Abstract
Mycoplasma genitalium is a potentially major cause of urethritis, cervicitis, pelvic inflammatory disease, infertility, and increased HIV risk. A better understanding of its natural history is crucial to informing control policy. Two extensive cohort studies (students in London, UK; Ugandan sex workers) suggest very different clearance rates; we aimed to understand the reasons and obtain improved estimates by making maximal use of the data from the studies. As M. genitalium is a sexually-transmitted infectious disease, we developed a model for time-to-event analysis that incorporates the processes of (re)infection and clearance, and fitted to data from the two cohort studies to estimate incidence and clearance rates under different scenarios of sexual partnership dynamics and study design (including sample handling and associated test sensitivity). In the London students, the estimated clearance rate is 0.80p.a. (mean duration 15 months), with incidence 1.31%-3.93%p.a. Without adjusting for study design, corresponding estimates from the Ugandan data are 3.44p.a. (mean duration 3.5 months) and 58%p.a. Apparent differences in clearance rates are probably mostly due to lower testing sensitivity in the Uganda study due to differences in sample handling, with 'true' clearance rates being similar, and adjusted incidence in Uganda being 28%p.a. Some differences are perhaps due to the sex workers having more-frequent antibiotic treatment, whilst reinfection within ongoing sexual partnerships might have caused some of the apparently-persistent infection in the London students. More information on partnership dynamics would inform more accurate estimates of natural-history parameters. Detailed studies in men are also required.
Introduction
Sexually-transmitted Mycoplasma genitalium has recently gained increasing attention as a major cause of urethritis [1–3], cervicitis [1,2,4], pelvic inflammatory disease (PID) [1,2], infertility [2,5], and increased HIV risk [2,6]. Currently testing is not routinely done in, e.g., UK or USA, and there is only limited testing in Australia [7–10], so disease would be usually diagnosed syndromically, e.g., non-chlamydial non-gonococcal urethritis. Furthermore, frequent treatment failures [10–12] and high prevalence of macrolide-resistant strains [9,13–15] indicate suboptimal infection management and treatment [16,17].
M. genitalium’s impact on sexual and reproductive health necessitates a greater understanding of its natural history, including duration of untreated infection, proportion of infections that are symptomatic, and infectivity, to inform decisions regarding if and how public health interventions should be implemented. There have been calls for such interventions for M. genitalium [15–17], but we note that continued uncertainty regarding the natural history of Chlamydia trachomatis [18,19] means that the (cost-)effectiveness of screening remains unknown, and the interventions now in place complicate further study.
Two extensive cohort studies [20–23] have examined aspects of M. genitalium’s natural history in women, including rates of clearance of infection; intriguingly, the clearance rates were apparently very different. As cohort studies are difficult, expensive and time-consuming to conduct, it is important to obtain the maximum information from them.
In this paper we obtain refined parameter estimates through using an analytic approach that synthesizes additional evidence reported by the studies. In particular, we take into account that M. genitalium is a sexually-transmitted infection, and that members of the study cohort might acquire infection during the study, and that that those infected at enrolment might recover and become infected again by the time of follow-up, which would not be distinguishable from a persistent infection.
Furthermore, we aim to gain insight into the reasons for the differences reported by the studies, including potential reinfection within stable sexual partnerships (in a prolonged partnership if one partner is infected then there is an elevated risk that both partners will be infected, so that if one partner recovers during the partnership, there is an elevated risk of the person becoming infected again rapidly), to determine if the differences are likely to be due to differences in study design or due to ‘real’ biological or behavioral differences. Finally, we make recommendations for improving future studies to inform decisions regarding if and how public-health decision-making regarding if and how interventions should be implemented.
Materials and Methods
We estimated the clearance rates from data that were collected in two cohort studies, one of students in London, UK, [20] and the other of Ugandan sex workers [21–23], using models that include acquisition of infection, including recurrent infection, as well as recovery. We further analyzed how two factors, (i) duration of sexual partnerships and (ii) test sensitivity, influence parameter estimates.
In this paper, we use “recurrent infection” to refer to an infection acquired after clearance of a previous infection, and “reinfection” as a recurrent infection that is acquired within a stable sexual partnership.
Data
Female students, London, UK
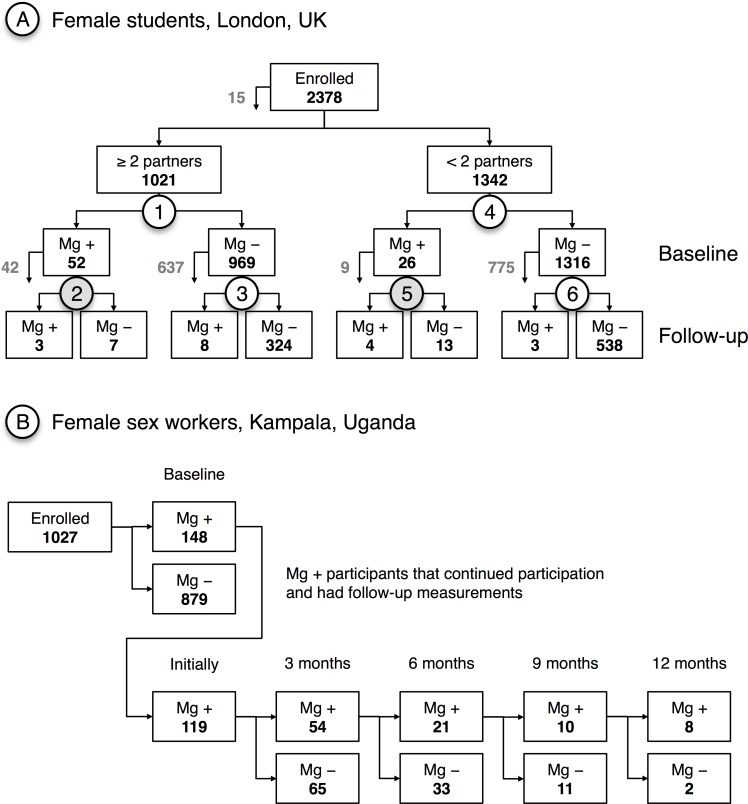
Oakeshott et al. [20] conducted a combined C. trachomatis and M. genitalium cohort study of female students in London (mean age: 21 years). Participants completed a sexual-behavior questionnaire at baseline and provided self-taken vaginal swabs at baseline and follow-up, 11–32 months later. Specimens were stored at -80°C until tested for M. genitalium by PCR. Fig 1A summarizes results.
Fig 1. Flow charts of two cohort studies.
(A) Oakeshott et al. [20]; numbers 1 to 6 are data items that are referred-to in the text; follow-up was after 12–21 months (median 16 months) for items 2 and 5 (grey), and after 11–32 months (median 16 months) for items 3 and 6; arrows exiting boxes indicate numbers of participants lost. (B) Vandepitte et al. [21]; numbers of M. genitalium-positive and -negative participants at baseline, as well as numbers of participants consistently M. genitalium-positive at consecutive time points, and numbers testing negative at each time point, who were not considered further in the analysis.
Female sex workers, Kampala, Uganda
Vandepitte et al. [21–23] conducted a cohort study of women working in the sex industry in Kampala, Uganda (median age: 26 years [23]). Participants were asked to visit a project clinic at 3-month intervals, where they were repeatedly interviewed and where specimens were collected to be tested for HIV, HSV2, syphilis, gonorrhea, chlamydia, T. vaginalis, Candida, and M. genitalium. M. genitalium specimens were taken by project clinic staff using endocervical swabs. Those reporting STI symptoms or testing positive for any STI other than M. genitalium (which was tested for ex-post) were treated promptly. Specimens were brought to a laboratory within 12 hours and stored at -20°C until tested for M. genitalium by PCR. Fig 1B summarizes results.
