Abstract
Rationale
Food insecurity has emerged as an important, and potentially modifiable, risk factor for depression. Few studies have brought longitudinal data to bear on investigating this association in sub-Saharan Africa.
Objective
To estimate the association between food insufficiency and depression symptom severity, and to determine the extent to which any observed associations are modified by social support.
Methods and Results
We conducted a secondary analysis of population-based, longitudinal data collected from 1,238 pregnant women during a three-year cluster-randomized trial of a home visiting intervention in Cape Town, South Africa. Surveys were conducted at baseline, 6 months, 18 months, and 36 months (85% retention). A validated, single-item food insufficiency measure inquired about the number of days of hunger in the past week. Depression symptom severity was measured using the Xhosa version of the 10-item Edinburgh Postnatal Depression Scale. In multivariable regression models with cluster-correlated robust estimates of variance, lagged food insufficiency had a strong and statistically significant association with depression symptom severity (β=0.70; 95% CI, 0.46-0.94), suggesting a 6.5% relative difference in depression symptom severity per day of hunger. In stratified analyses, food insufficiency had a statistically significant association with depression among women with low levels of instrumental support. Using quantile regression, we found that the adverse impacts of food insufficiency were experienced to a greater degree by women in the upper end of the conditional distribution of depression symptom severity. Estimates from fixed-effects regression and fixed-effects quantile regression, accounting for unobserved confounding by time-invariant characteristics, were similar.
Conclusions
Food insufficiency was associated with depression symptom severity, particularly for women in the upper end of the conditional depression distribution. Instrumental social support buffered women against the adverse impacts of food insufficiency.
Keywords: food insufficiency, depression, social support, South Africa
INTRODUCTION
Depressive disorders are among the most disabling conditions worldwide, comprising a substantial proportion of the global burden of disease (Whiteford et al., 2013). The social and economic conditions of poverty -- including stressful life events, social exclusion, malnutrition, and other stressors that are particularly pervasive in resource-limited settings -- have been linked to increased risks of developing depressive disorders generally (Lund et al., 2010) as well as during critical periods such as pregnancy and postpartum (Fisher et al., 2012). The public health impacts of untreated or sub-optimally treated depression extend beyond index cases, as depression has been shown to undermine economic productivity (Ettner, Frank, & Kessler, 1997), and maternal depression compromises caregiving and child health (Perry, 2008; Rahman, Iqbal, Bunn, Lovel, & Harrington, 2004; Tsai & Tomlinson, 2012).
Food insecurity, which occurs whenever the availability of nutritionally adequate food or the ability to procure food in culturally acceptable ways is limited or uncertain (Anderson, 1990), has recently emerged as a particularly important -- and potentially modifiable -- risk factor for depression. The construct of food insecurity comprises a number of different concepts, including food insufficiency, inadequacy of coping strategies, and hunger. While numerous cross-sectional studies from resource-limited settings have examined the association between food insecurity and mental health, only four of these have examined this relationship using longitudinal data (Cole & Tembo, 2011; Hadley & Patil, 2008; Maes, Hadley, Tesfaye, & Shifferaw, 2010; Tsai et al., 2012). Pregnancy and the puerperium represent particularly vulnerable periods for women, yet in two recently published systematic reviews of risk factors for postpartum depression (Fisher et al., 2012; Yim, Tanner Stapleton, Guardino, Hahn-Holbrook, & Dunkel Schetter, 2015), only three studies -- all cross-sectional, and only one conducted in sub-Saharan Africa (Dewing, Tomlinson, le Roux, Chopra, & Tsai, 2013) -- were noted to have assessed the association between food insecurity and postpartum depression. Finally, all of these studies have focused exclusively on investigating locational shifts in the distribution of depression, with less attention paid to the shape of the distribution. This is an important gap in the literature: if the effects of a potential food security intervention vary across the distribution of depression in a population, then this could provide insight into vulnerable subgroups who might benefit the most from such interventions. The overall thrust of this body of research is that food insecurity, food insufficiency, and hunger all exert negative impacts on mental health, but significant gaps remain.
To address these gaps in the literature, we conducted a secondary analysis of population-based, longitudinal data collected from 1,238 pregnant women during a three-year cluster-randomized trial in Cape Town, South Africa. The study’s primary aim was to determine whether a community-based home visiting program could improve maternal and child health over three years post-delivery. With repeated measures of both food insufficiency and depression symptom severity, these data offered us the opportunity to estimate their relationship while adjusting for both observed and unobserved confounding.
CONCEPTUAL FRAMEWORK
Our conceptual framework draws heavily on Pearlin and colleagues’ (Pearlin, 1989, 1999; Pearlin, Lieberman, Menaghan, & Mullan, 1981) conceptualization of stressors as being rooted in social and economic structures of daily living. Stressors with more consequential impacts for mental health are those for which culturally embedded aspects of role function are particularly implicated (Kessler, Price, & Wortman, 1985). In settings of generalized poverty where subsistence-level strategies are needed to ensure household viability, food insufficiency should be expected to emerge as a strong predictor of emotional distress, particularly among women, who occupy a central role in food production for their households (Quisumbing, Brown, Feldstein, Haddad, & Pena, 1995). In many countries in sub-Saharan Africa, insufficiency of food is the predominant stressor experienced in daily living (Pike & Patil, 2006).
In many ways, the hypothesized association between food insecurity and depression provides a unique illustration of Krieger’s (2001) concept of embodiment. In Krieger’s (2001) formulation, embodiment is defined as “how we literally incorporate, biologically, the material and social world in which we live” (p.672). Peri-urban South Africa has been described as an environment that compromises the well-being of women, who are subject to numerous co-occurring and potentially synergistic (i.e., “syndemic” (Singer, 1994; Tsai & Burns, 2015)) psychosocial health risks. These risks include depression, non-communicable disease, intimate partner violence, HIV, and substance abuse (Dewing, Tomlinson, le Roux, Chopra, & Tsai, 2013; O’Connor et al., 2011; Pitpitan et al., 2013; Tomlinson et al., 2014). Qualitative work has described how structural violence (Farmer, 1999) plays a fundamental role in undermining South African women’s access to affordable, reliable, and healthy food, and how the resulting food insecurity in turn becomes manifest as poor health (Mendenhall, 2015; Mendenhall & Norris, 2015). The lived experiences of these chronic, conjoint health risks as “daily stressors” (Miller & Rasmussen, 2010) may uniquely erode coping resources, ultimately converging to result in “syndemic suffering” (Mendenhall & Norris, 2015).
In an analysis of food insecurity and emotional distress in urban Ethiopia, Maes, Hadley, Tesfaye, and Shifferaw (2010) hypothesized that the adverse mental health impacts of food crises could potentially be moderated by social networks of psychological support and exchange. Their hypothesis is consistent with the theory that social support exerts a “buffering,” or moderating, influence against life stressors (Cassel, 1976; Cobb, 1976). We therefore hypothesized that the association between food insufficiency and depressed mood would be weaker among women with less social support. We further hypothesized that the extent of buffering would be strongest for instrumental social support rather than emotional social support. This hypothesis is consistent with the “matching” theory (Cohen & McKay, 1984), which predicts that the experience of food insufficiency should be most effectively buffered with support that is delivered in the form that most closely counters the stressor. Thus, we expected that instrumental support -- as distinguished from emotional, informational, or diffuse support (Cohen & Wills, 1985) -- would be the most relevant type of social support to consider when testing the buffering hypothesis.
METHODS
Ethics Statement
All research assistants received training on how to administer surveys for gathering sensitive information and provided assurances of confidentiality. Written informed consent was obtained from all study participants. The survey was framed generally as being part of a study of family health and well-being. In consultation with on-site supervisors, research assistants provided referrals to local counseling resources and/or child social services as needed, with standardized protocols in place to refer women to emergency services in the case of acutely elevated risk of harm to self or harm from others. All study procedures were approved by the South General Institutional Review Board of the University of California at Los Angeles and the Health Research Ethics Committee of the Stellenbosch University Faculty of Health Sciences. A four-person Data Safety Monitoring Board populated by local and international experts monitored implementation of the study.
