Abstract
Objective
Assessing local health departments' (LHDs') informatics capacities is important, especially within the context of broader, systems-level health reform. We assessed a nationally representative sample of LHDs' adoption of information systems and the factors associated with adoption and implementation by examining electronic health records, health information exchange, immunization registry, electronic disease reporting system, and electronic laboratory reporting.
Methods
We used data from the National Association of County and City Health Officials' 2013 National Profile of LHDs. We performed descriptive statistics and multinomial logistic regression for the five implementation-oriented outcome variables of interest, with three levels of implementation (implemented, plan to implement, and no activity). Independent variables included infrastructural and financial capacity and other characteristics associated with informatics capacity.
Results
Of 505 LHDs that responded to the survey, 69 (13.5%) had implemented health information exchanges, 122 (22.2%) had implemented electronic health records, 245 (47.5%) had implemented electronic laboratory reporting, 368 (73.0%) had implemented an electronic disease reporting system, and 416 (83.8%) had implemented an immunization registry. LHD characteristics associated with health informatics adoption included provision of greater number of clinical services, greater per capita public health expenditures, health information systems specialists on staff, larger population size, decentralized governance system, one or more local boards of health, metropolitan jurisdiction, and top executive with more years in the job.
Conclusion
Many LHDs lack health informatics capacity, particularly in smaller, rural jurisdictions. Cross-jurisdictional sharing, investment in public health informatics infrastructure, and additional training may help address these shortfalls.
Public health informatics is the systematic application of information, analytics, computer science, and technology to support the day-to-day work of public health, including surveillance, quality improvement, research, reporting, and health promotion.1 It implies the electronic exchange of data to support public health operations.2 Information is a central driving force for population health improvement,3 and use of that information requires an information technology (IT) infrastructure. In the early 2000s, IT infrastructure became central in health discussions as a facilitator of knowledge, an enabler of consultations across distances, and a means of making job performance more efficient.4 What began as a conversation around the use of personal computers to systematically organize and report surveillance information has evolved into the field of public health informatics.5
The Health Information Technology for Economic and Clinical Health (HITECH) Act spurred the adoption and use of health IT in the United States, especially electronic health records (EHRs).6–8 HITECH's provisions and funding have the potential to affect the way local health departments (LHDs) receive and use information,9 although the primary purpose of the HITECH Act was to improve clinical care. Eligible systems and professionals can receive technical assistance through the HITECH Act in planning and implementing EHRs and participating in data exchanges.10 LHDs have opportunities for partnerships with eligible providers and hospitals for compliance with their own federal requirements for meaningful use of EHRs.11
Across the country, LHDs use various information systems (ISs), including EHRs,12 health information exchanges (HIEs), immunization registries (IRs), electronic disease reporting systems (EDRSs), electronic laboratory reporting (ELR), and electronic syndromic surveillance (ESS) systems. However, all LHDs may not have uniform access to these systems.13–15 LHD informatics capacity allows ESS systems to detect influenza-like illnesses, bioterrorism events, and foodborne illnesses. Increased use of EHRs and laboratory systems, as well as improved speed, ascertainment, and reusability of surveillance information, have enabled public health agencies to receive and process data in near real time.16 Although LHDs may potentially use any or all of these systems in their day-to-day work, in practice, these information-related capacities may not exist. Given that health informatics has undergone rapid changes in recent years, and that the existing studies on the local public health agencies' informatics capacity and its determinants have used data prior to many recent changes in the health policy landscape, assessment of current capacity is imperative but practically nonexistent.
McCullough and colleagues found that clinical care provision and per capita spending are significantly associated with uptake of EHRs by LHDs, and that having larger populations was associated with continued use of EHRs from 2010 to 2013.12 Although EHRs are most relevant to those LHDs that provide clinical services,12 other areas of informatics use, including HIEs, IRs, EDRSs, and ELR, are useful across the spectrum of LHDs.17–19 To address this knowledge gap, we used the most recent data, collected in late 2013, to identify the factors associated with LHDs' adoption of individual ISs. This study's analysis of organizational survey data identifies and describes structural characteristics of LHDs amenable to policies to improve IT/IS capability or use, so that organizations lacking such capacity can be targeted for intervention.
METHODS
Data source and study design
Data used in this study were collected by the National Association of County and City Health Officials (NACCHO) from the 2013 Profile of Local Health Departments Survey (hereinafter, 2013 Profile).20 The 2013 Profile is the latest of the Profile surveys, conducted to provide a comprehensive picture of LHDs' infrastructure, governance structure, activities, workforce, and a variety of other topics. Designed to serve as the nation's LHD surveillance system, the previous six Profile surveys included 1989, 1992–1993, 1996–1997, 2005, 2008, and 2010.
In addition to the core set of questions administered to all 2,532 LHDs across the country, a representative subsample of LHDs also received a module questionnaire (referred to as Module 2 in the 2013 Profile) containing several questions on public health informatics, emergency preparedness, access to health-care services, and health disparities. The nationally representative sample receiving Module 2 consisted of 625 LHDs, of which 505 LHDs completed the survey (81% response rate). To account for the sampling design that over-sampled larger LHDs, as well as for disproportional nonresponse rates by LHD size, we applied statistical weights that accounted for jurisdictional size. Additional details about the Profile study design are available elsewhere.20
Dependent variables
In the 2013 Profile study, LHDs' level of implementation of health informatics systems was operationalized with the question: “Indicate your LHD's level of activity for each of the following IT areas.” The question included five IT areas: EHRs, HIEs, IRs, EDRSs, and ELR. The response categories for each IT area were (1) no activity, (2) have investigated, (3) planning to implement, and (4) have implemented. Original categories 2 and 3 were combined to reflect a level of informatics capacity between “no activity” and “have implemented.” As a result, five outcome variables with three response categories were included in the multivariate model.
