Abstract
Background and aim
The efficacy of CO2 insufflation during balloon-assisted enteroscopy remains controversial. This study aimed to perform a systematic review with meta-analysis of randomized controlled trials (RCTs) in which CO2 insufflation was compared with air insufflation in balloon-assisted enteroscopy.
Methods
PubMed, the Cochrane library, and the Igaku-Chuo-Zasshi database were searched to identify RCTs eligible for inclusion in the systematic review. Data from the eligible studies were combined to calculate the pooled odds ratios (ORs) or weighted mean differences (WMDs) with 95% confidence intervals (CIs).
Results
Four RCTs (461 patients) were identified. Compared with air insufflation, CO2 insufflation significantly increased intubation depth of oral enteroscopy (WMD: 55.2, 95% CI: 10.77–99.65, p = 0.015). However, there was significant heterogeneity. The intubation depth of anal enteroscopy showed no significant difference between the CO2 group and the air group. CO2 insufflation significantly reduced abdominal pain compared with air insufflation (WMD: −2.463, 95% CI: −4.452 to −0.474, p = 0.015), without significant heterogeneity. The PaCO2 or end-tidal CO2 level showed no significant difference between the CO2 group and air group.
Conclusions
Compared with air insufflation, CO2 insufflation during balloon-assisted enteroscopy caused less post-procedural pain without CO2 retention.
Keywords: Carbon dioxide, balloon-assisted enteroscopy, systematic review, meta-analysis
Introduction
In the past, the small bowel has been a blind spot for gastrointestinal endoscopy, as it has been only partially accessible with conventional endoscopes. Yamamoto et al. first described double-balloon enteroscopy in 2001, and single-balloon enteroscopy was developed in 2008.1,2 A recent multicenter randomized controlled trial (RCT) showed that the diagnostic yield and pain scores were similar in single-balloon and double-balloon systems.3 These balloon-assisted enteroscopies are now performed globally.
Insufflation of gas into the bowel is necessary to ensure adequate visualization. Air is still the standard gas used for insufflation during gastrointestinal endoscopy. Balloon-assisted enteroscopy is time-consuming and requires large volumes of insufflated air, leading to significant distention of the small bowel during and after the procedure. Unlike air, carbon dioxide (CO2) is rapidly absorbed from the bowel.4 Several RCTs have evaluated the efficacy of CO2 in balloon-assisted enteroscopy. Domagk et al. reported that CO2 insufflation was superior to air regarding intubation depth and level of patient discomfort.5 However, other studies produced inconsistent results.6–8 The number of patients enrolled in some trials has been too few to achieve statistically conclusive results. We proposed that systematically pooling data from all published reports might provide a better understanding of the efficacy of CO2 insufflation for balloon-assisted enteroscopy. Our objective was to perform a systematic review and meta-analysis of RCTs comparing the impact of CO2 versus air insufflation for balloon-assisted enteroscopy.
Methods
Before performing the meta-analysis, we developed a protocol to define search strategies, determine criteria for the selection of studies, and to identify methods for relevant data extraction, quality assessment, and statistical analysis.9
Search strategy
PubMed, the Cochrane library, and the Igaku-Chuo-Zasshi database in Japan (from 2001 to December 2014) were used to perform a systematic literature search. A combination of the following words was used for the search: (carbon dioxide) AND (enteroscopy). Articles published in any language were included.
Inclusion and exclusion criteria
Studies meeting the following criteria were eligible for inclusion: (1) study type: RCT; (2) population: patients who underwent single-balloon enteroscopy or double-balloon enteroscopy; (3) intervention: CO2 insufflation; (4) comparator: air insufflation; (5) outcome: efficacy and safety of CO2. Duplicate publications, reviews, and conference abstracts were excluded.
Outcome measures
The primary outcome for this study was intubation depth. The secondary outcome was the degree of abdominal pain measured along a visual analogue scale (VAS) ranging from 0 to 100 mm and CO2 gas retention after balloon-assisted enteroscopy.
Data extraction
Standardized data abstraction sheets were prepared. Extracted data included study design, study quality, intervention, and outcomes. Two reviewers (TN and AF) independently examined all articles for eligibility. Disagreements were resolved by consulting a third reviewer (HS).