Study Population
The protocol for the randomized trial was registered with ClinicalTrials.gov (NCT00972699), and the 6-, 18-, and 36-month outcomes have been published (le Roux, Rotheram-Borus, Stein, & Tomlinson, 2014; le Roux et al., 2013; Rotheram-Borus et al., 2011; Rotheram-Borus et al., 2014; Rotheram-Borus, Tomlinson, Roux, & Stein, 2015). The study was conducted in three informal settlements near Cape Town, South Africa, where major community health challenges include HIV, tuberculosis, malnutrition, and alcohol use (Hartley et al., 2011; O’Connor et al., 2011; Tomlinson et al., 2014). Research assistants went from house to house to identify all pregnant women living in 24 neighborhoods (matched on population density, number of bars, distance to health care, and access to public works infrastructure) and invited their participation in the study. Only 2 percent of pregnant women refused participation. These matched neighborhoods were randomized in blocks of four to either a home visiting intervention or standard clinic care groups. Standard clinic care was available (within 5 kilometers) to all women living in the study catchment area and generally consisted of tuberculosis and HIV testing, partner HIV testing, antiretroviral therapy, antenatal and postnatal care, well-child clinics, and primary health care (Rotheram-Borus et al., 2011).
The intervention was implemented by the Philani Maternal, Child Health, and Nutrition Project, a non-governmental organization operating in South Africa since 1979 and more recently in Ethiopia and Swaziland. Their “mentor mother” program recruits women from the community who have successfully raised thriving children despite concentrated adversity, and then provides them with paraprofessional training to conduct home visits among pregnant women in the community. In the cluster-randomized trial, the standard Philani intervention was standardized and augmented with problem-solving and cognitive-behavioral techniques to address major community health challenges, including HIV, tuberculosis, malnutrition, and alcohol use (Rotheram-Borus et al., 2011). Survey data were collected at baseline, 6 months, 18 months, and 36 months by Xhosa-speaking research assistants. Participants completed all assessments between 2009 and 2014. Previous publications have reported that the “Philani Plus” intervention improved a wide range of maternal and child health outcomes related to HIV prevention behaviors, breastfeeding, child growth, and emotional well-being (le Roux, Rotheram-Borus, Stein, & Tomlinson, 2014; le Roux et al., 2013; Rotheram-Borus et al., 2014; Rotheram-Borus, Tomlinson, Roux, & Stein, 2015). The secondary analysis described in this article utilized the full set of data from the randomized trial.
Primary Variables of Interest
The outcome of interest was depression symptom severity, which was measured at all time points using the Xhosa version of the 10-item Edinburgh Postnatal Depression Scale (EPDS) (Cox, Holden, & Sagovsky, 1987). Scale items inquire about depressive symptoms within a seven-day recall period, with responses scored on a four-point Likert-type scale ranging from 0 (“not at all”) to 3 (“all the time”). As a screening instrument, the EPDS measurements should not be regarded as equivalent to clinical diagnoses of major depressive disorder (with or without postpartum onset) as made by mental health professionals. The EPDS measures the affective and cognitive symptoms that typically accompany depressive disorders (Kagee, Tsai, Lund, & Tomlinson, 2013). In this specific population of Xhosa-speaking pregnant and postpartum women, the EPDS has been shown to have a coherent internal structure (De Bruin, Swartz, Tomlinson, Cooper, & Molteno, 2004), high sensitivity and specificity for detecting major depressive disorder (Hung et al., 2014; Tsai et al., 2013; Tsai et al., 2014), and good construct validity (Dewing, Tomlinson, le Roux, Chopra, & Tsai, 2013; Hartley et al., 2011). Its internal consistency was confirmed in the baseline sample: the Cronbach’s alpha was 0.89, with a 95% confidence interval [CI] (computed using 500 bootstrap replications) of 0.88-0.90.
Food insufficiency was measured using a single-item question, “How many days in the past week have you gone hungry? By this I mean days when you felt you didn’t have enough to eat.” While single-item measures of food insufficiency have been validated in population-based studies in sub-Saharan Africa (Tsai et al., 2011; Weiser et al., 2007) and the U.S. (Briefel & Woteki, 1992), the specific measure used in our study had not heretofore been validated among Xhosa-speaking women. Therefore, at the 36-month follow-up interview we simultaneously administered the Household Food Insecurity Access Scale (HFIAS) to provide additional evidence of construct validity (see Electronic Supplementary Appendix).
The breadth of each participant’s emotional and instrumental support was measured, at baseline only, with a series of ten questions about trust and support from intimate partners and family members derived from the Significant Others Scale (Power, Champion, & Aris, 1988). These items inquire about frequency of instrumental support and the extent to which a participant has an intimate partner, mother, or father she trusts and from whom she receives emotional or instrumental support. Six of the items relate to emotional support, and four of the items relate to instrumental support (see Electronic Supplementary Appendix). To generate the indices of emotional and instrumental support, following Kling, Liebman, and Katz (2007) we defined summary indices as the equally weighted average of the z-scores: each item was standardized to a mean of 0 and standard deviation of 1, the summary emotional support index was defined as the average value across the six standardized items, and the summary instrumental support index was defined as the average value across the four standardized items.
Other Covariates
In the multivariable regression models, we adjusted for a number of different time-invariant and time-varying covariates. Time-invariant covariates were elicited at the baseline interview and included binary indicators denoting whether the participant had been randomized to an intervention or standard clinic care cluster, age at baseline, and whether the mother had completed high school. Household asset wealth was elicited by asking participants a series of 13 questions about household assets and housing characteristics (e.g., whether there is a flush toilet in the home, whether a household member owns a radio, etc.). Then, following the method of Filmer and Pritchett (2001), we applied principal components analysis to these variables. The first principal component was retained and used to define the asset wealth index, and participants were sorted into quintiles of relative asset wealth.
Time-varying covariates were elicited at baseline, 6 months, 18 months, and 36 months. Time elapsed since the baseline interview was measured in months. We included binary indicators denoting whether the participant was employed (either full- or part-time) and whether the father of the child remained with the participant as an intimate partner. Additionally we adjusted for several indicators of health status, given that poor health may compromise food-securing activities (Hyder et al., 2005) and may also be a risk factor for depression (Polsky et al., 2005): HIV serostatus (classified as HIV-positive, HIV-negative, or unknown/refused testing), and whether the participant had been diagnosed with high blood pressure or diabetes. Household monthly income was measured in South African Rand. Alcohol abuse was measured with the three-item consumption subset of the Alcohol Use Disorders Identification Test (AUDIT-C) (Saunders, Aasland, Babor, de la Fuente, & Grant, 1993).
Statistical Analysis
Given that the data were characterized by a repeated measures design, we sought to estimate the association between food insufficiency and depression symptom severity, while adjusting for the time-invariant and time-varying covariates described above. We fit a linear regression model to the pooled cross-sectional data, specifying the EPDS score as the continuous dependent variable and food insufficiency as the continuous explanatory variable of interest, with cluster-correlated robust estimates of variance (Froot, 1989; Rogers, 1993; Williams, 2000) to correct standard errors for clustering within participants over time. To ensure the correct temporal sequence of the exposure and outcome, food insufficiency was lagged by one assessment period. Thus, the pooled regression estimates provided information about the association between food insufficiency at one time point and depression symptom severity at the subsequent time point (e.g., food insufficiency at 6 months was correlated with depression symptom severity at 18 months). To aid in interpretation of the estimates and because caseness for (probable) depression is frequently of clinical interest, we defined probable depression as EPDS ≥13 (Hung et al., 2014; Rochat et al., 2006; Tsai et al., 2014) and re-fit a logistic regression model to the data. This model specified probable depression as the binary dependent variable and lagged food insufficiency as the explanatory variable of interest. Regression coefficients were transformed to marginal effects for ease of interpretation (Bartus, 2005).
To determine whether the adverse impacts of food insufficiency were experienced to a greater or lesser extent by women at different points in the conditional distribution of depression symptom severity, we used a quantile regression approach (Koenker & Bassett, 1978). By construction, a quantile regression estimates the impact of an explanatory variable on an arbitrarily specified quantile of the dependent variable conditional on specific values of the covariates. Quantile regression models are appropriate models to use when the entire shape of the distribution changes meaningfully and investigating changes in the mean is insufficient; then the analytic aim is to estimate the different associations between an exposure and outcome along the outcome distribution. Specifically, we fit quantile regression models to estimate the association between lagged food insufficiency and the 20th, 40th, 60th, and 80th percentiles of the distribution of EPDS, using a covariance matrix of the asymptotic distribution of the quantile regression estimator that permits within-participant correlation over time (Parente & Santos Silva, 2015). If food insufficiency affects both the location and the shape of the depression distribution, then we would expect to observe systematic differences in the regression coefficient estimates across quintiles.