Independent variables
The independent variables considered for the multivariate analyses included LHD infrastructural characteristics and other characteristics theoretically associated with informatics capacity. Variables representing infrastructural/financial capacity included population of LHD jurisdiction;21–23 per capita expenditures22 (coded as: not reported; quintiles [first <$19; second $19–$30; third $31–$46; fourth $46–$75; and fifth ≥$76]); whether or not an LHD had rollover reserve funds, also known as “contingency fund (restricted or unrestricted) that allows the department to accumulate fund balances from year to year for use by the health department”20 (no/don't know, yes); and whether or not the LHD had an IS specialist on staff (yes, no).21 The NACCHO Profile defines this staff type as including computer system, network, and database administrators and analysts; software engineers; and computer support specialists.20 The scope and scale of the LHD was captured through two variables: population size in the jurisdiction and number of clinical services provided by LHDs.24,25 The distribution of the population size was non-normal; therefore, natural log of the population was used in the analyses.
Because EHRs and their clinical use are more relevant to LHDs providing clinical services,12 we included the number of clinical services provided by LHDs (as quartile 1: <8; quartile 2: 8–11; quartile 3: 12–15; and quartile 4: ≥16 services). Other independent variables included length of top executive tenure (in years),26 whether the LHD comprised metropolitan or non-metropolitan jurisdictions, and geographic location of LHD by census region (Northeast, Midwest, South, and West).27 The LHD jurisdiction's metropolitan vs. non-metropolitan status was created based on the National Center for Health Statistics definition for urban-rural counties.28 For LHDs not consisting of a single county or those consisting of other complex structures, NACCHO's geographic IS data table29 was used to designate metropolitan (when all of the geographic units were metropolitan), non-metropolitan (when all of the geographic units were non-metropolitan), predominantly metropolitan (when metropolitan areas of the LHD had a greater population than non-metropolitan areas), and predominantly non-metropolitan (when non-metropolitan areas of the LHD had a greater population than metropolitan areas).
Analysis
We performed descriptive analyses to compute percentages for the categorical variables and means for the continuous variables, population size, and tenure of the top executive director. For the multivariate analysis, we considered several options, first dichotomizing at “have implemented” vs. all other response items. Specification tests showed better model fit under a multinomial approach allowing for an interim category between “no activity” and “have implemented.” We considered ordered logit and tested assumption of parallel lines (c2=20.885, p=0.007), indicating that the location parameters were the same across response categories. However, to draw more specific conclusions from our findings, it was important to determine which variables showed a stronger association with the two opposite categories (have implemented vs. no activity) as well as with the other comparison (have investigated/plan to implement vs. no activity).
Recognizing that drivers of the implementation of IS/IT systems could theoretically differ across system types, we computed five separate multinomial logistic regressions. Nagelkerke Pseudo R-squares for the five models were 0.28 (EHRs), 0.22 (HIEs) 0.36 (IRs), 0.22 (EDRSs), and 0.23 (ELR), indicating a fair amount of variation explained by the independent variables. The likelihood ratio chi-squared statistics for each of the five models—673.4 (EHRs), 504.0 (HIEs), 638.5 (IRs), 440.3 (EDRSs), and 541.2 (ELRs)—had p<0.001, showing that there was no model for which all of the regression coefficients in the model were equal to zero. We performed all analyses for this study using SPSS® version 22.0.30 We calculated 95% confidence intervals (CIs) and other statistics using Stata® version 14.0.31
RESULTS
Of 505 LHDs, 144 (21.8%) had an IS specialist on staff, 345 (70.6%) had one or more local boards of health, 405 (79.1%) were decentralized (i.e., locally governed), 234 (47.0%) had rollover reserve funds, and 285 (61.0%) had a female top executive (Table 1). Of the five informatics outcomes by LHDs, 122 (22.2%) had implemented EHRs in a clinical context, 69 (13.5%) had implemented HIEs, 416 (83.8%) had implemented an IR, 368 (73.0%) had implemented an EDRS, and 245 (47.5%) had implemented ELR (Table 2).
Table 1.
