. Ocular and systemic pseudo exfoliation syndrome. Am J Ophthalmol. 2006;141(5):921–37. doi: 10.1016/j.ajo.2006.01.047. http://dx.doi.org/10.1016/j.ajo.2006.01.047 . [DOI] [PubMed] [Google Scholar]
- [9].Gartaganis SP, Patsoukis NE, Nikolopoulos DK, Georgiou CD. Evidence for oxidative stress in lens epithelial cells in pseudoexfoliation syndrome. Eye (Lond) 2007;21(11):1406–11. doi: 10.1038/sj.eye.6702596. http://dx.doi.org/10.1038/sj.eye.6702596 . [DOI] [PubMed] [Google Scholar]
- [10].Koliakos GG, Befani CD, Mikropoulos D, Ziakas NG, Konstas AG. Pro-oxidant-antioxidant balance, peroxide and catalase activity in the aqueous humour and serum of patients with exfoliation syndrome or exfoliative glaucoma. Graefes Arch Clin Exp Ophthalmol. 2008;246(10):1477–83. doi: 10.1007/s00417-008-0871-y. http://dx.doi.org/10.1007/s00417-008-0871-y . [DOI] [PubMed] [Google Scholar]
- [11].Borazan M, Karalezli A, Kucukerdonmez C, Bayraktar N, Kulaksizoglu S, Akman A, et al. Aqueous humor and plasma levels of vascular endothelial growth factor and nitric oxide in patients with pseudoexfoliation syndrome and pseudo exfoliation glaucoma. J Glaucoma. 2010;19(3):207–11. doi: 10.1097/IJG.0b013e3181aae93e. http://dx.doi.org/10.1097/IJG.0b013e3181aa.e93e . [DOI] [PubMed] [Google Scholar]
- [12].Tanito M, Kaidzu S, Takai Y, Ohira A. Status of systemic oxidative stresses in patients with primary open-angle glaucoma and pseudoexfoliation syndrome. PLoS One. 2012;7(11):e49680. doi: 10.1371/journal.pone.0049680. http://dx.doi.org/10.1371/journal.pone.0049680 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Demirdögen BC, Ceylan OM, Isikoglu S, Mumcuoglu T, Erel O. Evaluation of oxidative stress and paraoxonase phenotypes in pseudoexfoliation syndrome and pseudoexfoliation glaucoma. Clin Lab. 2014;60(1):79–86. doi: 10.7754/clin.lab.2013.121229. [DOI] [PubMed] [Google Scholar]
- [14].Yilmaz N. Relationship between paraoxonase and homocysteine:Crossroads of oxidative diseases. Arch Med Sci. 2012;8(1):138–53. doi: 10.5114/aoms.2012.27294. http://dx.doi.org/10.5114/aoms.2012.27294 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Mackness M, Mackness B. Human paraoxonase-1 (PON1):Gene structure and expression, promiscuous activities and multiple physiological roles. Gene. 2015;567(1):12–21. doi: 10.1016/j.gene.2015.04.088. http://dx.doi.org/10.1016/j.gene.2015.04.088 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Rozenberg O, Shih DM, Aviram M. Paraoxonase 1 (PON1) attenuates macrophage oxidative status:Studies in PON1 transfected cells and in PON1 transgenic mice. Atherosclerosis. 2005;181(1):9–18. doi: 10.1016/j.atherosclerosis.2004.12.030. http://dx.doi.org/10.1016/j.atherosclerosis.2004.12.030 . [DOI] [PubMed] [Google Scholar]
- [17].Guns PJ, Van Assche T, Verreth W, Fransen P, Mackness B, Mackness M, et al. Paraoxonase 1 gene transfer lowers vascular oxidative stress and improves vasomotor function in apolipoprotein E-deficient mice with pre-existing atherosclerosis. Br J Pharmacol. 2008;153(3):508–16. doi: 10.1038/sj.bjp.0707585. http://dx.doi.org/10.1038/sj.bjp.0707585 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Eren E, Ellidag HY, Aydin O, Yilmaz N. HDL functionality and crystal-based sterile inflammation in atherosclerosis. Clin Chim Acta. 2015;439:18–23. doi: 10.1016/j.cca.2014.09.024. http://dx.doi.org/10.1016/j.cca.2014.09.024 . [DOI] [PubMed] [Google Scholar]
