Abstract
Objective
To examine if motivation to quit is associated with parental smoker’s perceived presence of a personal or child health illness or risk due to tobacco use.
Design/Methods
This was a cross-sectional study of a convenience sample of 218 parental smokers who presented to the pediatric emergency department with their child. We assessed factors related to motivation to quit, including personal and child smoking-related illness, perceived personal and child health risk, smoking behaviors, and demographic characteristics. Motivation to quit was measured using the Contemplation Ladder score.
Results
The mean score on the Contemplation Ladder was 6.2 (SD, 2.5), representing the response: thinking about cutting down or quitting. Eighty-four participants (39%) had high motivation to quit (Contemplation Ladder score 8). Bivariate analysis showed significant associations between high motivation to quit and perceived child health risk with continued smoking and perceived personal and child health benefit following smoking cessation. Parents with high motivation to quit were more likely to have high perceived self-efficacy and confidence in their ability to quit, prior quit attempts, and lower nicotine dependence. With the exception of race/ethnicity, demographic variables were not associated with motivation to quit.
Conclusions
A significant proportion of parental smokers who present to the pediatric emergency department endorse strong motivation to quit. Parents who endorse health risk or quitting-related health benefits in their child are more likely to have high motivation to quit smoking. Future studies are needed to determine if high motivation translates into smoking cessation.
Keywords: smoking cessation, parental smoker, motivation to quit, second hand smoke exposure
Tobacco use continues to be the most preventable cause of morbidity and mortality in the United States.1 Recently, the Institute of Medicine, the American College of Emergency Physicians, and the Public Health Service’s Clinical Practice Guideline Treating Tobacco Use and Dependence2 have stated that emergency departments (EDs) are an important venue in which to conduct cessation interventions.3,4 Tobacco screening and brief cessation interventions have been shown to be feasible in the ED setting and have the potential for resulting in a large public health impact.2,5–8 Adult smokers who visit the pediatric ED (PED) with their children have rates of smoking that exceed that of the general population,9–12 and their children are at increased risk of suffering from secondhand smoke exposure (SHSe)–related illnesses such as bronchiolitis, asthma, pneumonia, and ear infections.13,14 These parental smokers are concerned that their tobacco use may be harmful to their children, and they are interested in receiving cessation advice in the PED.11 However, the PED remains an underutilized and understudied venue in which to provide parental smoking interventions.15–19 If PED practitioners were to use each PED visit as a “teachable moment” to encourage and counsel parental smokers to quit, this may increase the parent’s subsequent quit attempts and may not only improve the health of the parent, but also improve the health of their child by decreasing SHSe-related visits and morbidity.
Motivation to quit smoking is a key factor in determining cessation success. Motivation predicts participation in smoking cessation treatment, attempts to quit,20,21 and successful cessation.21 Research indicates that when a child has an SHSe-related illness such as asthma, parents may have increased motivation to quit compared with parents whose child does not have an SHSe-related illness.22,23 A recent study of parental smokers who had a child with asthma demonstrated that parents who believed that their child’s asthma symptoms would decrease if they quit smoking or who felt that their child’s asthma was not under good control were more motivated to quit smoking.24 Similarly, smokers who believe that they have a personal tobacco-related diagnosis or who have concerns about the effects of smoking on their health have a stronger motivation to quit compared with those without such concerns.3,20,25,26 Furthermore, studies in the adult ED setting have indicated that adult patients who anticipate greater health improvement with smoking cessation and those with greater perceived self-efficacy to quit are more motivated to quit.26 Given the increasing demands on resources in the PED, it is important to identify which factors are associated with motivation to quit so that interventions can be targeted to those smokers who are likely to succeed in their quitting attempts. Simply asking a smoker whether he/she is interested in quitting does not discriminate well those who are prepared to quit smoking and may actually make a serious attempt, as most smokers will express interest in quitting.26–28
The primary aim of this study was to determine if parental motivation to quit smoking was related to their perception of their personal or child’s smoking-related health risk or illness. Our hypothesis was that parental smokers who perceived that they, or their child, had a smoking-related health risk or illness would be more likely to be motivated to quit compared with those who did not. Our secondary aim was to determine demographics and smoking behavior characteristics associated with motivation to quit among parental smokers.