Number and percent of local health departments responding to a module on information systems adoption in a survey by NACCHO,a by infrastructural, governance, and financial characteristics, United States, 2013
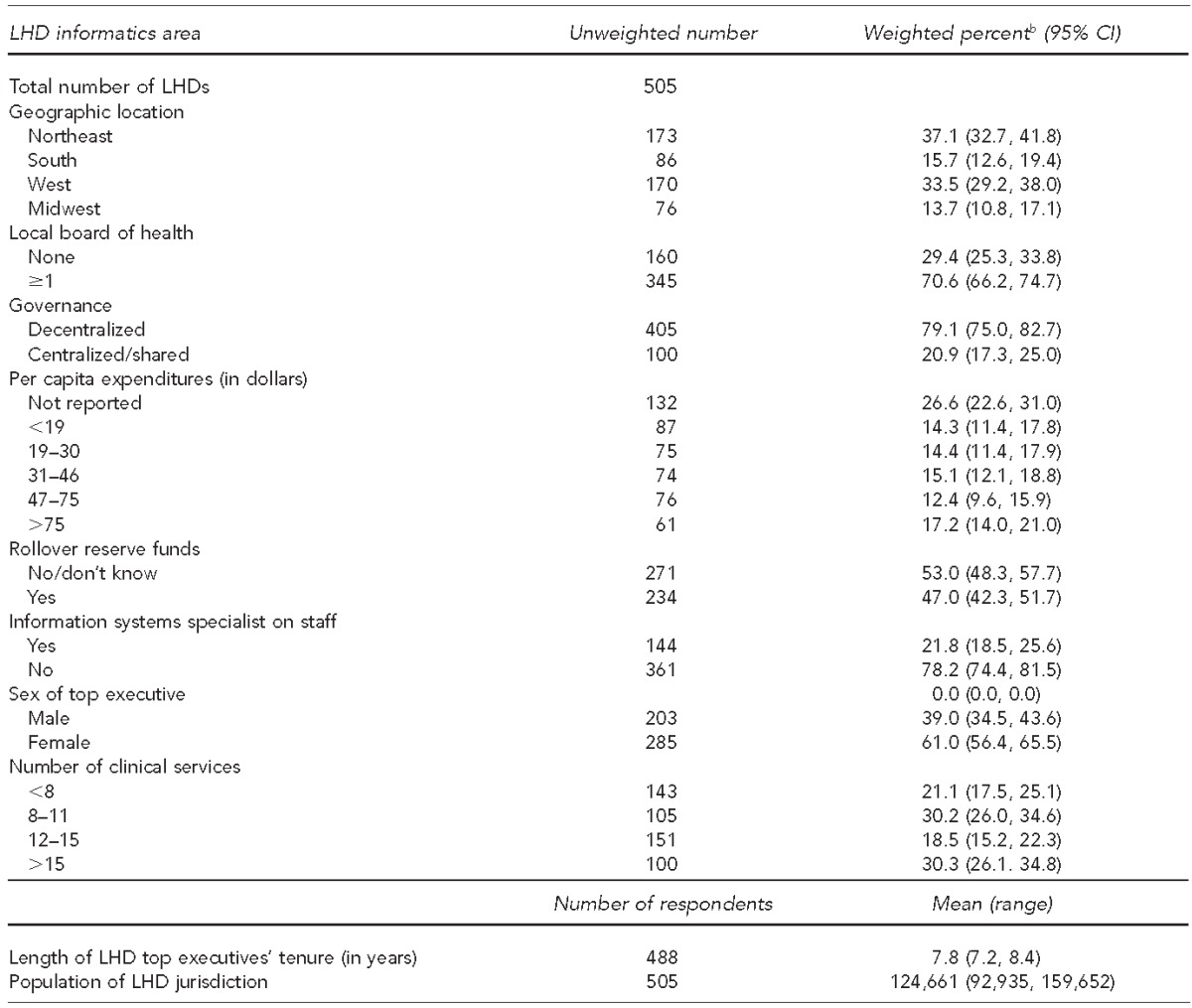
Data source: National Association of County and City Health Officials. 2013 national profile of local health departments. 2014 [cited 2015 Feb 20]. Available from: http://www.naccho.org/topics/infrastructure/profile/upload/2013-national-profile-of-local-health-departments-report.pdf
bPercentages may not total to 100 due to rounding.
NACCHO = National Association of County and City Health Officials
LHD = local health jurisdiction
CI = confidence interval
Table 2.
Number and percent of local health departments responding to a module on information systems adoption in a survey by NACCHO,a by level of implementation of informatics areas, United States, 2013
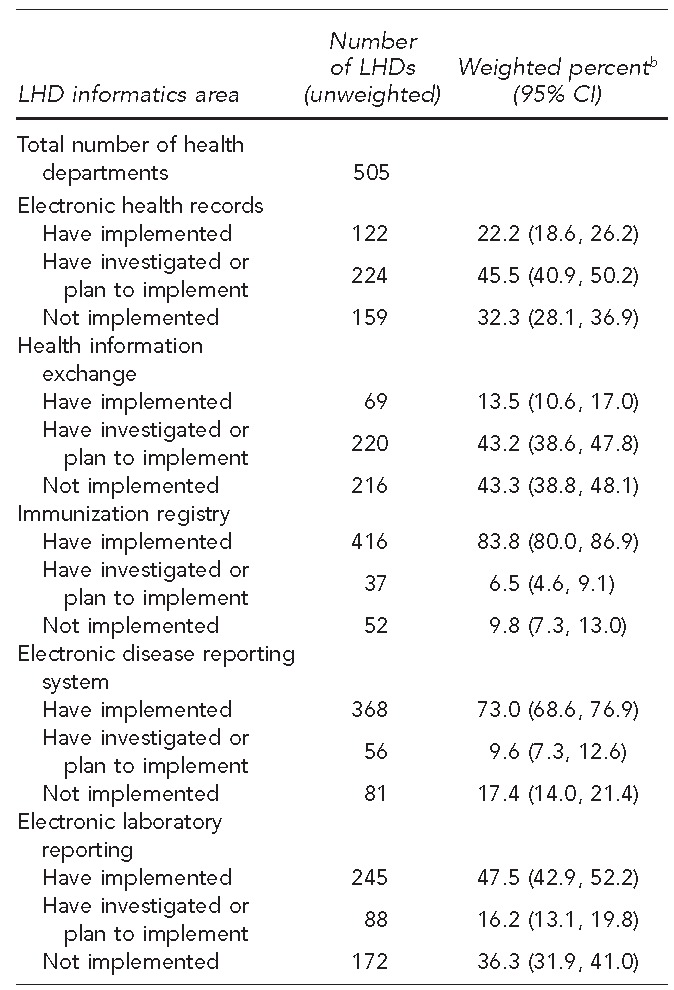
Data source: National Association of County and City Health Officials. 2013 national profile of local health departments. 2014 [cited 2015 Feb 20]. Available from: http://www.naccho.org/topics/infrastructure/profile/upload/2013-national-profile-of-local-health-departments-report.pdf
bPercentages may not total to 100 due to rounding.
