Abstract
Purpose
Peer support groups for cancer patients show mixed findings regarding effectiveness on psychological wellbeing. When embedded in a psychosocial intervention, such as mindfulness-based stress reduction (MBSR), peer support might be of more benefit to participants. This study is a qualitative exploration of how women with breast cancer experience the possible benefits and impediments of participating with fellow patients in an MBSR training.
Methods
Five focus groups (n = 37) and three individual interviews (n = 3) were conducted with breast cancer patients who participated in MBSR. The qualitative data were analysed with the constant comparative method in order to develop a grounded theory.
Results
We could identify a process where at the start of MBSR, patients experienced anticipatory fear for facing the suffering of fellow patients, especially for those who could not be cured anymore. In most women, this fear gradually subsided during the first two sessions. The atmosphere in the MBSR training was experienced as safe and supportive, providing a context where participants could connect with and trust one another. In turn, this facilitated participants to learn from one another.
Conclusions
Our findings do not only show that the peer group facilitates the learning process in MBSR, but the MBSR also seemed to provide an atmosphere that promotes the experienced social support in participants. In addition, the results emphasize the importance for mindfulness teachers to acknowledge and explore the fear for facing fellow patients in the group. Future research should examine whether the results are generalizable to patients with other cancer types.
Keywords: Mindfulness-based stress reduction, Breast cancer, Peer support, Qualitative, Focus group
Introduction
With an estimated 1.4 million new cases each year, breast cancer is the most frequently diagnosed cancer among women worldwide [1]. Around one third of breast cancer patients report heightened levels of distress, often requiring psychosocial care [2–4].
Since the early 1980s, support groups of cancer patients have been widely studied [5]. Peer support entails the mutual exchange of support based on shared personal experiences and experiential empathy between cancer patients and/or survivors [5, 6]. A systematic review examining 43 studies on peer support programs for cancer patients concluded that participants report high satisfaction levels with peer support groups but showed mixed results regarding the effectiveness on psychological wellbeing. A few studies even found adverse outcomes, such as increased emotional suppression [7, 8], increased dissatisfaction with medical care [7] and more anxious coping styles [9]. These results suggest that merely sharing personal experiences between cancer patients is not always helpful to patients. For instance, patients may suppress their emotions because they are afraid of burdening others. Peer support in combination with an intervention that helps patients cope with their distress may prevent the possible adverse outcomes of peer support [7].
A well-validated and often studied intervention in cancer patients that is offered in groups, but not focused on peer support, is mindfulness-based stress reduction (MBSR). Mindfulness is defined as intentionally paying attention to present-moment experiences in an accepting and non-judgmental way [10]. Recent meta-analyses concluded that mindfulness-based interventions are effective in decreasing psychological distress in cancer patients [11, 12], including improvements in anxiety and depressive symptoms, mood and quality of life. MBSR is an 8-week group-based training consisting of mindfulness practices and didactic teaching on coping with stress. Each session there is also a time to share experiences with other participants. As patients practice observing their experiences in a non-judgmental way, they gain insight into their behavioural patterns, such as suppressing or identifying with their emotions [13]. In turn, patients may learn allowing and accepting their emotions as well as letting go of emotions, enabling them to be present with one’s own and other patients’ suffering without automatically reacting to it [14]. As such, the training might provide a context for patients where they feel safe to express their emotions and share personal experiences.
A recent randomized controlled trial in breast cancer patients [15] compared MBSR with supportive expressive group therapy (SET), a psychotherapy specially designed to increase social support and express disease-related emotions [16]. The intention-to-treat analyses showed that women in MBSR showed more improvement over time on stress symptoms compared with women in SET. Interestingly, per-protocol analyses showed that patients felt more supported after MBSR compared to SET.
Qualitative studies also report on the effects of experienced peer support in MBSR for cancer patients. In men with advanced prostate cancer, the mindfulness-based therapy combined with experiencing peer support in a group setting enhanced acceptance of the cancer progression [17]. A pilot study in lung cancer patients and their partners showed mixed results [18]. While some participants experienced the peer group as distressing when fellow participants dropped out due to illness progression, the majority of participants experienced it as facilitating because of the mutual understanding.