METHODS
Study Design and Setting
This was a cross-sectional study of a convenience sample of parents/legal guardians who presented to the PED at Cincinnati Children’s Hospital Medical Center between January 2011 and May 2011. Cincinnati Children’s Hospital Medical Center is an inner-city, tertiary-care pediatric hospital with a PED that has an annual patient census of more than 100,000 visits.
Participants and Screening
All parents/legal guardians of children younger than 18 years triaged to the nonurgent or urgent category who reported current tobacco use were potentially eligible. Parents screened positive for current tobacco use if they answered “yes” to the following question: “Have you smoked at least 1 cigarette daily in the previous week?” Parents were not eligible if they were non–English speaking (because of lack of resources for translation of study materials) or if they had been previously enrolled. Parents who screened positive were given a study information sheet by the research assistant. The study was reviewed and approved by the Cincinnati Children’s Hospital Medical Center Institutional Review Board.
Assessments
To assess our primary outcome of motivation to quit smoking, we used the Contemplation Ladder,29 a 1-item, 11-point scale of motivation (0 = no thought of quitting to 10 = taking action to quit). The Contemplation Ladder is a validated score that correlates with the likelihood of making a quit attempt in the next 6 months and participation in activities associated with quit attempts. As used in prior research,24 high motivation to quit was defined by a Contemplation Ladder score of 8 or greater representing the response “have cut down and seriously considering quitting” and “ready to quit now.”
Parent demographics were collected including age, sex, race/ethnicity, education level, insurance type, and utilization of a primary care physician. We also assessed characteristics of parent’s smoking behavior, including current smoking status, smoking history, and prior quit attempts. To determine nicotine dependence, we used the Heavy Smoking Index (HSI), which is a validated, 2-item self-report measure of nicotine dependence derived from the Fagerstrom Test for Nicotine Dependence, a commonly used method to determine nicotine dependence in smokers. The 2 items on the HSI assess the number of cigarettes smoked per day and the time to first cigarette after waking in the morning. Each item is scored on a 1- to 4-point scale and then summed. The range of scores is 2 to 8, with higher scores indicating greater nicotine dependence. A cutoff score of 4 or greater is recommended to designate nicotine dependence.
To assess parent’s perception of their personal and their child’s smoking-related health risks, we used measures adapted from Wagener et al.30 These items were as follows: personal and child health risk, quitting and personal/child health improvement, and personal/child smoking-related illness (Table 1). Participants were also asked to rate their views on quitting using the Importance-Readiness-Confidence rulers, which had scales of 1 to 10 as shown in Table 1.31
TABLE 1.
Assessment Questions and Response Options
| Personal and child health risk: if you keep smoking, how likely is it do you feel that you/your child will develop a serious disease because of smoking? (Likert scale 1–7: no chance to 100% certain) |
| Quitting and personal/child health benefit: if you stopped smoking, how do you think you/your child’s current health would change? (Likert scale 1–6, not at all to completely better) |
| Personal/child smoking related illness: have you/your child ever had a serious health problem that you believe was caused or made worse by smoking? (Yes, no, don’t know) |
| Importance-Readiness-Confidence Rulers |
| Importance: how important is stopping smoking to you? (Scale 1–10, not at all important to most important goal of my life) |
| Readiness: how ready are you to quit smoking within the next month? (Scale 1–10, not at all ready to 100% ready) |
| Confidence: how confident are you that you could quit smoking within the next month and stay quit for good? (Scale 1–10, not at all confident to 100% confident) |
Study Proceedings
Eligible parental smokers who verbally consented to the study were asked by the research assistant to complete an electronic baseline questionnaire on a Web-enabled tablet study computer.
Sample Size Calculation
We estimated that we would need a total sample size of approximately 106 in each group in order to detect a 20-percentage-point difference in whether parents were motivated to quit smoking between parents who endorsed the presence of a personal smoking-related illness and increased health risk and parents who do not endorse such perceptions. Based on the existing literature in the adult ED, pediatric primary care, and hospital settings,18 we estimated that 55% of parental smokers who endorse the presence of a personal smoking-related illness would report that they are motivated to quit compared with 35% of parents who would not. We used these proportions as planning values and assumed a 2-sided significance level of 0.05 and a power of 80%. Although we could not estimate a priori how the sample would be distributed among the 2 comparison groups, a sensitivity analysis indicated that unequal sample sizes, such as a 70/30 split between the 2 groups would still result in a power greater than 70%.