NACCHO = National Association of County and City Health Officials
LHD = local health department
CI = confidence interval
Characteristics of LHDs significantly associated with implementation of EHRs included having a more experienced top executive reflected by longer tenure in office (AOR=1.02, p=0.011), having a larger jurisdiction population size (AOR=1.18, p=0.003), being located in the Northeast vs. the Midwest (AOR=1.57, p=0.021), having decentralized vs. centralized or shared governance (AOR=8.79, p<0.001), having higher per capita expenditures (fourth quintile AOR=2.32 and fifth quintile AOR=3.76, p<0.001) not having rollover/reserve funds (AOR=1.51, p=0.003), performing a greater number of clinical services (AOR=2.80 for the third quartile and AOR=3.42 for the fourth quartile, p<0.001), and LHD jurisdiction comprising a metropolitan/predominantly metropolitan area rather than a non-metropolitan area (AOR=1.64, p=0.003) (Table 3).
Table 3.
Multinomial logistic regression of local health department implementation of electronic health records, health information exchange, and immunization registries, in response to a module on information systems adoption in a survey by NACCHO, United States, 2013a
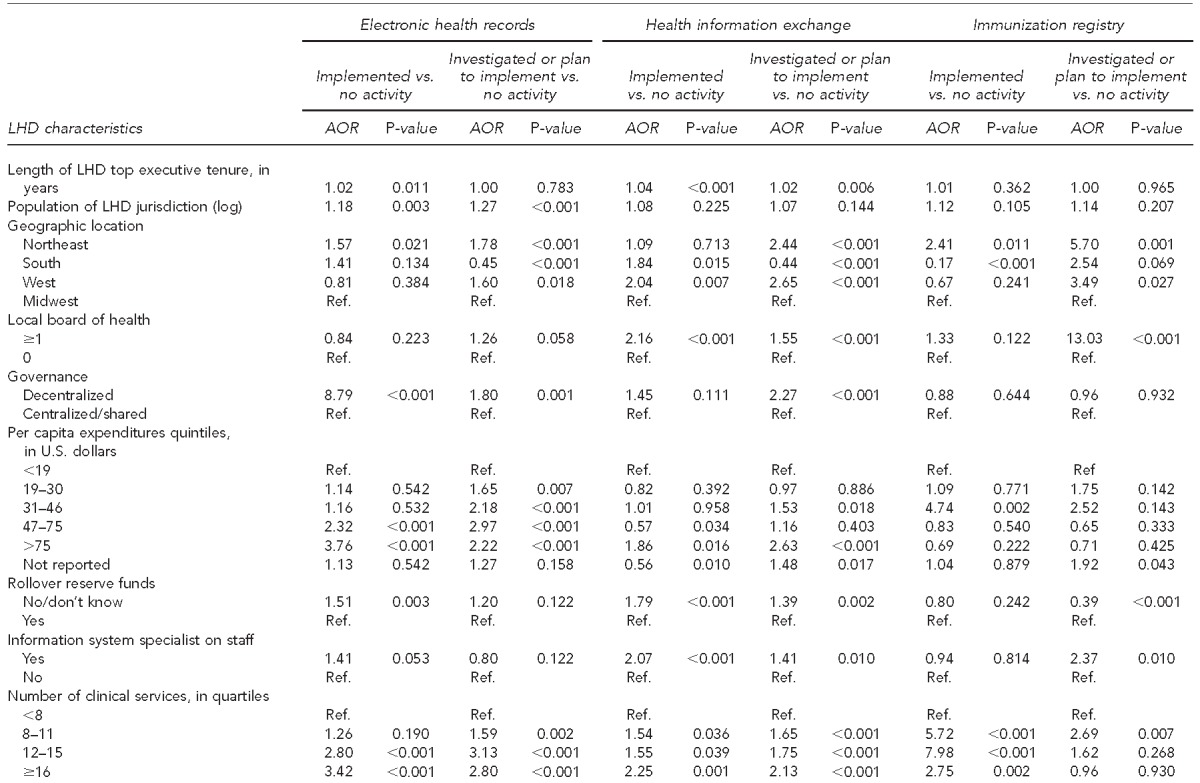
Data source: National Association of County and City Health Officials. 2013 national profile of local health departments. 2014 [cited 2015 Feb 20]. Available from: http://www.naccho.org/topics/infrastructure/profile/upload/2013-national-profile-of-local-health-departments-report.pdf
NACCHO = National Association of County and City Health Officials
LHD = local health department
AOR = adjusted odds ratio
Ref. = reference group
Characteristics significantly associated with LHDs' implementation of HIE were top executive's length of tenure (AOR=1.04, p<0.001), South (AOR=1.84, p=0.015) and West (AOR=2.04, p=0.007) geographic locations, having higher per capita expenditures (fifth quintile AOR=1.86, p=0.016), not having rollover/reserve funds (AOR=1.79, p<0.001), having an IS specialist on staff (AOR=2.07, p<0.001), and performing more clinical services (second quartile AOR=1.54, p=0.036; third quartile AOR=1.55, p=0.039; and fourth quartile AOR=2.25, p=0.001). Having a local board of health was associated with increased implementation of HIEs (AOR=2.16, p<0.001) (Table 3).
LHD characteristics significantly associated with IR included per capita expenditures (third quartile AOR=4.74, p=0.002), Northeast vs. Midwest (AOR=2.41, p=0.011), and performing more clinical services (second quartile AOR=5.72, p<0.001; third quartile AOR=7.98, p<0.001; and fourth quartile AOR=2.75, p=0.002) (Table 3).