For a formal assessment of the extent to which the strength of the food insufficiency-depression relationship differed according to baseline social support, we included social support in the regression model along with a product term for the interaction between food insufficiency and social support. If the estimated associations were stronger among women with lower social support (i.e., below the median) at baseline, this pattern of associations was interpreted as evidence favoring the buffering hypothesis. To investigate the matching hypothesis, we examined both instrumental and emotional support as potential effect modifiers. If the interaction term had greater statistical significance for instrumental (vs. emotional) support, this pattern of associations was interpreted as evidence favoring the matching hypothesis.
Finally, we fit a fixed-effects regression model to the data, using within-participant variation over time to identify the estimated associations (Mundlak, 1961). The estimated regression coefficients are interpreted as providing information about the association between changes in food insufficiency and changes in depression symptom severity. This model adjusts for confounding, whether observed or unobserved, that is time-invariant over the period of study. In the setting of this randomized trial, there are two specific examples of omitted variable bias that could be important. Qualitative studies conducted in diverse cultural contexts have shown that feelings of helplessness, shame, and humiliation are central to the experience of food insufficiency (Coates et al., 2006; Hamelin, Beaudry, & Habicht, 2002; Nordanger, 2007). Thus, the observed association between food insufficiency and depression could simply be due to artifactual overlap between both constructs. A related concern is that personality structure may affect the reporting of both food insufficiency and depression symptom severity (Epstein, 1992): For example, if certain types of people are prone to over-report difficulties obtaining food and to also over-report symptoms of depression, then an observed association between food insufficiency and depression could be spurious. In the fixed-effects specification, participants effectively serve as their own controls. Assuming that the unobservable heterogeneity is constant within participants over time (e.g., personality structure is stable in the short term), then the unobserved heterogeneity and any potential overlap in the scales used to measure the exposure and outcome is differenced away. An important limitation of the fixed-effects specification is that, because only within-participant variation is used to estimate the associations, the fixed effects are collinear with all time-fixed covariates; therefore, the fixed-effects regression models contained only the time-varying covariates. To determine whether changes in food insufficiency were differentially associated with changes in depression symptom severity at different points in the conditional depression distribution, we used the fixed-effects quantile regression model Canay (2011) described.
RESULTS
Characteristics of the Sample
Of 1,238 women initially randomized and followed from 2009-2014, there were 117 mother-child dyads in which either the mother or the child died, and these were removed from the study (and, therefore, this analysis) (Rotheram-Borus, Tomlinson, Roux, & Stein, 2015). Of these, 958 (85%) remained at 36-month follow-up (see online supplement for summary details of the sample). Women lost to follow-up had lower depression symptom severity (9.5 vs. 10.9; t=2.62, P=0.01) but had similar levels of food insufficiency (1.17 vs. 1.16; t=−0.07, P=0.94). Women lost to follow-up also had higher levels of emotional support (P=0.10) and were less likely to be employed (P=0.051) but were otherwise similar on other covariates (P-values ranged from 0.10-0.99). Intra-class correlation values showed sufficient variation within participants over time, ranging from 0.19-0.34 for the outcome and exposure variables, and from 0.12-0.66 for the time-varying covariates.
Food Insufficiency and Depression Symptom Severity
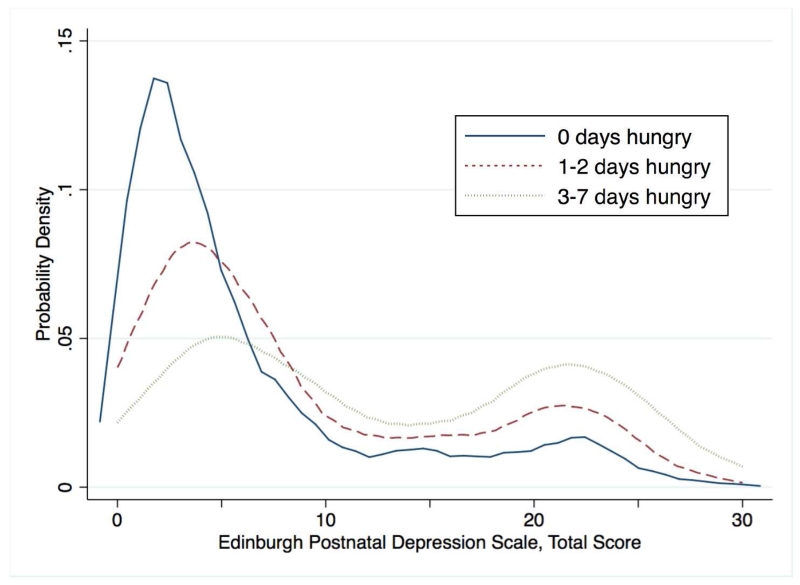
Kernel density plots suggested that food insufficiency was associated with greater depression symptom severity in a dose-response fashion (Figure 1). The changes in both the mean and distribution of depression suggest the need to investigate shape as well as locational shifts in the outcome. In a multivariable regression model, lagged food insufficiency had a strong and statistically significant association with depression symptom severity (β=0.70; 95% CI, 0.46-0.94) (Table 1, column 1). Expressed differently, each additional day in the past week the participant experienced food insufficiency was associated with a 0.7-point increase in the EPDS. Compared with the baseline mean and standard deviation, this estimate represented a 0.7 / 10.7 = 6.5% relative difference (per day of hunger) or 0.7 / 6.98 = 0.1 standard deviation units (per day of hunger). In the logistic regression model, each additional day of food insufficiency was associated with a 2.4 percentage point difference (95% CI, 1.4-3.3) in probable depression. Compared with the baseline prevalence of probable depression, this estimate represented a 0.024 / 0.39 = 6.2% relative difference (per day of hunger). The quantile regression estimates indicate that the adverse impacts of food insufficiency were experienced to a greater degree by women in the upper end of the conditional depression distribution, with a more than tenfold difference in the magnitudes of the estimated associations among women in the 20th percentile vs. women in the 80th percentile (Table 1, columns 2-5).
Figure 1. Kernel density plot of depression symptom severity, by frequency of food insufficiency.
Table 1. Association between depression symptom severity and lagged food insufficiency.
