Abstract
Objectives
A major responsibility of a local health department (LHD) is to assure public health service availability throughout its jurisdiction. Many LHDs face expanded service needs and declining budgets, making billing for services an increasingly important strategy for sustaining public health service provision. Yet, little practice-based data exist to guide practitioners on what to expect financially, especially regarding timing of reimbursement receipt. This study provides results from one LHD on the lag from service delivery to reimbursement receipt.
Methods
Reimbursement records for all transactions at Maricopa County Department of Public Health immunization clinics from January 2013 through June 2014 were compiled and analyzed to determine the duration between service and reimbursement. Outcomes included daily and cumulative revenues received. Time to reimbursement for Medicaid and private payers was also compared.
Results
Reimbursement for immunization services was received a median of 68 days after service. Payments were sometimes taken back by payers through credit transactions that occurred a median of 333 days from service. No differences in time to reimbursement between Medicaid and private payers were found.
Conclusions
Billing represents an important financial opportunity for LHDs to continue to sustainably assure population health. Yet, the lag from service provision to reimbursement may complicate budgeting, especially in initial years of new billing activities. Special consideration may be necessary to establish flexibility in the budget-setting processes for services with clinical billing revenues, because funds for services delivered in one budget period may not be received in the same period. LHDs may also benefit from exploring strategies used by other delivery organizations to streamline billing processes.
Among the 10 essential public health services that all public health departments are expected to perform is the responsibility to “link people to needed personal health services and assure the provision of health care when otherwise unavailable.”1 As such, health departments are often involved in directly providing public health services within their jurisdiction.2,3 These direct services are costly to provide, but many health departments provide direct clinical services because of their sizable impact on population health4 and a health department's role in assuring the provision of health care when otherwise unavailable.5,6 Immunizations provide an example of financial pressures facing many health departments.
Vaccinations prevent more than 14 million incident cases of disease and 33,000 deaths per year,7 and LHDs play a critical role in assuring access to vaccinations within their jurisdiction. Approximately 85% of all local health departments (LHDs) provide immunization services8 and deliver one of every seven vaccinations in the United States.9 Since 2000, the number of recommended vaccines has more than doubled and the cost to purchase these vaccines has more than tripled.9,10 At the same time, half of all LHDs have seen their core budgets cut because of the 2008–2010 recession.11 These trends mean that health departments can no longer provide all services with government funding and increasingly rely on billing Medicaid or private insurance to backfill some of these cuts.10,12 Thus, billing for services such as vaccinations has become a widely practiced method of recouping revenue to support the provision of public health services by LHDs.12 An emerging consensus suggests that billing for services provided to individuals with health insurance ensures equitable and efficient allocation of program resources toward individuals truly unable to afford it (i.e., those without health insurance).13
Partly because of these factors, more than 80% of LHDs report plans to begin new billing activities or expand billing activities.14 Widespread adoption of billing by LHDs is at least partially supported by the considerable technical assistance devoted to creating resources to facilitate billing for clinical services.15 Brief case reports from several successful LHD and state health department clinical billing efforts have been reported.16
However, multiple challenges confront many LHDs that are beginning or expanding clinical billing: licensing or credentialing staff members, receiving Medicare or Medicaid qualifications, contracting with private insurance payers, establishing billing systems and protocols, and training staff members in completing and submitting claims.17 Furthermore, in some states, health departments face complex statutory requirements that may preclude billing some patients' insurance providers for certain services.18 Some health departments are required to receive certification as essential community providers to contract with private health insurance plans.13 After navigating these issues, health departments vary in their statutory ability to set prices for services (vs. authority to set reimbursement amounts determined by state statute) and retain billing reimbursements within the department (vs. having to remit these funds to a county or state treasury).18 Insofar as health departments engage in billing to recoup some or all of the costs of providing services, how much reimbursement a department receives and when it receives it are critical issues, given the regimented nature of the annual budgetary processes at most LHDs. To date, the scholarly literature lacks empirical evidence in both of these areas. This study explored reporting results from one health department on the lag from date of service to receipt of reimbursement.