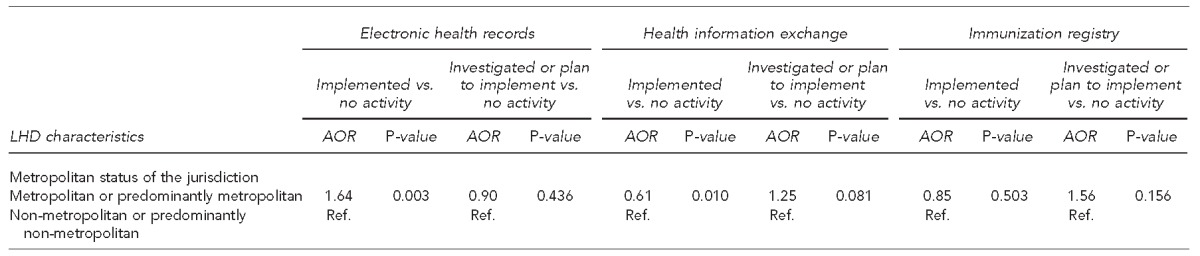
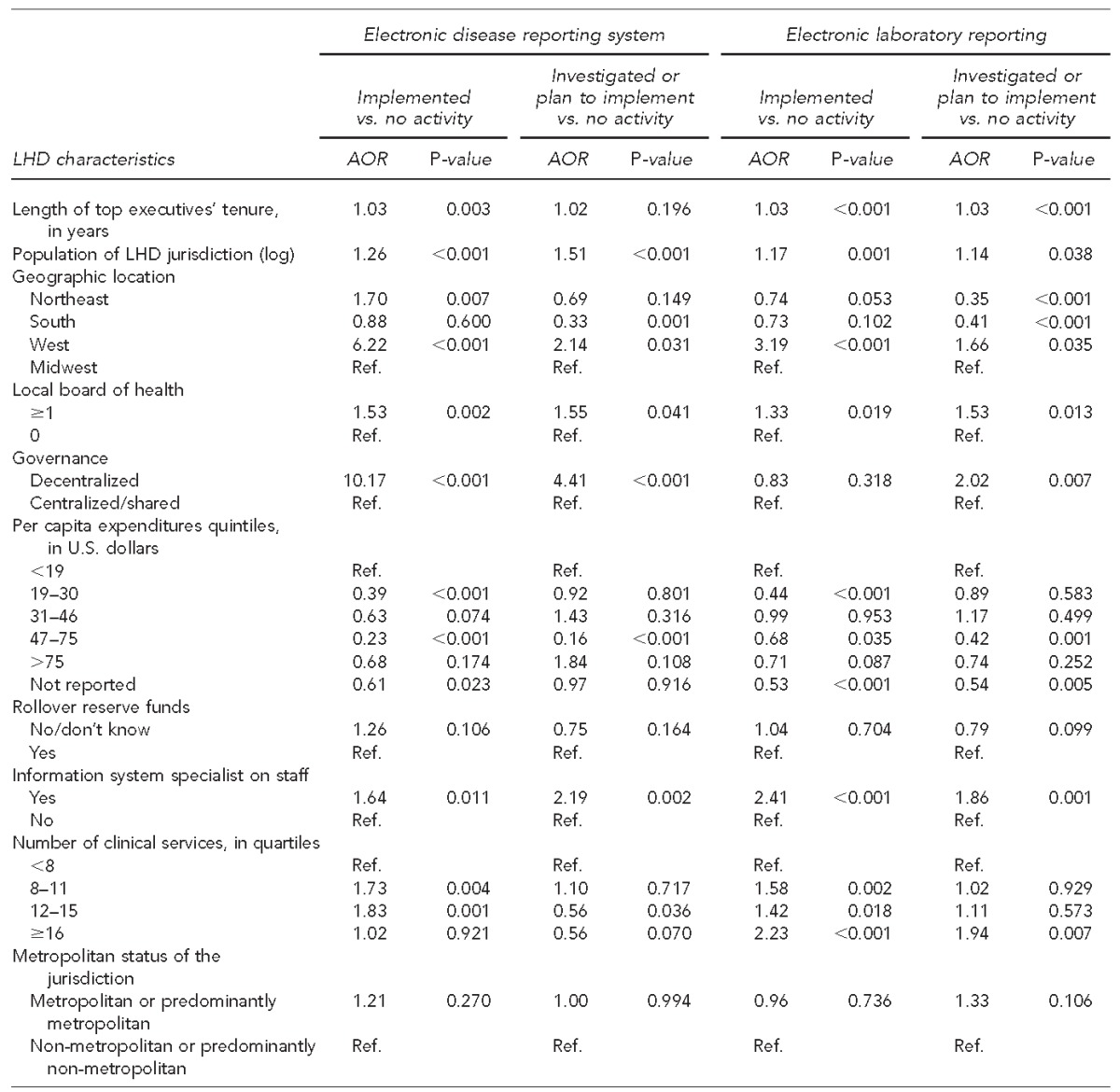
LHD characteristics significantly associated with implementation of EDRSs included length of tenure (AOR=1.03, p=0.003), jurisdiction population size (AOR=1.26, p<0.001), geographic locations in the Northeast (AOR=1.70, p=0.007) or West (AOR=6.22, p<0.001), having a local board of health (AOR=1.53, p=0.002), having decentralized governance (AOR=10.17, p<0.001), having an IS specialist on staff (AOR=1.64, p=0.011), and having a higher number of clinical services (AOR=1.83 for the third quartile, p=0.001; AOR=1.73 for the second quartile, p=0.004) (Table 4).