Assessment of methodological quality
The methodological quality of each study was assessed using the risk-of-bias tool outlined in the Cochrane Handbook for Systematic Reviews of Interventions (version 5.1.0).10 Two reviewers (TN and HS) evaluated all studies and assessed six key RCT quality influencers: sequence generation, allocation concealment, blinding of participants and outcome assessors, management of incomplete outcome data, completeness of outcome reporting, and other potential threats to validity.
Statistical analysis
Data were entered into the StatsDirect statistical package (StatsDirect Ltd., Cheshire, UK). Separate analyses were performed for each outcome using an odds ratio (OR) or weighted mean difference (WMD) with 95% confidence intervals (CIs).11 We always used a random-effect model, regardless of the significance of the heterogeneity.12,13 Heterogeneity between studies was assessed by Cochran’s Q and I2 tests. Because of the low power of the Q test, a cut-off value (<0.10) was used to reject homogeneity, which thereby indicated heterogeneity. An I2 score of ≥50% indicates more than moderate heterogeneity. Some trials reported means as the measure of treatment effect, with an accompanying standard error (SE) or 95% CI. For the purpose of our analysis, standard deviation (SD) was estimated from the SE, and 95% CI as follows: SD = SE × square root of n; SD = 95% CI range × square root of n/3.92. Finally, we used funnel plot asymmetry to detect any publication bias in the meta-analysis and Egger’s regression test to measure funnel plot asymmetry.14,15
Results
Search results
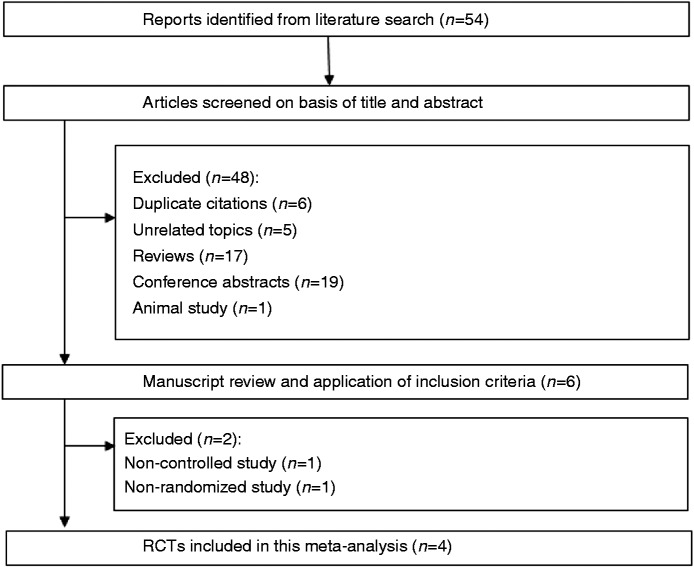
Our database search yielded 54 citations (Figure 1). After adjusting for duplicates, 48 studies remained. Of these, 42 studies were rejected based on exclusion criteria (five unrelated topics, 17 reviews, 19 conference abstracts, and one animal study). The remaining six studies were examined in detail. Two studies were then excluded (one for lack of a control group and one owing to lack of randomization). Finally, four studies were included in the systematic review and meta-analysis. The characteristics of these studies are summarized in Table 1.
Figure 1.
Flow of RCTs included in the systematic review.
Table 1.
Characteristics of studies included in the systematic review
| Author | Country | Enteroscopy | Sedation | Insufflation | Patients | Age | Gender | Oral | Anal |
|---|---|---|---|---|---|---|---|---|---|
| Year | number | ±SD | M/F | approach | approach | ||||
| Domagk | Germany | Double-balloon | Pethidine with | CO2 | 48 | 55.6 ± 18.7 | 28/20 | 30 | 18 |
| 2007 | Norway | Propofol or midazolam | air | 52 | 55.2 ± 21.3 | 27/25 | 29 | 23 | |
| Hirai | Japan | Double-balloon | Midazolam with | CO2 | 20 | 42.7 ± 17.9 | 13/7 | 2 | 18 |
| 2011 | Buprenorphine | air | 20 | 46.3 ± 18.2 | 15/5 | 3 | 17 | ||
| Lenz | Germany | Single-balloon | Propofol | CO2 | 52 | 56.5 ± 17.9 | 23/29 | 48 | 32 |
| 2014 | Italy | ±Pethidine | air | 55 | 56.7 ± 17.6 | 30/25 | 50 | 39 | |
| Li | China | Single-balloon | General anesthesia | CO2 | 106 | 41.2 ± 14.3 | 65/41 | 19 | 14 |
| 2014 | air | 108 | 40.5 ± 17.6 | 60/48 | 16 | 14 |
Quality assessment
The risk of bias for the included RCTs is shown in Table 2. In general, the included RCTs were at low risk of bias for most of the aspects evaluated. One RCT did not describe the specific methods used for random sequence generation. All four RCTs performed allocation concealment, blinding of participants, and outcomes assessment. The four RCTs were also found to adequately assess incomplete outcomes, avoid selective outcome reporting, and were free of other biases.