In sum, while patients are satisfied with peer support groups, it does not always benefit their psychological wellbeing. Peer support embedded in the context of an intervention aiming to help patients cope with their distress might be more beneficial for patients. Although MBSR is not focused on increasing peer support, sharing personal experience while practicing mindfulness might be of benefit to participants. The aim of the present study is to further explore how women with breast cancer experience the possible benefits and impediments of participating with fellow patients in the context of an MBSR training.
Material and methods
Study population
Females with breast cancer were recruited at the outpatient oncology clinic of the Radboud University Medical Centre in Nijmegen and Hospital Rijnstate in Arnhem and trough the website of the national foundation for breast cancer patients (www.pinkribbon.nl) from September 2012 to March 2014. We included patients who were previously diagnosed with breast cancer, at least 18 years of age and able to understand and use the Dutch language. The local medical ethics committee indicated that no formal approval was required as the study was an uncontrolled study of an intervention already used in clinical care (registration number CMO2012/493). All participants provided written informed consent.
Procedure
Interested patients were invited for a research interview at the Radboud Centre for Mindfulness to offer information about MBSR, explore their motivation and whether they wanted to participate alone or together with their partner. Before and after the intervention, patients filled out questionnaires on psychosocial functioning and an evaluation form about MBSR training. Patients who participated in MBSR for breast cancer patients only were invited for a focus group interview 1 week after completion of the training. Patients who participated with their partner in MBSR for mixed cancer patients and their partners were invited for an individual interview after they completed the training.
Focus groups
Focus groups were chosen as it encourages participants to openly explore the introduced topics in the original composition of the MBSR group and discuss the issues of importance to them [19]. Focus groups took place at the Radboud Centre for Mindfulness 1 week after completion of MBSR and lasted 100–120 min. Four focus groups were led by AS, a professor in psychiatry and qualified mindfulness teacher, and one focus group was conducted by EJ, a psychologist and qualified mindfulness teacher. Both interviewers had not been involved with the MBSR courses themselves. Focus groups started with explaining confidentiality and the explorative nature of the interview. Questions were asked in an open non-directive manner, allowing participants to speak freely about their experiences. One of the discussed topics was peer support, assessed with the following question: ‘How did you experience participation with other (breast) cancer patients in the MBSR training?’
As only a limited number of patients wanted to participate with their partner, these patients were interviewed individually instead of in a focus group. EJ conducted the individual semi-structured in-depth interviews, which lasted 30–60 min and took place at the centre or by phone, according to patients’ preferences.
Both focus groups and individual interviews were audio-taped and transcribed verbatim. A summary was sent back to the participants for a member-check. Participants indicated that their answers had been interpreted correctly.
Intervention
The MBSR curriculum as developed by Kabat-Zinn was closely followed [10]. MBSR is an 8-weekly group-based training of 2.5-h sessions and a 6-h silent day between sessions 6 and 7. Sessions consisted of mediation practices (such as the body scan, gentle yoga, sitting and walking meditation), didactic teaching on stress and sharing experiences with one another. Participants were invited to practice at home for 45 min each day. They received a CD with guided meditations and a folder with information about the content of the training. To tailor the intervention to cancer patients, psycho-education about grief was added [20]. Furthermore, patients could invite their partner or close other to attend a session on mindful communication, discussing the impact of cancer on their relationship. The training was conducted by a medical social worker who was a professionally trained mindfulness teacher, fulfilling the mindfulness-based intervention teacher assessment criteria [21].
Data analysis
The data of the focus groups and interviews on participating with fellow patients were analysed with the constant comparative method in order to develop a grounded theory [22]. Data analysis started as the first focus group was transcribed and continued with each additional focus group or interview. Two researchers (EJ and MS, behavioural scientist and mindfulness teacher in training) coded the transcripts independently. After three focus groups, the codes were compared and discussed by three researchers (MS, EJ and AS) until reaching consensus. This led to a new coding scheme, to which new codes could be added. After five focus groups and three interviews, saturation was reached. Consequently, the three researchers grouped the codes referring to the same step in the process into subthemes, and subthemes into themes, enabling them to derive hypotheses from the data.