Table 4.
Multinomial logistic regression of local health department implementation of electronic disease reporting systems and electronic laboratory reporting, in response to a module on information systems adoption in a survey by NACCHO, United States, 2013a
Data source: National Association of County and City Health Officials. 2013 national profile of local health departments. 2014 [cited 2015 Feb 20]. Available from: http://www.naccho.org/topics/infrastructure/profile/upload/2013-national-profile-of-local-health-departments-report.pdf
NACCHO = National Association of County and City Health Officials
LHD = local health department
AOR = adjusted odds ratio
Ref. = reference group
Significant factors associated with implementation of ELR included length of tenure (AOR=1.03, p<0.001), jurisdiction population size (AOR=1.17, p=0.001), West geographic location (AOR=3.19, p<0.001), having an IS specialist on staff (AOR=2.41, p=0.001), having a local board of health (AOR=1.33, p=0.019), and performing a greater number of clinical services (second quartile AOR=1.58, p=0.002; third quartile AOR=1.42, p=0.018; and fourth quartile AOR=2.23, p<0.001) (Table 4).
The factors most strongly associated with implementation of all five health informatics areas included provision of greater number of clinical services, greater per capita expenditures, having an IS specialist on staff, having a larger population size, having a decentralized governance system, having one or more local boards of health, having a top executive with greater number of years in the position, and being located in the Northeast or West regions (vs. Midwest) (Table 4).
DISCUSSION
Public health is fundamentally an information business.5 Health informatics plays a critical role in the daily operation of LHDs and in activities such as mapping, disease surveillance, strategic planning, quality assurance, community resource assessment, vital statistics, environmental health, immunization tracking, and laboratory reporting in addition to strategically making sense of, and guiding, changes in their environment.4,32–34 This study highlights tremendous variation in the sophistication and uptake of IS to support the work of governmental public health. In 2013, several organizational characteristics appeared to be major drivers of IT/IS uptake: the employment of IS specialists, financial resources, geography, and governance status. Greater provision of clinical services also appeared to drive uptake of several informatics-oriented programs, especially EHRs. Previous research suggests that greater uptake of informatics for LHDs providing more clinical services is both a function of streamlining workflow and the result of billing for clinical services.35
Employing IS specialists was associated both with having implemented or having plans to implement most of the IT/IS systems examined in this study. However, only about 20% of LHDs had IS specialists on staff. The vast majority of smaller jurisdictions did not have an IS specialist on staff. Even at the state level, approximately 5% of the workforce includes IS or IT specialists.36 Not having an IS specialist on staff presents a workforce development opportunity; the natural evolution of the epidemiologist to the informatics-oriented epidemiologist may be a potential solution. This process is already underway in many health departments across the country.16
The increasing need for and value of disease surveillance and care coordination in the post-Affordable Care Act era necessitate that LHDs use EHRs, EDRSs, and ELR and exchange data through HIEs. Our results about LHDs' lack of implementation of IS highlight a need for policy attention, and our results indicating which factors influence their implementation provide research evidence on how to target improvements in LHDs' informatics capacity. As one of the primary end users of more voluminous and sophisticated data accessible in a new world of EHRs and HIEs, public health practitioners should have targeted informatics training to augment their abilities and support informatics capacity development in large and small health departments. Informatics capacity development of LHDs may take the form of in-place training by specialists from state health agencies, academic training on informatics from schools and programs of public health, or distance-learning trainings aimed at epidemiologists and other frontline staff. Examples include the Informatics Academy, which trains public health workers on the design and implementation of public health informatics systems,37 and the American Medical Informatics Association 10x10 Program for public health professionals.38 The recent reorganization of the Public Health Training Centers into regional extension centers also presents a potential opportunity to focus on distance learning in informatics. A continued challenge, however, is that four of five smaller health departments (population <25,000) do not have an epidemiologist on staff.18 A potential approach is to provide more dedicated informatics staff members at the state level to support LHD surveillance needs or, more plausibly, cross-jurisdictional sharing or regionalization of certain informatics activities.
IS and IT play a critical role in the daily operation of LHDs but are not uniformly available.32 In the post-Great Recession era, being funded at a higher level affects LHDs' informatics capacity. Public health agencies often struggle with issues of data integration, data quality, and effective data exchange with other public health agencies and health-care organizations, which are potential barriers to uptake.35,39 Our study also shows that staffing, financial, and geographic factors are also highly correlated with differential uptake of various informatics programs. Although geography is not modifiable from an LHD's perspective, greater focus on training existing staff members and leveraging existing clinical systems and demand for direct services to support the work of public health are modifiable behaviors. Association of implementation of these ISs with variables indicating economies of scale (e.g., population size, number of clinical services provided) and per capita expenditures may mean that targeted investments may be essential, particularly in LHDs lacking economies of scale. These investments may target professional education and training focused on explaining benefits and use of various informatics components, incentivizing recruitment and retention of staff members trained in health informatics, and developing/updating interoperable public health ISs.
Supporting the effective performance of informatics activities is critical because the majority of these activities are the sole purview of the public health system. Public health is uniquely charged with communicable and non-communicable disease control and prevention. Furthermore, if the nation's health-care and public health systems are to optimally align, and the recent movement for integration of primary care and public health is to successfully materialize,40,41 public health organizations must become as sophisticated as the health-care industry in their adoption of interoperable ISs and use of HIEs.