Table 2.
Evaluation of bias of RCTs included in the systematic review
| First author | Random sequence generation | Allocation concealment | Blinding of participants and personnel | Blinding of outcome assessment | Adequate assessment of incomplete outcome | Selective reporting avoided | No other bias |
|---|---|---|---|---|---|---|---|
| Domagk | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Hirai | Unclear | Yes | Yes | Yes | Yes | Yes | Yes |
| Lenz | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Li | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
Yes: Low risk of bias.
No: High risk of bias.
Unclear: Unclear risk of bias.
Meta-analysis results
Intubation depth
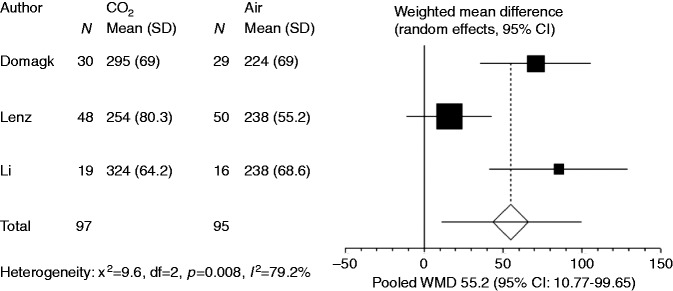
The intubation depth of oral enteroscopy was recorded in three studies. In two studies, intubation depth of oral enteroscopy was defined as intubation distal to the pylorus. In one study, the intubation depth was defined as intubation distal to the ligament of Treitz. Since the number of studies was limited, data that were obtained using different measurement methods were combined in the present meta-analysis. Compared with air insufflation, CO2 insufflation significantly increased intubation depth of oral enteroscopy (WMD: 55.2, 95% CI: 10.77−99.65, p = 0.015, Figure 2). However, there was also significant heterogeneity among the trial results (I2 = 79.2%, p = 0.008). Although Domagk et al.5 and Li et al.8 excluded cases with previous abdominal surgery or narrow strictures in proximal jejunum, Lenz et al.7 included patients with previous abdominal surgery. Lenz et al.7 reported that the oral insertion depth was significantly lower in patients with previous abdominal surgery than in patients without such a history. When we excluded Lenz et al.’s study, the heterogeneity disappeared (p = 0.62).
Figure 2.
Forest plot displaying the weighted mean difference (WMD) and 95% confidence intervals (95% CIs) of each study for the intubation depth of oral enteroscopy.
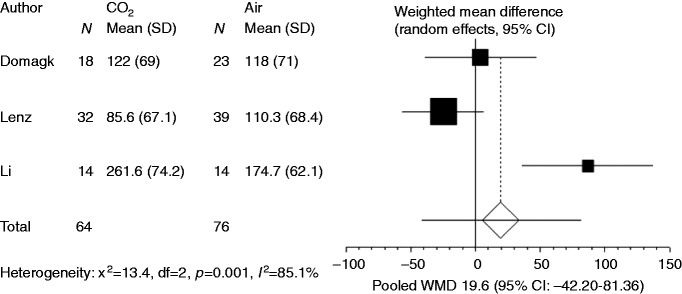
The intubation depth of anal enteroscopy was recorded in three studies. Intubation depth of anal enteroscopy was defined as proximal to the ileocecal valve. Pooling the results for anal enteroscopy showed no significant difference between the CO2 group and the air group (WMD: 19.58, 95% CI: −42.20 to 81.36, p = 0.535, Figure 3).
Figure 3.
Forest plot displaying the weighted mean difference (WMD) and 95% confidence intervals (95% CIs) of each study for the intubation depth of anal enteroscopy.