Data Analysis
Descriptive statistics, frequencies, and cross-tabulations by level of motivation to quit smoking were developed to describe demographic characteristics, parent-reported smoking-related illnesses, health care utilization, and smoking-related variables. A bivariate analysis consisting of χ2 analyses for categorical variables and t tests for continuous and Likert scale variables was conducted to identify significant differences between parents with low and parents with high motivation to quit smoking. Logistic regression was used to determine the association between perceived parent and child health risks and parent motivation to quit smoking. Separate models were developed for each of the 4 measures of health risk. First, a bivariate logistic regression analysis was conducted in which the dichotomized motivation to quit measure was the dependent variable and the measure of perceived risk was the independent variable. Second, multivariable models were developed in order to control for the following parent characteristics: education, type of insurance, race, ethnicity, sex, prior quit attempts, HSI, and confidence in their ability to quit smoking. The nonparametric Wilcoxon rank sum test was used to conduct a matched paired analysis on attitudes about personal and child health effects. Finally, a multivariable model was developed to examine which demographic and smoking-related variables were independent predictors of motivation to quit. The predictors included in the model were sex, education, insurance type, ethnicity, race, HSI, no prior quit attempt, and confidence to quit. The software packages SAS (version 9.3, SAS Institute Inc, Cary, NC) and IBM SPSS (version 19, IBM, Chicago, IL) were used to conduct the analysis.
RESULTS
A total of 940 adults were approached; 347 were eligible, and 218 (63%) verbally consented to participate in the study. Reasons for not participating included lack of interest, time constraints, being occupied with other things, or child illness. The mean score on the Contemplation Ladder was 6.2 (SD, 2.5), representing the response: “Thinking about quitting or cutting down.” Eighty-four participants (39%) had high motivation to quit (Contemplation Ladder score ≥8). Table 2 displays the demographic characteristics of the sample overall and by level of motivation to quit. African Americans were more likely to be highly motivated to quit compared with whites; all other sociodemographic variables were not associated with motivation to quit.
TABLE 2.
Sample Demographics by Motivation to Quit Smoking
| Overall (n = 218) | Low Motivation† (n = 131) | High Motivation† (n = 84) | |
|---|---|---|---|
| Parent sex | |||
| Male | 23% | 20% | 29% |
| Female | 77% | 80% | 71% |
| Parent race* | |||
| White | 61% | 69% | 50% |
| Black | 36% | 30% | 45% |
| Other | 3% | 2% | 5% |
| Parent age, mean (SD), y | 30.9 (8.7) | 30.5 (8.6) | 31.8 (9.0) |
| Parent education | |||
| High school graduate or less | 48% | 47% | 50% |
| Insurance | |||
| Commercial | 21% | 24% | 18% |
| Child has primary care physician | |||
| Yes | 69% | 66% | 74% |
Significantly different by motivation level (P ≤ 0.05).
Low motivation defined by Contemplation Ladder score <8; high motivation ≥8.
Table 3 summarizes the smoking-related measures for the overall sample and by level of motivation to quit. The majority (79%) had made a serious quit attempt in the past year, and 27% were seriously thinking about quitting in the next 30 days. Most parents (74%) were nicotine dependent with an HSI of 4 or greater. Parents were more likely to have a higher motivation to quit if they reported: fewer numbers of cigarettes smoked per day; smoking within 5 minutes of wakening; desire to quit in the next 30 days; prior quit attempts; higher scores on importance, readiness, and confidence; and smoking-related illness in their child.
TABLE 3.