Limitations
Data used in this study were drawn from a national sample of LHDs. The NACCHO Profile is widely used in public health systems and services research, but it does have limitations. The most substantial limitation is that the Profile is self-reported, and interpretations of implementation status for the various IT/IS areas are subject to several potential biases, including social desirability and inconsistent understanding and interpretation of informatics terms. In the past decade, NACCHO has attempted to standardize this question by consulting with its informatics team and the advisory workgroups.17 The outcome of that process is expected to have resulted in a decrease in observed IT/IS capacity from 2008 to 2013, which has been attributed to respondents better understanding the definitions of the terms.
CONCLUSION
The capacity of LHDs to use real-time, local data and information is critical. Many LHDs did not have this capacity because of lack of specialized staff members, availability of data systems, or a host of other political or organizational constraints. Such lack of capacity to use real-time data was especially the case for smaller jurisdictions. Cross-jurisdictional sharing or regionalization of some informatics and surveillance functions may be a reasonable approach to address these shortfalls. A combination of investment in public health informatics infrastructure, additional training of new informatics staff members and existing epidemiologists, and better integration with health-care systems is needed to augment LHD informatics capacity and ensure governmental public health can meet the information needs of the 21st century.
Footnotes
This study was conducted with financial support from the de Beaumont Foundation. The authors thank the National Association of County and City Health Officials for providing the 2013 Profile Data. The Institutional Review Board of Georgia Southern University approved this study as exempt from a full review.
REFERENCES
- 1.Yasnoff WA, O'Carroll PW, Koo D, Linkins RW, Kilbourne EM. Public health informatics: improving and transforming public health in the information age. J Public Health Manag Pract. 2000;6:67–75. doi: 10.1097/00124784-200006060-00010. [DOI] [PubMed] [Google Scholar]
- 2.Cheatham M. Washington: National Association of County and City Health Officials; 2007. Informatics works in local health departments: findings from the 2005 National Profile of Local Health Departments study. [Google Scholar]
- 3.Baker EL, Ross DA. Managing information—addressing a central challenge of the public health enterprise. J Public Health Manag Pract. 2013;19:383–5. doi: 10.1097/PHH.0b013e318296f43f. [DOI] [PubMed] [Google Scholar]
- 4.Magruder C, Burke M, Hann NE, Ludovic JA. Using information technology to improve the public health system. J Public Health Manag Pract. 2005;11:123–30. doi: 10.1097/00124784-200503000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Lumpkin JR, Magnuson JA. History and significance of information systems and public health. In: Magnuson JA, Paul C, editors. Public health informatics and information systems. 2nd ed. London: Springer-Verlag; 2014. pp. 19–36. [Google Scholar]
- 6.Ostrovsky A, Katz MH. The San Francisco Community Vital Signs: using Web-based tools to facilitate the mobilizing for action through planning and partnerships process. J Public Health Manag Pract. 2011;17:457–71. doi: 10.1097/PHH.0b013e318208e750. [DOI] [PubMed] [Google Scholar]
- 7.Richardson JE, Abramson EL, Pfoh ER, Kaushal R. How communities are leveraging the health information technology workforce to implement electronic health records. AMIA Annu Symp Proc. 2011;2011:1186–95. [PMC free article] [PubMed] [Google Scholar]
- 8.Kirkwood J, Jarris PE. Aligning health informatics across the public health enterprise. J Public Health Manag Pract. 2012;18:288–90. doi: 10.1097/PHH.0b013e31824eb919. [DOI] [PubMed] [Google Scholar]
- 9.National Association of County and City Health Officials. The top eight things LHDs should know about the HITECH Act [cited 2014 Dec 1] Available from: http://www.naccho.org/topics/infrastructure/informatics/resources/upload/top-8-with-NACCHO-letterhead-2.pdf.
- 10.National Association of County and City Health Officials. Top seven things regional extension centers (RECs) should know about local health departments (LHDs) [cited 2015 Jan 14] Available from: http://www.naccho.org/topics/infrastructure/informatics/resources/upload/top-7-with-NACCHO-letterhead-RECs-ST-8-25-2.pdf.
- 11.Davidson A. Why should local health departments care about meaningful use? NACCHO Exchange. 2013;12:17–9. [Google Scholar]
- 12.McCullough JM, Goodin K. Patterns and correlates of public health informatics capacity among local health departments: an empirical typology. Online J Public Health Inform. 2014;6:e199. doi: 10.5210/ojphi.v6i3.5572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shah GH, Rogers V, Lovelace KA. Local public health agencies' involvement in electronic health records and syndromic surveillance systems. Presentation at the American Public Health Association Annual Meeting; 2011 Nov 2; Washington, D.C. [Google Scholar]
- 14.Shah GH, Rogers V. Local health departments' (LHDs) meaningful use readiness, general informatics capacity, needs, and barriers. Presentation at the CDC Public Health Informatics Annual Conference; 2011 Aug 21–24; Atlanta. [Google Scholar]
- 15.Savel TG, Foldy S. The role of public health informatics in enhancing public health surveillance. MMWR Morb Mortal Wkly Rep. 2012;61(03):20–4. [PubMed] [Google Scholar]
- 16.Smith PF, Hadler JL, Stanbury M, Rolfs RT, Hopkins RS CSTE Surveillance Strategy Group. “Blueprint version 2.0”: updating public health surveillance for the 21st century. J Public Health Manag Pract. 2013;19:231–9. doi: 10.1097/PHH.0b013e318262906e. [DOI] [PubMed] [Google Scholar]
- 17.Merrick R, Hinrichs SH, Meigs M. Public health laboratories. In: Magnuson JA, Paul C, editors. Public health informatics and information systems. 2nd ed. London: Springer-Verlag; 2014. pp. 295–308. [Google Scholar]
- 18.Magnuson JA, Fu PC., Jr . Public health informatics and health information exchange. In: Magnuson JA, Paul C, editors. Public health informatics and information systems. 2nd ed. London: Springer-Verlag; 2014. pp. 429–48. [Google Scholar]
- 19.Stevens LA, Palma JP, Pandher KK, Longhurst CA. Immunization registries in the EMR era. Online J Public Health Inform. 2013;5:211. doi: 10.5210/ojphi.v5i2.4696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.National Association of County and City Health Officials. 2013 national profile of local health departments. 2014 [cited 2015 Feb 20] Available from: http://www.naccho.org/topics/infrastructure/profile/upload/2013-national-profile-of-local-health-departments-report.pdf.