More-detailed information about the study protocols is available in the related, freely accessible publications [20–23].
Simulation model calibrated to the London-student data
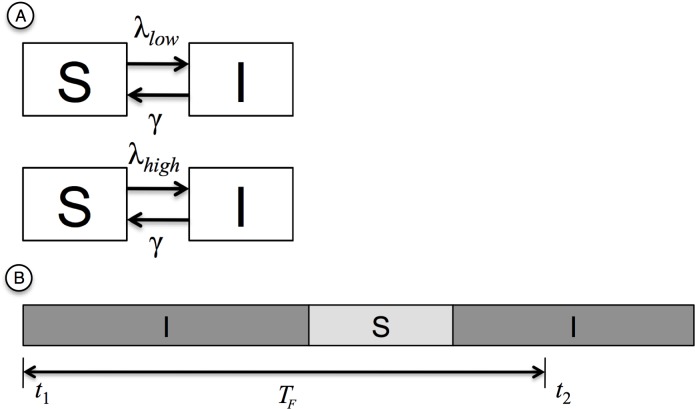
We represent individuals’ M. genitalium infection status with a Susceptible-Infected-Susceptible-type model, in which individuals are in one of two discrete states: Susceptible (S, uninfected) and Infected (I), as shown in Fig 2A. These are the same states as used in a typical statistical survival (time-to-event) analysis; however, our model has the important difference that we also allow for individuals to become (re-)infected over time. We assume the prevalence of M. genitalium-positive individuals is stable over time and, hence, also the force of infection or incidence rate (λ) is stable.
Fig 2. Schemata of model components.
(A) Schema of London-student model. S: Susceptible state; I: Infected state; λlow: incidence rate of low-risk group; λhigh: incidence rate of high-risk group; γ: recovery rate. (B) Schema of the succession of Infected and Susceptible states. S: Susceptible state; I: Infected state; t1: time at baseline; t2: time at follow-up; TF: time to follow-up; in this example, the individual was Infected at baseline and, again, at follow-up.
The transition S → I occurs with rate λlow for the London students with <2 partners in the previous year (low-risk group) and with rate λhigh for those with ≥2 partners (high-risk group), which are the groups reported by Oakeshott et al [20]. The transition I → S occurs with rate γ for all individuals. Hence, the infected period TI has a mean of γ-1 and it is exponentially distributed with exp(γ). The susceptible periods TS also follow exponential distributions with parameters λlow and λhigh, respectively. Individuals cycle between states S and I.
Our model aims at producing the overall best fit (maximum-likelihood) to six data items as in Fig 1A: the baseline prevalence in (1) the high-risk and (4) the low-risk group; the proportion of the initially infected individuals who were also infected at follow-up for (2) the high-risk and (5) the low-risk group; the proportion of those individuals whose initial M. genitalium test was negative that had a positive follow-up test for (3) the high-risk and (6) the low-risk group.
Prevalence
The probability PI,i that any given individual i is Infected at any time tx is given by λ/(λ+γ), with respective indices for low- and high-risk groups. Given the information about the prevalence in the low- and high-risk group (see Fig 1A), the log-likelihood functions are defined as
| (1) |
| (2) |
where L+ is the set of all study participants i who belonged to the low-risk group and tested positive for M. genitalium at baseline; L− is the set of all study participants j who belonged to the low-risk group, but had a negative initial test result; H+ and H− are the respective sets for the high-risk group.
Baseline versus follow-up measurements
The data in Fig 1A provide information about the infection status of all study participants at the baseline measurement, but also of many study participants at follow-up. The probability that individual i is Infected at time of follow-up, t2, depends on the infection status at baseline (i.e., at t1), the duration of the time period between baseline and follow-up measurement, TF, as well as on λlow, λhigh and γ.
Time to follow-up, TF, varied between study participants, and only the minimum, the maximum, and the median, μ1/2, are known for both the low- and the high-risk group (see Fig 1A). For any given individual i, TF is within interval [min, μ1/2] with a probability of 50% and within interval [μ1/2, max] also with a probability of 50%. In absence of further information about the distribution, we assume that TF follows a uniform distribution within each interval.
We determined the mean probability PI that an individual is Infected at follow-up–given the infection status at baseline and whether the individual belongs to the high- or low-risk group–stochastically, by cycling through Infected and Susceptible states until t2 is passed (Fig 2B). The infection status at time t2 determines the infection status at follow-up. For each set of parameters, the estimate of PI is based on at least 106 realizations, and in areas of the parameter space with a high likelihood, we used up to 107 realizations.
The likelihood functions Lbaseline+,low, Lbaseline+,high, Lbaseline–,low, and Lbaseline–,high are defined analogous to Eqs 1 and 2, using the mean probability of being infected at t2 as described above.
Combined log-likelihood function and parameter space
The combined log-likelihood is defined as
| (3) |
We established the likelihood landscape for a parameter space defined by vector for the intervals λlow in [0.0050, 0.0500] with a step width of 10−4, γ in [0.01, 4.00] with a step width of 0.01, and λhigh/λlow in [2.5, 3.5] with a step width of 0.1.
The parameter combination with the highest overall log-likelihood value represents with maximal likelihood the ‘true’ recovery and incidence rates, given that the underlying model is a good representation of the ‘real’ infection and clearance processes. We refer to this parameter combination as maximum likelihood estimate (MLE).
Sensitivity analyses
Having incomplete information means that we have to make some assumptions, e.g., the exact distribution of the time to follow-up. We examined scenarios to analyse how two key assumptions affect our results.
Time to follow-up: We assume that the time lag between the baseline and the follow-up measurements is uniformly distributed between the minimum and median as well as between the median and the maximum. For the sensitivity analysis, we define two other, extreme scenarios: one scenario, where TF = min with a probability of 50% and TF = μ1/2 with probability 50%; and an alternative scenario, where TF = μ1/2 or TF = max, both with a probability of 50%.
Partnership duration: We do not have any information about partnership durations, and, hence, our model does not incorporate the effects of stable sexual partnerships on infection transmission dynamics. In monogamous, stable partnerships, the risk of acquiring infections is either considerably elevated above the population average (if the partner is infected) [24] or non-existent (if the partner is not infected), compared to a situation with frequent casual partnerships (and no stable partnership). To assess the potential bias introduced by our assumption, we analyze how our results would differ, if we were to assume that all individuals of the low-risk group with two consecutive positive tests were in a stable partnership and became reinfected within this partnership; in our modeling framework, these cases could not contribute to the estimation of the recovery rate and so are excluded in the sensitivity analysis.
Model calibrated to Ugandan sex workers, including test sensitivity
In the study of sex workers in Uganda [21–23], sample-storage conditions and the type of specimens collected might have reduced sensitivity of testing relative to the London study [20], and we tested if this might be an explanation for the results having been different. We model both (i) the clearance of and recurrent infection with M. genitalium among the Ugandan sex-worker population–analogous to the model of the London students–and (ii) the detection of infection, allowing for false-negative test results. No information about differing levels of sexual activity are available and, hence, no further subdivision into risk groups is performed.
