Abstract
Objective
We assessed the association of neighborhood poverty with HIV diagnosis rates for males and females in New York City.
Methods
We calculated annual HIV diagnosis rates by ZIP Code, sex, and neighborhood poverty level using 2010–2011 New York City (NYC) HIV surveillance data and data from the U.S. Census 2010 and American Community Survey 2007–2011. Neighborhood poverty levels were percentage of residents in a ZIP Code with incomes below the federal poverty threshold, categorized as 0%–<10% (low poverty), 10%–<20% (medium poverty), 20%–<30% (high poverty), and 30%–100% (very high poverty). We used sex-stratified negative binomial regression models to measure the association between neighborhood-level poverty and HIV diagnosis rates, controlling for neighborhood-level education, race/ethnicity, age, and percentage of men who have sex with men.
Results
In 2010–2011, 6,184 people were newly diagnosed with HIV. Median diagnosis rates per 100,000 population increased by neighborhood poverty level overall (13.7, 34.3, 50.6, and 75.6 for low-, medium-, high-, and very high-poverty ZIP Codes, respectively), for males, and for females. In regression models, higher neighborhood poverty remained associated with higher diagnosis rates among males (adjusted rate ratio [ARR] = 1.63, 95% confidence interval [CI] 1.34, 1.97) and females (ARR=2.14, 95% CI 1.46, 3.14) for very high- vs. low-poverty ZIP Codes.
Conclusion
Living in very high- vs. low-poverty urban neighborhoods was associated with increased HIV diagnosis rates. After controlling for other factors, the association between poverty and diagnosis rates was stronger among females than among males. Alleviating poverty may help decrease HIV-related disparities.
More than 40,000 people in the United States are newly diagnosed with human immunodeficiency virus (HIV) every year.1 The National HIV/AIDS Strategy called for a 20% drop in this figure by 2015, and emphasis at the federal level on high-impact prevention is attempting to shift the focus of HIV prevention activities from individuals to entire communities or populations.2,3 Yet, most investigations of the determinants of HIV infection have focused on individual traits, typically identifying people as high risk based on factors such as race/ethnicity or sexual or drug use behaviors. For example, black and Hispanic people have HIV diagnosis rates more than twice that of white people and account for more than two-thirds of HIV diagnoses in the United States. Men who have sex with men (MSM) also account for more than two-thirds of HIV diagnoses.1,4
Area-based social conditions such as neighborhood poverty are increasingly being recognized as important determinants of health inequities, including HIV infection.4–9 In the United States, areas with relatively high poverty (where ≥20% of the population live in households with incomes below the federal poverty threshold) have the highest HIV diagnosis rates and account for about half of all new HIV diagnoses.4 County-level poverty has been shown to be significantly associated with HIV diagnosis rates in the United States, overall, by sex, and by race/ethnicity.8 However, this association has not been explored by ZIP Code within a U.S. city. Cities concentrate health risks, and disaggregating their health information (e.g., by neighborhood poverty level) uncovers disparities.10 Furthermore, it is not known if differences in HIV diagnosis rates by ZIP Code-level poverty can be explained by area-based differences in age and racial/ethnic distribution (e.g., people living in poorer neighborhoods are younger and more likely to be black or Hispanic, which are populations with higher HIV incidence) or area-based poverty is independently associated with HIV diagnosis rates, and whether or not this relationship differs between males and females.
The distribution of people with HIV in New York City (NYC) has been described by neighborhood and area-based poverty level.11 Because local governance is a key force in improving social conditions and reducing health inequalities,10 local demand for expanded analyses that more thoroughly assess the connection between poverty and health exists. The NYC Department of Health and Mental Hygiene (DOHMH) formed the Center for Health Equity in 2014. Its goals are to examine and develop policy that addresses health disparities and their causes, a chief one of which is poverty. To advance these goals, we investigated health disparities related to HIV and poverty among males and females, controlling for other factors.
We conducted an ecological analysis12 using NYC HIV surveillance data to examine if area-based poverty at the ZIP Code level is independently associated with HIV diagnosis rates among males and females.
METHODS
Level of analysis
Variables for our ecological analysis were at the ZIP Code or ZIP Code Tabulation AreaTM (ZCTA) level. ZIP Codes are a system of delineating areas for postal service, and ZCTAs approximate ZIP Codes.13 In NYC, the number of ZIP Codes is fewer (i.e., typically larger in size and population) than the number of census tracts but greater (i.e., typically smaller) than other common geographic units, including congressional districts and counties.
Data sources
We used four data sources for analytic variables (Table 1).
Table 1.
Data sources for analysis of the association between neighborhood poverty and HIV diagnoses among males and females, New York City, 2010–2011
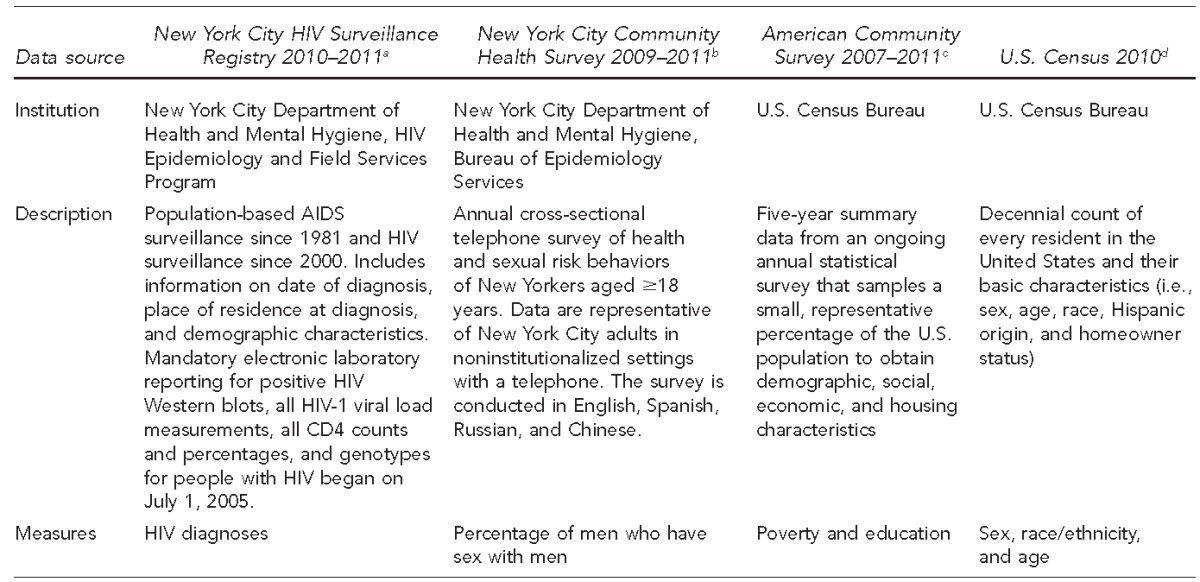
aNash D, Ramaswamy C, Manning S. Implementation of named HIV reporting—New York City, 2001. MMWR Morb Mortal Wkly Rep 2004;52(51 & 52):1248-52.