- [19].Eren E, Yilmaz N, Aydin O, Ellidag HY. Anticipatory role of high density lipoprotein and endothelial dysfunction:An overview. Open Biochem J. 2014;8:100–6. doi: 10.2174/1874091X01408010100. http://dx.doi.org/10.2174/1874091X01408010100 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Eren E, Ellidag HY, Aydin O, Yilmaz N. Homocysteine, paraoxonase-1 and vascular endothelial dysfunction:Omnibus viis romam pervenitur. J Clin Diagn Res. 2014;8(9):CE01–4. doi: 10.7860/JCDR/2014/7827.4773. http://dx.doi.org/10.7860/jcdr/2014/7827.4773 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Aviram M, Hardak E, Vaya J, Mahmood S, Milo S, Hoffman A, et al. Human serum paraoxonases (PON1) Q and R selectively decrease lipid peroxides in human coronary and carotid atherosclerotic lesions:PON1 esterase and peroxidase-like activities. Circulation. 2000;101(21):2510–7. doi: 10.1161/01.cir.101.21.2510. http://dx.doi.org/10.1161/01.CIR.101.21.2510 . [DOI] [PubMed] [Google Scholar]
- [22].Eckerson HW, Romson J, Wyte C, La Du BN. The human serum paraoxonase polymorphism:Identification of phenotypes by their response to salts. Am J Hum Genet. 1983;35(2):214–27. [PMC free article] [PubMed] [Google Scholar]
- [23].Richter RJ, Furlong CE. Determination of paraoxonase (PON1) status requires more than genotyping. Pharmacogenetics. 1999;9(6):745–53. [PubMed] [Google Scholar]
- [24].Mackness B, Davies GK, Turkie W, Lee E, Roberts DH, Hill E, et al. Paraoxonase status in coronary heart disease:Are activity and concentration more important than genotype? Arterioscler Thromb Vasc Biol. 2001;21(9):1451–7. doi: 10.1161/hq0901.094247. http://dx.doi.org/10.1161/hq0901.094247 . [DOI] [PubMed] [Google Scholar]
- [25].Eckerson HW, Wyte CM, La Du BN. The human serum paraoxonase/arylesterase polymorphism. Am J Hum Genet. 1983;35(6):1126–38. [PMC free article] [PubMed] [Google Scholar]
- [26].Haagen L, Brock A. A new automated method for phenotyping arylesterase (EC 3.1.1.2) based upon inhibition of enzymatic hydrolysis of 4-nitrophenyl acetate by phenyl acetate. Eur J Clin Chem Clin Biochem. 1992;30(7):391–5. doi: 10.1515/cclm.1992.30.7.391. http://dx.doi.org/10.1515/cclm.1992.30.7.391 . [DOI] [PubMed] [Google Scholar]
- [27].Erel O. A new automated colorimetric method for measuring total oxidant status. Clin Biochem. 2005;38(12):1103–11. doi: 10.1016/j.clinbiochem.2005.08.008. http://dx.doi.org/10.1016/j.clinbiochem.2005.08.008 . [DOI] [PubMed] [Google Scholar]
- [28].Erel O. A novel automated direct measurement method for total antioxidant capacity using a new generation, more stable ABTS radical cation. Clin Biochem. 2004;37(4):277–85. doi: 10.1016/j.clinbiochem.2003.11.015. http://dx.doi.org/10.1016/j.clinbiochem.2003.11.015 . [DOI] [PubMed] [Google Scholar]
- [29].Kosecik M, Erel O, Sevinc E, Selek S. Increased oxidative stress in children exposed to passive smoking. Int J Cardiol. 2005;100(1):61–4. doi: 10.1016/j.ijcard.2004.05.069. http://dx.doi.org/10.1016/j.ijcard.2004.05.069 . [DOI] [PubMed] [Google Scholar]