Prevalence
The observed prevalence from the participants’ first clinic visit is modeled–analogous to the London student study–as
| (4) |
where Psens denotes the test sensitivity and can take any value between 0 (i.e., the test does not detect any of the truly infected cases) and 1 (i.e., the test detects all infected cases and so produces no false-negative results). Set I includes all study participants who were infected as the first clinic visit, set S includes the complement.
Clearance
We model the expected distribution of the clinic visit at which the first negative test result occurred. A negative test result can be due to clearance (analogous to the London student model, see Fig 2B), or due to a false-negative test results. We model clearance and recurrent infection as for the London students, but record false-negative results with probability 1–Psens for every clinic visit where the simulated individual is infected.
We repeated this procedure 5∙106 times and obtained stochastic estimates for the probabilities P2, P3, P4 and P5 that any given individual had her first negative test result at the respective clinic visit, as well as for the probability Pno that an individual didn’t have a negative result throughout the entire duration of the study (i.e., consistently tested positive). This allows us to define a log-likelihood function for the clearance of M. genitalium:
| (5) |
Consistency with London-student data
We tested if we could construct a model (overall log-likelihood functions was the sum of Eqs 4 and 5) using recovery rate estimates from the London-student data and which is consistent with the Ugandan sex-worker data (α level of 0.05) if we vary the relative testing sensitivity in the Ugandan study to obtain the best fit to the empirical data.
We tested consistency using the following recovery rates from the London-student data:
γ, the maximum-likelihood estimate (MLE);
γUCL, the upper bound of the 95% confidence interval (CI) of the MLE;
γmax, the highest possible recovery rate, for which the outcomes of the London-student model are not significantly different from the London-student data (α level of 0.05);
γstable,max, the highest possible recovery rate, when we assumed that all low-risk students, who were positive at baseline and follow-up, were in stable partnerships.
Recurrent infection in Ugandan sex workers
We further analyzed which of the parameter sets (consisting of incidence and recovery rate as well as sensitivity) are consistent with apparently-recurrent infections that were observed in the Ugandan sex workers: 39% of the women who seemed to have cleared infection (i.e. tested negative after previously testing positive) tested positive again within 3 to 6 months [21].
We used our model of the Ugandan sex workers to determine how likely a sequence of positive-negative-positive results in successive tests is for the 109 women who had a negative test result at the 2nd, 3rd, or 4th clinic visit. We then used a binomial test (two-sided) to determine if the parameter-model combination is consistent with the observed 39% recurrent infections.
Confidence intervals and consistency
Confidence intervals for MLEs
We determined 95% confidence intervals for all MLEs with likelihood-ratio tests. The confidence interval is, hence, defined by
| (6) |
where is the MLE, θ is any other parameter vector, and crit. is a critical value. Since the likelihood-ratio statistic follows approximately the χ2 distribution, we obtain the critical value for an α-level of 0.05 from this distribution.
Consistency between data and model
For all data items where the outcome was dichotomous (i.e., Infected versus Susceptible), we used a binomial test (two-sided) to determine if a specific parameter-model combination could possibly produce the observed data. If a parameter set produces results that are significantly different (α-level of 0.05) from any observed data item, we deem the respective parameter set as inconsistent with the data.
One data item from the Ugandan sex worker study–the clinic visit when the participant had her first negative test result, if at all–is represented as a contingency table. Statistical difference between the observed data and the expected model outcome was evaluated with the G-test (α-level of 0.05).
Results
Overview of results
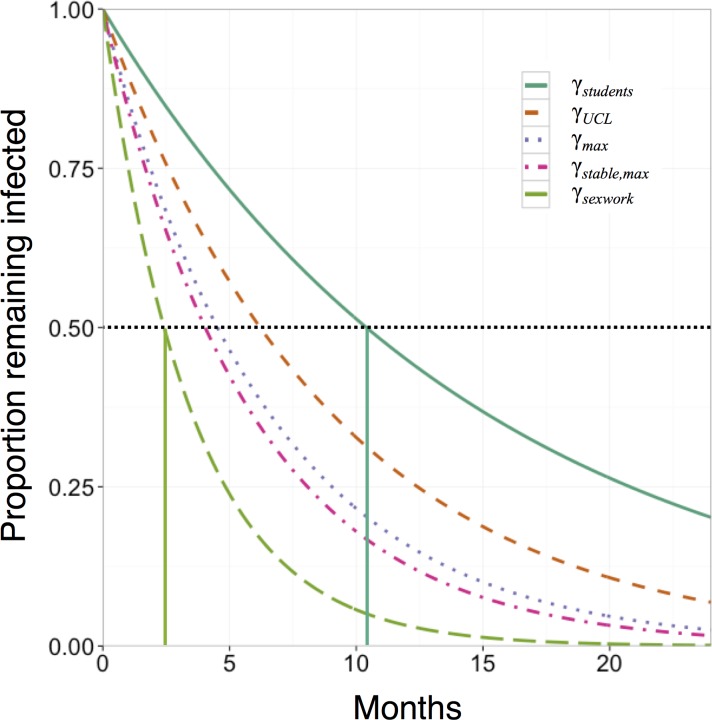
We present expected infection durations corresponding to the various estimates of clearance rate (from the two studies under different assumptions) in Fig 3, and describe the details of the analyses below.
Fig 3. Duration of infection.
Proportions of individuals remaining infected over time are shown for the various estimates of clearance rates, γstudents = 0.80p.a., γUCL = 1.34p.a., γmax = 1.84p.a., γstable,max = 2.06p.a. (all based on the London-student data), and γsexwork = 3.44p.a. (based on the Ugandan sex-worker data); vertical lines mark time points when, on average, half of the initially infected individuals will have cleared the infection, depending on the respective recovery rate.