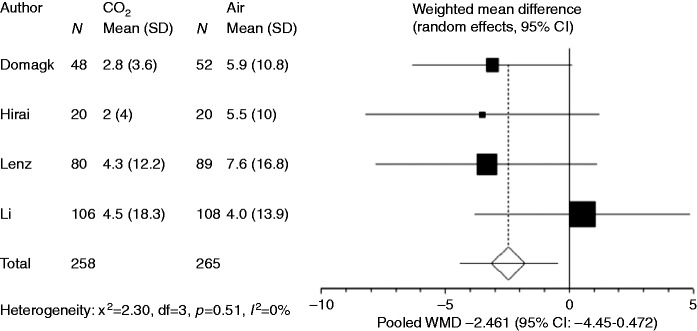
Abdominal pain
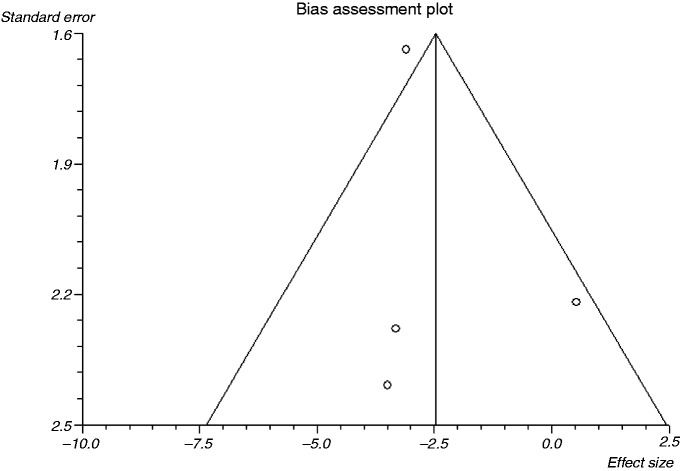
The degree of abdominal pain along a VAS at 1 and 3 h after balloon-assisted enteroscopy was recorded in all four studies. Although Li et al.8 described the mean VAS of each subgroup (oral route, anal route, and bilateral route group) in per-protocol analysis, the patient numbers of each subgroup in per-protocol analysis were not described. Instead, the patient numbers of each subgroup in the intention-to-treat analysis were used in this meta-analysis. Compared with air insufflation, CO2 insufflation significantly reduced VAS at 1 h after balloon-assisted enteroscopy (WMD: −2.461, 95% CI: −4.450 to −0.472, p = 0.015, Figure 4). There was no significant heterogeneity among the trial results (I2 = 0%, p = 0.51). Exclusion of Li et al.’s study did not significantly alter the outcome of the meta-analysis. The Egger test suggested no significant asymmetry of the funnel plot (p = 0.796), indicating no evidence of substantial publication bias (Figure 5). At 3 h after balloon-assisted enteroscopy, a trend towards abdominal pain reduction was shown in the CO2 group, but there was no significant difference between the CO2 group and air group (WMD: −1.009, 95% CI: −2.534 to 0.517, p = 0.195).
Figure 4.
Forest plot displaying the weighted mean difference (WMD) and 95% CIs of each study for abdominal pain score at 1 h after balloon-assisted enteroscopy.
Figure 5.
Funnel plot of the included studies for abdominal pain score at 1 h after balloon-assisted enteroscopy.
CO2 retention
Hirai et al.6 performed arterial blood gas analysis, and Li et al.8 recorded end-tidal CO2 after balloon-assisted enteroscopy. Both of these RCTs confirmed that CO2 levels did not differ significantly between the CO2 group and air group.
Discussion
This systematic review and meta-analysis indicates that CO2 insufflation significantly reduces abdominal pain after balloon-assisted enteroscopy.
Air insufflation during balloon-assisted enteroscopy unfortunately enhances bowel loops and reduces their ability to collapse onto the endoscope. Since CO2 is more rapidly absorbed from the gastrointestinal tract, CO2 would facilitate deeper bowel intubation. Soria et al. reported that CO2 insufflation improved intubation depth during double-balloon enteroscopy in the experimental animal study.16 This meta-analysis showed that CO2 insufflation improves intubation depth for oral enteroscopy. It is worth noting that this meta-analysis also demonstrates heterogeneity of intubation depth for oral enteroscopy. Factors contributing to this variability may include selection criteria of the participants, the degree of sedation, experience level of the endoscopists, single-balloon and double-balloon methods, and different methods for measuring intubation depth. Exclusion of the study that allowed patients with previous abdominal surgery might eliminate the heterogeneity.