- [30].Mackness B, Mackness MI, Arrol S, Turkie W, Durrington PN. Effect of the human serum paraoxonase 55 and 192 genetic polymorphisms on the protection by high density lipoprotein against low density lipoprotein oxidative modification. FEBS Lett. 1998;423(1):57–60. doi: 10.1016/s0014-5793(98)00064-7. http://dx.doi.org/10.1016/S0014-5793(98)00064-7 . [DOI] [PubMed] [Google Scholar]
- [31].Zhou G, Liu B. Single nucleotide polymorphisms of metabolic syndrome-related genes in primary open angle glaucoma. Int J Ophthalmol. 2010;3(1):36–42. doi: 10.3980/j.issn.2222-3959.2010.01.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Inagaki Y, Mashima Y, Funayama T, Ohtake Y, Fuse N, Yasuda N, et al. Paraoxonase 1 gene polymorphisms influence clinical features of open-angle glaucoma. Graefes Arch Clin Exp Ophthalmol. 2006;244(8):984–90. doi: 10.1007/s00417-005-0200-7. http://dx.doi.org/10.1007/s00417-005-0200-7 . [DOI] [PubMed] [Google Scholar]
- [33].Eren E, Yilmaz N, Aydin O. High density lipoprotein and it’s dysfunction. Open Biochem J. 2012;6:78–93. doi: 10.2174/1874091X01206010078. http://dx.doi.org/10.2174/1874091X01206010078 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Shah AS, Tan L, Long JL, Davidson WS. Proteomic diversity of high density lipoproteins:Our emerging understanding of its importance in lipid transport and beyond. J Lipid Res. 2013;54(10):2575–85. doi: 10.1194/jlr.R035725. http://dx.doi.org/10.1194/jlr.R035725 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Pavljasevic S, Asceric M. Primary open-angle glaucoma and serum lipids. Bosn J Basic Med Sci. 2009;9(1):85–8. doi: 10.17305/bjbms.2009.2863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Kim MJ, Kim MJ, Kim HS, Jeoung JW, Park KH. Risk factors for open-angle glaucoma with normal baseline intraocular pressure in a young population:The Korea National Health and Nutrition Examination Survey. Clin Experiment Ophthalmol. 2014;42(9) doi: 10.1111/ceo.12347. http://dx.doi.org/10.1111/ceo.12347 . [DOI] [PubMed] [Google Scholar]
- [37].Modrzejewska M, Grzesiak W, Zaborski D, Modrzejewska A. The role of lipid dysregulation and vascular risk factors in glaucomatous retrobulbar circulation. Bosn J Basic Med Sci. 2015;15(2):50–6. doi: 10.17305/bjbms.2015.299. http://dx.doi.org/10.17305/bjbms.2015.299 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Kim YH, Jung SW, Nam GE, Do Han K, Bok AR, Baek SJ, et al. High intraocular pressure is associated with cardiometabolic risk factors in South Korean men:Korean National Health and Nutrition Examination Survey 2008-2010. Eye (Lond) 2014;28(6):672–9. doi: 10.1038/eye.2014.43. http://dx.doi.org/10.1038/eye.2014.43 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Marcus MW, Müskens RP, Ramdas WD, Wolfs RC, De Jong PT, Vingerling JR, et al. Cholesterol-lowering drugs and incident open-angle glaucoma:A population-based cohort study. PLoS One. 2012;7(1):e29724. doi: 10.1371/journal.pone.0029724. http://dx.doi.org/10.1371/journal.pone.0029724 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Stein JD, Newman-Casey PA, Talwar N, Nan B, Richards JE, Musch DC. The relationship between statin use and open-angle glaucoma. Ophthalmology. 2012;119(10):2074–81. doi: 10.1016/j.ophtha.2012.04.029. http://dx.doi.org/10.1016/j.ophtha.2012.04.029 . [DOI] [PMC free article] [PubMed] [Google Scholar]