Parameter estimates for the London-student data
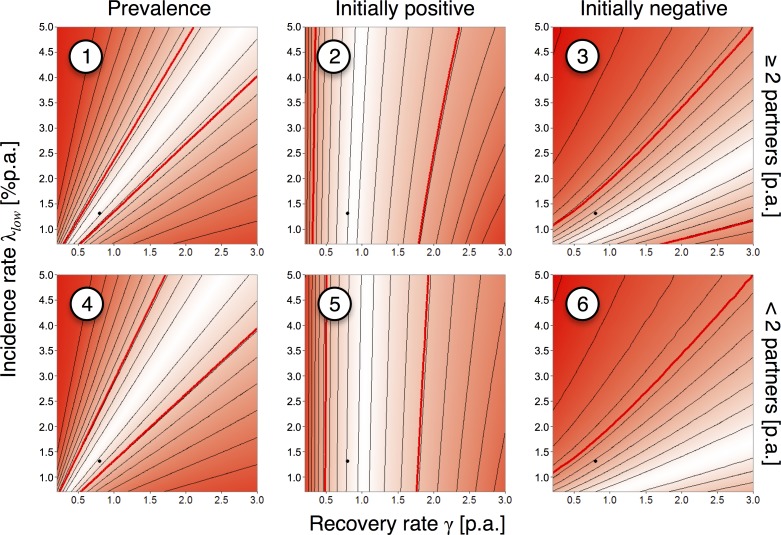
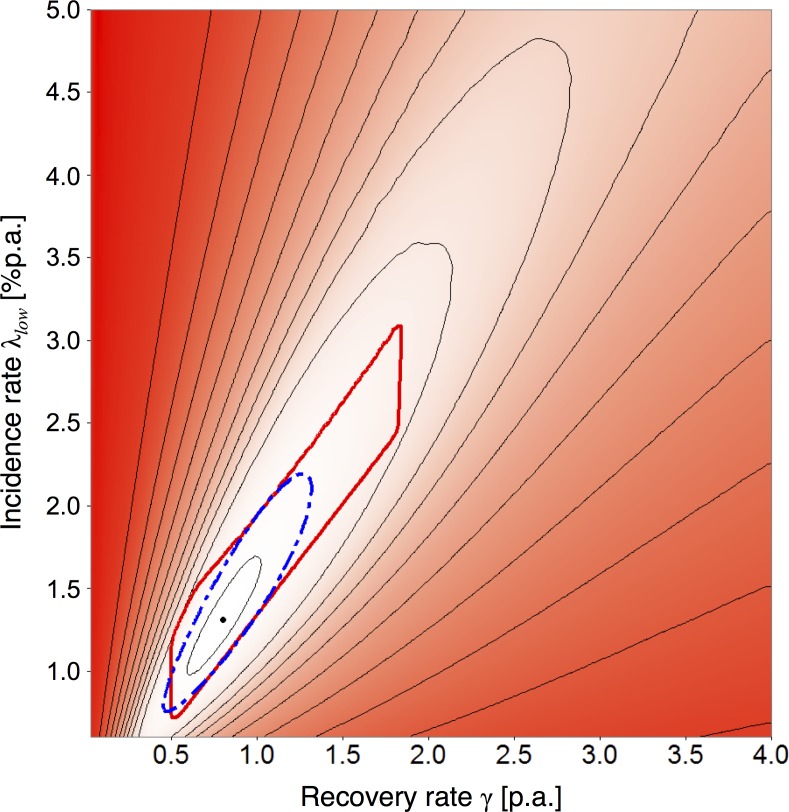
The best-fitting parameter combination, using all the available data items, is a recovery rate (γ) of 0.80p.a. (95% CI: 0.45–1.34; mean duration of infection of 15 months), with corresponding incidence rates, λlow = 1.31%p.a. (95% CI: 0.75%-2.25%) and λhigh = 3.93%p.a. (95% CI: 2.25%-6.75%), since the most likely λhigh/λlow is 3.0 (Figs 4 and 5). For comparison, Oakeshott et al.’s [20] estimated incidence was 0.9% (95% CI: 0.5%-1.6%). However, a very wide range of parameter values are compatible with (i.e., not significantly different from) the empirical data (area within red contour lines, Fig 5). The maximal recovery rate (γmax) for which the model outcomes are not significantly different from the empirical data is 1.84p.a. (mean duration ~6.5 months).
Fig 4. Likelihood landscapes by data item, London students.
Upper and lower rows of the panels correspond, respectively, to the high-risk group (≥2 partners in the preceding year at baseline) and low-risk group (<2 partners); columns of the panels correspond to the prevalence at baseline, the proportion of positive tests at follow-up among the initially M. genitalium-positive participants, and the proportion of positive test at follow-up among the initially negative participants. Numbering corresponds to Fig 1A; black dots: overall maximum-likelihood estimate (MLE) for the recovery (γ = 0.80p.a.) and the incidence rates (λlow = 1.31%p.a.); the ratio λhigh/λlow was fixed at the MLE of 3.0; thin, black contours: equal likelihood; colored areas: white indicates maximum likelihood, red indicates low likelihood; thick, red contours: parameter area where the model is consistent with the empirical data (α<0.05).
Fig 5. Recovery rate vs. incidence rate, maximum-likelihood estimate and plausible parameter range, London students.
Black dot: maximum-likelihood estimate (MLE) for the recovery rate (γ = 0.80p.a.) and the incidence rate (λlow = 1.31%p.a.); the ratio λhigh/λlow was fixed at the MLE of 3.0; thin, black contours: equal likelihood; combined likelihood for all six data items (see Fig 4); colored areas: white indicates maximum likelihood, red indicates low likelihood; thick, dashed, blue contour: 95% CI of the MLE; thick, red contour: parameter area where the model is consistent with the empirical data (α<0.05).
Fig 4 shows the likelihood landscape for all six data items from Fig 1A separately. The parameters λ and γ are tightly linked in the cases of prevalence (1 and 4) and infection of initially uninfected participants (3 and 6): high λ requires high γ to reproduce the data; low λ requires low γ. The slope of the most likely parameter range is steeper for items 1 and 4 than for items 3 and 6. The MLE for γ is predominantly driven by the data on the number of initially M. genitalium-positive participants who were still positive at the time of the follow-up (items 2 and 5).
The estimates are rather insensitive to changes in the assumed distribution of times to follow-up. In the scenario using the longest times that were consistent with the reported minimum, maximum, and median yields γh = 0.75p.a. (95% CI: 0.44–1.23) and λh,low = 1.24%p.a. (95% CI: 0.74%-2.10%). In the scenario using the shortest times, γl = 0.86p.a. (95% CI: 0.51–1.5) and λl,low = 1.46%p.a. (95% CI: 0.86%-2.52%).
If we assume that all low-risk individuals who were positive both at baseline and follow-up were potentially reinfected within a stable partnership, and therefore removed from the analysis, then the best estimate for the recovery rate shifts to γstable = 1.34p.a. (95% CI: 0.66–2.18) with λstable,low = 2.17%p.a. (95% CI: 1.08%-3.00%), but the highest possible recovery rate that was consistent with all six data items was only γstable,max = 2.06p.a., which corresponds to a mean duration of infection of ~5.8 months.
Clearance of M. genitalium infection in Ugandan sex workers
Clearance of M. genitalium in the Ugandan sex-worker cohort appeared to be relatively fast, compared with to the London-student cohort: a simple analysis, fitting an exponential curve to the five data points suggests a recovery rate γ = 3.14p.a., corresponding to a mean duration of infection of ~3.8 months.
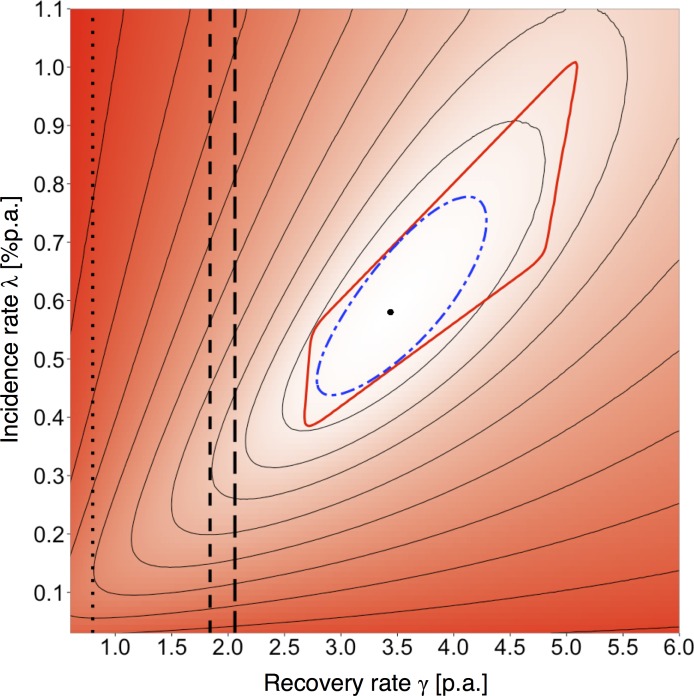
Fig 6 shows the results of a model fit, where we aimed at producing the best fit to the initial prevalence and the apparent clearance as in Fig 1B. The best-fitting parameter combination is γ = 3.44p.a. (95% CI: 2.78–4.29); λ = 58%p.a. (95% CI: 44%-78%). Neither the confidence intervals, nor the plausible parameter ranges for the London-student (γmax = 1.84p.a.) and the Ugandan sex-worker (γmin = 2.67p.a.) models overlap, suggesting that additional factors need to be incorporated in the model to explain both datasets with one common recovery rate.