bNew York City Department of Health and Mental Hygiene. Epiquery: NYC interactive health data: Community Health Survey 2009–2011 [cited 2014 Jan 9]. Available from: http://nyc.gov/health/epiquery
cCensus Bureau (US). 2007–2011 American Community Survey 5-year estimate [cited 2014 Feb 26]. Available from: https://www.census.gov/newsroom/releases/archives/news_conferences/20121203_acs5yr.html
dCensus Bureau (US). 2010 census [cited 2014 Feb 26]. Available from: http://www.census.gov/2010census
HIV = human immunodeficiency virus
AIDS = acquired immunodeficiency syndrome
Outcome measure.
We calculated annualized rates of new HIV diagnoses in 2010–2011 per 100,000 NYC residents aged ≥13 years citywide and for each NYC residential ZIP Code, overall and by sex. We used data from the HIV surveillance registry as of September 30, 2012, as numerators14 and U.S. Census 2010 data as denominators, divided by two to annualize the rates, and multiplied by 100,000. We calculated HIV diagnosis date as the earliest date of a positive HIV Western blot, detectable HIV viral load test, physician diagnosis, or acquired immunodeficiency syndrome (AIDS)-defining condition in a person not previously diagnosed with HIV.
Neighborhood poverty.
We acquired data on neighborhood poverty, the main exposure of interest, from the American Community Survey (ACS) 2007–201115,16 by ZCTA and assigned it based on people's NYC ZIP Code of residence at HIV diagnosis. We defined poverty level as the percentage of residents in each ZIP Code with incomes below the federal poverty threshold: 0% to <10% (low poverty), 10% to <20% (medium poverty), 20% to <30% (high poverty), and 30% to 100% (very high poverty).17 We selected poverty as the primary socioeconomic status (SES) variable and ZIP Code as the geographic level based on recommendations from the NYC DOHMH and the Public Health Disparities Geocoding Project, and because ZIP Code from medical chart reviews was the smallest readily available geographic unit for surveillance information.17–19
We excluded from analysis two of 182 NYC -residential ZIP Codes because they straddled the NYC border. Also, no HIV diagnoses occurred among their NYC residents.
Covariates.
We accounted for potential confounders of the relationship between neighborhood poverty and HIV diagnosis rates by controlling for other neighborhood socioeconomic and demographic characteristics. The other SES covariate was education among people aged ≥25 years (proportion with a bachelor's degree or higher) from ACS 2007–2011.
We developed three demographic covariates. The first, from U.S. Census 2010,20 was the proportion of the population that was black or Hispanic. The second was the proportion of the population that was in the middle 80% of ages of new HIV diagnoses citywide by sex, as an age adjustment to account for differing age distributions by neighborhood. To calculate this proportion, we reviewed the surveillance registry to determine sex-specific age ranges accounting for the middle 80% of diagnoses (for males, 21–53 years; for females, 22–57 years), and then we used U.S. Census 2010 data to determine the proportion of the male or female population of each ZIP Code in those ranges. The third covariate was the prevalence of MSM among sexually active men by United Hospital Fund area (comprising 2–9 ZIP Codes)21 from the NYC Community Health Survey (CHS) 2009–2011. For this measure, the percentage of sexually active males reporting ≥1 male sex partner in the past 12 months22 was weighted to the NYC adult population per U.S. Census 2000 (for CHS 2009 and 2010 data) and U.S. Census 2010 (for CHS 2011 data)23 using SAS®-callable SUDAAN®,24 age-adjusted to the 2000 U.S. standard population, and applied to all ZIP Codes within each United Hospital Fund area. Because we were interested in the total association between poverty and HIV, and because marital status is a mediator between poverty and HIV,25 we did not include marital status in the model.
Analytic method
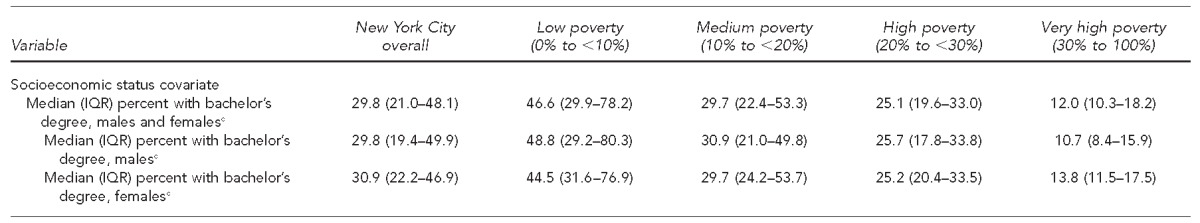
We mapped poverty levels and HIV diagnosis rates for males and females onto NYC ZIP Code base maps (GIS Center, NYC DOHMH) using ArcGIS®.26 Maps showed the distribution and proximity of neighborhoods with the highest diagnosis rates and high or very high poverty. We grouped diagnosis rates approximately as sextiles for males and used the same scale for the map of females; we rounded numbers for easier comprehension and potential future comparisons. We calculated the median and interquartile range of model outcomes and covariates, and number of ZIP Codes with no HIV diagnoses, overall and by sex, by neighborhood poverty level. We also calculated median ZIP Code-level HIV diagnosis rates overall and by sex by neighborhood poverty level and presented them in box plots showing median, interquartile range, and all outliers, using Microsoft® Excel. We then calculated the ratio of median male-to-female ZIP Code-level HIV diagnosis rates within each neighborhood poverty level, and the ratio of median HIV diagnosis rates for very high- vs. low-poverty ZIP Codes for males and females.