Parent Smoking-Related Variables
| Overall (n = 218) | Low Motivation (n = 131) | High Motivation (n = 84) | |
|---|---|---|---|
| Cigarettes per day* | |||
| 1–10 | 54% | 48% | 63% |
| 11–20 | 37% | 39% | 35% |
| >20 | 9% | 13% | 2% |
| Smoke in 5 min of wakening* | 28% | 33% | 20% |
| Want to quit in next 30 d* | 27% | 17% | 43% |
| Prior quit attempts* | 79% | 72% | 90% |
| Importance of stopping smoking,*† mean (SD) | 7.1 (2.5) | 6.3 (2.6) | 8.5 (1.6) |
| Readiness to quit smoking,*‡ mean (SD) | 5.5 (3.2) | 4.0 (2.6) | 7.8 (2.6) |
| Confidence that you can quit smoking,*§ mean (SD) | 4.6 (3.1) | 3.6 (2.7) | 6.1 (3.2) |
Significantly different by motivation to quit (P ≤ 0.05).
Scale 1–10, not important to most important goal.
scale 1–10, not at all ready to 100% ready.
scale 1–10, not at all confident to 100% confident.
When asked about personal health, only 14% of parents responded yes that they believe they have a serious health problem that was caused or made worse by smoking. Nine percent of parents reported a smoking-related illness in their child. Personal smoking-related illness was not significantly associated with high motivation to quit (P = 0.68); however, child smoking-related illness was associated with high motivation (P = 0.04).
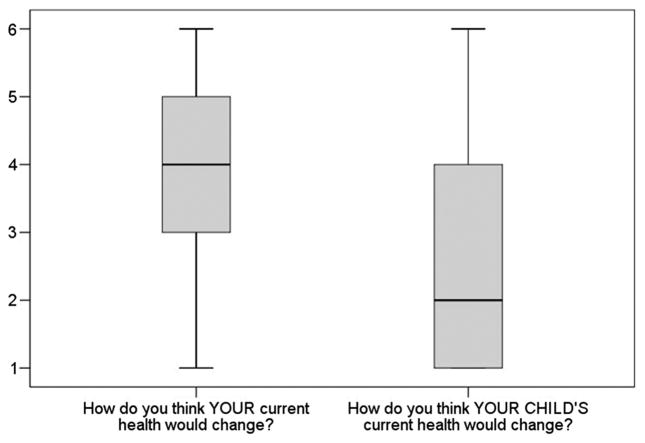
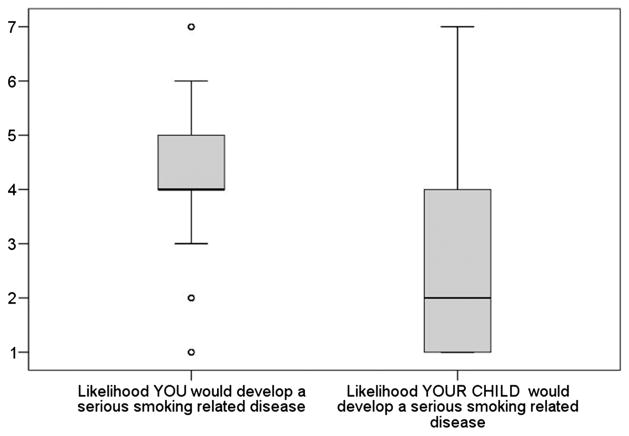
Figures 1 and 2 demonstrate the distribution of responses to the personal and child health benefit with smoking cessation and health risk with continued smoking. A matched paired analysis shows that parents were significantly more likely to report personal health benefits (Fig. 1) and risks (Fig. 2) compared with child health effects (P < 0.0001).
FIGURE 1.
Parent report of personal and child health benefit with smoking cessation. Note: Scale represents response to “If you stopped smoking, how do you think you/your child’s current health would change? Likert scale 1 = not at all to 6 = completely better.
FIGURE 2.
Parent report of personal and child health risk with continued smoking. Note: Scale represents response to “If you keep smoking, how likely is it do you feel that you/your child will develop a serious disease because of smoking? Likert scale 1 = no chance to 7 = 100% certain.
The unadjusted and adjusted odds ratios (ORs) from the logistic regression analysis for perceived health effects are shown in Table 4. The adjusted ORs showed that parents who reported that they or their child had higher health risk due to smoking were more likely to be highly motivated to quit. In addition, parents who believed their child’s health would improve if they quit smoking were more likely to be highly motivated to quit. Finally, of the variables that were used to develop the adjusted ORs, only the smoking-related variables were independently significantly (P < 0.05) associated with whether parents were highly motivated to quit. These variables were HSI, prior quit attempt, and confidence to quit. These results were consistent with the results of the multivariable model described below.