An improvement in intubation depth could only be shown when using the oral approach for balloon-assisted enteroscopy. A significant proportion of the anal approach fails to advance beyond the terminal ileum. The reason for the failure has been reported to be retroflection of the ileocecal valve and paradoxical withdrawal of colonic looping of the endoscope.7,17 A prospective European multicenter study reported the procedure failure in five of 35 patients (14%).18 Mehdizadeh et al. reported that the technical failure rate was 16%.17 Due to technical reason, the anal approach has been shown to be an unreliable parameter in intubation depth.
The meta-analysis by Wu et al. demonstrated the advantage of CO2 insufflation for the reduction of patient pain and discomfort during colonoscopy.19 These findings were confirmed by Wang et al., but not for double-balloon enteroscopy.20 They hypothesized that irritation to bowel nerves by balloon-assisted enteroscopy may result in pain and nullify the benefits of CO2 insufflation. However, their small sample size may not have provided sufficient statistical power. This updated meta-analysis reveals that there are clear benefits of CO2 insufflation with regard to post-procedural pain.
Domagk et al. reported that abdominal pain was significantly reduced in the CO2 group at 1 and 3 h after balloon-assisted enteroscopy.5 Lenz et al. reported abdominal pain was reduced in the CO2 group at 1 and 3 h after the procedure, but only reached statistical significance at 1 h after the anal procedure.7 Hirai et al. reported that VAS at 1 h after the procedure tended to be lower in the CO2 group, but without any significant difference.6 Li et al. reported there was no significant difference between CO2 group and air group.8 The different anesthesia approaches might have contributed to the discrepancy. Pooling the results only reached statistical significance at 1 h after the procedure.
This systematic review has several limitations. Different methods for reporting the intubation depth may be considered as a source of heterogeneity. We did not assess cost effectiveness in this review owing to the lack of related data. In addition, because of the limited number of eligible studies, subgroup analysis was not performed. Further studies with larger numbers of patients are warranted to clarify the safety and efficacy of CO2 insufflation during balloon-assisted enteroscopy.
In conclusion, when compared with air insufflation, CO2 insufflation during balloon-assisted enteroscopy was found to cause less post-procedural pain without CO2 retention. CO2 insufflation is recommended during balloon-assisted enteroscopy.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflicts of interest
During the last 2 years, Author H.S. received scholarship funds for the research from Astellas Pharm Inc., Astra-Zeneca K.K., Otsuka Pharmaceutical Co., Ltd., Takeda Pharmaceutical Co., Ltd., and Zeria Pharmaceutical Co., Ltd. and received service honoraria from Astellas Pharm Inc., Astra-Zeneca K.K., Eisai Co., Otsuka Pharmaceutical Co., Ltd., Takeda Pharmaceutical Co., Ltd., and Zeria Pharmaceutical Co., Ltd. Author T.K. received scholarship funds for the research from Astellas Pharm Inc., Astra-Zeneca K.K., Otsuka Pharmaceutical Co., Ltd., Takeda Pharmaceutical Co., Ltd., Eisai Pharmaceutical Co., Ltd., Zeria Pharmaceutical Co., Ltd., Tanabe Mitsubishi Pharmaceutical Co., Ltd. JIMRO Co., Ltd., Kyorin Pharmaceutical Co. Ltd., and received service honoraria from Astellas Pharm Inc., Eisai Pharmaceutical Co., Ltd., JIMRO Co., Ltd., Tanabe Mitsubishi Pharmaceutical Co., Ltd., Otsuka Pharmaceutical Co., Ltd., Takeda Pharmaceutical Co., Ltd., Miyarisan Pharmaceutical Co., Ltd., and Zeria Pharmaceutical Co., Ltd. Author N.Y. received scholarship funds for the research from Astra-Zeneca K.K., Takeda Pharmaceutical Co., Ltd., Eisai Co., Top Corporation, Kaigen Pharm Co., Ltd., ASKA Pharmaceutical Co., Ltd., FUJIFILM Corporation, Boston Scientific Japan K.K., Century Medical Inc., and Covidien Japan Inc. The funding source had no role in the design, practice or analysis of this study. There are no other conflicts of Interests for this article.