We created sex-stratified multivariable negative binomial regression models to determine the association between neighborhood poverty and HIV diagnosis rates for males and females, controlling for other neighborhood characteristics. To account for the varying number of people in each ZIP Code and to interpret the results as population rates, we offset our models by the natural log of the sex-specific ZCTA-level population size (i.e., number of males or females aged ≥13 years) from U.S. Census 2010.27
We built models with poverty only (unadjusted, including only the population size offset in addition to poverty) and poverty with other SES and demographic covariates (adjusted). Neighborhood poverty levels were treated as indicator variables in the models, with medium-, high-, and very high-poverty levels as variables and low poverty as the reference category. We constructed sex-stratified models to distinguish MSM from females and examine males overall, because area-based data were available for males but not for MSM. We sought to make the male and female models otherwise as similar as possible. We used SAS® for all analyses.28 We calculated p-values using the Wald chi-squared test.
RESULTS
Of 180 residential ZIP Codes in NYC, 65 (36.1%) were low-, 55 (30.6%) were medium-, 34 (18.9%) were high-, and 26 (14.4%) were very high-poverty ZIP Codes (Table 2). In 2010–2011, 6,184 people aged ≥13 years and living in these 180 ZIP codes were newly diagnosed with HIV (4,754 males and 1,430 females), for an overall annualized HIV diagnosis rate of 44.8 per 100,000 population. ZIP Code-level populations ranged from 130 to 89,231 people, and diagnosis rates ranged from 0.0 to 241.7 per 100,000 population. The median ZIP Code-level annualized diagnosis rates were 34.8 per 100,000 population overall, 56.2 per 100,000 males, and 10.4 per 100,000 females (Table 2).
Table 2.
Distribution of outcomes and demographic and socioeconomic covariates for models of HIV diagnosis rates, by neighborhood (ZIP Code) poverty level, among New York City ZIP Codes (n=180) overall and by ZIP Code poverty level, for males and females aged ≥13 years, New York City, 2010–2011
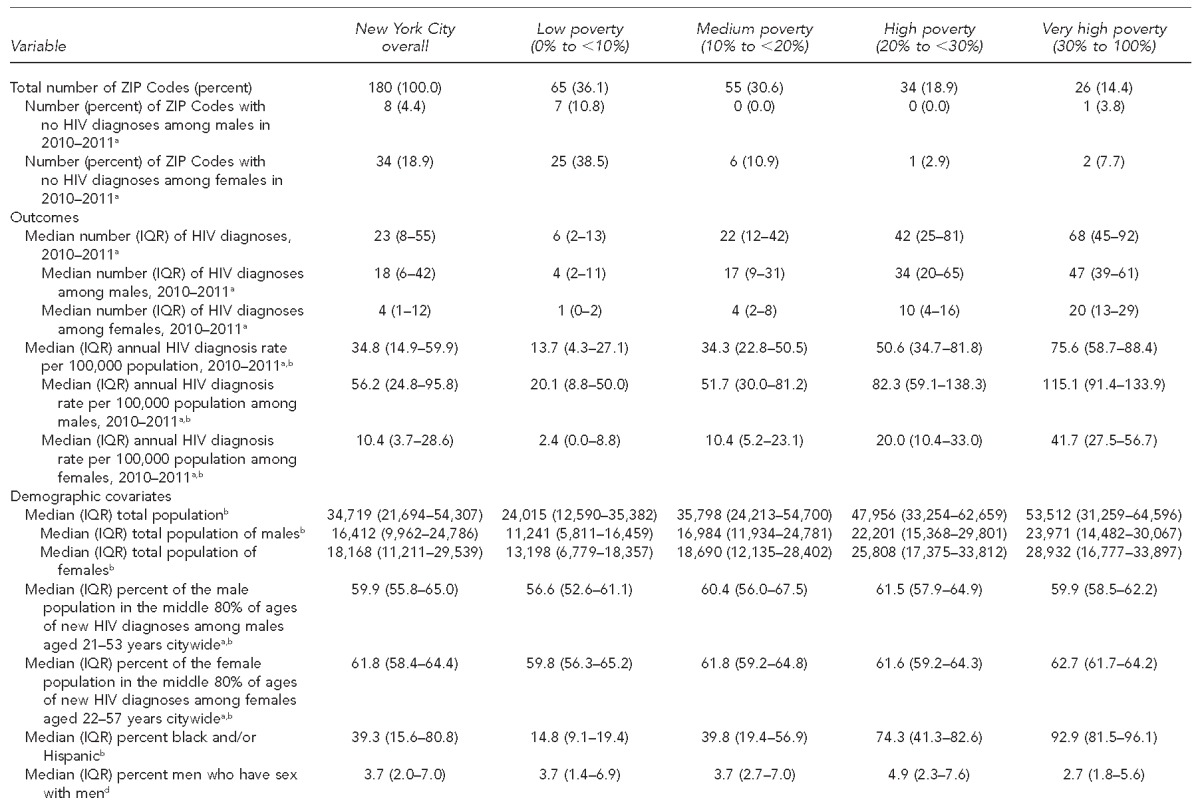
aNew York City Department of Health and Mental Hygiene, HIV Epidemiology and Field Services Program. 2012.
bCensus Bureau (US). 2010 census [cited 2014 Feb 26]. Available from: http://www.census.gov/2010census
cCensus Bureau (US). 2007–2011 American Community Survey 5-year estimate [cited 2014 Feb 26]. Available from: https://www.census.gov/newsroom/releases/archives/news_conferences/20121203_acs5yr.html
dNew York City Department of Health and Mental Hygiene. Epiquery: NYC interactive health data: Community Health Survey 2009–2011 [cited 2014 Jan 9]. Available from: http://nyc.gov/health/epiquery
HIV = human immunodeficiency virus
IQR = interquartile range
We found substantial overlap of high- or very high-poverty ZIP Codes and high HIV diagnosis rates, and ZIP codes adjacent to each other often had similar levels of poverty and diagnosis rates. We found several large concentrations of high- or very high-poverty ZIP codes with high diagnosis rates among males and females, particularly in Central Brooklyn, Upper Manhattan's Harlem and Washington Heights areas, and the South Bronx. One area, Chelsea and Greenwich Village in Lower Manhattan, had notably high diagnosis rates, primarily among males, accompanied by relatively low poverty (Figures 1a–c).
Figure 1.
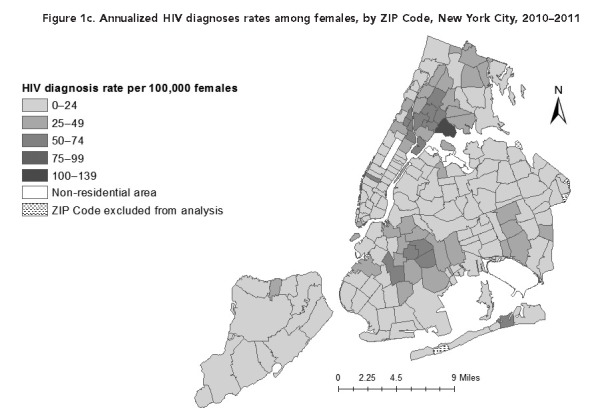
Poverty and annualized HIV diagnoses rates among males and females, by ZIP Code, New York City, 2010–2011
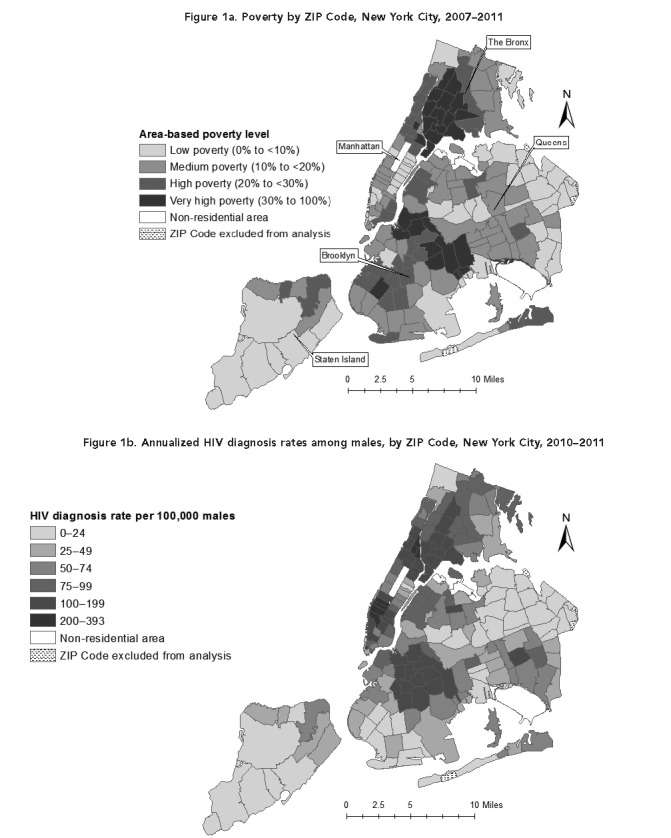
Diagnosis rates increased as ZIP Code-level poverty increased (median annualized diagnosis rates per 100,000 population: 13.7 in low-, 34.3 in medium-, 50.6 in high-, and 75.6 in very high-poverty ZIP Codes). This gradient was present overall as well as for both males and females (rates per 100,000 males: 20.0, 51.7, 82.3, and 115.1 for low-, medium-, high-, and very high-poverty ZIP Codes, respectively; rates per 100,000 females: 2.4, 10.4, 20.0, and 41.7 for low-, medium-, high-, and very high-poverty ZIP Codes, respectively). At each poverty level, males had higher diagnosis rates than females (Figures 2a–c).
Figure 2.
Annualized HIV diagnosis rates per 100,000 males aged ≥13 years, by ZIP Code poverty level (percentage of population below federal poverty threshold), (a) overall, (b) among males, and (c) among females, New York City, 2010–2011a
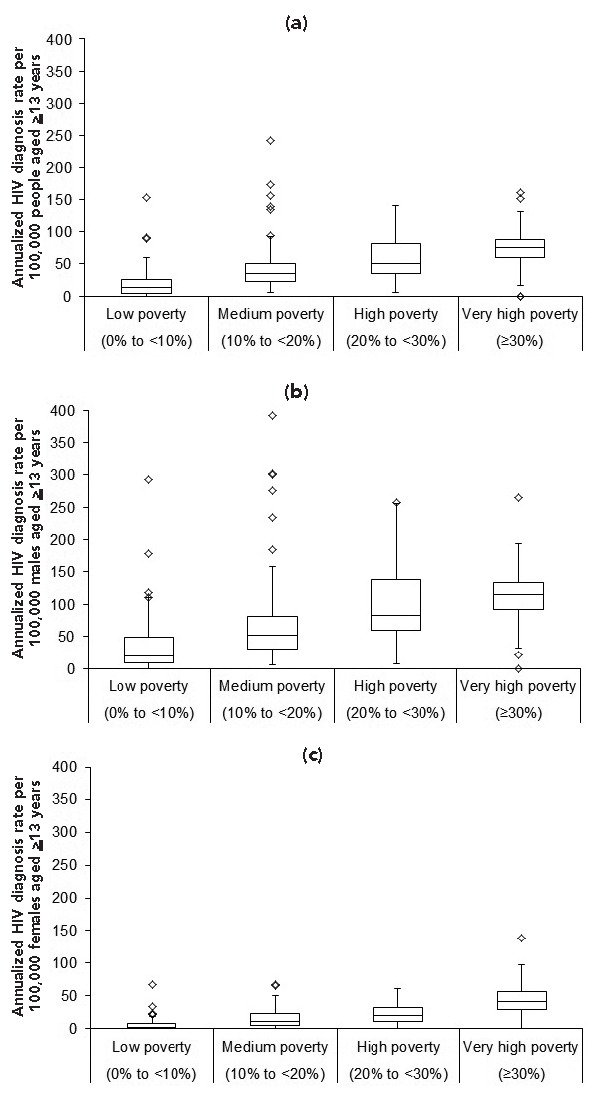
aBoxes include ZIP Codes with diagnosis rates between the first and third quartile of diagnosis rates within the poverty level. The line in each box is the median ZIP Code-level diagnosis rate within the poverty level. Ends of the whiskers are set at 1.5* interquartile range (IQR) above the third quartile and 1.5*IQR below the first quartile. Each diamond (◊) represents one ZIP Code outlier.
However, relative differences in diagnosis rates across poverty levels were starker for females than for males. Among females, residents of very high-poverty ZIP Codes were 17 times more likely than their counterparts in low-poverty ZIP Codes to be diagnosed with HIV, whereas males were six times more likely than their counterparts in low-poverty ZIP Codes to be diagnosed with HIV. The relative difference between median male and female diagnosis rates by poverty level decreased with increasing poverty (e.g., the male rate was eight times higher than the female rate in low-poverty ZIP Codes vs. three times higher than the female rate in very high-poverty ZIP Codes).
Compared with low-poverty ZIP codes, crude rate ratios of diagnosis rates increased significantly with each increase in ZIP Code-level poverty among both males and females, ultimately reaching 2.42 (95% confidence interval [CI] 2.10, 2.78) for males in very high-poverty ZIP Codes and 6.52 (95% CI 4.81, 8.84) for females in very high-poverty ZIP Codes (p<0.001). After controlling for other ZIP Code-level demographic and SES characteristics (e.g., racial/ethnic composition, age distribution, proportion MSM [for males], and education), higher ZIP Code-level poverty remained significantly associated with higher HIV diagnosis rates among both males and females. For example, for very high-poverty vs. low-poverty ZIP Codes, the adjusted rate ratio was 1.63 (95% CI 1.34, 1.97) among males and 2.14 (95% CI 1.46, 3.14) among females (p<0.001) (Table 3).
Table 3.
Poisson regression analyses of the association between neighborhood poverty and HIV diagnosis rates among males and females in 180 ZIP Codes, New York City, 2010–2011
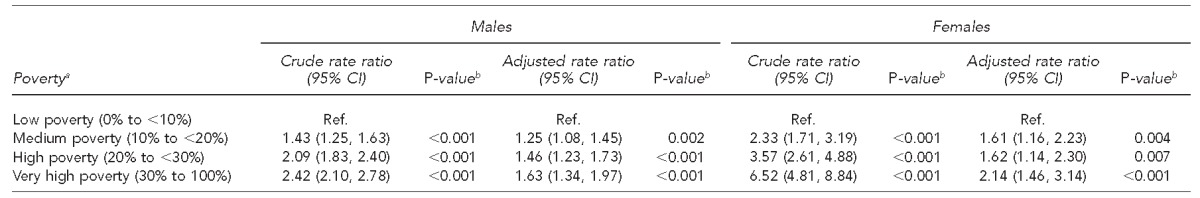
aPoverty is defined as the percentage of the population below the federal poverty threshold.
bP-values were calculated using the Wald chi-squared test.
HIV = human immunodeficiency virus
CI = confidence interval
Ref. = reference group
DISCUSSION
To our knowledge, this analysis was the first ecological analysis of HIV diagnosis rates and poverty at the ZIP Code level and in a U.S. city, and one of few analyses to assess sex differences in the poverty-HIV relationship. We found a direct relationship between neighborhood poverty and annualized HIV diagnosis rates, with neighborhoods that had higher levels of poverty having, on average, higher HIV diagnosis rates. Males had higher diagnosis rates than females at every poverty level, but the relative difference between low- and high-poverty neighborhoods was particularly large for women. Similarly, the relative difference between male and female diagnosis rates narrowed with increasing neighborhood poverty. After adjusting for other neighborhood characteristics, living in very high- vs. low-poverty neighborhoods was associated with an increase in HIV diagnosis rates of 63% for males and 114% for females. For females, diagnosis rates in medium- or high-poverty neighborhoods were elevated about as much as diagnosis rates for males in very high-poverty neighborhoods. These larger effect measures for females than males at each poverty level suggest that the overall association between poverty and HIV diagnosis rates was stronger among females than among males.
We focused entirely on the association between neighborhood poverty and HIV diagnosis rates, accounting for other neighborhood characteristics, assuming that background HIV prevalence and risk are influenced by these other characteristics.12,29 The ratio of diagnosis rates in very high- to low-poverty neighborhoods was attenuated in the multivariable models, suggesting that racial/ethnic distribution, age distribution, education level, and (for males) prevalence of MSM among sexually active males are also associated with HIV diagnoses. The attenuation was especially large for females, indicating that these other non-poverty neighborhood-level factors explained more of the crude HIV diagnosis rates for females than for males. This difference supports continued sex-specific HIV prevention (i.e., interventions targeting either males or females) and underscores the potential influence of neighborhood-level HIV prevention interventions in general for females. This finding is also consistent with results of a previous study of HIV diagnosis rates by county in the United States, which found that, although HIV diagnosis rates increased as community poverty level increased, this association varied by sex and race/ethnicity.8
Data for this analysis were from NYC, a diverse city that has the largest HIV epidemic in the western hemisphere and substantial income inequality.30 NYC also has many poor neighborhoods with not only high rates of HIV diagnosis, but also high HIV prevalence and death rates among people with HIV.31 The United States has the highest income inequality of any developed nation,32 which may exacerbate disparities in HIV diagnosis rates across areas.
Our analysis does not explain how poverty influences HIV or why the relative impact of poverty is greater on females than on males. The latter may be partly because a large portion of the HIV epidemic among NYC males is among MSM, who may socialize and have sex in different neighborhoods than those in which they live,33,34 and whose risk for HIV may therefore be less influenced by residential neighborhood poverty levels than the risk for women and heterosexual males. Indeed, in the United States overall, the distribution of HIV cases across neighborhood poverty levels is more balanced for MSM than for heterosexual males.4 To the extent that neighborhood poverty may still influence MSM HIV risk, the lower impact on males than on females could partially be explained by MSM disproportionately living in less-poor neighborhoods. However, it is not clear that MSM disproportionately live in less-poor neighborhoods: although same-sex male couples tend to live in ZIP Codes with higher median property values than do other households,35 and have average incomes exceeding those for opposite-sex couples,36 poverty rates among males living alone are higher among those who are gay than among those who are straight.37 Furthermore, MSM diagnosed with HIV in NYC and the United States are increasingly young, black, and Hispanic, and fewer are older and white.38 If these trends continue and these younger MSM tend to live in poorer neighborhoods than the older MSM, the poverty gradient among males (i.e., the increase in diagnosis rates from low- to very high-poverty neighborhoods) may become more pronounced in the future. Currently, absolute numbers and rates of HIV diagnoses for the United States reveal differences across poverty levels for both sexes, but a smaller relative difference among males than among females4 and no difference for white males.8 We did not find local or U.S. analyses of rates of other sexually transmitted infections by poverty level and sex. A California analysis of poverty and race/ethnicity found that higher census tract-level poverty was associated with higher gonorrhea rates, both overall and within racial/ethnic groups.39 In another study, tuberculosis rates in NYC did not differ by sex but, rather, had relative increases from lowest to higher-poverty neighborhoods that were comparable between males and females.40
Limitations
This study was subject to several limitations. One limitation was the level of geographic analysis and the outcome measured. Although the geographic level at which we analyzed data (i.e., ZIP Code) was finer than that in previous analyses of HIV/AIDS diagnosis rates and area-based poverty (which used county data8,25,41,42), it was still not as fine as has been recommended for optimal detection of area-based public health disparities (i.e., census tract and census block18). Additionally, NYC ZIP Codes have average populations of more than 40,000 people and can be heterogeneous with respect to poverty level, race/ethnicity, and other demographic and socioeconomic characteristics, as would be the case in other densely populated locales. Finally, ZIP Code-level analyses such as ours require using approximations of ZIP Codes (i.e., ZCTAs) to incorporate U.S. Census and ACS data, as those sources do not collect data by ZIP Code.13 These ZIP Code-related limitations notwithstanding, we used ZIP Code because it was the smallest geographic measure readily available in NYC HIV surveillance, and its use is acceptable under these circumstances.17 Additionally, it allowed the division of NYC into 180 geographic groups.
Another limitation was that we investigated HIV diagnosis rates rather than HIV incidence rates, as only diagnoses are reportable to surveillance. Diagnoses require both prior infection and HIV testing, and many people go months or years after infection before they are tested.11 HIV testing behavior, and perhaps testing opportunities, are generally higher in poorer neighborhoods, but testing rates and opportunities are high in NYC overall and in most groups43 and have increased during the last decade. As such, differential testing may have little influence on the association between poverty and HIV diagnosis rates in this setting. New York State's universal testing law44–46 and local campaigns for universal HIV testing (e.g., New York Knows) appear to be improving the detection of HIV infections,47,48 bringing diagnoses even closer in alignment with infections.
Additionally, divergent levels of poverty and income inequality by level of urbanization and U.S. region may limit the generalizability of our findings to other U.S. regions or non-urban areas.49 For example, U.S. black-white HIV prevalence rate ratios have been shown to vary by poverty and urbanization.50
Finally, as in any ecological analysis, our findings should not be applied at the individual level. We found higher poverty at the neighborhood level, but not necessarily the individual level, to be associated with higher diagnosis rates and smaller male-female disparities. Individual-level SES data are not recorded by HIV surveillance.
CONCLUSION
Because neighborhood poverty was associated with HIV diagnosis rates in NYC, our findings support the consideration of interventions that look beyond individual characteristics, such as race/ethnicity and behavioral risk, to implement health-promoting social and structural changes. For example, improving economic status for a group of people51 via urban poverty alleviation strategies at the neighborhood level (and perhaps also at the individual or city level) might help decrease HIV diagnosis rates. Higher-poverty neighborhoods with high sex-specific diagnosis rates may be potential targets for such initiatives. Ensuring that such efforts address and decrease HIV risk among females in higher-poverty neighborhoods might decrease the disproportionate impact of poverty on HIV diagnosis rates among females. Increases during the last decade in HIV diagnoses among young black and Hispanic MSM might exacerbate the poverty-diagnosis link among males and should be monitored for this potential impact. Future research should also investigate the potential influence of neighborhood poverty on the continuum of care for HIV-infected males and females after diagnosis.52,53
Footnotes
The authors thank Susan Resnick of the New York City Department of Health and Mental Hygiene, Division of Informatics Information Technology and Telecommunications, for her map formatting suggestions. This study was a routine analysis of surveillance data that did not require institutional review board review.
REFERENCES
- 1.Centers for Disease Control and Prevention (US) Diagnoses of HIV infection in the United States and dependent areas, 2013. HIV Surveillance Report. 2015;25:1–82. Atlanta: CDC; 2015. [Google Scholar]
- 2.The White House (US), Office of National AIDS Policy. National HIV/AIDS strategy. 2010 [cited 2015 Nov 20] Available from: https://www.whitehouse.gov/administration/eop/onap/nhas.
- 3.Centers for Disease Control and Prevention (US) High-impact HIV prevention: CDC's approach to reducing HIV infections in the United States. 2011 [cited 2015 Nov 20] Available from: http://www.cdc.gov/hiv/policies/hip/hip.html.
- 4.Centers for Disease Control and Prevention (US) Social determinants of health among adults with diagnosed HIV infection in 18 areas, 2005–2009. HIV Surveillance Supplemental Report. 2013;18:1–28. Atlanta: CDC; 2013. [Google Scholar]
- 5.Yen IH, Kaplan GA. Neighborhood social environment and risk of death: multilevel evidence from the Alameda County Study. Am J Epidemiol. 1999;149:898–907. doi: 10.1093/oxfordjournals.aje.a009733. [DOI] [PubMed] [Google Scholar]
- 6.Dean HD, Fenton KA. Addressing social determinants of health in the prevention and control of HIV/AIDS, viral hepatitis, sexually transmitted infections, and tuberculosis. Public Health Rep. 2010;125(Suppl 4):1–5. doi: 10.1177/00333549101250S401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Latkin CA, German D, Vlahov D, Galea S. Neighborhoods and HIV: a social ecological approach to prevention and care. Am Psychol. 2013;68:210–24. doi: 10.1037/a0032704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.An Q, Prejean J, McDavid Harrison K, Fang X. Association between community socioeconomic position and HIV diagnosis rate among adults and adolescents in the United States, 2005 to 2009. Am J Public Health. 2013;103:120–6. doi: 10.2105/AJPH.2012.300853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization, Commission on Social Determinants of Health. Geneva: WHO; 2008. Closing the gap in a generation: health equity through action on the social determinants of health. Final report of the Commission on Social Determinants of Health. [Google Scholar]
- 10.UN-HABITAT, World Health Organization. Geneva: WHO; 2010. Hidden cities: unmasking and overcoming health inequities in urban settings. [Google Scholar]
- 11.New York City Department of Health and Mental Hygiene, HIV Epidemiology and Field Services Program. New York: New York City Department of Health and Mental Hygiene; 2013. HIV surveillance annual report, 2012. [Google Scholar]
- 12.Susser M. The logic in ecological: I. The logic of analysis [published erratum appears in Am J Public Health 1995;85(8 Pt 1):1063] Am J Public Health. 1994;84:825–9. doi: 10.2105/ajph.84.5.825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Census Bureau (US) ZIP Code” Tabulation Areas (ZCTAs”) [cited 2013 Dec 13] Available from: http://www.census.gov/geo/reference/zctas.html.
- 14.Nash D, Ramaswamy C, Manning S. Implementation of named HIV reporting—New York City, 2001. MMWR Morb Mortal Wkly Rep. 2004;52(51 & 52):1248–52. [PubMed] [Google Scholar]
- 15.Census Bureau (US) 2007–2011 American Community Survey 5-year estimate [cited 2014 Feb 26] Available from: https://www.census.gov/newsroom/releases/archives/news_conferences/20121203_acs5yr.html.
- 16.Census Bureau (US) How the Census Bureau measures poverty [cited 2014 Mar 20] Available from: http://www.census.gov/hhes/www/poverty/about/overview/measure.html.
- 17.Toprani A, Hadler JL. New York: New York City Department of Health and Mental Hygiene; 2013. Selecting and applying a standard area-based socioeconomic status measure for public health data: analysis for New York City. [Google Scholar]
- 18.Krieger N, Waterman PD, Chen JT, Soobader MJ, Subramanian SV. Monitoring socioeconomic inequalities in sexually transmitted infections, tuberculosis, and violence: geocoding and choice of area-based socioeconomic measures—the Public Health Disparities Geocoding Project (US) Public Health Rep. 2003;118:240–60. doi: 10.1093/phr/118.3.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shepard CW, Gortakowski HW, Nasrallah H, Cutler BH, Begier EM. Using GIS-based density maps of HIV surveillance data to identify previously unrecognized geographic foci of HIV burden in an urban epidemic. Public Health Rep. 2011;126:741–9. doi: 10.1177/003335491112600517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Census Bureau (US) 2010 census [cited 2014 Feb 26] Available from: http://www.census.gov/2010census.
- 21.New York City Department of Health and Mental Hygiene. New York City United Hospital Fund (UHF) neighborhoods and NYC ZIP Code areas [cited 2013 Dec 20] Available from: http://www.nyc.gov/html/doh/downloads/pdf/survey/uhf_map_100604.pdf.
- 22.New York City Department of Health and Mental Hygiene. Epiquery: NYC interactive health data: Community Health Survey 2009–2011 [cited 2014 Jan 9] Available from: http://nyc.gov/health/epiquery.
- 23.Norton J, Sanderson M, Gupta L, Holder-Hayes E, Immerwahr S, Konty K, et al. Methodology updates to the New York City Community Health Survey. New York City Department of Health and Mental Hygiene: Epi Research Report. 2012:1–12. [Google Scholar]
- 24.RTI International. Research Triangle Park (NC): RTI International; 2008. SUDAAN®: Version 10.0.1. [Google Scholar]
- 25.Song R, Hall HI, Harrison KM, Sharpe TT, Lin LS, Dean HD. Identifying the impact of social determinants of health on disease rates using correlation analysis of area-based summary information. Public Health Rep. 2011;126(Suppl 3):70–80. doi: 10.1177/00333549111260S312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.ESRI. Redlands (CA): ESRI; 2014. ArcMap”: Version 10.2.1. [Google Scholar]
- 27.Osgood DW. Poisson-based regression analysis of aggregate crime rates. J Quant Criminol. 2000;16:21–43. [Google Scholar]
- 28.SAS Institute, Inc. Cary (NC): SAS Institute, Inc.; 2011. SAS®: Version 9.3. [Google Scholar]
- 29.Koopman JS, Longini IM., Jr The ecological effects of individual exposures and nonlinear disease dynamics in populations. Am J Public Health. 1994;84:836–42. doi: 10.2105/ajph.84.5.836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Weinberg DH. Washington: Census Bureau (US); 2011. U.S. neighborhood income inequality in the 2005–2009 American Community Survey Reports. [Google Scholar]
- 31.New York City Department of Health and Mental Hygiene, HIV Epidemiology and Field Services Program. New York: New York City Department of Health and Mental Hygiene; 2014. HIV surveillance annual report, 2013. [Google Scholar]
- 32.Organization for Economic Co-Operation and Development. Washington: OECD; 2013. Crisis squeezes income and puts pressure on inequality and poverty. [Google Scholar]
- 33.Koblin BA, Egan JE, Rundle A, Quinn J, Tieu HV, Cerda M, et al. Methods to measure the impact of home, social, and sexual neighborhoods of urban gay, bisexual, and other men who have sex with men. PLoS One. 2013;8:e75878. doi: 10.1371/journal.pone.0075878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Duncan DT, Kapadia F, Halkitis PN. Examination of spatial polygamy among young gay, bisexual, and other men who have sex with men in New York City: the P18 Cohort Study. Int J Environ Res Public Health. 2014;11:8962–83. doi: 10.3390/ijerph110908962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kolko J. Welcome to the gayborhood. Trulia's blog 2012 Jun 15 [cited 2013 Dec 17] Available from: http://trends.truliablog.com/2012/06/welcome-to-the-gayborhood.
- 36.Census Bureau (US) 2012 American Community Survey 1-year data file: same-sex couples [cited 2015 Dec 9] Available from: https://www.census.gov/programs-surveys/acs/data.html.
- 37.Badgett MVL, Durso LE, Schneebaum A. Los Angeles: UCLA School of Law, The Williams Institute; 2013. New patterns of poverty in the lesbian, gay, and bisexual community. [Google Scholar]
- 38.New York City Department of Health and Mental Hygiene, HIV Epidemiology and Field Services Program. New York: New York City Department of Health and Mental Hygiene; 2014. Feb, HIV/AIDS among men who have sex with men (MSM) in New York City, 2012. [Google Scholar]
- 39.Springer YP, Samuel MC, Bolan G. Socioeconomic gradients in sexually transmitted diseases: a geographic information system-based analysis of poverty, race/ethnicity, and gonorrhea rates in California, 2004–2006. Am J Public Health. 2010;100:1060–7. doi: 10.2105/AJPH.2009.172965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.New York City Department of Health and Mental Hygiene. Epiquery: NYC Interactive Health Data: tuberculosis surveillance data 2012 [cited 2014 Sep 16] Available from: http://nyc.gov/health/epiquery.
- 41.Lopez-De Fede A, Stewart JE, Hardin JW, Mayfield-Smith K, Sudduth D. Spatial visualization of multivariate datasets: an analysis of STD and HIV/AIDS diagnosis rates and socioeconomic context using ring maps. Public Health Rep. 2011;126(Suppl 3):115–26. doi: 10.1177/00333549111260s316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gant Z, Lomotey M, Hall HI, Hu X, Guo X, Song R. A county-level examination of the relationship between HIV and social determinants of health: 40 states, 2006–2008. Open AIDS J. 2012;6:1–7. doi: 10.2174/1874613601206010001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.New York City Department of Health and Mental Hygiene. Epiquery: NYC Interactive Health Data: Community Health Survey 2010 [cited 2014 Jan 19] Available from: http://nyc.gov/health/epiquery.
- 44. N.Y.S. Laws, Ch. 308 of the Laws of 2010.
- 45.O'Connell DA, Martin EG, Cutler B, Birkhead GS. The evolution of HIV testing requirements in New York State, 1989–2013. J Acquir Immune Defic Syndr. 2015;68(Suppl 1):S5–9. doi: 10.1097/QAI.0000000000000422. [DOI] [PubMed] [Google Scholar]
- 46.Newton-Dame R, Wang JJ, Kim MS, Edelstein ZR, Cutler B, Tsoi BW. Evaluating the 2010 New York State HIV testing law in NYC ambulatory practices using electronic health records. J Acquir Immune Defic Syndr. 2015;68(Suppl 1):S15–20. doi: 10.1097/QAI.0000000000000407. [DOI] [PubMed] [Google Scholar]
- 47.Myers JE, Braunstein SL, Shepard CW, Cutler BH, Mantsios AR, Sweeney MM, et al. Assessing the impact of a community-wide HIV testing scale-up initiative in a major urban epidemic. J Acquir Immune Defic Syndr. 2012;61:23–31. doi: 10.1097/QAI.0b013e3182632960. [DOI] [PubMed] [Google Scholar]
- 48.Nunn A, Yolken A, Cutler B, Trooskin S, Wilson P, Little S, et al. Geography should not be destiny: focusing HIV/AIDS implementation research and programs on microepidemics in US neighborhoods. Am J Public Health. 2014;104:775–80. doi: 10.2105/AJPH.2013.301864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kusim LD. Washington: Department of Agriculture (US); 2013. Rural America at a glance: 2013 edition. [Google Scholar]
- 50.Vaughan AS, Rosenberg E, Shouse RL, Sullivan PS. Connecting race and place: a county-level analysis of white, black, and Hispanic HIV prevalence, poverty, and level of urbanization. Am J Public Health. 2014;104:e77–84. doi: 10.2105/AJPH.2014.301997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Blankenship KM, Friedman SR, Dworkin S, Mantell JE. Structural interventions: concepts, challenges and opportunities for research. J Urban Health. 2006;83:59–72. doi: 10.1007/s11524-005-9007-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cohen SM, Van Handel MM, Branson BM, Blair JM, Hall HI, Hu X, et al. Vital signs: HIV prevention through care and treatment—United States. MMWR Morb Mortal Wkly Rep. 2011;60(47):1618–23. [PubMed] [Google Scholar]
- 53.Nachega JB, Marconi VC, van Zyl GU, Gardner EM, Preiser W, Hong SY, et al. HIV treatment adherence, drug resistance, virologic failure: evolving concepts. Infect Disord Drug Targets. 2011;11:167–74. doi: 10.2174/187152611795589663. [DOI] [PMC free article] [PubMed] [Google Scholar]