- 21.Vest JR, Menachemi N, Ford EW. Governance's role in local health departments' information system and technology usage. J Public Health Manag Pract. 2012;18:160–8. doi: 10.1097/PHH.0b013e318226c9ef. [DOI] [PubMed] [Google Scholar]
- 22.Shah GH, Lovelace K, Mays GP. Diffusion of practice-based research in local public health: what differentiates adopters from nonadopters? J Public Health Manag Pract. 2012;18:529–34. doi: 10.1097/PHH.0b013e3182602e5b. [DOI] [PubMed] [Google Scholar]
- 23.Handler AS, Turnock BJ. Local health department effectiveness in addressing the core functions of public health: essential ingredients. J Public Health Policy. 1996;17:460–83. [PubMed] [Google Scholar]
- 24.Singh S, Bernet PM. Economies of scale and scope in public health: an analysis of food hygiene services provided by local health departments in Florida. Front Public Health Serv Syst Res. 2014;3(3) [Google Scholar]
- 25.Santerre RE. Jurisdiction size and local public health spending. Health Serv Res. 2009;44:2148–66. doi: 10.1111/j.1475-6773.2009.01006.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Luo H, Sotnikov S, Shah G, Galuska DA, Zhang X. Variation in delivery of the ten essential public health services by local health departments for obesity control in 2005 and 2008. J Public Health Manag Pract. 2013;19:53–61. doi: 10.1097/PHH.0b013e31824dcd81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Barnes PA, Curtis AB. A national examination of partnerships among local health departments and faith communities in the United States. J Public Health Manag Pract. 2009;15:253–63. doi: 10.1097/01.PHH.0000349740.19361.ac. [DOI] [PubMed] [Google Scholar]
- 28.National Center for Health Statistics (US) NCHS urban-rural classification scheme for counties [cited 2015 Mar 23] Available from: http://www.cdc.gov/nchs/data_access/urban_rural.htm.
- 29.National Association of County and City Health Officials. Data requests & technical documentation: GIS shapefiles (2008–13) [cited 2014 Mar 23] Available from: http://nacchoprofilestudy.org/data-requests.
- 30.IBM Corp. Armonk (NY): IBM Corp; 2013. IBM SPSS® Statistics: Version 22.0 for Windows. [Google Scholar]
- 31.StataCorp. College Station (TX): StataCorp; 2015. Stata®: Version 14.0. [Google Scholar]
- 32.Choo CW. New York: Oxford University Press; 1998. The knowing organization: how organizations use information to construct meaning, create knowledge, and make decisions. [Google Scholar]
- 33.Yi Q, Hoskins RE, Hillringhouse EA, Sorensen SS, Oberle MW, Fuller SS, et al. Integrating open-source technologies to build low-cost information systems for improved access to public health data. Int J Health Geogr. 2008;7:29. doi: 10.1186/1476-072X-7-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vest JR, Issel LM. Data sharing between local health and state health departments: developing and describing a typology of data gaps. J Public Health Manag Pract. 2013;19:357–65. doi: 10.1097/PHH.0b013e31826d8045. [DOI] [PubMed] [Google Scholar]
- 35.Menachemi N, Collum TH. Benefits and drawbacks of electronic health record systems. Risk Manag Healthc Policy. 2011;4:47–55. doi: 10.2147/RMHP.S12985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dixon BE, McFarlane TD, Dearth S, Grannis SJ, Gibson PJ. Characterizing informatics roles and needs of public health workers: results from the Public Health Workforce Interests and Needs Survey. J Public Health Manag Pract. 2015;21(Suppl 6):S130–40. doi: 10.1097/PHH.0000000000000304. [DOI] [PubMed] [Google Scholar]
- 37.Public Health Informatics Institute. The Informatics Academy [cited 2015 Mar 22] Available from: http://phii.org/academy.
- 38.American Medical Informatics Association. AMIA 10x10 courses: training health care professionals to serve as informatics leaders [cited 2015 Aug 1] Available from: https://www.amia.org/education/10x10-courses.
- 39.Vest JR, Kirk HM, Issel LM. Quality and integration of public health information systems: a systematic review focused on immunization and vital records systems. Online J Public Health Inform. 2012;4(2) doi: 10.5210/ojphi.v4i2.4198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Scutchfield FD, Michener JL, Thacker SB. Are we there yet? Seizing the moment to integrate medicine and public health. Am J Prev Med. 2012;42(6 Suppl 2):S97–102. doi: 10.1016/j.amepre.2012.04.001. [DOI] [PubMed] [Google Scholar]
- 41.Koo D, Felix K, Dankwa-Mullan I, Miller T, Waalen J. A call for action on primary care and public health integration. Am J Public Health. 2012;102(Suppl 3):S307–9. doi: 10.2105/AJPH.2012.300824. [DOI] [PMC free article] [PubMed] [Google Scholar]