Fig 6. Recovery rate vs. incidence rate, maximum-likelihood estimate and plausible parameter range, Ugandan sex workers.
Black dot: maximum-likelihood estimate (MLE) for the recovery rate (γ = 3.44p.a.) and the incidence rate (λlow = 58%p.a.); thin, black contours: equal likelihood; colored areas: white indicates maximum likelihood, red indicated low likelihood; thick, dashed, blue contour: 95% CI of the MLE; thick, red contour: parameter area where the model is consistent with the empirical data (α<0.05); vertical lines: estimates from London-student data; dotted: maximum-likelihood estimate (γ = 0.80p.a.); short-dashed: highest plausible estimate (γmax = 1.84p.a.); long-dashed: highest plausible with stable partnership assumption (γstable,max = 2.06p.a.).
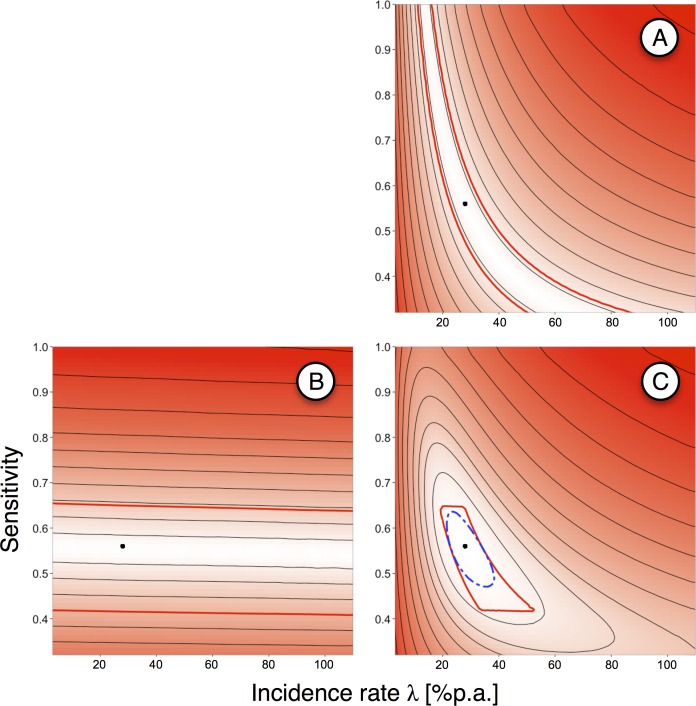
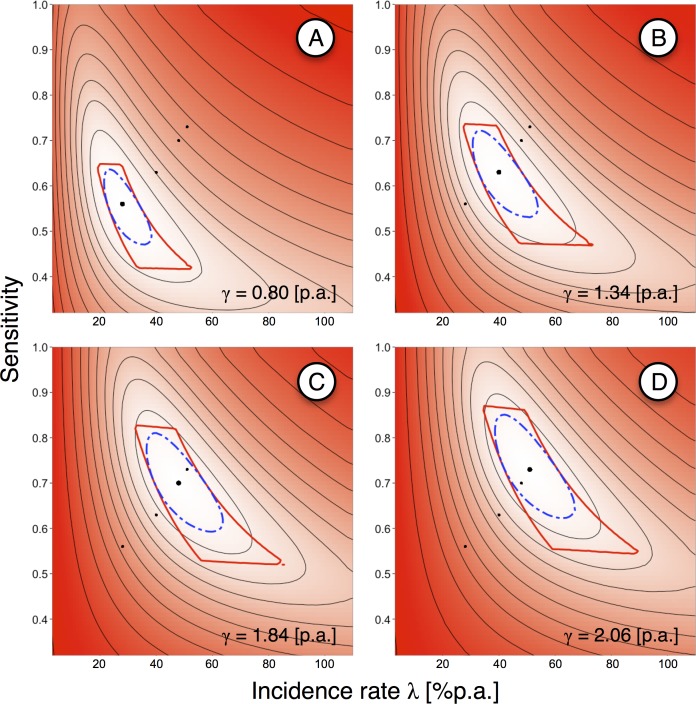
Since one explanation for the apparent differences between the studies in clearing M. genitalium might be lower testing sensitivity in the Vandepitte et al. study [21], due to different swabbing sites and sample handling, we varied the sensitivity to see if this could ‘reconcile’ the observed patterns (cf. Fig 7). Fig 8 shows sensitivity and incidence estimates for various recovery rates that were derived from the London-student model. For γ = 0.80p.a., the best fitting parameter combination was λ = 28%p.a. (95% CI: 22%-38%) with a sensitivity of 56% (95% CI: 47%-63%). The highest relative sensitivity that is consistent with the data is 64%. For γstable,max = 2.06p.a. (i.e., the highest plausible recovery rate in the scenario where all seemingly-persistent infections in the low-risk student group were due to reinfection within a stable partnership), the MLE for the sensitivity is 73% (95% CI: 63%-85%), and the highest plausible sensitivity is 86%.
Fig 7. Incidence rate vs. sensitivity, maximum-likelihood estimate and plausible parameter range, Ugandan sex workers.
(A) Initial prevalence. (B) continuously M. genitalium-positive participants over time. (C) Both data items combined. Thick, black dot: maximum-likelihood estimate (MLE) for the incidence rate (λlow = 28%p.a.) and sensitivity (56%) with recovery rate fixed at γ = 0.80p.a. (from London-student data); thin, black contours: equal likelihood; colored areas: white indicates maximum likelihood, red indicated low likelihood; thick, dashed, blue contour: 95% CI of the MLE; thick, red contour: parameter areas where the model is consistent with the empirical data (α<0.05).
Fig 8. Incidence rate vs. sensitivity, maximum-likelihood estimates and plausible parameter ranges for different recovery rates, Ugandan sex workers.
Recovery rates, γ, all from London-student data. (A) maximum-likelihood estimate, γ = 0.80p.a. (B) upper bound of 95% confidence interval, γUCL = γstable = 1.34p.a. (C) highest possible estimate, γmax = 1.84p.a. (D) highest possible estimate when assumed stable partnerships were excluded, γstable,max = 2.06p.a. Thick, black dots: MLEs for incidence rate and sensitivity with fixed recovery rates; thin, black dots: maximum-likelihood estimates (MLEs) for the other recovery rates; thin, black contours: equal likelihood; colored areas: white indicates maximum likelihood, red indicated low likelihood; thick, dashed, blue contour: 95% CI of the MLE; thick, red contour: parameter areas where the model is consistent with the empirical data (α<0.05).
Vandepitte et al. [21] report that “39% of the women who cleared the infection re-gained positive samples again within 3 to 6 months. Some of these recurrent infections could have been persistent infections after a previous false-negative result”; this reported percentage is consistent with our estimate of that study’s sensitivity, and with γ = 0.80p.a., the clearance rate which best explains information from both cohort studies. Higher clearance rates combined with higher sensitivities resulted in substantially lower percentages of participants expected showing this pattern, and they were significantly different from the observed figure and, hence, inconsistent with the empirical data.