References
- 1.Yamamoto H, Sekine Y, Sato Y, et al. Total enteroscopy with a nonsurgical steerable double-balloon method. Gastrointest Endosc 2001; 53: 216–220. [DOI] [PubMed] [Google Scholar]
- 2.Tsujikawa T, Saitoh Y, Andoh A, et al. Novel single-balloon enteroscopy for diagnosis and treatment of the small intestine: Preliminary experiences. Endoscopy 2008; 40: 11–15. [DOI] [PubMed] [Google Scholar]
- 3.Domagk D, Mensink P, Aktas H, et al. Single- vs. double-balloon enteroscopy in small-bowel diagnostics: A randomized multicenter trial. Endoscopy 2011; 43: 472–476. [DOI] [PubMed] [Google Scholar]
- 4.Hussein AM, Bartram CI, Williams CB. Carbon dioxide insufflation for more comfortable colonoscopy. Gastrointest Endosc 1984; 30: 68–70. [DOI] [PubMed] [Google Scholar]
- 5.Domagk D, Bretthauer M, Lenz P, et al. Carbon dioxide insufflation improves intubation depth in double-balloon enteroscopy: A randomized, controlled, double-blind trial. Endoscopy 2007; 39: 1064–1067. [DOI] [PubMed] [Google Scholar]
- 6.Hirai F, Beppu T, Nishimura T, et al. Carbon dioxide insufflation compared with air insufflation in double-balloon enteroscopy: A prospective, randomized, double-blind trial. Gastrointest Endosc 2011; 73: 743–749. [DOI] [PubMed] [Google Scholar]
- 7.Lenz P, Meister T, Manno M, et al. CO2 insufflation during single-balloon enteroscopy: A multicenter randomized controlled trial. Endoscopy 2014; 46: 53–58. [DOI] [PubMed] [Google Scholar]
- 8.Li X, Zhao YJ, Dai J, et al. Carbon dioxide insufflation improves the intubation depth and total enteroscopy rate in single-balloon enteroscopy: A randomised, controlled, double-blind trial. Gut 2014; 63: 1560–1565. [DOI] [PubMed] [Google Scholar]
- 9.Nishizawa T, Suzuki H, Kinoshita S, et al. Second-look endoscopy after endoscopic submucosal dissection for gastric neoplasms. Dig Endosc 2015; 27: 279–284. [DOI] [PubMed] [Google Scholar]
- 10.Higgins J and Green Se. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration. 2011: Available from www.cochrane-handbook.org.
- 11.Nishizawa T, Suzuki H, Sagara S, et al. Dexmedetomidine versus midazolam for gastrointestinal endoscopy: A meta-analysis. Dig Endosc 2015; 27: 8–15. [DOI] [PubMed] [Google Scholar]
- 12.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986; 7: 177–188. [DOI] [PubMed] [Google Scholar]
- 13.Nishizawa T, Suzuki H, Matsuzaki J, et al. Propofol versus traditional sedative agents for endoscopic submucosal dissection. Dig Endosc 2014; 26: 701–706. [DOI] [PubMed] [Google Scholar]
- 14.Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997; 315: 629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nishizawa T, Nishizawa Y, Yahagi N, et al. Effect of supplementation with rebamipide for Helicobacter pylori eradication therapy: A systematic review and meta-analysis. J Gastroenterol Hepatol 2014; 29(Suppl 4): 20–24. [DOI] [PubMed] [Google Scholar]
- 16.Soria F, Lopez-Albors O, Morcillo E, et al. Carbon dioxide insufflation safety in double-balloon enteroscopy: An experimental animal study. Dig Endosc 2013; 25: 39–46. [DOI] [PubMed] [Google Scholar]
- 17.Mehdizadeh S, Han NJ, Cheng DW, et al. Success rate of retrograde double-balloon enteroscopy. Gastrointest Endosc 2007; 65: 633–639. [DOI] [PubMed] [Google Scholar]
- 18.Ell C, May A, Nachbar L, et al. Push-and-pull enteroscopy in the small bowel using the double-balloon technique: Results of a prospective European multicenter study. Endoscopy 2005; 37: 613–616. [DOI] [PubMed] [Google Scholar]
- 19.Wu J, Hu B. The role of carbon dioxide insufflation in colonoscopy: A systematic review and meta-analysis. Endoscopy 2012; 44: 128–136. [DOI] [PubMed] [Google Scholar]
- 20.Wang WL, Wu ZH, Sun Q, et al. Meta-analysis: The use of carbon dioxide insufflation vs. room air insufflation for gastrointestinal endoscopy. Aliment Pharmacol Ther 2012; 35: 1145–1154. [DOI] [PubMed] [Google Scholar]