METHODS
Setting
Data for this study came from immunization clinics operated by the Maricopa County Department of Public Health (MCDPH) in Arizona. MCDPH serves nearly 4 million people, one of the largest LHD jurisdictions in the nation. MCDPH operates three immunization clinics and seeks reimbursement for services from both Medicaid and private health insurance plans.
Immunization services are delivered by MCDPH nurses and staff members. During each patient encounter, patients or guardians complete a consent form and are screened for current health insurance coverage. MCDPH nurses query a Web-based immunization registry to determine recommended vaccinations, and then prepare and administer vaccinations. Service records are kept on paper forms in the clinics. After updating the immunization registry to reflect services delivered, the service records are delivered to The Arizona Partnership for Immunization (TAPI), a nonprofit organization that has served as the centralized claims processor for many Arizona LHDs since 2008. Claims are then entered by TAPI into an electronic billing system and submitted to payers for reimbursement. Additional details about TAPI and MCDPH billing practices are available elsewhere.12,15 MCDPH and TAPI have previously received technical assistance support from the Centers for Disease Control and Prevention's (CDC's) Billables Project, including an in-depth analysis comparing billing system investments with additional reimbursements received. The support did not address—or attempt to minimize—time to reimbursement in MCDPH clinics.
Billing and reimbursement
Because of the complex nature of immunization financing,19 billing and reimbursement vary across payer type and by state. For uninsured patients and those insured through Medicaid, CDC offers the vaccine product to providers free of charge through the Vaccines for Children program.20,21 Providers can then seek reimbursement for administering the vaccination to Medicaid-insured individuals, but not for the product itself. For privately insured patients, providers purchase, administer, and seek reimbursement for the product and for vaccine administration. Thus, two vaccine inventories must be maintained and accurately tracked in all MCDPH immunization clinics. In Arizona, the amounts that can be reimbursed for some services (e.g., vaccine administration) are set via statute. The amounts that can be charged for other products or services delivered to privately insured patients are negotiated with payers (i.e., insurance companies).
Payers receive the request for reimbursement and, after verifying the claim (e.g., patient enrollment, services delivered), remit payment to the provider. These transactions (i.e., when an insurance company reimburses the provider) are known as debit transactions. Reimbursement can occur in single lump-sum transactions or across multiple transactions (e.g., two smaller payments instead of one full payment). In some cases, a payer may reassess a previously reimbursed claim and determine that the payment was made in error or in excess of allowed rates. In these instances, the payer then takes back some or all previously issued payments. These transactions are known as credit transactions. Records of all adjudicated claims for reimbursements—including debit, credit, and denied claims—are distributed from TAPI to MCDPH monthly.
Data
Data for this study included records of all reimbursement (as described previously) for credit transactions and debit transactions received from January 1, 2013, through June 30, 2014. For this study, reimbursement data were compiled according to the number of days between date of service and date(s) of reimbursement.
The dataset included transaction records for immunization encounters at MCDPH clinics from July 2006 to June 2014. About 50% of records in the dataset were for vaccinations delivered from March 2013 to April 2014. Transactions for vaccinations delivered prior to 2009 (n=33) were to close out records of services delivered prior to TAPI's involvement. Therefore, these transactions are not reflected in the analysis, because no payment was made. In addition, clinic visit data from fiscal year 2014 (FY2014: July 1, 2013, to June 30, 2014) were obtained from MCDPH immunization program staff members to determine the total number of visits to the three clinics during the relevant time periods. Total reimbursement was calculated by summing all debit and credit transactions for each vaccination to arrive at a final settlement date and amount received.
Two main outcomes of interest were explored: (1) daily revenue, defined as the percentage of total revenues received each day from service delivery date (e.g., percentage of revenue received on the 30th day from when service was provided); and (2) cumulative total percentage of reimbursements received as of each day from service delivery date (e.g., percentage of total revenue received as of 30 days from service).
Payer type (Medicaid vs. private insurance) was not directly available in the dataset; as such, an algorithm was used to determine payer type. As described previously, for children insured through Medicaid, MCDPH bills for administering the vaccination but not for the vaccine product itself. Thus, visits with no billing claims other than vaccine administration (Current Procedural Terminology codes 90460, 90461, 90471, 90472, 90473, and 90474) were assumed to be paid by Medicaid, while visits for billing claims including vaccine products were assumed to be paid by privately insured patients. The difference in time to reimbursement for Medicaid vs. private payers was calculated and tested for significance using a Mann-Whitney test. Analysis was performed using Stata® version 13.1.22
RESULTS
In FY2014, MCDPH clinics vaccinated 48,462 patients. Of these patients, 28,540 (59%) were uninsured, 14,563 (30%) were insured through Medicaid, 4,707 (10%) had private insurance, and 652 (1%) were underinsured. Claims records were available for 73,931 billing transactions, representing 61,250 unique vaccinations and 29,374 patient visits spanning more than six years.
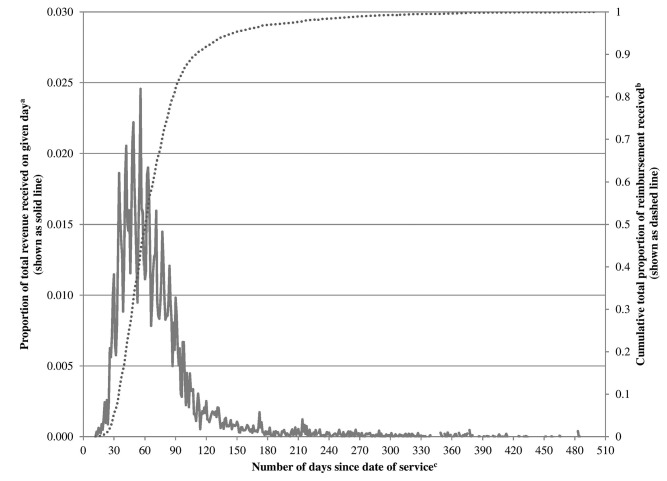
Reimbursements were received after a median of 68 days (range: 12–2,350, interquartile range 50–94). Approximately 85% of revenues for all services rendered in a given year were reimbursed within that same year. The remaining 15% would be received in subsequent budget periods (Figure 1).
Figure 1.
Time between service provision and receipt of reimbursement for services delivered at Maricopa County Department of Public Health immunization clinics, Arizona, January 2013 through June 2014
aProportion shown represents the total amount of reimbursements received on a given day divided by the grand total amount of reimbursements ever received by the health department.
bProportion shown represents the sum of all reimbursements received to date as of a given day divided by the grand total amount of reimbursements ever received by the health department.
cFigure is truncated at 510 days from service.
Reimbursement for vaccinations provided often occurred in more than one transaction. In some cases, reimbursements (i.e., debit transactions) were later followed by take-backs (i.e., credit transactions). Of the 73,931 transactions analyzed, 2,491 (3%) were credits. Credit transactions occurred a median of 333 days from date of service (range: 27–737), which was significantly longer than debit transactions (range: 12–2,350) (p<0.001).
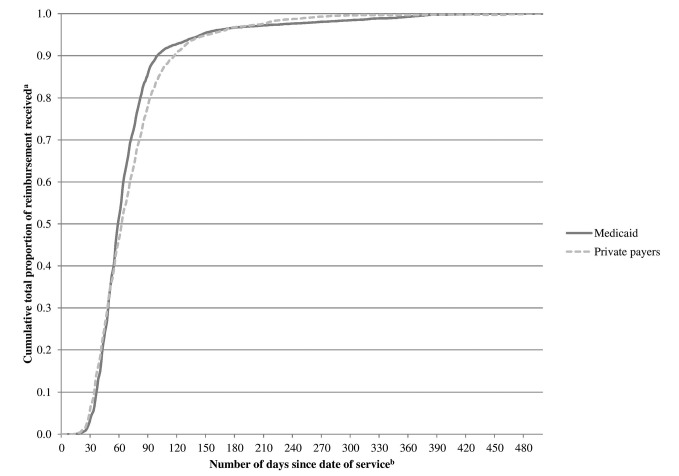
Median time to reimbursement for Medicaid-paid visits was 59 days (range: 12–478), while median time to reimbursement for privately insured patients was 63 days (range: 13–2,350) (Figure 2).
Figure 2.
Timing of reimbursement for Medicaid vs. private insurance payers for services delivered at Maricopa County Department of Public Health immunization clinics, Arizona, January 2013 through June 2014
aProportion shown represents the sum of all reimbursements received to date as of a given day divided by the grand total amount of reimbursements ever received by the health department.
bFigure is truncated at 500 days from service.
DISCUSSION
Billing for clinical services is a common and increasingly important strategy for LHDs to support provision of services that are vital to population health.10,12–15 Revenues from billing efforts are important sources of revenue in an era of declining LHD budgets.11 Without these additional revenues, LHDs may not always be able to sustain current service levels.14 In Maricopa County, more than 28,000 uninsured children received services from these immunization clinics in FY2014, making the department one of the larger sources of vaccinations in the community and an important safety net provider. Yet, even though LHDs are likely to rely on revenue from clinical billing to support provision of these services,12,13,17 little empirical evidence exists to help guide LHD practitioners interested in beginning, expanding, or improving billing activities.
Data from this study showed that reimbursements for services provided at three county-run immunization clinics in Maricopa County took a median of 68 days to be reimbursed, with time to reimbursement consistent for both Medicaid and privately insured patients. The majority (70%) of reimbursements were received within a one- to three-month window from date of service. Yet in some instances, claims are adjudicated more than one to two years from date of service. This lag may present challenges and opportunities for LHDs.
A potential challenge is that budget processes, targets, and limitations may not align with a three-month lag. For example, if an LHD begins billing for services on day one of a new fiscal year, based on our findings, a sizable percentage (15%) of the revenues for those services would be received in subsequent budget periods. Therefore, financial reconciliation of services rendered vs. revenues received for any given fiscal year may pose a real challenge, because reimbursement for funds expended in one year may not be received until subsequent periods. To address this point, it may be important for health departments engaged in billing to generate their own estimates of time to reimbursement and the proportion of reimbursement likely to be received in subsequent budget periods. These estimates can help managers develop more accurate projections to match future expenditures with future revenues.
Given that the vast majority of health departments plan to begin or expand billing efforts,14 many departments are likely to encounter the need for large, upfront expenditures (e.g., acquiring new space, hiring new staff members, or purchasing a new supply of vaccines to begin serving privately insured individuals). The findings of this study suggest that health departments should plan to make these purchases with the understanding that it may take two or more months from when service delivery begins before beginning to receive full reimbursement. Careful attention should be paid to preparing a realistic budget not only for the run-up to opening a new line of billing, but also for the initial months of operation.
Additionally, portions of some payments are likely to be taken back by payers over time. Linking -payments received for services rendered can therefore be difficult and may vary over time (e.g., a snapshot of total reimbursements received on one day might be different than a snapshot in the next month).
Although these issues may be familiar to experienced practitioners, they have not been widely discussed, and our review of the existing literature did not reveal promising practices on how to minimize risks and uncertainties that accompany not knowing when payment will be received and if that payment might someday be taken back. To date, discussion of financial best practices for receiving and accounting for billing revenues is absent from the scholarly literature.
One potential opportunity for health departments may lie in the ability to streamline billing processes. The reimbursement lag includes time spent by the LHD preparing the paper record of the service(s) rendered, delivering the bill to the billing partners, creating and submitting the claim, and waiting for reimbursement from the payer. MCDPH uses both paper forms and electronic billing methods. Process improvement or investing in a fully digitized billing process may offer opportunities to tighten the window between service delivery and receipt of reimbursement. Shortening the lag between service delivery and reimbursement would mean more rapid availability of funds for health departments to use or return to general funds.
A reimbursement lag is not unique to public health departments—private providers also report lags between service provision and receipt of reimbursement. Reported delays from other health-care delivery systems ranged from 37 to 115 days,23 which is roughly consistent with results from this study (median = 68 days). This finding suggests that, at least for the billing system examined at one health department, billing experiences may generally reflect standard practices in medical payment. Yet, serious efforts to streamline bill submission and payment windows are underway in other billing settings.24 Given the professionalized nature of medical billing, LHDs may benefit from exploring and incorporating best practices in medical billing across the health-care delivery system. Particular attention should be paid to the portions of the billing process that are amenable to health department intervention, including streamlining time from service delivery to submission of reimbursement claim or integration of an electronic billing system.
Limitations
Findings from this study should be viewed in light of several limitations. Billing practices and experiences may be highly localized across health departments and states. Other settings may experience reimbursement lags of varying durations. Arizona and TAPI are participants in CDC's Billables Project,17 suggesting that lags persist in a setting that has previously received enhanced technical assistance to establish a billing program. Information on date of service and date of reimbursement receipt is retained in one data system, while information on the date that a claim was originally submitted to a payer is retained separately. Manual matching of these two large data systems was outside the scope of this project. Standard practice at TAPI is to electronically submit bills to payers no more than one week from receipt of a paper claim. It generally takes several days (one to two weeks at certain times of the year) for paper claims to be delivered to TAPI from MCDPH. Both of these periods were included in the lag between service and reimbursement, although other settings with different workflows or procedures may experience different durations between service and submission of claims for reimbursement. This study did not examine the level of reimbursement for certain procedures or billing codes, including amounts reimbursed relative to private providers. Future studies in this area may shed additional light on important billing practices, such as the time between service delivery and claim submission.
CONCLUSION
In this setting, LHD-run immunization clinics served as a source of important public health services for more than 28,000 uninsured children in FY2014. Assuring a health department's ability to provide these services in a financially sustainable manner requires an efficient and effective clinical billing component.
Budgeting for new or expanded clinical service billing must recognize and account for challenges, including a substantial lag between service delivery and reimbursement receipt. The findings from this study demonstrate that a sizable portion of revenues from billing is likely to be received in a different budget period than when the services were delivered. Thus, administrative flexibility may be essential in the budget setting process for services or divisions in LHDs that receive clinical billing revenues. Efforts to improve the quality or efficiency of service delivery of LHDs may benefit from consideration of strategies to shorten the window between service delivery and submission of claims, which is especially important for new or expanded service lines and the large upfront expenditures they often require.
This study contributes to a nascent body of -empirical evidence on issues that confront health departments engaged in clinical billing. More practice-based research may help identify and test promising practices for financial best practices for receiving and accounting for billing revenues. Billing by health departments is recognized as widespread,8 rational,12 and in alignment with the broader health department mission.13 A next generation of research centering on evidence from the field can help to identify challenges to successful billing and promote dissemination of best practices.
Footnotes
This study was reviewed by the Arizona State University Institutional Review Board (IRB) and was determined to be exempt from IRB review and approval.
REFERENCES
- 1.Centers for Disease Control and Prevention (US) The public health system and the 10 essential public health services [cited 2015 Feb 17] Available from: http://www.cdc.gov/nphpsp/essentialservices.html.
- 2.Keane C, Marx J, Ricci E. Privatization and the scope of public health: a national survey of local health department directors. Am J Public Health. 2001;91:611–7. doi: 10.2105/ajph.91.4.611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Institute of Medicine. Washington: National Academies Press; 2002. The future of the public's health in the 21st century. [PubMed] [Google Scholar]
- 4.Ten great public health achievements—United States, 1900–1999. MMWR Morb Mortal Wkly Rep. 1999;48(12):241–3. [PubMed] [Google Scholar]
- 5.Szilagyi PG, Humiston SG, Shone LP, Barth R, Kolasa MS, Rodewald LE. Impact of vaccine financing on vaccinations delivered by health department clinics. Am J Public Health. 2000;90:739–45. doi: 10.2105/ajph.90.5.739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schaffer SJ, Fontanesi J, Rickert D, Grabenstein JD, Rothholz MC, Wang SA, et al. How effectively can health care settings beyond the traditional medical home provide vaccines to adolescents? Pediatrics. 2008;121(Supplement 1):S35–45. doi: 10.1542/peds.2007-1115E. [DOI] [PubMed] [Google Scholar]
- 7.Zhou F, Santoli J, Messonnier ML, Yusuf HR, Shefer A, Chu SY, et al. Economic evaluation of the 7-vaccine routine childhood immunization schedule in the United States, 2001. Arch Pediatr Adolesc Med. 2005;159:1136–44. doi: 10.1001/archpedi.159.12.1136. [DOI] [PubMed] [Google Scholar]
- 8.National Association of County and City Health Officials. Washington: -NACCHO; 2014. 2013 national profile of local health departments. [Google Scholar]
- 9.Lindley MC, Shen AK, Orenstein WA, Rodewald LE, Birkhead GS. Financing the delivery of vaccines to children and adolescents: challenges to the current system. Pediatrics. 2009;124(Suppl 5):S548–57. doi: 10.1542/peds.2009-1542O. [DOI] [PubMed] [Google Scholar]
- 10.Kilgus D. Innovative projects to improve reimbursement in public health department clinics. 2011 [cited 2015 Jun 10] Available from: http://www.cdc.gov/vaccines/programs/billables-project/downloads/billing-partner-brief-kilgus-2011-slides.pdf.
- 11.Willard R, Shah GH, Leep C, Ku L. Impact of the 2008–2010 economic recession on local health departments. J Public Health Manag Pract. 2012;18:106–14. doi: 10.1097/PHH.0b013e3182461cf2. [DOI] [PubMed] [Google Scholar]
- 12.England B. Billing for public health services: perfectly rational, and yet…. J Public Health Manag Pract. 2015;21(Suppl 1):S76–80. doi: 10.1097/PHH.0000000000000137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Costich JF. Local health departments as essential community providers for health benefits exchange plans. Am J Public Health. 2014;104:e12–4. doi: 10.2105/AJPH.2013.301830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Newman SJ, Leep CJ. Local health department billing for clinical services: findings from the 2014 Forces of Change Survey. J Public Health Manag Pract. 2014;20:672–5. doi: 10.1097/PHH.0000000000000144. [DOI] [PubMed] [Google Scholar]
- 15.Etkind P, Gehring R, Ye J, Kitlas A, Pestronk R. Local health departments and billing for clinical services. J Public Health Manag Pract. 2014;20:456–8. doi: 10.1097/PHH.0000000000000103. [DOI] [PubMed] [Google Scholar]
- 16.Quintanilla C, Duncan L, Luther L. Billing third party payers for vaccines: state and local health department perspectives. J Public Health Manag Pract. 2009;15:E1–5. doi: 10.1097/PHH.0b013e3181a23dd5. [DOI] [PubMed] [Google Scholar]
- 17.Kilgus CD, Redmon GS. Enabling reimbursement to health departments for immunization services. J Public Health Manag Pract. 2014;20:453–5. doi: 10.1097/PHH.0b013e3182a9dc03. [DOI] [PubMed] [Google Scholar]
- 18.Temple University Public Health Law Research Group. Insurance billing for sensitive health services: statutory and regulatory analysis using LawAtlasSM. 2014 [cited 2015 Jun 29] Available from: http://lawatlas.org/files/std/insurance%20billing%20for%20sensitive%20health%20services%20report.pdf.
- 19.Hinman AR, Orenstein WA, Rodewald L. Financing immunizations in the United States. Clin Infect Dis. 2004;38:1440–6. doi: 10.1086/420748. [DOI] [PubMed] [Google Scholar]
- 20.Johnson KA, Sardell A, Richards B. Federal immunization policy and funding: a history of responding to crises. Am J Prev Med. 2000;19(3 Suppl):99–112. doi: 10.1016/s0749-3797(00)00210-5. [DOI] [PubMed] [Google Scholar]
- 21.Santoli JM, Rodewald LE, Maes EF, Battaglia MP, Coronado VG. Vaccines for Children Program, United States, 1997. Pediatrics. 1999;104:e15. doi: 10.1542/peds.104.2.e15. [DOI] [PubMed] [Google Scholar]
- 22.StataCorp. College Station (TX): StataCorp LP; 2013. Stata®: Release 13. [Google Scholar]
- 23.Cunningham PJ, O'Malley AS. Do reimbursement delays discourage Medicaid participation by physicians? Health Aff (Millwood) 2009;28:w17–28. doi: 10.1377/hlthaff.28.1.w17. [DOI] [PubMed] [Google Scholar]
- 24.Green MA, Rowell JC. Clifton Park (NY): Delmar Cengage Learning; 2012. Understanding health insurance: a guide to billing and reimbursement. [Google Scholar]