Results
Of the 50 patients who started with MBSR, 43 patients completed the training. Reasons for dropout were the reluctance to face other (palliative) patients (n = 5), training did not fit in schedule (n = 1) and side effects of chemotherapy (n = 1). Of the 43 patients who completed the training, data of 40 patients were available for qualitative data analysis. Thirty-seven patients who participated in MBSR solely for breast cancer patients participated in the focus groups. One palliative patient who could not attend the focus group was interviewed individually, because she could have different experiences as being a minority in the group. Two patients who participated in the group for mixed cancer patients were also interviewed individually. Demographic and clinical characteristics of the study participants are summarized in Table 1.
Table 1.
Demographic and clinical characteristics of the 40 patients who participated in the focus groups and interviews
| Patients (n = 40) | ||
|---|---|---|
| n | (%) | |
| Age, M (SD) | 52.3 | (7.43) |
| Marital status | ||
| Married | 23 | (57.5) |
| Living together | 8 | (20.0) |
| Divorced | 1 | (2.5) |
| Widowed | 2 | (5.0) |
| Single | 5 | (12.5) |
| Living apart together | 1 | (2.5) |
| Educational level | ||
| Low | 1 | (2.5) |
| Intermediate | 16 | (40.0) |
| High | 23 | (57.5) |
| Stage of disease | ||
| Curative | 37 | (92.5) |
| Palliative | 3 | (7.5) |
| Time since diagnosis in months | ||
| <3 months | 3 | (7.5) |
| 3 months to 1 year | 17 | (42.5) |
| >1 year | 17 | (42.5) |
| >5 years | 3 | (7.5) |
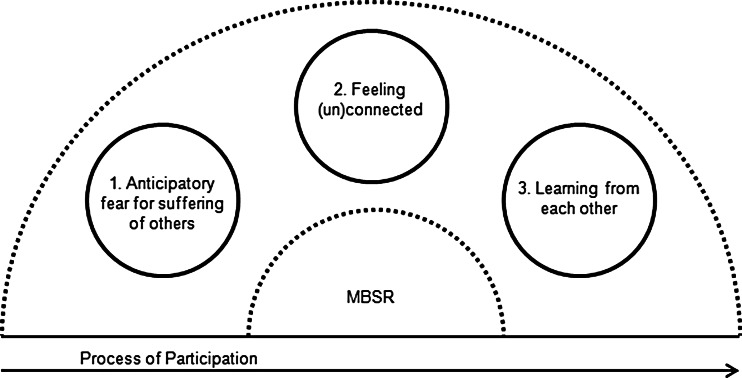
The analysis of the focus group and interview data resulted in three main themes: anticipatory fear for suffering of others, feeling (un)connected and learning from each other, which can be subdivided into 11 subthemes (see Table 2). It appears that participants go through a process of participation where fear for facing fellow patients especially palliative patients is mostly apparent before the start of MBSR. Throughout the training, participants feel more connected with and supported by one another, which resulted in learning from each other (see Fig. 1).
Table 2.
Themes and subthemes of how women experienced participation with other breast cancer patients in an MBSR training
| Themes | Subthemes |
|---|---|
| Anticipatory fear for suffering of others | Avoidance of facing fellow patients |
| Fear for negative disease course | |
| Identification with suffering of others | |
| Survivors’ guilt | |
| Feeling (un)connected | Recognition |
| Feeling accepted | |
| Feeling disconnected | |
| Learning from each other | Acknowledging emotions |
| De-identification with disease | |
| Gaining other perspectives | |
| Learning to cope |
Fig. 1.
Process of participation with fellow patients embedded in an MBSR training
Theme 1: anticipatory fear for suffering of others
Four categories of anticipatory fear for suffering of others emerged: avoidance of facing fellow patients, fear for a negative course of the disease, identification with suffering of others and survivors’ guilt.
Avoidance of facing fellow patients
Many participants mentioned that before they started with the training, they tended to avoid meeting other breast cancer patients.
Yes so, I did not really need all these stories from my fellow patients. One drama story after another, I was like I’d rather focus on my own story and get that right. That was my starting point.
As a consequence some patients mentioned that they detached themselves from the experiences of fellow patients to protect themselves, especially at the start of the MBSR.
And then, the first time I really did not hear some of your stories. I was thinking, I can’t do it and I won’ t do it. Just to only listen to these stories, so, sure I did miss some things the first time [laughs]. I just could not absorb it all.