| Predictor | Mean | Q20 | Q40 | Q60 | Q80 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
| β | 95% CI | β | 95% CI | β | 95% CI | β | 95% CI | β | 95% CI | |
| Food insufficient in past week (per day) |
0.70 | 0.46,0.94 | 0.18 | 0.07,0.29 | 0.43 | 0.29,0.57 | 0.85 | 0.49,1.22 | 2.09 | 1.30,2.87 |
| Assigned to intervention arm | −0.10 | −0.72,0.52 | −0.12 | −0.34,0.10 | −0.17 | −0.47,0.13 | −0.08 | −0.60,0.43 | 0.18 | −1.54,1.90 |
| Age (per 5 years) | 0.35 | 0.03,0.67 | 0.10 | −0.00,0.21 | 0.23 | 0.06,0.40 | 0.36 | 0.10,0.61 | 0.35 | −0.68,1.38 |
| Household asset wealth | ||||||||||
| Poorest | Ref | Ref | Ref | Ref | Ref | |||||
| Poorer | −0.73 | −1.72,0.26 | −0.41 | −0.82,−0.00 | −0.40 | −0.87,0.08 | −0.37 | −1.26,0.51 | −1.88 | −6.58,2.81 |
| Middle | −1.14 | −2.21,−0.07 | −0.70 | −1.08,−0.32 | −0.87 | −1.32,−0.41 | −0.96 | −1.91,−0.01 | −2.40 | −6.83,2.03 |
| Richer | −1.02 | −2.09,0.05 | −0.51 | −0.95,−0.07 | −0.59 | −1.05,−0.13 | −0.76 | −1.84,0.31 | −1.11 | −5.96,3.75 |
| Richest | −1.32 | −2.35,−0.28 | −0.58 | −0.98,−0.17 | −0.68 | −1.12,−0.24 | −0.9 | −1.87,0.07 | −2.49 | −6.70,1.72 |
| Completed high school | −1.43 | −2.45,−0.41 | −0.42 | −0.84,0.01 | −0.83 | −1.34,−0.31 | −1.06 | −2.00,−0.12 | −4.08 | −6.83,−1.32 |
| Time point | ||||||||||
| Baseline | Ref | Ref | Ref | Ref | Ref | |||||
| 6 months | −0.6 | −1.33,0.12 | 0.06 | −0.23,0.34 | −0.20 | −0.60,0.19 | −0.67 | −1.40,0.06 | −3.33 | −6.29,−0.36 |
| 18 months | −0.66 | −1.40,0.08 | −0.60 | −0.88,−0.32 | −0.97 | −1.39,−0.56 | −0.79 | −1.64,0.06 | −2.07 | −4.93,0.79 |
| Employed | −1.13 | −1.86,−0.41 | −0.35 | −0.62,−0.07 | −0.35 | −0.69,−0.01 | −0.91 | −1.44,−0.38 | −2.69 | −4.44,−0.93 |
| Father of child present | −0.48 | −1.16,0.19 | −0.19 | −0.43,0.06 | −0.36 | −0.66,−0.07 | −0.70 | −1.29,−0.10 | −0.66 | −2.45,1.13 |
| HIV serostatus | ||||||||||
| HIV-negative | Ref | Ref | Ref | Ref | Ref | |||||
| Unknown | 0.89 | −0.82,2.60 | −0.06 | −0.75,0.63 | 0.05 | −0.73,0.82 | 0.66 | −0.96,2.27 | 1.17 | −3.86,6.20 |
| HIV-positive | 0.54 | −0.20,1.28 | 0.21 | −0.06,0.48 | 0.23 | −0.11,0.57 | 0.33 | −0.31,0.97 | 1.11 | −2.35,4.57 |
| AUDIT-C score (per point) | 0.12 | −0.04,0.29 | 0.05 | −0.01,0.11 | 0.09 | −0.00,0.18 | 0.12 | −0.07,0.31 | 0.24 | −0.20,0.68 |
| Monthly household income | ||||||||||
| 0-499 ZAR | Ref | Ref | Ref | Ref | Ref | |||||
| 500-1000 ZAR | 0.05 | −1.58,1.68 | 0.12 | −0.66,0.89 | 0.03 | −0.79,0.86 | −0.70 | −3.52,2.11 | 3.19 | −6.83,13.20 |
| 1001-2000 ZAR | −0.65 | −2.18,0.88 | 0.03 | −0.66,0.71 | −0.37 | −1.14,0.39 | −0.81 | −3.52,1.91 | 0.24 | −10.97,11.44 |
| 2001-5000 ZAR | −1.03 | −2.57,0.50 | −0.26 | −0.93,0.40 | −0.70 | −1.45,0.06 | −1.02 | −3.73,1.69 | −1.56 | −12.95,9.82 |
| 5001-8000 ZAR | −1.64 | −3.37,0.08 | −0.14 | −0.86,0.57 | −0.79 | −1.60,0.03 | −1.54 | −4.24,1.15 | −2.97 | −14.13,8.18 |
| ≥8000 ZAR | −2.17 | −4.13,−0.20 | −0.32 | −1.10,0.46 | −1.08 | −1.97,−0.20 | −1.83 | −4.62,0.95 | −2.76 | −14.24,8.72 |
| Self-reported diabetes | 2.32 | −0.57,5.22 | 0.09 | −1.02,1.20 | 1.45 | −0.89,3.79 | 2.52 | −1.57,6.60 | 1.19 | −18.90,21.28 |
| Self-reported hypertension | 1.06 | −0.15,2.27 | 0.24 | −0.16,0.65 | 0.42 | −0.14,0.99 | 0.83 | −0.06,1.72 | 3.76 | −1.81,9.33 |
AUDIT-C, three-item consumption subset of the Alcohol Use Disorders Identification Test; ZAR, South African Rand
The first column displays the results from the conditional mean regression. Q20, Q40, Q60, and Q80 denote quantile regression estimates at the respective percentiles of the conditional distribution of the Edinburgh Postnatal Depression Scale (EPDS).
The findings were also consistent with the buffering hypothesis. When added to the regression models, both types of social support had statistically significant main effects, but instrumental support had a statistically significant interaction with food insufficiency (P=0.009) while emotional support did not (P=0.22). In stratified analyses, food insufficiency did not have a statistically significant association with depression symptom severity among women with a level of instrumental support greater than the median (β=0.12; 95% CI, −0.35 to 0.59) but did have a statistically significant association with depression among women with lower levels of support (β=0.79; 95% CI, 0.51-1.07).
In the fixed-effects specification adjusting for all time-invariant confounding, the estimated association between food insufficiency and depression symptom severity remained statistically significant (β=0.94; 95% CI, 0.67-1.22) (Table 2, column 1). A one-day increase (from one time point to the next) in the number of days of hunger was associated with a nearly one-point increase in the EPDS over the same time period. The fixed-effects quantile regression estimates again confirmed that the impacts of food insufficiency were greater among the most severely depressed women, with a nearly threefold difference in magnitudes between the lowest and highest quintile (Table 2, columns 2-5).
Table 2. Association between changes in depression symptom severity and changes in food insufficiency.
| Mean | Q20 | Q40 | Q60 | Q80 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||
| Predictor | β | 95% CI | β | 95% CI | β | 95% CI | β | 95% CI | β | 95% CI |
| Food insufficient in past week (per day) |
0.94 | 0.67,1.22 | 0.59 | 0.39,0.80 | 0.7 | 0.55,0.86 | 0.97 | 0.82,1.11 | 1.68 | 1.45,1.91 |
| Time point | ||||||||||
| Baseline | Ref | Ref | Ref | Ref | Ref | |||||
| 6 months | −3.27 | −3.86,−2.67 | −3.31 | −3.96,−2.66 | −3.61 | −4.13,−3.09 | −3.97 | −4.52,−3.42 | −4.42 | −5.24,−3.61 |
| 18 months | −3.95 | −4.56,−3.33 | −3.93 | −4.62,−3.24 | −4.18 | −4.77,−3.60 | −4.35 | −4.91,−3.79 | −5.16 | −5.94,−4.39 |
| 36 months | −4.11 | −4.78,−3.43 | −4.21 | −4.94,−3.49 | −4.47 | −4.98,−3.96 | −4.79 | −5.36,−4.21 | −5.01 | −5.99,−4.04 |
| Employed | 0.11 | −0.68,0.89 | 0.43 | −0.21,1.08 | 0.32 | −0.06,0.69 | 0.04 | −0.29,0.37 | 0.00 | −0.66,0.66 |
| Father of child present | −0.66 | −1.53,0.21 | −0.41 | −0.94,0.12 | −0.31 | −0.60,−0.02 | −0.7 | −0.94,−0.45 | −0.97 | −1.47,−0.46 |
| HIV serostatus | ||||||||||
| HIV-negative | Ref | Ref | Ref | Ref | Ref | |||||
| Unknown | −0.41 | −1.96,1.14 | 0.4 | −1.86,2.67 | 0.08 | −0.91,1.08 | −0.52 | −1.32,0.27 | −1.17 | −2.88,0.55 |
| HIV-positive | 0.08 | −1.41,1.58 | −0.34 | −0.93,0.24 | −0.21 | −0.56,0.13 | 0.28 | 0.01,0.55 | 0.82 | 0.16,1.47 |
| AUDIT-C score (per point) | 0.23 | 0.07,0.40 | 0.09 | −0.02,0.20 | 0.16 | 0.07,0.26 | 0.25 | 0.16,0.33 | 0.36 | 0.22,0.49 |
| Monthly household income | ||||||||||
| 0-499 ZAR | Ref | Ref | Ref | Ref | Ref | |||||
| 500-1000 ZAR | −1.25 | −2.62,0.12 | −1.49 | −2.78,−0.20 | −1.37 | −2.24,−0.50 | −0.83 | −1.89,0.22 | −0.31 | −2.00,1.37 |
| 1001-2000 ZAR | −1.75 | −3.04,−0.46 | −1.96 | −3.15,−0.77 | −1.94 | −2.72,−1.16 | −1.47 | −2.31,−0.63 | −1.31 | −2.91,0.29 |
| 2001-5000 ZAR | −1.93 | −3.21,−0.65 | −1.89 | −3.01,−0.76 | −2.13 | −2.86,−1.39 | −1.83 | −2.64,−1.01 | −1.47 | −2.97,0.03 |
| 5001-8000 ZAR | −2.08 | −3.62,−0.54 | −1.6 | −2.94,−0.26 | −1.97 | −2.80,−1.14 | −1.89 | −2.80,−0.97 | −1.77 | −3.38,−0.15 |
| ≥8000 ZAR | −2.36 | −4.15,−0.57 | −1.81 | −3.29,−0.33 | −2.33 | −3.37,−1.28 | −2.07 | −3.03,−1.12 | −2.05 | −4.01,−0.09 |
| Self-reported diabetes | −1.85 | −4.50,0.80 | −2.23 | −4.51,0.05 | −0.75 | −1.83,0.34 | −0.91 | −2.07,0.25 | −1.16 | −2.82,0.50 |
| Self-reported hypertension | 0.83 | −0.28,1.94 | 0.15 | −0.84,1.13 | 0.71 | 0.12,1.29 | 0.69 | 0.09,1.28 | 1.75 | 0.56,2.94 |
AUDIT-C, three-item consumption subset of the Alcohol Use Disorders Identification Test; ZAR, South African Rand
The first column displays the results from the conditional mean (fixed-effects) regression. Q20, Q40, Q60, and Q80 denote fixed-effects quantile regression estimates at the respective percentiles of the conditional distribution of the Edinburgh Postnatal Depression Scale (EPDS).