Discussion
We aimed to improve estimates of the recovery and incidence rates of M. genitalium from cohort studies. Whilst incidence of infection and rates of antibiotic treatment are dependent upon context and patient behavior, and, hence, may vary markedly between studies, rates of natural clearance are likely to be less variable. Estimation of the clearance rate requires adjusting for other factors that are particular to each study setting.
Factors which impact on clearance rate estimates
There are several factors that might have affected our estimates.
Study protocols
Oakeshott et al. [20] used self-taken vaginal swabs and Vandepitte et al. [21] used staff-taken endocervical swabs. Previous studies suggest that vaginal swab specimens have a higher relative sensitivity than endocervical swab specimens [25,26], and that self-obtained specimens appear to be of similar quality as specimens collected by trained staff [25].
Furthermore, Oakeshott et al. [20] stored samples at lower temperatures than Vandepitte et al. [21]: -80°C compared with initial storage at 4°C (up to 12 hours) followed by -20°C for more than two years before they were tested for M. genitalium. Others have reported that DNA degradation might be slower at -80°C than -20°C [27], affecting test sensitivity.
Also, other factors, such as the transport media, DNA extraction methods, and PCR test kits might have influenced clearance rate estimates. A thorough assessment as to how exactly these differences might have had an impact on test sensitivity cannot be provided at this time, as they have not been studied or findings have not been published, so far.
In light of the discussed protocol differences, we would expect more false-negative test results in the Ugandan study, which would bias parameter estimates towards shorter infection periods because individuals were no longer considered in the published data after their first negative test result. This is corroborated by the agreement of our model results with the frequency of positive-negative-positive results for consecutive time-points, as reported by Vandepitte et al. [21].
A consequence of low relative sensitivities in the Ugandan study is also a higher prevalence than the crude estimate of 14.4%. The highest relative sensitivity estimate compatible with the data is 64%, and the maximum-likelihood estimate is 56%; using these estimates increases the prevalence estimate to 22.5% and 25.7%, respectively. These estimates are consistent with M. genitalium prevalence estimates for female sex worker populations in developing countries, which were up to 33.5% in Honduras [28] and 26.3% in Ghana and Benin [29].
Unintentional treatment
Neither cohort study provided treatment specifically for M. genitalium. However, individuals with symptomatic infection might have been treated presumptively, and those who were co-infected with another bacterial STI, particularly C. trachomatis or N. gonorrhoeae, were given treatment for the co-infection, which might have cured them of M. genitalium.
Vandepitte et al. reported treating participants with antibiotics, including doxycycline, ciprofloxacin, ceftriaxone, and metronidazole [21]. Doxycycline has a reported cure rate for M. genitalium of 17%-94% [30]. A wide range of antibiotics are effective or partly effective against at least some M. genitalium strains [31,32]. Therefore, treatment for non-STI infections might also have unintentionally cleared M. genitalium. However, Vandepitte et al. did not detect a higher clearance rate in co-infected participants and reported that they did not detect an association between clearance of M. genitalium and receipt of antibiotics [21].
Although any effect may have been marginal, we expect that unintentional treatment of M. genitalium would have been more frequent in the Ugandan study, since there was frequent STI testing and treatment [22]. Furthermore, STI co-infection was more common among Ugandan sex workers than London students, particularly for N. gonorrhoeae, which occurred in 20.9% of M. genitalium-positive samples from Ugandan sex workers, whilst no co-infection was detected in the London students. In the London study at baseline 10% of M. genitalium infections were co-infected with C. trachomatis compared to 12% in the Ugandan study. Due to the difference in N. gonorrhoeae co-infection, any effect of unintentional treatment of M. genitalium will have likely been smaller in the London study.
Sexual behavior
For C. trachomatis, it is thought that subclinical infections can be transmitted back and forth between partners in a steady sexual relationship without being detected and treated [33,34]. Since M. genitalium infections are frequently asymptomatic [20,35], repeated reinfection within stable partnerships (potentially with several cycles of recovery and reinfection) might be an important cause of apparently-persistent infection within an individual when the interval between testing is relatively long, as in the London study. (The authors reported that genotyping suggested patients testing positive at baseline and follow-up had persistent infections, but these results are also consistent with recovery and reinfection within stable partnerships.) This would bias our estimates towards lower recovery rates (i.e., longer infection duration) and lower incidence estimates.
Biological differences
The London and Uganda cohorts will have differed in their ethnic composition, with the former being more ethnically diverse [20]. People of different ethnicities might have genetic or other biological differences affecting effectiveness of drug treatments [36] or susceptibility to certain infections [37]. Women of African descent might differ from white women in their immune response to bacterial STIs related to PID [38,39]. Finally, the strains of M. genitalium in the two populations might have had different phenotypes. However, we have no direct evidence for biological differences and the results of our analyses suggest that any such differences are unlikely to have a substantial impact on the two studies.
Parts of the Uganda cohort were infected with HIV, but Vandepitte et al. [21] found no association between clearance rates of M. genitalium and HIV status per se. Only those HIV-positive participants with a very low CD4 count (<350/ml) had a slower clearance rate than HIV-negatives. With only 16 such individuals in the cohort, modeling this group explicitly will have had little impact on our estimates.
Interpretation of results
Infection duration in the London-student data appeared to be long (mean duration 15 months), whereas in the Ugandan sex-worker cohort more than half of the initially M. genitalium-positive participants appeared to have cleared the infection after three months (Fig 3).
We tested the importance of incomplete information by comparing the results of scenarios using different assumptions. Uncertainty in the timing of follow-up testing in the London study makes relatively little difference to estimates, whilst scenarios regarding reinfection result in potentially substantial differences. We identified partnership duration as well as the temporal gap until reinfection within a partnership occurs as critical factors affecting the recovery rate estimate; both are unknown. The basic model for the London data (which ignores partnership duration) might have overestimated the infection duration, but the corresponding MLE also explained recurrent infection in the Ugandan sex workers best. The Ugandan data most likely suggests too-short durations of (untreated) infection because of unintentional treatment of M. genitalium in co-infected individuals, and probably reduced test sensitivity due to long-term sample storage at -20°C (and, potentially, the choice of transport media or DNA extraction method) and the use of endocervical instead of vaginal swabs. Possibly–although Vandepitte et al. did not detect an effect–unintentional treatment of M. genitalium in co-infected individuals might have played a minor role.
Incorporating the effects of (i) reinfection within stable partnerships in the London students and (ii) expected lower test sensitivity in the Ugandan sex-worker study in the model result in a common recovery rate to be plausible. Including all available information, the ‘true’ clearance rate appears to be close to the best estimate for the London-student data. Interestingly, both the London-student and the Ugandan sex-worker data are inconsistent with the findings of Tosh et al. [40], who reported that among adolescent women in the USA “31.3% of untreated M. genitalium cases had infection lasting over 8 weeks”, suggesting a mean duration of <2 months–i.e., a recovery rate >6p.a., which is outside the plausible ranges of both the London-student and the Ugandan sex-worker model. Long-term storage (up to 2 years, although at -70°C) and treatment of co-infections (15/52 M. genitalium-positive women tested positive for C. trachomatis and were treated [40]) might have contributed to this high apparent recovery rate (drug resistance in M. genitalium may have been lower at the time of the study enrollment, 1999–2006, than more recently [7]), but the difference from the other two studies is not fully understood. An in vitro study also suggests that infection may be prolonged [41].
Future research needs
M. genitalium is causing increasing concern, particularly regarding if and how it should be managed at the population level, including whether there should be screening or targeted testing [7,9,13,16,17]. Robust parameter estimates are needed for improved understanding of M. genitalium epidemiology, to inform public health policy, including assessment of cost-effectiveness of intervention strategies.