Fear for a negative course of the disease
Although patients chose to participate in a mindfulness training for breast cancer, they felt reluctant to face fellow patients, especially palliative patients, as they gave rise to feelings of uncertainty about their own prognosis.
I find that so difficult, every little ache makes me scared that I might die after all.
Identification with suffering of others
For some participants, being in a group with fellow-patients led to identifying with the suffering of others. This identification process appeared to be distressing and could result in fear when experiences of others were used as references for possible outcomes in their own lives.
Well, I thought it was a little scary, (…) my last chemo was not that long ago and I was scared of what would come and then you hear all these stories. I was thinking: oh my goodness, that can happen to me too
Experiencing the stories of fellow patients weighted heavily upon the shoulders of some participants.
Recognition is fine, but I did also experience it as difficult. (…) The intensity of the stories that you hear and the intensity of the emotions and other people’s problems, that I carry along with me
These fears gradually subsided as the training proceeded.
Survivors’ guilt
In each MBSR group, only one to two patients who could not be cured anymore participated. Patients with a curative perspective mentioned that they would have found a higher number of palliative group members difficult, in that they might have felt reluctant in sharing their own difficulties which seemed much less important than those of fellow-group members who had to face dying.
I would feel uncomfortable to express my minor concerns, because these are less heavy in comparison to the ones people are dealing with who know they are not going to get better
Theme 2: feeling (un)connected
Participating in the MBSR training with fellow patients resulted in feeling connected with each other. Most participants emphasized the fact that everyone faced the challenge of coping with (breast) cancer as an important benefit of participating in MBSR with fellow-patients. However, participants who were less represented in the group, for example, being the only one with palliative treatment or the only one with a proportionally less intensive treatment for her cancer, reported feeling disconnected from the rest. The theme feeling (un)connected was subdivided into three subthemes: recognition, feeling accepted and feeling disconnected.
Recognition
Since participants shared a (breast) cancer diagnosis, participants recognized themselves in each other. This recognition lessened the need to explain things that people without (breast) cancer might not understand.
xIt’s really easy because you do not have to explain everything, going through it together makes it really easy for me to be with fellow patients. I think that is the same for everyone. (…) The starting point is about the same.
Because all participants specifically chose for a mindfulness-based training, there was also recognition in the way they wanted to deal with their breast cancer diagnosis.
Because we all chose mindfulness, I think that is also important. You are looking for some deeper feelings
Feeling accepted
The MBSR training provided an atmosphere of support and safety. The majority of the patients mentioned that participating with fellow patients in MBSR resulted in feelings of connectedness, solidarity and trust.
The fact that you can talk about it without any constraint and that you also feel safe.(…) That you feel safe because you say what you want to say and you don’t feel restricted in what you would like to say because it could be very difficult of upsetting. There were no constraints and I got the impression it was the same for others. That you have a safe place to be.
Feeling disconnected
A few participants belonged to a minority in the group, due to having a poor prognosis or a less intensive treatment than most others in the group, which made them feel less connected with the other patients. One patient described how having incurable cancer, which separated her from the others in the group, made her angry:
It was grief really, after all you do meet women who can continue for another ten years doing hormone therapies or take all kinds of pills. After awhile I was noticing I was getting angry. Like, damn it why are they taking this from me. My life. Although I still try to just go on.
Theme 3: learning from each other
As the training continued and participants gained insight into their feelings, thoughts and emotions, contact with fellow patients facilitated the individual learning processes. The following dimensions of learning emerged from the analysis: acknowledging emotions, de-identification with the disease, gaining different perspective and learning to cope.
Acknowledging emotions
Seeing and hearing how fellow patients learned to deal with their emotions during MBSR, facilitated how participants learned to recognize and acknowledge these emotions within themselves. Moreover, they learned to allow these feelings and to experience the positive effects of the willingness of being vulnerable.
Yes, in the whole process of being ill I have learnt to show my vulnerability. Like I just said, I was always tough and yes, I’m OK and no problem at all. I hear the same from others around.’
Furthermore, participants mentioned it was helpful for them to see how others in their group expressed their feelings.
And it really helped me, I find it very difficult to always explain or say how I feel, and they put that into words. And then I realize, well, this is what I mean.
De-identification with disease
In contact with fellow patients, women started to see and get to know the person behind the disease and consequently person and disease became more and more distinct from each other. De-identification took place in how they viewed themselves as well as the others, meaning redefining their identity from being a breast cancer patient to having breast cancer.
We just formed a group of all kinds of people and not diagnoses. And I didn’t think that would happen beforehand. It wasn’t confronting, it wasn’t a nuisance. I mean: Well, D. is incurably ill, but when I think of D. I do not think of her as being incurably ill.
Gaining different perspectives
During the MBSR, patients gained insight into their thoughts, feelings and automatic reaction patterns. Sharing their perspectives with one another led to change in their views and facilitated understanding of what they experienced themselves.
It was very inspiring to hear the other women talk about their experiences especially after the silent retreat day. Hearing other people’s stories helps me put my own problems into perspective. That’s the reason why it’s nice to hear about other experiences
Learning to cope
Seeing how others dealt with having breast cancer in the MBSR training, gave patients strength and helped patients learning to cope differently.
Because I see how she is handling it and that gives me strength as well. Just because if I would ever be in the same situation then that is the way I would like to deal with it. That is really beautiful. That shows me, I don’t have to fear it, I could do it in this way, too.
Discussion
The present qualitative study explored the role of experienced benefits and impediments of participating with fellow breast cancer patients in the MBSR training. Before the start of the training, most patients experienced anticipatory fear of meeting other breast cancer patients. For some patients, this anticipatory fear of facing the suffering of other patients was a reason to drop out the training. However, in most women, this fear attenuated after one or two sessions. During the training, the interaction with fellow patients resulted in a feeling of being connected with one another. The atmosphere in the MBSR training was experienced as safe and supportive, providing a context where participants could connect with and trust one another. Patients felt accepted. This supportive environment helped patients to facilitate each other’s learning processes, such as acknowledging their emotions and gaining different perspectives. A few women who formed a minority in the group felt less connected with the others, which could prevent them from fully participating and learning from one another during the MBSR.
Our findings are in line with former qualitative studies on MBSR in cancer showing how the peer group facilitates participation in the MBSR training and benefits the process of coping with the cancer [17, 18]. A recent meta-ethnography [23] of 14 studies on how different patient populations experience mindfulness-based interventions (MBI) showed that the group context in MBI facilitates the change in how participants experience their illness. Sharing the same diagnosis enhanced a sense of community [24], which facilitated the communal mindfulness journey.
Besides the finding that the peer group facilitates the learning process in MBSR, we also found that MBSR provides an atmosphere that promotes the experienced peer support. Like seen in other peer support contexts [6], participants experienced fear at the start of the MBSR training. By avoiding that fear or indentifying with the suffering of others, patients can remain stuck in that fear. The MBSR program, however, provides an atmosphere of nonjudgmental awareness and compassion, which fosters the allowing and accepting of emotions [13]. More specifically, by turning towards fear, sadness and loneliness and cultivating the willingness to be equally near to the pleasant and unpleasant, one may learn to experience thoughts and emotions as simply unfolding in this moment. Participants may start to recognize the continually changing nature of life. Realizing these unpleasant emotions are not unique and personal but also experienced by others can create a sense of common humanity, that one is not alone in one’s pain and that suffering is inherent to life [14].
Strengths and limitations
The present study has a number of strengths. The relatively large sample size enabled us to reach data saturation and report a broad view of experiences. Moreover, we performed member-checks to ensure the validity of the interpretations.
Despite the adequate sample size and data saturation, the present study has sampling limitations. All patients who participated in the training were invited for focus groups or individual interviews. However, some patients declined participation. Therefore, we cannot ascertain whether the full range of possible cases was included [19]. Moreover, patients who dropped out were not included in the analysis. We did interview these patients by telephone, giving us an impression why they dropped out, indicating the majority of dropouts stopped because they did not want to be confronted with other patients. Another possible limitation of the study is primarily using focus groups. While focus groups are efficient in exploring experiences, it can hold back participants from speaking up when their experiences diverge from the majority. This could be a reason that the subtheme feeling disconnected has not been so extensively explored. By combining different data sources (e.g. written evaluation, participating observation, individual interview), the results could be strengthened. In addition, only two patients participated in a mixed cancer group, and while their results are similar to the patients in the breast cancer group, the number is too small to generalize these results to mixed cancer groups.
Implications
The present study implies that the group-based setting in MBSR is of added value to breast cancer patients. To prevent dropout it is important to acknowledge patients’ anticipatory fear of being in a group with other (palliative) patients at the start of the training. During the training, the mindfulness teacher should be alert on expressions of fear, acknowledge them and explore these in the group. In addition, our results suggest that trainers should be aware of incurable patients in the group who might feel disconnected from the others and acknowledge these patients in their grief and anger. Moreover, it might be helpful to include a mix of participants (e.g. different stages of disease, age groups) in the training, so each participant has a few peers in similar circumstances to relate to.
Although our results suggest that both curative and palliative patients can participate together in MBSR, future research could examine the experiences of the palliative patients more extensively. Additionally, to examine the generalizability of the current findings, it would be helpful if future research could include the role of participating with fellow patients in mixed cancer groups as this is the most common context of offering MBSR in clinical practice.
Acknowledgments
This research was funded by the national foundation for breast cancer Pink Ribbon. We would like to thank Rinie van den Boogaart for teaching the MBSR classes, and we are grateful to Rhoda Schuling, Kees Kennedy and Felicia Maer for translating the relevant quotations.
Conflict of interest
We received funding from the Dutch charitable foundation Pink Ribbon. We have full control of all primary data, and we agree to allow the journal to review the data if requested.
Footnotes
Melanie P. J. Schellekens and Ellen T. M. Jansen share first authorship
References
- 1.Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61(2):69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 2.Carlson LE, Angen M, Cullum J, Goodey E, Koopmans J, Lamont L, MacRae JH, Martin M, Pelletier G, Robinson J, Simpson JSA, Speca M, Tillotson L, Bultz B. High levels of untreated distress and fatigue in cancer patients. Br J Cancer. 2004;90(12):2297–2304. doi: 10.1038/sj.bjc.6601887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Henselmans I, Helgeson VS, Seltman H, de Vries J, Sanderman R, Ranchor AV. Identification and prediction of distress trajectories in the first year after a breast cancer diagnosis. Health Psychol. 2010;29(2):160–168. doi: 10.1037/a0017806. [DOI] [PubMed] [Google Scholar]
- 4.Fiszer C, Dolbeault S, Sultan S, Brédart A. Prevalence, intensity, and predictors of the supportive care needs of women diagnosed with breast cancer: a systematic review. Psycho-Oncology. 2014;23(4):361–374. doi: 10.1002/pon.3432. [DOI] [PubMed] [Google Scholar]
- 5.Gray R, Fitch M, Davis C, Phillips C. A qualitative study of breast cancer self-help groups. Psycho-Oncology. 1997;6(4):279–289. doi: 10.1002/(SICI)1099-1611(199712)6:4<279::AID-PON280>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]
- 6.Hoey LM, Ieropoli SC, White VM, Jefford M. Systematic review of peer-support programs for people with cancer. Patient Educ Couns. 2008;70(3):315–337. doi: 10.1016/j.pec.2007.11.016. [DOI] [PubMed] [Google Scholar]
- 7.Giese-Davis J, Bliss-Isberg C, Carson K, Star P, Donaghy J, Cordova MJ, Stevens N, Wittenberg L, Batten C, Spiegel D. The effect of peer counseling on quality of life following diagnosis of breast cancer: an observational study. Psycho-Oncology. 2006;15(11):1014–1022. doi: 10.1002/pon.1037. [DOI] [PubMed] [Google Scholar]
- 8.Lieberman MA, Golant M, Giese-Davis J, Winzlenberg A, Benjamin H, Humphreys K, Kronenwetter C, Russo S, Spiegel D. Electronic support groups for breast carcinoma—a clinical trial of effectiveness. Cancer. 2003;97(4):920–925. doi: 10.1002/cncr.11145. [DOI] [PubMed] [Google Scholar]
- 9.McGovern RJ, Heyman EN, Resnick MI. An examination of coping style and quality of life of cancer patients who attend a prostate cancer support group. J Psychosoc Oncol. 2002;20(3):57–68. doi: 10.1300/J077v20n03_04. [DOI] [Google Scholar]
- 10.Kabat-zinn J. Full catastrophe living: using the wisdom of your body and mind to face stress, pain and illness. New York: Delacourt; 1990. [Google Scholar]
- 11.Cramer H, Lauche R, Paul A, Dobos G. Mindfulness-based stress reduction for breast cancer—a systematic review and meta-analysis. Curr Oncol. 2012;19(5):E343–E352. doi: 10.3747/co.19.1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Piet J, Wurtzen H, Zachariae R. The effect of mindfulness-based therapy on symptoms of anxiety and depression in adult cancer patients and survivors: a systematic review and meta-analysis. J Consult Clin Psychol. 2012;80(6):1007–1020. doi: 10.1037/a0028329. [DOI] [PubMed] [Google Scholar]
- 13.Segal ZV, Williams JMG, Teasdale JD. Mindfulness-based cognitive therapy for depression: a new approach to preventing relapse. New York: Guilford Press; 2002. [Google Scholar]
- 14.Feldman C, Kuyken W. Compassion in the landscape of suffering. Contemp Buddhism. 2011;12(1):143–155. doi: 10.1080/14639947.2011.564831. [DOI] [Google Scholar]
- 15.Carlson LE, Doll R, Stephen J, Faris P, Tamagawa R, Drysdale E, Speca M (2013) Randomized controlled trial of mindfulness-based cancer recovery versus supportive expressive group therapy for distressed survivors of breast cancer (MINDSET). J Clin Oncol. 2012.2047. 5210 [DOI] [PubMed]
- 16.Classen CC, Kraemer HC, Blasey C, Giese-Davis J, Koopman C, Palesh OG, Atkinson A, DiMiceli S, Stonisch-Riggs G, Westendorp J, Morrow GR, Spiegel D. Supportive-expressive group therapy for primary breast cancer patients: a randomized prospective multicenter trial. Psycho-Oncology. 2008;17(5):438–447. doi: 10.1002/pon.1280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chambers SK, Foley E, Galt E, Ferguson M, Clutton S. Mindfulness groups for men with advanced prostate cancer: a pilot study to assess feasibility and effectiveness and the role of peer support. Support Care Cancer. 2012;20(6):1183–1192. doi: 10.1007/s00520-011-1195-8. [DOI] [PubMed] [Google Scholar]
- 18.van den Hurk DGM, Schellekens MPJ, Molema J, Speckens AEM, van der Drift MA. Mindfulness-based stress reduction for lung cancer patients and their partners: results of a mixed methods pilot study. Palliat Med. 2015 doi: 10.1177/0269216315572720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pope C, Mays N, editors. Qualitative research in health care. BMJ books. 2. London: BMJ Publishing Group; 1999. [Google Scholar]
- 20.Schellekens MPJ, van den Hurk DGM, Prins JB, Molema J, Donders ART, Woertman WH, van der Drift MA, Speckens AEM (2014) Study protocol of a randomized controlled trial comparing mindfulness-based stress reduction with treatment as usual in reducing psychological distress in patients with lung cancer and their partners: the MILON study. BMC Cancer 14(1):3 [DOI] [PMC free article] [PubMed]
- 21.Crane RS, Kuyken W, Williams JMG, Hastings RP, Cooper L, Fennell MJV. Competence in teaching mindfulness-based courses: concepts, development and assessment. Mindfulness. 2012;3:76–84. doi: 10.1007/s12671-011-0073-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Corbin J, Strauss A. Grounde theory research. Procedures, canons, and evaluative criteria. Qual Sociol. 1990;13:S1–S21. doi: 10.1007/BF00988593. [DOI] [Google Scholar]
- 23.Malpass A, Carel H, Ridd M, Shaw A, Kessler D, Sharp D, Bowden M, Wallond J. Transforming the perceptual situation: a meta-ethnography of qualitative work reporting patients’ experiences of mindfulness-based approaches. Mindfulness. 2012;3(1):60–75. doi: 10.1007/s12671-011-0081-2. [DOI] [Google Scholar]
- 24.Mackenzie MJ, Carlson LE, Munoz M, Speca M. A qualitative study of self-perceived effects of mindfulness-based stress reduction (MBSR) in a psychosocial oncology setting. Stress Health. 2007;23(1):59–69. doi: 10.1002/smi.1120. [DOI] [Google Scholar]