TABLE 4.
Relationship Between Perceived Health Effects and Whether Parents Are Highly Motivated to Quit
| Risk/Benefit Perception Scale† | Unadjusted OR (95% CI) | Adjusted OR* (95% CI) |
|---|---|---|
| Personal smoking-related illness | 0.85 (0.45–1.60) | 0.69 (0.32–1.49) |
| Child smoking-related illness | 2.06 (1.05–4.04) | 2.33 (1.02–5.36) |
| Quitting and personal health benefit | 1.29 (1.04–1.59) | 1.20 (0.93–1.53) |
| Personal health risk with continued smoking | 1.11 (0.91–1.35) | 1.39 (1.08–1.78) |
| Quitting and child health benefit | 1.24 (1.04–1.47) | 1.33 (1.07–1.65) |
| Child health risk with continued smoking | 1.26 (1.04–1.53) | 1.41 (1.11–1.80) |
An OR of greater than 1 indicates a positive association between report yes/don’t know of a smoking-related illness, increased perceived health risks with continued smoking or benefits with smoking cessation, and the likelihood that the parent is highly motivated to quit smoking.
Adjusted for sex, education, insurance type, ethnicity, race, prior quit attempt, confidence, and nicotine dependence.
Higher ratings denote higher perceived health risk with continued smoking or higher perceived benefit with smoking cessation.
The multivariable regression model showed that smoking variables were associated with motivation to quit. Nicotine dependence (ie, HSI) was negatively associated with motivation to quit (OR, 0.73; 95% confidence interval [CI], 0.56–0.96) as were no prior quit attempts (OR, 0.25; 95% CI, 0.10–0.63). Conversely, confidence in quitting smoking was positively associated with high motivation to quit (OR, 1.26; 95% CI, 1.12–1.41). Demographic variables were not significant predictors.
DISCUSSION
This study addresses factors associated with motivation to quit in parental smokers who present to the PED with their children. Motivation to quit smoking is crucial to participation in smoking cessation activities, quit attempts, and successful quitting.32 In the adult ED setting, it is known that cessation interventions are more likely to be more successful in smokers who are highly motivated to quit. These smokers are more interested and ready to quit, and they feel it is more important to quit.20 In addition, it has been shown that smokers who believed that their ED visit was due to a smoking-related illness were twice as likely to quit than those who did not.25 We hypothesized that these findings would translate to the PED setting, as we expected that parents who reported a personal smoking-related illness would be more motivated to quit. Our findings, however, did not support this hypothesis. Furthermore, parents who felt their health would improve with smoking cessation did not have more motivation to quit smoking. In contrast, parents who reported perceived personal health risk with continued smoking were more likely to be highly motivated to quit. This inconsistency in response may represent a fundamental lack of understanding of the health effects associated with smoking. This is supported by several earlier studies that demonstrate that many smokers underestimate the effects that current smoking has on their own health.33,34
Prior work has demonstrated that parental smokers of children with asthma who believe that their child’s asthma symptoms will decrease if they quit smoking or who felt that their child’s asthma is not under good control are more motivated to quit smoking.24 A recent meta-analysis reported that parental smoking cessation interventions that focused on child health in pediatric clinics and during inpatient hospitalization demonstrated increased parental quit rates.35 In our study, parents who reported a smoking-related illness in their child and child health risk with continued smoking were more likely to have high motivation to quit smoking. Our study was conducted in the PED where the focus is on the child’s health; this may in part explain the stronger association between high motivation to quit and parental perception of their child’s, but not their own, personal health effects. In addition, parents who recognized child health benefit with smoking cessation were more likely to have significantly higher motivation to quit smoking, in contrast to endorsement of personal health benefit. These findings indicate that cessation interventions for parental smokers in the PED setting that focus on the health risk of child SHSe may represent a unique opportunity that could translate to a powerful teachable moment that would potentially benefit a large population of children with SHSe.
Our study supports the hypothesis that parents who perceived child health risk with continued smoking and child health benefit with smoking cessation were more motivated to quit. However, many parental smokers in our study population appeared to be unaware of the harmful effects of SHSe on their child’s health. As shown in Figures 1 and 2, a significantly higher proportion of parents reported personal health risk if they continued smoking compared with health risk in their child. The majority of parents reported high, very high or certain personal health risk and no change, very low, or low health risk in their child. Similarly, parental smokers also seemed to have a greater awareness of the personal health benefits of quitting smoking versus the benefits in their child. However, parents who reported smoking-related illness in their child were 2.3 times more likely to report high motivation to quit compared with those who do not report child smoking-related illness. These results may indicate a knowledge deficit regarding the effects of SHSe on their child and represent an area for future educational intervention. In addition, teaching parents to be aware of the health risk of SHSe in their child despite good current pediatric health represents another potential area for intervention.
Our findings contrast with research in the adult ED and inpatient setting, which found that demographic characteristics such as higher socioeconomic status and private insurance were associated with high motivation to quit smoking. In our population, these demographics, in addition to age, sex, and education, did not correlate with a difference in motivation to quit. Because smoking prevalence is variable based on regional characteristics and demographics, it is likely that our results differ because of the population sampled. Prior quit attempts,24 low nicotine dependence,21 and high self-efficacy26 have been found to be associated with motivation to quit, and our results are consistent with that research.
In our population, 39% of parental smokers who presented to the PED with their child had a high motivation to quit smoking, reporting that they have cut down and are thinking about quitting or ready to quit now. Of the population sampled, most parental smokers (85%) intend to quit smoking; however, a much smaller proportion (27%) was ready to do so quickly within the next 30 days. This is important to remember when designing an intervention. Those who intend to quit smoking but have no immediate plans to quit require an intervention that will activate them to move from just intending to quit, to action.
Our study has several potential limitations. Our study population was a convenience sample, so the parents surveyed may not be representative of all parental smokers. Also, our study sample was collected in an urban, Midwest PED setting where the majority of subjects had a low socioeconomic status, which limits the generalizability of our results. We excluded parents of children who were moderately or acutely ill who may have had acute exacerbations of SHS-related illnesses. Thus, we were unable to assess if severity of illness impacted parental motivation to quit smoking. Finally, our enrollment rate was 63% of eligible parents; therefore, we may have excluded parents who were less motivated to quit.
Future studies are needed to determine if high motivation to quit translates into cessation attempts and long-term smoking abstinence. Interventions that combine an educational component with active support, such as nicotine replacement therapy, may encourage highly motivated parental smokers to quit.
CONCLUSIONS
The PED visit is a unique opportunity to address smoking cessation in parental smokers who present with their children. Parents who endorse health risk or quitting-related health benefits in their child are more likely to have high motivation to quit smoking. However, parents also show limited understanding of the effects of smoking on their child’s health. Future interventions that target the child’s health and provide education on the effects of child SHSe are needed and may be more effective in this setting. In addition, more research is needed to determine if high motivation translates into smoking cessation.
Acknowledgments
This study was funded by a divisional research grant. No external funding was secured for this study.
Footnotes
Disclosure: The authors declare no conflict of interest.
References
- 1.Centers for Disease Control and Prevention (CDC) Behavioral Risk Factor Surveillance System Survey Data. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention & Health Promotion, Centers for Disease Control and Prevention; 2010. [Accessed June 30, 2012]. Available at: http://apps.nccd.cdc.gov/brfss. [Google Scholar]
- 2.Clinical Practice Guideline Treating Tobacco Use and Dependence 2008 Update Panel, Liaisons, and Staff. A clinical practice guideline for treating tobacco use and dependence: 2008 update. A US Public Health Service report. Am J Prev Med. 2008;35:158–176. doi: 10.1016/j.amepre.2008.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Institute of Medicine. Committee on Reducing Tobacco Use. Strategies barriers and consequences. In: Bonnie RJ, Stratton KR, Wallace RB, editors. Ending the Tobacco Problem: A Blueprint for the Nation. Washington, DC: National Academies Press; 2007. [Google Scholar]
- 4.Bernstein SL, Boudreaux ED, Cydulka RK, et al. Tobacco control interventions in the emergency department: a joint statement of emergency medicine organizations. Ann Emerg Med. 2006;48:e417–e426. doi: 10.1016/j.annemergmed.2006.02.018. [DOI] [PubMed] [Google Scholar]
- 5.Cunningham RM, Bernstein SL, Walton M, et al. Alcohol, tobacco, and other drugs: future directions for screening and intervention in the emergency department. Acad Emerg Med. 2009;16:1078–1088. doi: 10.1111/j.1553-2712.2009.00552.x. [DOI] [PubMed] [Google Scholar]
- 6.Bock BC, Becker BM, Niaura RS, et al. Smoking cessation among patients in an emergency chest pain observation unit: outcomes of the Chest Pain Smoking Study (CPSS) Nicotine Tob Res. 2008;10:1523–1531. doi: 10.1080/14622200802326343. [DOI] [PubMed] [Google Scholar]
- 7.Bernstein SL, Bijur P, Cooperman N, et al. A randomized trial of a multicomponent cessation strategy for emergency department smokers. Acad Emerg Med. 2011;18:575–583. doi: 10.1111/j.1553-2712.2011.01097.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bernstein SL, Becker BM. Preventive care in the emergency department: diagnosis and management of smoking and smoking-related illness in the emergency department: a systematic review. Acad Emerg Med. 2002;9:720–729. doi: 10.1111/j.1553-2712.2002.tb02153.x. [DOI] [PubMed] [Google Scholar]
- 9.Mahabee-Gittens EM. Smoking in parents of children with asthma and bronchiolitis in a pediatric emergency department. Pediatr Emerg Care. 2002;18:4–7. doi: 10.1097/00006565-200202000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Mahabee-Gittens EM, Huang B. ED environmental tobacco smoke counseling. Am J Emerg Med. 2005;23:916–918. doi: 10.1016/j.ajem.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 11.Mahabee-Gittens EM, Gordon JS, Krugh ME, et al. A smoking cessation intervention plus proactive quitline referral in the pediatric emergency department: a pilot study. Nicotine Tob Res. 2008;10:1745–1751. doi: 10.1080/14622200802443494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pitts SR, Niska RW, Xu J, et al. National Hospital Ambulatory Medical Care Survey: 2006 Emergency Department Summary. National Health Statistics Reports. 2008:1–38. [PubMed] [Google Scholar]
- 13.Tutka P, Wielosz M, Zatonski W. Exposure to environmental tobacco smoke and children health. Int J Occup Med Environ Health. 2002;15:325–335. [PubMed] [Google Scholar]
- 14.Vargas PA, Brenner B, Clark S, et al. Exposure to environmental tobacco smoke among children presenting to the emergency department with acute asthma: a multicenter study. Pediatr Pulmonol. 2007;42:646–655. doi: 10.1002/ppul.20637. [DOI] [PubMed] [Google Scholar]
- 15.Mahabee-Gittens EM, Gordon J. Acceptability of tobacco cessation interventions in the pediatric emergency department. Pediatr Emerg Care. 2008;24:214–216. doi: 10.1097/PEC.0b013e31816a8d6f. [DOI] [PubMed] [Google Scholar]
- 16.Boudreaux ED, Kim S, Hohrmann JL, et al. Interest in smoking cessation among emergency department patients. Health Psychol. 2005;24:220–224. doi: 10.1037/0278-6133.24.2.220. [DOI] [PubMed] [Google Scholar]
- 17.Boudreaux ED, Baumann BM, Friedman K, et al. Smoking stage of change and interest in an emergency department–based intervention. Acad Emerg Med. 2005;12:211–218. doi: 10.1197/j.aem.2004.09.022. [DOI] [PubMed] [Google Scholar]
- 18.Bock BC, Becker B, Monteiro R, et al. Physician intervention and patient risk perception among smokers with acute respiratory illness in the emergency department. Prev Med. 2001;32:175–181. doi: 10.1006/pmed.2000.0799. [DOI] [PubMed] [Google Scholar]
- 19.Klinkhammer MD, Patten CA, Sadosty AT, et al. Motivation for stopping tobacco use among emergency department patients. Acad Emerg Med. 2005;12:568–571. doi: 10.1197/j.aem.2004.11.027. [DOI] [PubMed] [Google Scholar]
- 20.Bernstein SL, Boudreaux ED, Cabral L, et al. Nicotine dependence, motivation to quit, and diagnosis among adult emergency department patients who smoke: a national survey. Nicotine Tob Res. 2008;10:1277–1282. doi: 10.1080/14622200802239272. [DOI] [PubMed] [Google Scholar]
- 21.Bernstein SL, Cannata M. Nicotine dependence, motivation to quit, and diagnosis in emergency department patients who smoke. Addict Behav. 2006;31:288–297. doi: 10.1016/j.addbeh.2005.05.007. [DOI] [PubMed] [Google Scholar]
- 22.Jarvis MJ. The association between having children, family size and smoking cessation in adults. Addiction. 1996;91:427–434. [PubMed] [Google Scholar]
- 23.Winickoff JP, Hibberd PL, Case B, et al. Child hospitalization: an opportunity for parental smoking intervention. Am J Prev Med. 2001;21:218–220. doi: 10.1016/s0749-3797(01)00355-5. [DOI] [PubMed] [Google Scholar]
- 24.Halterman JS, Borrelli B, Conn KM, et al. Motivation to quit smoking among parents of urban children with asthma. Patient Educ Couns. 2010;79:152–155. doi: 10.1016/j.pec.2009.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Boudreaux ED, Baumann BM, Camargo CA, Jr, et al. Changes in smoking associated with an acute health event: theoretical and practical implications. Ann Behav Med. 2007;33:189–199. doi: 10.1007/BF02879900. [DOI] [PubMed] [Google Scholar]
- 26.Boudreaux ED, Hunter GC, Bos K, et al. Predicting smoking stage of change among emergency department patients and visitors. Acad Emerg Med. 2006;13:39–47. doi: 10.1197/j.aem.2005.07.030. [DOI] [PubMed] [Google Scholar]
- 27.Bernstein SL. The impact of smoking-related illness in the ED: an attributable risk model. Am J Emerg Med. 2002;20:161–164. doi: 10.1053/ajem.2002.32645. [DOI] [PubMed] [Google Scholar]
- 28.Richman PB, Dinowitz S, Nashed A, et al. Prevalence of smokers and nicotine-addicted patients in a suburban emergency department. Acad Emerg Med. 1999;6:807–810. doi: 10.1111/j.1553-2712.1999.tb01211.x. [DOI] [PubMed] [Google Scholar]
- 29.Biener L, Abrams DB. The Contemplation Ladder: validation of a measure of readiness to consider smoking cessation. Health Psychol. 1991;10:360–365. doi: 10.1037//0278-6133.10.5.360. [DOI] [PubMed] [Google Scholar]
- 30.Wagener TL, Gregor KL, Busch AM, McQuaid EL, Borrelli B. Risk perception in smokers with children with asthma. J Consul Clin Psychol. 2010;78:980–985. doi: 10.1037/a0021094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Miller WR, Rollnick S. Motivational Interviewing. New York: Guilford; 2002. [Google Scholar]
- 32.Williams GC, McGregor H, Sharp D, et al. Testing a self-determination theory intervention for motivating tobacco cessation: supporting autonomy and competence in a clinical trial. Health Psychol. 2006;25:91–101. doi: 10.1037/0278-6133.25.1.91. [DOI] [PubMed] [Google Scholar]
- 33.Strecher VJ, Kreuter MW, Kobrin SC. Do cigarette smokers have unrealistic perceptions of their heart attack, cancer, and stroke risks? J Behav Med. 1995;18:45–54. doi: 10.1007/BF01857704. [DOI] [PubMed] [Google Scholar]
- 34.Weinstein ND. Accuracy of smokers’ risk perceptions. Ann Behav Med. 1998;20:135–140. doi: 10.1007/BF02884459. [DOI] [PubMed] [Google Scholar]
- 35.Rosen LJ, Noach MB, Winickoff JP, et al. Parental smoking cessation to protect young children: a systematic review and meta-analysis. Pediatrics. 2012;129:141–152. doi: 10.1542/peds.2010-3209. [DOI] [PubMed] [Google Scholar]