To better understand the epidemiology of M. genitalium, we need robust knowledge about fundamental natural-history parameters [17,30,42], including the duration of untreated infection [10], for reliably identifying groups of individuals that are more likely to contract new infections and/or that are more likely to transmit infection to others [43]. (In Britain, 66% of individuals aged 16–44 years who were infected with Chlamydia had not been tested in the last year [44], making the duration of untreated infection an important determinant of transmission.) There is still considerable uncertainty in rates of sequelae due to C. trachomatis [18], contributing to continuing uncertainty in cost-effectiveness of screening for that infection [16,30]; we suggest that corresponding knowledge gaps for M. genitalium should be addressed before decision are taken.
Future studies would ideally have larger numbers of initially M. genitalium-positive participants, followed-up sufficiently frequently to detect changes on timescales of a few weeks [40]. Specimens should be collected from the vagina and from the cervix, if possible, as this results in higher sensitivity [25,26].
Further, ideally, all factors mentioned in the previous section would be controlled for. Collecting more detailed information on sexual behavior and antibiotic use (e.g., Walker et al. [10]) would greatly enhance the value of cohort studies. As we have shown, to estimate the duration of infection, it is important to have information on the incidence (which can lead to recurrent infection) at the individual level, as it is highly heterogeneous: persons in a stable sexual partnership with an infected partner experience a high incidence, typically greater than persons who have frequent casual partnerships (but no stable partner), whilst those in an uninfected mutually monogamous partnership have no infection risk. Estimating natural clearance rates requires accounting for antibiotic treatment, including unintentional treatment (e.g., for coinfections).
Finally, as M. genitalium is a sexually-transmitted infection which infected women typically acquire from men, it is important to better understand its natural history in males; further studies are required.
Acknowledgments
TS and PJW thank Pippa Oakeshott and Sarah Kerry for providing additional information. We also thank the anonymous reviewers and academic editors for their helpful comments.
Data Availability
All relevant data are within the paper.
Funding Statement
This work was supported by the UK National Institute for Health Research Health Protection Research Unit (NIHR HPRU) in Modelling Methodology at Imperial College London in partnership with Public Health England (PHE) [grant number HPRU-2012-10080;http://www.nihr.ac.uk] and by the UK Medical Research Council for Centre funding [grant number MR/K010174/1; http://www.mrc.ac.uk]. The funders had no role in study design, data analysis, decision to publish, or preparation of the manuscript. The views expressed are those of the authors and not necessarily those of the MRC, NHS, the NIHR, the Department of Health, or Public Health England.
References
- 1.Workowski KA, Berman SM. Centers for Disease Control and Prevention Sexually Transmitted Disease Treatment Guidelines. Clin Infect Dis. 2011; 53: S59–S63. 10.1093/cid/cir694 [DOI] [PubMed] [Google Scholar]
- 2.Taylor-Robinson D, Jensen JS. Mycoplasma genitalium: from chrysalis to multicolored butterfly. Clin Microbiol Rev. 2011; 24: 498–514. 10.1128/CMR.00006-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Horner P, Thomas B, Gilroy CB, Egger M, Taylor-Robinson D. Role of Mycoplasma genitalium and Ureaplasma urealyticum in acute and chronic nongonococcal urethritis. Clin Infect Dis. 2001; 32: 995–1003. [DOI] [PubMed] [Google Scholar]
- 4.Manhart LE, Critchlow CW, Holmes KK, Dutro SM, Eschenbach DA, Stevens CE, et al. Mucopurulent cervicitis and Mycoplasma genitalium. J Infect Dis. 2003; 187: 650–657. [DOI] [PubMed] [Google Scholar]
- 5.Svenstrup HF, Fedder J, Kristoffersen SE, Trolle B, Birkelund S, Christiansen G. Mycoplasma genitalium, Chlamydia trachomatis, and tubal factor infertility–a prospective study. Fertil Steril. 2008; 90: 513–520. [DOI] [PubMed] [Google Scholar]
- 6.Vandepitte J, Weiss HA, Bukenya J, Kyakuwa N, Muller E, Buvé A, et al. Association between Mycoplasma genitalium infection and HIV acquisition among female sex workers in Uganda: evidence from a nested case-control study. Sex Transm Infect. 2014; 90: 545–549. 10.1136/sextrans-2013-051467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Manhart LE. Diagnostic and resistance testing for Mycoplasma genitalium: what will it take? Clin Infect Dis. 2014; 59: 31–33. 10.1093/cid/ciu224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Le Roy C, Pereyre S, Bébéar C. Evaluation of two commercial real-time PCR assays for detection of Mycoplasma genitalium in urogenital specimens. J Clin Microbiol. 2014; 52: 971–973. 10.1128/JCM.02567-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Taylor-Robinson D. Diagnosis and antimicrobial treatment of Mycoplasma genitalium infection: sobering thoughts. Expert Rev Anti Infect Ther. 2014; 12: 715–722. 10.1586/14787210.2014.919220 [DOI] [PubMed] [Google Scholar]
- 10.Walker J, Fairley CK, Bradshaw CS, Tabrizi SN, Twin J, Chen MY, et al. Mycoplasma genitalium. Incidence, Organism Load, and Treatment Failure in a Cohort of Young Australian Women. Clin Infect Dis. 2013; 56:1094–1100. 10.1093/cid/cis1210 [DOI] [PubMed] [Google Scholar]
- 11.Manhart LE, Gillespie CW, Lowens MS, Khosropour CM, Colombara DV, Golden MR, et al. Standard treatment regimens for nongonococcal urethritis have similar but declining cure rates: a randomized controlled trial. Clin Infect Dis. 2013; 56: 934–942. 10.1093/cid/cis1022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mena LA, Mroczkowski TF, Nsuami M, Martin DH. A randomized comparison of azithromycin and doxycycline for the treatment of Mycoplasma genitalium-positive urethritis in men. Clin Infect Dis. 2009; 48: 1649–1654. 10.1086/599033 [DOI] [PubMed] [Google Scholar]
- 13.Salado-Rasmussen K, Jensen JS. Mycoplasma genitalium testing pattern and macrolide resistance: a Danish nationwide retrospective survey. Clin Infect Dis. 2014; 59: 24–30. 10.1093/cid/ciu217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jensen JS, Bradshaw CD, Tabrizi SN, Fairley CK, Hamasuna R. Azithromycin treatment failure in Mycoplasma genitalium-positive patients with nongonococcal urethritis is associated with induced macrolide resistance. Clin Infect Dis. 2008; 47: 1546–1553. 10.1086/593188 [DOI] [PubMed] [Google Scholar]
- 15.Pond MJ, Nori AV, Witney AA, Lopeman RC, Butcher PD, Sadiq ST. High prevalence of antibiotic-resistant Mycoplasma genitalium in nongonococcal urethritis: the need for routine testing and the inadequacy of current treatment options. Clin Infect Dis. 2014; 58: 631–637. 10.1093/cid/cit752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Horner P, Blee K, Adams E. Time to manage Mycoplasma genitalium as an STI: but not with azithromycin 1g! Curr Opin Infect Dis. 2014, 27: 68–74. 10.1097/QCO.0000000000000030 [DOI] [PubMed] [Google Scholar]