DISCUSSION
In this secondary analysis of data from a population-based, randomized controlled trial of 1,238 pregnant women near Cape Town, South Africa followed from pregnancy to 36 months post-delivery, we found that food insufficiency had a statistically significant association with depression symptom severity, particularly among the most severely depressed women. The pattern of associations was consistent with our conceptual model of how social support that is most appropriately matched to a particular stressor can provide a buffer against its adverse mental health impacts. Our findings are also consistent with what has been observed in smaller longitudinal studies conducted with more specialized samples, such as 456 persons with HIV in Uganda followed for less than 2 years (Tsai et al., 2012) and 110 community health volunteers in Ethiopia followed for less than 1 year (Maes, Hadley, Tesfaye, & Shifferaw, 2010). In terms of the estimated magnitudes of the associations, the experience of two days of hunger in the past week had an effect on mean EPDS scores that was comparable (in the opposite direction) to the treatment effects observed in short-term randomized-controlled trials of psychotherapy interventions for peripartum depression (Mulcahy, Reay, Wilkinson, & Owen, 2010; Spinelli & Endicott, 2003). Thus, our findings are not only statistically significant but also substantive in magnitude. Taken together, our findings have important policy and programmatic implications for women’s health in sub-Saharan Africa.
Methodologically, our study makes two unique contributions to the literature. First, few studies have employed fixed-effects regression to adjust for unobserved time-invariant confounding, including three studies in the U.S. (Heflin, Siefert, & Williams, 2005; Kim & Frongillo, 2007; Palar et al., 2015) and one study in rural Uganda (Tsai et al., 2012). We are unable to directly compare the relative magnitudes of the estimates, but our findings are broadly consistent with theirs. The second methodological contribution of our study is that we used quantile regression, and fixed-effects quantile regression, to demonstrate strong evidence of heterogeneous associations between food insufficiency and depression symptom severity. Namely, food insufficiency appeared to shift the upper quantiles of the conditional depression distribution by a much larger degree than the lower quantiles. Thus, even in this highly vulnerable sample of low-income pregnant and postpartum women, there appear to be pockets of even more concentrated adversity. A key implication is that interventions addressing food insufficiency may function to compress the distribution of depression, reducing the top of the depression distribution (i.e., the most disadvantaged) more than the bottom.
Social support was found to be an effect modifier of the relationship between food insufficiency and depression symptom severity, consistent with the “buffering” hypothesis (Cassel, 1976; Cobb, 1976). Specifically, our analyses showed that food insufficiency compromised mental health among women with low levels of social support, while women with high levels of social support appeared to be more resilient. A similar finding has been described in two other studies, including a population-based, cross-sectional study from Canada (Wu & Schimmele, 2005) and a longitudinal study of persons with HIV in rural Uganda (Tsai et al., 2012). In addition, consistent with the “matching” hypothesis (Cohen & McKay, 1984; Cohen & Wills, 1985), we found that instrumental support provided buffering against the adverse impacts of food insufficiency while emotional support did not.
Limitations
Interpretation of our findings is subject to several limitations. First, while the EPDS is a reliable, sensitive, and valid instrument for assessing depression symptom severity (Tsai et al., 2013), it was intended for use as a screening instrument and not as a definitive diagnosis (Kagee, Tsai, Lund, & Tomlinson, 2013). Notably, the EPDS does not provide information about whether participants met formal diagnostic criteria for major depressive disorder (with or without peripartum onset). Nonetheless, even sub-syndromal symptoms of depression are associated with significant psychosocial impairment and are therefore of public health interest (Judd et al., 1998). Second, pregnancy and postpartum can be uniquely vulnerable time periods for women, both in terms of food insecurity (Laraia, Vinikoor-Imler, & Siega-Riz, 2015) and depression (Sawyer, Ayers, & Smith, 2010), so our findings may not generalize beyond this population. On the other hand, the study sample represented nearly all (98%) pregnant women in the population. This population-based design is a significant strength of this study compared with the only other study of food insecurity and depression from sub-Saharan Africa to employ a similarly rigorous analytic approach (Tsai et al., 2012).
Third, our primary explanatory variable consisted of a single item measuring food insufficiency. The broader construct of food insecurity also includes nutritional inadequacy, cultural unacceptability, and uncertainty about food supply (Anderson, 1990; Coates, 2013). Inability to obtain foods of acceptable nutritional quality may be particularly stressful, especially for women experiencing comorbid health risks such as diabetes (Mendenhall & Norris, 2015). However, our ancillary analyses provide strong evidence of the construct validity of our single-item measure in relation to the HFIAS (which is reliable and valid, and is one of the most widely used measures of food insecurity (Hadley & Crooks, 2012)), thereby suggesting its adequacy for the empirical task at hand.
Fourth, most studies in the field have used a latency period of 3-6 months for evaluating subsequent changes in mental health in response to a life stressor, whether due to insufficiency of food, medical illness, or some other circumstance (Hammen, 2005; Palar et al., 2015; Tsai et al., 2012). In contrast, our study had an average latency period of 12 months, which could lead some to potentially argue that the lag between exposure and outcome exceeds a reasonable latency period of response. However, in many studies in this literature, extended latency periods are not uncommon and may extend from 12 months (Heflin, Siefert, & Williams, 2005) to two years or even more (Polsky et al., 2005; Rees et al., 2014). In ancillary analyses we did not find a statistically significant interaction between food insufficiency and assessment time (P=0.78), but the lagged association between food insufficiency and depression symptom severity did weaken in both magnitude and statistical significance with greater lag times: The association between food insufficiency at baseline and depression symptom severity at 6 months was β=0.78 (t=4.05); between food insufficiency at 6 months and depression symptom severity at 18 months, β=0.71 (t=3.60); and between food insufficiency at 18 months and depression symptom severity at 36 months, β=0.59 (t=2.88).
Fifth, while study participants (“large N”) were followed over a 36-month period, there were only four data collection time points (“small T”). The two-step estimator proposed by Canay (2011) is consistent and asymptotically normal only when both N and T go to infinity. Given any fixed N, a smaller T implies a larger finite sample bias for our fixed-effects quantile regression estimates. However, the simulation analyses Canay (2011) provided also indicate good coverage of the asymptotic confidence interval even in the setting of small T.
Conclusions
These limitations notwithstanding, our findings have substantial programmatic implications for population mental health generally, and for South Africa specifically, where more than a quarter of households may be food insecure (Sorsdahl et al., 2011) and where postpartum depression is highly prevalent (Hartley et al., 2011; Tsai & Tomlinson, 2012). Given the inequitable distribution of human resources for mental health in countries like South Africa (Saxena, Thornicroft, Knapp, & Whiteford, 2007), existing programs and policies should target potentially modifiable risk factors for poor mental health outcomes. For example, nutrition support programs could be integrated into existing antepartum and postpartum care programs, similar to the ways in which HIV care and treatment programs have been explored as potential vehicles for the delivery of food aid to persons with HIV (Cantrell et al., 2008; Mamlin et al., 2009; Rawat, Faust, Maluccio, & Kadiyala, 2014; Yager, Kadiyala, & Weiser, 2011). If such resources cannot be mobilized to directly address primary insults to mental health, then social support interventions, delivered through community-based outreach, could potentially be used to support the resilience of women in withstanding these and other life stressors. Our findings suggest that instrumental support interventions, rather than emotional support interventions, would be most suited to this purpose. A classical example of an emotional support intervention might include the counseling intervention employed in the Enhancing Recovery in Coronary Heart Disease (ENRICHD) study, which was designed to modify participants’ behavioral and social skill deficits, cognitive factors contributing to the perception of unsatisfying relationships, and social outreach and network development (ENRICHD Investigators, 2001). Instrumental support interventions, in contrast, would focus on meeting participants’ tangible needs, either through social protection schemes offering direct assistance (Goudge et al., 2009) or livelihood training (Weiser et al., 2015), or through counseling directed specifically at helping participants mobilize their social networks (Perry & Pescosolido, 2015) toward instrumental ends. As noted by Kawachi (1999), “Even apparently trivial differences in the willingness of neighbors to help each other (e.g., through cash loans or labor in kind) might conceivably affect the health of individuals living in deprived communities” (p. 121).
In summary, we provide novel, population-based evidence from a longitudinal study describing an important association between food insufficiency and depression symptom severity among more than 1,200 pregnant women in economically deprived settlements surrounding Cape Town, South Africa. The estimated associations are large in magnitude and even larger for the most severely depressed women, although women with high levels of social support appear to be resilient to the adverse mental health impacts. Interventions aimed at improving food security and/or social support for new mothers in resource-limited settings are likely to benefit their health and mental health and may also benefit their children as well.
Supplementary Material
HIGHLIGHTS.
Food insufficiency is an important, modifiable risk factor for depression
We investigate this association using longitudinal data from South Africa
Food insufficiency has a strong association with depressive symptoms
The estimates are robust to fixed effects and quantile specifications
Acknowledgments
The authors thank Kate Desmond, Erin Greco, Mary Hartley, Faith Idemundia, Ingrid Le Roux, Karl Le Roux, Nokwanele Mbewu, Mary J. O’Connor, Jacqueline Stewart, Dallas Swendeman, Robert E. Weiss, and Carol M. Worthman for their contributions to study conception, study design, data collection, and implementation; and Aaron W. Scheffler, for his contributions to data management and analysis.
Funding: This study was funded by U.S. National Institutes of Health (NIH) R01AA017104 and supported by R24AA022919, P30MH058107 (Center for HIV Identification, Prevention, and Treatment Services), P30AI028697 (UCLA Center for AIDS Research), and UL1TR000124 (National Center for Advancing Translational Science through the UCLA Clinical and Translational Science Institute). The authors also acknowledge salary support through K23MH096620 (ACT) and the National Research Foundation of South Africa (MT).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Anderson SA. Core indicators of nutritional state for difficult-to-sample populations. Journal of Nutrition. 1990;120(11):1559–1600. doi: 10.1093/jn/120.suppl_11.1555. [DOI] [PubMed] [Google Scholar]
- Bartus T. Estimation of marginal effects using margeff. Stata J. 2005;5(3):309–329. [Google Scholar]
- Briefel RR, Woteki CE. Development of food sufficiency questions for the third national health and nutrition examination survey. Journal of Nutrition Education. 1992;24(1 Suppl 1):24S–28S. [Google Scholar]
- Canay IA. A simple approach to quantile regression for panel data. Economet J. 2011;14(3):368–386. [Google Scholar]
- Cantrell RA, Sinkala M, Megazinni K, Lawson-Marriott S, Washington S, Chi BH, Stringer JS. A pilot study of food supplementation to improve adherence to antiretroviral therapy among food-insecure adults in Lusaka, Zambia. 2008;49(2):190–195. doi: 10.1097/QAI.0b013e31818455d2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassel J. The contribution of the social environment to host resistance: the Fourth Wade Hampton Frost Lecture. American Journal of Epidemiology. 1976;104(2):107–123. doi: 10.1093/oxfordjournals.aje.a112281. [DOI] [PubMed] [Google Scholar]
- Coates J. Build it back better: deconstructing food security measurement and action. Glob Food Sec. 2013;2(3):188–194. [Google Scholar]
- Coates J, Frongillo EA, Rogers BL, Webb P, Wilde PE, Houser R. Commonalities in the experience of household food insecurity across cultures: what are measures missing? Journal of Nutrition. 2006;136(5):1438S–1448S. doi: 10.1093/jn/136.5.1438S. [DOI] [PubMed] [Google Scholar]
- Cobb S. Presidential Address-1976. Social support as a moderator of life stress. Psychosomatic Medicine. 1976;38(5):300–314. doi: 10.1097/00006842-197609000-00003. [DOI] [PubMed] [Google Scholar]
- Cohen S, McKay G. Social support, stress and the buffering hypothesis: a theoretical analysis. In: Baum A, Taylor SE, Singer JE, editors. Handbook of psychology and health. Lawrence Erlbaum Associates, Inc.; Hillsdale: 1984. pp. 253–267. [Google Scholar]
- Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychological Bulletin. 1985;98(2):310–357. [PubMed] [Google Scholar]
- Cole SM, Tembo G. The effect of food insecurity on mental health: panel evidence from rural Zambia. Social Science and Medicine. 2011;73(7):1071–1079. doi: 10.1016/j.socscimed.2011.07.012. [DOI] [PubMed] [Google Scholar]
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. British Journal of Psychiatry. 1987;150(6):782–786. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- De Bruin GP, Swartz L, Tomlinson M, Cooper PJ, Molteno C. The factor structure of the Edinburgh Postnatal Depression scale in a South African peri-urban settlement. South African Journal of Psychology. 2004;34(1):113–121. [Google Scholar]
- Dewing S, Tomlinson M, le Roux IM, Chopra M, Tsai AC. Food insecurity and its association with co-occurring postnatal depression, hazardous drinking, and suicidality among women in peri-urban South Africa. Journal of Affective Disorders. 2013;150(2):460–465. doi: 10.1016/j.jad.2013.04.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ENRICHD Investigators Enhancing Recovery in Coronary Heart Disease (ENRICHD) study intervention: rationale and design. Psychosomatic Medicine. 2001;63(5):747–755. [PubMed] [Google Scholar]
- Epstein S. Coping ability, negative self-evaluation, and overgeneralization: experiment and theory. Journal of Personality and Social Psychology. 1992;62(5):826–836. doi: 10.1037//0022-3514.62.5.826. [DOI] [PubMed] [Google Scholar]
- Ettner SL, Frank RG, Kessler RC. The impact of psychiatric disorders on labor market outcomes. 1997;51(1):64–81. [Google Scholar]
- Farmer P. Infections and inequalities: the modern plagues. University of California Press; Berkeley: 1999. [Google Scholar]
- Filmer D, Pritchett LH. Estimating wealth effects without expenditure data -- or tears: an application to educational enrollments in states of India. Demography. 2001;38(1):115–132. doi: 10.1353/dem.2001.0003. [DOI] [PubMed] [Google Scholar]
- Fisher J, Cabral de Mello M, Patel V, Rahman A, Tran T, Holton S, Holmes W. Prevalence and determinants of common perinatal mental disorders in women in low- and lower-middle-income countries: a systematic review. Bulletin of the World Health Organization. 2012;90(2):139G–149G. doi: 10.2471/BLT.11.091850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Froot KA. Consistent covariance matrix estimation with cross-sectional dependence and heteroskedasticity in financial data. Journal of Financial and Quantitative Analysis. 1989;24(3):333–355. [Google Scholar]
- Goudge J, Russell S, Gilson L, Gumede T, Tollman S, Mills A. Illness-related impoverishment in rural South Africa: why does social protection work for some households but not others? J Int Dev. 2009;21(2):231–251. [Google Scholar]
- Hadley C, Crooks DL. Coping and the biosocial consequences of food insecurity in the 21st century. American Journal of Physical Anthropology. 2012;149(Suppl 55):72–94. doi: 10.1002/ajpa.22161. [DOI] [PubMed] [Google Scholar]
- Hadley C, Patil CL. Seasonal changes in household food insecurity and symptoms of anxiety and depression. 2008;135(2):225–232. doi: 10.1002/ajpa.20724. [DOI] [PubMed] [Google Scholar]
- Hamelin AM, Beaudry M, Habicht JP. Characterization of household food insecurity in Quebec: food and feelings. Social Science and Medicine. 2002;54(1):119–132. doi: 10.1016/s0277-9536(01)00013-2. [DOI] [PubMed] [Google Scholar]
- Hammen C. Stress and depression. Annual Review of Clinical Psychology. 2005;1(1):293–319. doi: 10.1146/annurev.clinpsy.1.102803.143938. [DOI] [PubMed] [Google Scholar]
- Hartley M, Tomlinson M, Greco E, Comulada WS, Stewart J, le Roux I, Rotheram-Borus MJ. Depressed mood in pregnancy: prevalence and correlates in two Cape Town peri-urban settlements. Reproductive Health. 2011;8:9. doi: 10.1186/1742-4755-8-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heflin CM, Siefert K, Williams DR. Food insufficiency and women’s mental health: findings from a 3-year panel of welfare recipients. Social Science and Medicine. 2005;61(9):1971–1982. doi: 10.1016/j.socscimed.2005.04.014. [DOI] [PubMed] [Google Scholar]
- Hung KJ, Tomlinson M, le Roux IM, Dewing S, Chopra M, Tsai AC. Community-based prenatal screening for postpartum depression in a South African township. International Journal of Gynaecology and Obstetrics. 2014;126(1):74–77. doi: 10.1016/j.ijgo.2014.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyder AA, Maman S, Nyoni JE, Khasiani SA, Teoh N, Premji Z, Sohani S. The pervasive triad of food security, gender inequity and women’s health: exploratory research from sub-Saharan Africa. 2005;5(4):328–334. doi: 10.5555/afhs.2005.5.4.328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Judd LL, Akiskal HS, Maser JD, Zeller PJ, Endicott J, Coryell W, Keller MB. A prospective 12-year study of subsyndromal and syndromal depressive symptoms in unipolar major depressive disorders. Archives of General Psychiatry. 1998;55(8):694–700. doi: 10.1001/archpsyc.55.8.694. [DOI] [PubMed] [Google Scholar]
- Kagee A, Tsai AC, Lund C, Tomlinson M. Screening for common mental disorders: reasons for caution and a way forward. International Health. 2013;5(1):11–14. doi: 10.1093/inthealth/ihs004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi I. Social capital and community effects on population and individual health. 1999;896:120–130. doi: 10.1111/j.1749-6632.1999.tb08110.x. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Price RH, Wortman CB. Social factors in psychopathology: stress, social support, and coping processes. Annual Review of Psychology. 1985;36:531–572. doi: 10.1146/annurev.ps.36.020185.002531. [DOI] [PubMed] [Google Scholar]
- Kim K, Frongillo EA. Participation in food assistance programs modifies the relation of food insecurity with weight and depression in elders. Journal of Nutrition. 2007;137(4):1005–1010. doi: 10.1093/jn/137.4.1005. [DOI] [PubMed] [Google Scholar]
- Kling JR, Liebman JB, Katz LF. Experimental analysis of neighborhood effects. Econometrica. 2007;75(1):83–119. [Google Scholar]
- Koenker R, Bassett G. Regression quantiles. Econometrica. 1978;46(1):33–50. [Google Scholar]
- Krieger N. Theories for social epidemiology in the 21st century: an ecosocial perspective. 2001;30(4):668–677. doi: 10.1093/ije/30.4.668. [DOI] [PubMed] [Google Scholar]
- Laraia B, Vinikoor-Imler LC, Siega-Riz AM. Food insecurity during pregnancy leads to stress, disordered eating, and greater postpartum weight among overweight women. Obesity (Silver Spring) 2015;23(6):1303–1311. doi: 10.1002/oby.21075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- le Roux IM, Rotheram-Borus MJ, Stein J, Tomlinson M. The impact of paraprofessional home visitors on infants’ growth and health at 18 months. Vulnerable Child Youth Stud. 2014;9(4):291–304. doi: 10.1080/17450128.2014.940413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- le Roux IM, Tomlinson M, Harwood JM, O’Connor MJ, Worthman CM, Mbewu N, Rotheram-Borus MJ. Outcomes of home visits for pregnant township mothers and their infants in South Africa: a cluster randomised controlled trial. AIDS. 2013;27(9):1461–1471. doi: 10.1097/QAD.0b013e3283601b53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lund C, Breen A, Flisher AJ, Kakuma R, Corrigall J, Joska JA, Patel V. Poverty and common mental disorders in low and middle income countries: A systematic review. Social Science and Medicine. 2010;71(3):517–528. doi: 10.1016/j.socscimed.2010.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maes KC, Hadley C, Tesfaye F, Shifferaw S. Food insecurity and mental health: Surprising trends among community health volunteers in Addis Ababa, Ethiopia during the 2008 food crisis. Social Science and Medicine. 2010;70(9):1450–1457. doi: 10.1016/j.socscimed.2010.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mamlin J, Kimaiyo S, Lewis S, Tadayo H, Jerop FK, Gichunge C, Einterz R. Integrating nutrition support for food-insecure patients and their dependents into an HIV care and treatment program in Western Kenya. 2009;99(2):215–221. doi: 10.2105/AJPH.2008.137174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendenhall E. Syndemic suffering in Soweto: violence and inequality at the nexus of health transition in South Africa. Ann Anthropol Pract. 2015;38(2):300–316. [Google Scholar]
- Mendenhall E, Norris SA. When HIV is ordinary and diabetes new: Remaking suffering in a South African Township. Global Public Health. 2015;10(4):449–462. doi: 10.1080/17441692.2014.998698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller KE, Rasmussen A. War exposure, daily stressors, and mental health in conflict and post-conflict settings: bridging the divide between trauma-focused and psychosocial frameworks. 2010;70(1):7–16. doi: 10.1016/j.socscimed.2009.09.029. [DOI] [PubMed] [Google Scholar]
- Mulcahy R, Reay RE, Wilkinson RB, Owen C. A randomised control trial for the effectiveness of group Interpersonal Psychotherapy for postnatal depression. Arch Womens Ment Health. 2010;13(2):125–139. doi: 10.1007/s00737-009-0101-6. [DOI] [PubMed] [Google Scholar]
- Mundlak Y. Empirical production function free of management bias. J Farm Econ. 1961;43(1):44–56. [Google Scholar]
- Nordanger D. Discourses of loss and bereavement in Tigray, Ethiopia. Culture, Medicine and Psychiatry. 2007;31(2):173–194. doi: 10.1007/s11013-007-9050-6. [DOI] [PubMed] [Google Scholar]
- O’Connor MJ, Tomlinson M, Leroux IM, Stewart J, Greco E, Rotheram-Borus MJ. Predictors of alcohol use prior to pregnancy recognition among township women in Cape Town, South Africa. Social Science and Medicine. 2011;72(1):83–90. doi: 10.1016/j.socscimed.2010.09.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palar K, Kushel M, Frongillo EA, Riley ED, Grede N, Bangsberg D, Weiser SD. Food insecurity is longitudinally associated with depressive symptoms among homeless and marginally-housed individuals living with HIV. AIDS and Behavior. 2015;19(8):1527–1534. doi: 10.1007/s10461-014-0922-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parente PMDC, Santos Silva JMC. Quantile regression with clustered data. Journal of Econometric Methods. 2015 in press. Epub 27 Feb 2015. [Google Scholar]
- Pearlin LI. The sociological study of stress. Journal of Health and Social Behavior. 1989;30(3):241–256. [PubMed] [Google Scholar]
- Pearlin LI. The stress process revisited: reflections on concepts and their interrelationships. In: Aneshensel CS, Phelan JC, editors. Handbook of the sociology of mental health. Springer; New York: 1999. pp. 395–416. [Google Scholar]
- Pearlin LI, Lieberman MA, Menaghan EG, Mullan JT. The stress process. Journal of Health and Social Behavior. 1981;22(4):337–356. [PubMed] [Google Scholar]
- Perry BL, Pescosolido BA. Social network activation: the role of health discussion partners in recovery from mental illness. Social Science and Medicine. 2015;125:116–128. doi: 10.1016/j.socscimed.2013.12.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perry CD. Does treating maternal depression improve child health management? The case of pediatric asthma. Journal of Health Economics. 2008;27(1):157–173. doi: 10.1016/j.jhealeco.2007.03.005. [DOI] [PubMed] [Google Scholar]
- Pike IL, Patil CL. Understanding women’s burdens: preliminary findings on psychosocial health among Datoga and Iraqw women of northern Tanzania. Culture, Medicine and Psychiatry. 2006;30(3):299–330. doi: 10.1007/s11013-006-9022-2. [DOI] [PubMed] [Google Scholar]
- Pitpitan EV, Kalichman SC, Eaton LA, Cain D, Sikkema KJ, Watt MH, Pieterse D. Co-occurring psychosocial problems and HIV risk among women attending drinking venues in a South African township: a syndemic approach. Annals of Behavioral Medicine. 2013;45(2):153–162. doi: 10.1007/s12160-012-9420-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polsky D, Doshi JA, Marcus S, Oslin D, Rothbard A, Thomas N, Thompson CL. Long-term risk for depressive symptoms after a medical diagnosis. Archives of Internal Medicine. 2005;165(11):1260–1266. doi: 10.1001/archinte.165.11.1260. [DOI] [PubMed] [Google Scholar]
- Power MJ, Champion LA, Aris SJ. The development of a measure of social support: the Significant Others (SOS) Scale. British Journal of Clinical Psychology. 1988;27(Pt 4):349–358. doi: 10.1111/j.2044-8260.1988.tb00799.x. [DOI] [PubMed] [Google Scholar]
- Quisumbing AR, Brown L, Feldstein H, Haddad L, Pena C. Women: the key to food security. International Food Policy Research Institute; Washington, D.C.: 1995. [Google Scholar]
- Rahman A, Iqbal Z, Bunn J, Lovel H, Harrington R. Impact of maternal depression on infant nutritional status and illness: a cohort study. Archives of General Psychiatry. 2004;61(9):946–952. doi: 10.1001/archpsyc.61.9.946. [DOI] [PubMed] [Google Scholar]
- Rawat R, Faust E, Maluccio JA, Kadiyala S. The impact of a food assistance program on nutritional status, disease progression, and food security among people living with HIV in Uganda. Journal of Acquired Immune Deficiency Syndromes. 2014;66(1):e15–22. doi: 10.1097/QAI.0000000000000079. [DOI] [PubMed] [Google Scholar]
- Rees S, Steel Z, Creamer M, Teesson M, Bryant R, McFarlane AC, Silove D. Onset of common mental disorders and suicidal behavior following women’s first exposure to gender based violence: a retrospective, population-based study. BMC Psychiatry. 2014;14:312. doi: 10.1186/s12888-014-0312-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rochat TJ, Richter LM, Doll HA, Buthelezi NP, Tomkins A, Stein A. Depression among pregnant rural South African women undergoing HIV testing. Journal of the American Medical Association. 2006;295(12):1376–1378. doi: 10.1001/jama.295.12.1376. [DOI] [PubMed] [Google Scholar]
- Rogers WH. Regression standard errors in clustered samples. Stata Tech Bull. 1993;13:19–23. [Google Scholar]
- Rotheram-Borus MJ, le Roux IM, Tomlinson M, Mbewu N, Comulada WS, le Roux K, Swendeman D. Philani Plus (+): a Mentor Mother community health worker home visiting program to improve maternal and infants’ outcomes. Prevention Science. 2011;12(4):372–388. doi: 10.1007/s11121-011-0238-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Tomlinson M, le Roux IM, Harwood JM, Comulada S, O’Connor MJ, Worthman CM. A cluster randomised controlled effectiveness trial evaluating perinatal home visiting among South African mothers/infants. Public Library of Science One. 2014;9(10):e105934. doi: 10.1371/journal.pone.0105934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Tomlinson M, Roux IL, Stein JA. Alcohol use, partner violence, and depression: a cluster randomized controlled trial among urban South African mothers over 3 years. American Journal of Preventive Medicine. 2015;49(5):715–725. doi: 10.1016/j.amepre.2015.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption--II. Addiction. 1993;88(6):791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Sawyer A, Ayers S, Smith H. Pre- and postnatal psychological wellbeing in Africa: a systematic review. Journal of Affective Disorders. 2010;123(1-3):17–29. doi: 10.1016/j.jad.2009.06.027. [DOI] [PubMed] [Google Scholar]
- Saxena S, Thornicroft G, Knapp M, Whiteford H. Resources for mental health: scarcity, inequity, and inefficiency. Lancet. 2007;370(9590):878–889. doi: 10.1016/S0140-6736(07)61239-2. [DOI] [PubMed] [Google Scholar]
- Singer M. AIDS and the health crisis of the U.S. urban poor; the perspective of critical medical anthropology. Social Science and Medicine. 1994;39(7):931–948. doi: 10.1016/0277-9536(94)90205-4. [DOI] [PubMed] [Google Scholar]
- Sorsdahl K, Slopen N, Siefert K, Seedat S, Stein DJ, Williams DR. Household food insufficiency and mental health in South Africa. Journal of Epidemiology and Community Health. 2011;65(5):426–431. doi: 10.1136/jech.2009.091462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spinelli MG, Endicott J. Controlled clinical trial of interpersonal psychotherapy versus parenting education program for depressed pregnant women. American Journal of Psychiatry. 2003;160(3):555–562. doi: 10.1176/appi.ajp.160.3.555. [DOI] [PubMed] [Google Scholar]
- Tomlinson M, O’Connor MJ, le Roux IM, Stewart J, Mbewu N, Harwood J, Rotheram-Borus MJ. Multiple risk factors during pregnancy in South Africa: the need for a horizontal approach to perinatal care. Prev Sci. 2014;15(3):277–282. doi: 10.1007/s11121-013-0376-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai AC, Bangsberg DR, Frongillo EA, Hunt PW, Muzoora C, Martin JN, Weiser SD. Food insecurity, depression and the modifying role of social support among people living with HIV/AIDS in rural Uganda. Social Science and Medicine. 2012;74(12):2012–2019. doi: 10.1016/j.socscimed.2012.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai AC, Burns BFO. Syndemics of psychosocial problems and HIV risk: a systematic review of empirical tests of the disease interaction concept. Social Science and Medicine. 2015;139(1):26–35. doi: 10.1016/j.socscimed.2015.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai AC, Leiter K, Wolfe WR, Heisler M, Shannon K, Phaladze NA, Weiser SD. Prevalence and correlates of forced sex perpetration and victimization in Botswana and Swaziland. American Journal of Public Health. 2011;101(6):1068–1074. doi: 10.2105/AJPH.2010.300060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai AC, Scott JA, Hung KJ, Zhu JQ, Matthews LT, Psaros C, Tomlinson M. Reliability and validity of instruments for assessing perinatal depression in African settings: systematic review and meta-analysis. Public Library of Science One. 2013;8(12):e82521. doi: 10.1371/journal.pone.0082521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai AC, Tomlinson M. Mental health spillovers and the Millennium Development Goals: The case of perinatal depression in Khayelitsha, South Africa. Journal of Global Health. 2012;2(1):010302. doi: 10.7189/jogh.02.010302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai AC, Tomlinson M, Dewing S, le Roux IM, Harwood JM, Chopra M, Rotheram-Borus MJ. Antenatal depression case-finding by community health workers in South Africa: feasibility of a mobile phone application. Arch Womens Ment Health. 2014;17(5):423–431. doi: 10.1007/s00737-014-0426-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiser SD, Bukusi EA, Steinfeld RL, Frongillo EA, Weke E, Dworkin SL, Cohen CR. Shamba Maisha: randomized controlled trial of a multisectoral agricultural and finance intervention to improve nutrition and HIV health outcomes in Kenya. AIDS. 2015;29(14):1889–1894. doi: 10.1097/QAD.0000000000000781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiser SD, Leiter K, Bangsberg DR, Butler LM, Percy-de Korte F, Hlanze Z, Heisler M. Food insufficiency is associated with high-risk sexual behavior among women in Botswana and Swaziland. Public Library of Science Medicine. 2007;4(10):1589–1597. doi: 10.1371/journal.pmed.0040260. discussion 1598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, Vos T. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet. 2013;382(9904):1575–1586. doi: 10.1016/S0140-6736(13)61611-6. [DOI] [PubMed] [Google Scholar]
- Williams RL. A note on robust variance estimation for cluster-correlated data. Biometrics. 2000;56(2):645–646. doi: 10.1111/j.0006-341x.2000.00645.x. [DOI] [PubMed] [Google Scholar]
- Wu Z, Schimmele CM. Food insufficiency and depression. Sociol Persp. 2005;48(4):481–504. [Google Scholar]
- Yager JE, Kadiyala S, Weiser SD. HIV/AIDS, food supplementation and livelihood programs in Uganda: a way forward? PloS One. 2011;6(10):e26117. doi: 10.1371/journal.pone.0026117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yim IS, Tanner Stapleton LR, Guardino CM, Hahn-Holbrook J, Dunkel Schetter C. Biological and psychosocial predictors of postpartum depression: systematic review and call for integration. Annual Review of Clinical Psychology. 2015;11:99–137. doi: 10.1146/annurev-clinpsy-101414-020426. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.