- 17.Daley GM, Russell DB, Tabrizi SN, McBride J. Mycoplasma genitalium: a review. Int J STD AIDS. 2014; 25: 475–487. [DOI] [PubMed] [Google Scholar]
- 18.Haggerty CL, Gottlieb SL, Taylor BD, Low N, Xu Fujie, Ness RB. Risk of sequelae after Chlamydia trachomatis genital infection in women. J Infect Dis. 2010; 201(S2): S134–S155. [DOI] [PubMed] [Google Scholar]
- 19.Davies B, Anderson S-J, Turner KME, Ward H. How robust are the natural history parameters used in chlamydia transmission dynamic models? A systematic review. Theor Biol Med Model. 2014; 11: 8 10.1186/1742-4682-11-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Oakeshott P, Aghaizu A, Hay P, Reid F, Kerry S, Atherton H, et al. Is Mycoplasma genitalium in women the ‘new chlamydia?’ A community-based prospective cohort study. Clin Infect Dis. 2010; 51: 1160–1166. 10.1086/656739 [DOI] [PubMed] [Google Scholar]
- 21.Vandepitte J, Weiss HA, Kyakuwa N, Nakubulwa S, Muller E, Buvé A, et al. Natural history of Mycoplasma genitalium infection in a cohort of female sex workers in Kampala, Uganda. Sex Transm Dis. 2013; 40: 422–427. 10.1097/OLQ.0b013e31828bfccf [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vandepitte J, Bukenya J, Weiss HA, Nakubulwa S, Francis SC, Hughes P, et al. HIV and other sexually transmitted infections in a cohort of women involved in high-risk sexual behaviour in Kampala, Uganda. Sex Transm Dis. 2011; 38: 316–323. [PMC free article] [PubMed] [Google Scholar]
- 23.Vandepitte J, Muller E, Bukenya J, Nakubulwa S, Kyakuwa N, Buvé A, et al. Prevalence and correlates of Mycoplasma genitalium infection among female sex workers in Kampala, Uganda. J Infect Dis. 2012; 205: 289–296. 10.1093/infdis/jir733 [DOI] [PubMed] [Google Scholar]
- 24.Manhart LE, Kay N. Mycoplasma genitalium: is it a sexually transmitted pathogen? Curr Infect Dis Rep. 2010; 12: 306–313. 10.1007/s11908-010-0114-3 [DOI] [PubMed] [Google Scholar]
- 25.Wroblewski JKH, Manhart LE, Dickey KA, Hudspeth MK, Totten PA. Comparison of transcription-mediated amplification and PCR assay results for various genital specimen types for detection of Mycoplasma genitalium. J Clin Microbiol. 2006; 44: 3306–3312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lillis RA, Nsuami MJ, Myers L, Martin DH. Utility of urine, vaginal, cervical, and rectal specimens for detection of Mycoplasma genitalium. J Clin Microbiol. 2011; 49: 1990–1992. 10.1128/JCM.00129-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Carlsen K, Jensen J. Mycoplasma genitalium PCR: does freezing of specimens affect sensitivity? J Clin Microbiol. 2010; 48: 3624–3627. 10.1128/JCM.00232-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Johnston LG, Paz Bailey G, Morales-Miranda S, Morgan M, Alvarez B, Hickman L, et al. High prevalence of M. genitalium among female sex workers in Honduras: implications for the spread of HIV and other sexually transmitted infections. Int J STD AIDS. 2012; 23: 5–11. 10.1258/ijsa.2009.009446 [DOI] [PubMed] [Google Scholar]
- 29.Pépin J, Labbé A- C, Khonde N, Deslandes S, Alary M, Dzokoto A, et al. Mycoplasma genitalium: an organism commonly associated with cervicitis among west African sex workers. Sex Transm Infect. 2005; 81: 67–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Manhart LE, Broad JM, Golden MR. Mycoplasma genitalium: should we treat and how? Clin Infect Dis. 2011; 53: S129–S142. 10.1093/cid/cir702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hamasuna R, Osada Y, Jensen JS. Antibiotic susceptibility testing of Mycoplasma genitalium by TaqMan 5' nuclease real-time PCR. Antimicrob Agents Chemother. 2005; 49: 4993–4998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Duffy LB, Crabb D, Searcey K, Kempf MC. Comparative potency of gemifloxacin, new quinolones, macrolides, tetracycline and clindamycin against Mycoplasma spp. J Antimicrob Chemother. 2000; 45: 29–33. [DOI] [PubMed] [Google Scholar]
- 33.Hosenfeld CB, Workowski KA, Berman S, Zaidi A, Dyson J, Mosure D, et al. Repeat infection with chlamydia and gonorrhea among females: a systematic review of the literature. Sex Transm Dis. 2009; 36: 478–489. 10.1097/OLQ.0b013e3181a2a933 [DOI] [PubMed] [Google Scholar]
- 34.Golden M, Whittington W. Effect of expedited treatment of sex partners on recurrent or persistent gonorrhea or chlamydial infection. N Engl J Med. 2005; 352: 676–685. [DOI] [PubMed] [Google Scholar]
- 35.Anagrius C, Loré B, Jensen JS. Mycoplasma genitalium: prevalence, clinical significance, and transmission. Sex Transm Infect. 2005; 81: 458–462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Burroughs V, Maxey R, Levy R. Racial and ethnic differences in response to medicines: towards individualized pharmaceutical treatment. J Natl Med Assoc. 2002; 94: 1–26. [PMC free article] [PubMed] [Google Scholar]
- 37.Stead W, Senner J, Reddick W, Lofgren JP. Racial differences in susceptibility to infection by Mycobacterium tuberculosis. N Engl J Med. 1990; 322: 422–427. [DOI] [PubMed] [Google Scholar]
- 38.Taylor BD, Darville T, Ferrell RE, Ness RB, Haggerty CL. Racial variation in toll-like receptor variants among women with pelvic inflammatory disease. J Infect Dis. 2013; 207: 940–946. 10.1093/infdis/jis922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Taylor BD, Darville T, Ferrell RE, Kammerer CM, Ness RB, Haggerty CL. Variants in toll-like receptor 1 and 4 genes are associated with Chlamydia trachomatis among women with pelvic inflammatory disease. J Infect Dis. 2012; 205:603–9. 10.1093/infdis/jir822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tosh AK, Van der Pol B, Fortenberry J, Williams JA, Katz BP, Batteiger BE, et al. Mycoplasma genitalium among adolescent women and their partners. J Adolesc Health. 2007; 40: 412–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.McGowin CL, Annan RS, Quayle AJ, Greene SJ, Ma L, Mancuso MM, et al. Persistent Mycoplasma genitalium infection of human endocervical epithelial cells elicits chronic inflammatory cytokine secretion. Infect Immun. 2012; 80: 3842–3849. 10.1128/IAI.00819-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Manhart LE, McClelland RS. Mycoplasma genitalium Infection in Sub-Saharan Africa: How Big Is the Problem? Sex Transm Dis. 2013; 40: 429–430. [DOI] [PubMed] [Google Scholar]
- 43.Smieszek T, Salathé M. A low-cost method to assess the epidemiological importance of individuals in controlling infectious disease outbreaks. BMC Med. 2013; 11: 35 10.1186/1741-7015-11-35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sonnenberg P, Clifton S, Beddows S, Field N, Soldan K, Tanton C, et al. Prevalence, risk factors, and uptake of interventions for sexually transmitted infections in Britain: findings from the National Surveys of Sexual Attitudes and Lifestyles (Natsal). Lancet. 2013; 382: 1795–1806. 10.1016/S0140-6736(13)61947-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper.