Abstract
OBJECTIVES:
We examined the prevalence of Early Intervention (EI) enrollment in Massachusetts comparing singleton children conceived via assisted reproductive technology (ART), children born to mothers with indicators of subfertility but no ART (Subfertile), and children born to mothers who had no indicators of subfertility and conceived naturally (Fertile). We assessed the natural direct effect (NDE), the natural indirect effect (NIE) through preterm birth, and the total effect of ART and subfertility on EI enrollment.
METHODS:
We examined maternal and infant characteristics among singleton ART (n = 6447), Subfertile (n = 5515), and Fertile (n = 306 343) groups and characteristics associated with EI enrollment includingpreterm birth using χ2 statistics (α = 0.05). We estimated the NDE and NIE of the ART–EI enrollment relationship by fitting a model for enrollment, conditional on ART, preterm and the ART-preterm delivery interaction, and covariates. Similar analyses were conducted by using Subfertile as the exposure.
RESULTS:
The NDE indicated that the odds of EI enrollment were 27% higher among the ART group (odds ratioNDE = 1.27; 95% confidence interval (CI): 1.19 – 1.36) and 20% higher among the Subfertilegroup (odds ratioNDE = 1.20; 95% CI: 1.12 – 1.29) compared with the Fertile group, even if the rate of preterm birth is held constant.
CONCLUSIONS:
Singleton children conceived through ART and children of subfertile mothers both have elevated risks of EI enrollment. These findings have implications for clinical providers as they counsel women about child health outcomes associated with ART or subfertility.
What’s Known on This Subject:
The association of assisted reproductive technology (ART) and risks of adverse perinatal outcomes among singleton children is well established. The risk of Early Intervention enrollment among children conceived through the use of ART and children born to subfertile mothers remains unknown.
What This Study Adds:
Early Intervention enrollment among children born to ART and subfertile mothers is mainly due to the direct effect of ART and subfertility; preterm birth is not the primary contributor through which ART and subfertility are associated with enrollment.
In 2011, Massachusetts had 7502 assisted reproductive technology (ART) procedures performed per 1 million women aged 15 to 44 years, >3 times the US national average of 2401.1Based on2010 data from the 14th European IVF–Monitoring Consortium, only 2 European countries, Denmark and Slovenia, had higher proportions of births from ART (5.9% and 5.1%, respectively) than Massachusetts (4.5%).1,2 In the United States, states such as Massachusetts with ART-coverage insurance mandates have reported higher ART utilization rates.3
Previous research described associations between ART, subfertility, and risks of adverse perinatal outcomes, including multiple birth, preterm birth, low birth weight, small for gestational age, and long-term disability.4–12 Children with these adverse outcomes are at increased risk of poor developmental and behavioral outcomes and are specifically in need of Early Intervention (EI) programs.13–16 Cognitive, behavioral, and social outcomes can be improved if developmental/behavioral interventions are initiated early in life.15,17,18 These beneficial and long-lasting services can be provided through EI programs to children with developmental delays or at risk for such delays at no cost. As the number of children born from ART increases, it is important to understand the health and developmental needs of these children.
The likelihood of EI enrollment among children conceived through the use of ART remains unknown. Given that ART is associated with preterm birth19 and that preterm birth is associated with EI enrollment,13 we assumed that preterm birth may contribute to the ART/subfertility–EI enrollment relationship. In this study, we tested the hypothesis that EI enrollment among ART children and children born to subfertile mothers is partially explained by preterm status using the single-mediator model.20 This approach is used when a factor is on the causal pathway between the exposure and the outcome, and as such should not be adjusted for in the analysis of the total effect.
Our objectives were as follows: (1) to examine the prevalence of, and characteristics associated with, EI enrollment among singletons in Massachusetts comparing 3 groups (children conceived via ART, children born to women with indicators of subfertility but no ART [Subfertile], and children born to women with neither ART nor indicators of subfertility [Fertile]); (2) describe the most frequent reasons for EI enrollment; and (3) assess the direct, indirect (through preterm birth), and total effects of ART and subfertility on EI enrollment among singletons using a mediation model.
Methods
Data Sources
This study linked 3 population-based data systems: the Society for Assisted Reproductive Technology Clinic Outcome Reporting System (SART CORS), the Massachusetts Pregnancy to Early Life Longitudinal data system (PELL), and the EI program participation data. SART CORS contains ART treatment records collected in compliance with the Fertility Clinic Success Rate and Certification Act of 1992.21 All ART clinics in Massachusetts during our study period contributed data to SART CORS, which includes data on patient demographic characteristics, medical history, infertility diagnoses, ART treatments, and pregnancy outcomes.1 SART CORS has been described elsewhere.22,23
PELL is a population-based database of mothers and children, which links delivery records to their corresponding hospital discharge records for the delivery and non–birth-related inpatient admissions, observational stays, and emergency department visits over time and deaths of mothers and children. More than 99% of all deliveries in Massachusetts from 1998 to 2012 have been linked in PELL. The PELL linkage allows children born to the same mother to be identified as siblings and multiple hospitalization records belonging to the same women or children to be attributed as such.15
EI program participation data are collected by the Massachusetts Department of Public Health (MDPH) under part C of the Individuals with Disabilities Education Act (IDEA 97). EI programs provide services at no cost to infants/children aged 0 to 3 years at risk of or with established developmental delays due to birth, social/emotional, and environmental factors. There are 4 categories of eligibility: (1) established conditions, (2) established developmental delays, (3) at risk of developmental delays, and (4) clinical judgment. Many of these risk factors are recognizable at the time of birth and recorded on birth or delivery hospitalization records.14,15 Eligibility is determined by using an approved tool, the Battelle Developmental Inventory, Second Edition, or informed clinical opinion if the child does not meet the current definition of established condition or developmental delay when qualitative concerns can be documented. The most commonly used EI services include developmental specialists, occupational therapists, and speech and language pathologists.13 When children are determined to be eligible for EI services, an Individualized Family Service Plan (IFSP) is developed by EI providers and parents. The EI data system contains information on all EI participants, including demographic characteristics, reasons for referral, referral date, and types of EI services provided. Each child in the data system has a unique ID.16
Data Linkage and Study Sample
We constructed the Massachusetts Outcomes Study of Assisted Reproductive Technology (MOSART) database by linking PELL and SART CORS usingmother’s first and last name, father’s last name, andmother’s and infant’s dates of birth. The 5-phase linkage algorithm used to construct MOSART has been previously described.24 All linkages and analyses were performed by using SAS version 9.2 (SAS Institute, Cary, NC) and Link Pro(InfoSoft, Inc, Winnipeg, Manitoba, Canada).
We used a previously described algorithm to identify subfertile deliveries in the MOSART database.25 Briefly, a delivery was classified as subfertile if it met any of the following conditions from the data sources included in the MOSART database: (1) at least 1 of the 2 fertility-treatment questions on the Massachusetts birth certificate was answered “yes” for an index delivery or on a delivery record to the same woman within the 5 years before the index delivery, (2) a hospital encounter for a condition specifically related to infertility was associated with an index delivery or occurred in the 5 years before an index pregnancy, and (3) an ART cycle before the index delivery was found in SART CORS. We then removed those cases where a mother received ART for the index delivery, and the remaining deliveries were classified as subfertile.
We linked 334 152 state-resident deliveries in PELL occurring in Massachusetts between July 1, 2004, and December 31, 2008, to 42 649 eligible ART treatment cycles between January 1, 2004, and December 31, 2008, derived from SART CORS, with an overall linkage rate of 89.7% and a 95.0% linkage rate among Massachusetts-resident women receiving ART treatment in Massachusetts clinics. These linkage rates were previously published.24 The resulting database contained 342 035 live births and fetal deaths associated with the 334 152 deliveries.
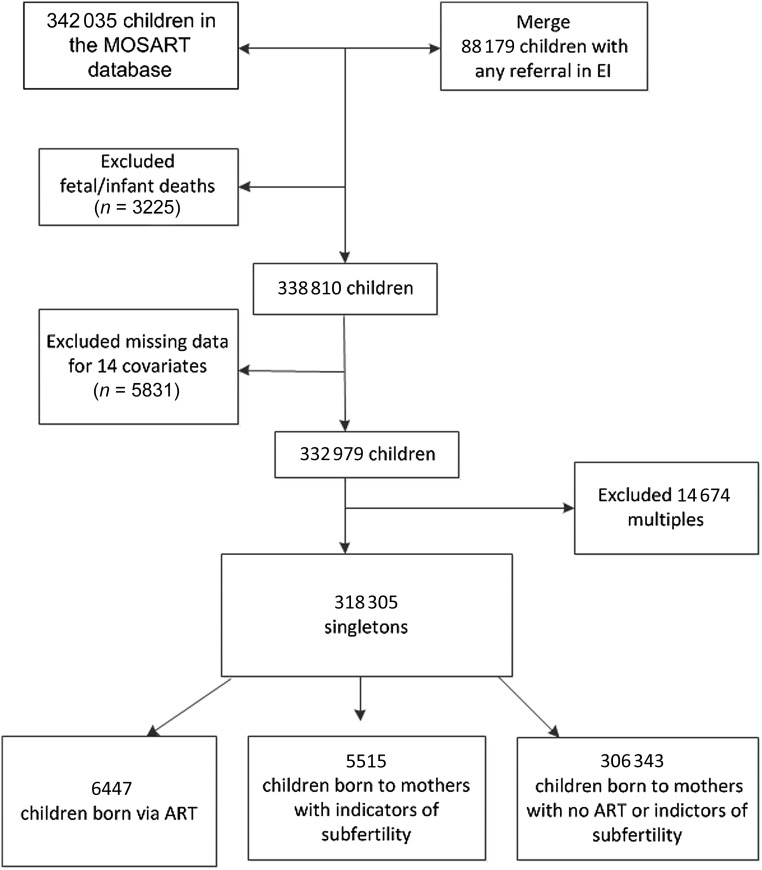
We then linked EI program data with PELL using the PELL unique child ID. The EI linkage algorithm to PELL has been previously described.26 The 342 035 live births were subsequently merged with 88 179 children who had any referral to EI between July 1, 2004, and December 31, 2011, to capture all potential enrollments from birth to age 3 (Fig 1). Almost 86% of EI enrollees linked to a PELL birth certificate. We excluded all multiple births from this study because of the high rate of plurality among ART-conceived pregnancies; and more importantly, after preliminary analysis, we found that multiple births did not meet the criteria for mediation analysis as described below.27 There is also a well-established association of plurality with adverse outcomes including low birth weight, perinatal mortality, and preterm birth.4,28 After excluding fetal and infant deaths (3225), records missing covariates (5831), and multiples (14 674), our final study sample included 318 305 children (ART, n = 6447; Subfertile, n = 5515; and Fertile, n = 306 343).
FIGURE 1.
Flow diagram of study sample with inclusion and exclusion criteria.
Dependent Variable
Our dependent variable was EI enrollment, defined here as having a signed IFSPin the EI database.
Independent Variables and Mediator
Our main independent variable was fertility status of the delivery for the index child categorized as ART, Subfertile, or Fertile. We conducted 2 separate analyses comparing the association of EI enrollment among (1) ART children and children born to fertile mothers and (2) children born to subfertile and children born to fertile mothers. Our mediator was preterm birth defined as a delivery at <37 weeks’ completed gestation.
Covariates
Covariates were selected on the basis of known risk factors for preterm birth, EI enrollment, and ART. These included maternal age, race and Hispanic ethnicity, education, nativity, marital status, delivery payer source, parity, prenatal care, infant gender, cigarette smoking during pregnancy, complications of labor and delivery, and abnormal conditions of the newborn.
Mediation Approach
Consistent with Ananth and VanderWeele’s mediation analysis approach,27 which involves several “no-unmeasured confounding assumptions,” we presumed that adjusting for the set of covariates listed above would be sufficient to control for confounding of (1) exposure–outcome (ART–EI enrollment), (2) mediator–outcome (preterm–EI enrollment), and (3) exposure –mediator (ART–preterm). We made similar assumptions using Subfertile as the independent variable. This mediation approach allowed us to split the total effect of ART and subfertility on EI enrollment into natural direct effect (NDE) and natural indirect effect (NIE).29,30 Figure 2 illustrates our mediation framework.
FIGURE 2.
Mediation framework for assessing whether preterm birth is a mediator of ART or subfertility in EI enrollment.
Statistical Analysis
We examined maternal and infant characteristics among singleton ART, Subfertile, and Fertile and prevalence and reasons for EI enrollment by fertility status using χ2 statistics (α = 0.05). We used logistic regression to estimate crude odds ratios (ORs) and adjusted ORs (aORs) and 95% confidence intervals (CIs) to assess the 3 mediation conditions defined above for ART versus Fertile and Subfertile versus Fertile. Using Ananth and VanderWeele’s approach,27 we estimated the NDE and NIE of the ART–EI enrollment relationship by fitting a model for enrollment (Y), conditional on ART (X), preterm delivery (M), and ART–preterm delivery interaction (X × M) and the covariates (C). We then fit a model for preterm delivery (M), conditional on ART (X) and the covariates (C). We conducted similar analyses using subfertility as the exposure. We ruled out the possibility of effect modification of preterm birth on the association of Subfertile and EI enrollment after we examined the interaction terms in our models. The mediation analysis was conducted using the mediation macro provided by Valerie and VanderWeele.
29 This study was approved by the Institutional Review Board of MDPH.
Results
Table 1 presents the distribution of infant and maternal characteristics of our study sample by fertility status. All P values were significant at <.001, except for gender. Preterm birth was significantly higher among ART and Subfertile (10.1% and 7.8%, respectively) compared with the Fertile (6.2%) group.
TABLE 1.
Maternal and Infant Characteristics by Fertility Status: Massachusetts Singleton Births, July 1, 2004, to December 31, 2008
| Distribution of Study Sample at Birth, % | |||
|---|---|---|---|
| ART (n = 6447) | Subfertile (n = 5515) | Fertile (n = 306 343) | |
| Maternal characteristics | |||
| Age | |||
| <30 years | 7.8 | 11.9 | 48.4 |
| 30 to <35 years | 30.9 | 33.7 | 30.4 |
| 35 to <40 years | 40.2 | 39.8 | 17.6 |
| 40 to <45 years | 18.1 | 13.7 | 3.5 |
| ≥45 years | 3.0 | 0.9 | 0.1 |
| Race/ethnicity | |||
| White non-Hispanic | 86.1 | 85.1 | 67.4 |
| Black non-Hispanic | 3.0 | 3.0 | 8.4 |
| Asian/Pacific Islander | 6.7 | 6.3 | 7.5 |
| Hispanic | 3.1 | 4.4 | 14.3 |
| Other non-Hispanic | 1.1 | 1.2 | 2.4 |
| Marital status | |||
| Married | 96.1 | 94.5 | 66.3 |
| Not married | 3.9 | 5.5 | 33.7 |
| Education | |||
| Less or no HS/GED | 9.4 | 11.9 | 37.7 |
| Some college/associate degree | 16.5 | 18.0 | 21.6 |
| Bachelor/postgraduate | 74.0 | 70.1 | 40.7 |
| Nativity | |||
| Foreign-born | 17.5 | 17.3 | 27.6 |
| US-born | 82.5 | 82.7 | 72.4 |
| Delivery payer source | |||
| Private | 96.8 | 92.1 | 58.8 |
| Public | 3.2 | 7.9 | 41.2 |
| Cigarettes during pregnancy | |||
| No | 99.2 | 98.2 | 92.3 |
| Yes | 0.8 | 1.8 | 7.7 |
| Prenatal care | |||
| Inadequate/intermediate | 7.4 | 8.9 | 17.2 |
| Adequate | 43.9 | 43.5 | 45.4 |
| Adequate plus | 48.7 | 47.6 | 37.4 |
| Parity | |||
| 1 | 62.4 | 39.3 | 45.7 |
| 2 | 30.0 | 40.0 | 34.2 |
| ≥3 | 7.6 | 20.7 | 20.1 |
| Complications of labor delivery and risk factors | |||
| No | 27.9 | 34.3 | 39.1 |
| Yes | 72.1 | 65.7 | 60.9 |
| Infant characteristics | |||
| Gender a | |||
| Male | 50.9 | 50.5 | 51.1 |
| Female | 49.1 | 49.5 | 48.9 |
| Abnormal conditions of newborn | |||
| No | 68.8 | 72.3 | 73.7 |
| Yes | 31.2 | 27.7 | 26.3 |
| Prematurity | |||
| No | 89.9 | 92.2 | 93.8 |
| Yes | 10.1 | 7.8 | 6.2 |
N = 318 305 singleton births. HS/GED, high school/general educational development.
P = .69 for ART versus Fertile and 0.33 for Subfertile versus Fertile.
Table 2 shows the prevalence of EI enrollmentby fertilitystatusand infant and maternal characteristics among singleton children. All P values were significant at <.001. The prevalences of EI enrollment among ART, Subfertile, and Fertile groups for singleton term children were 15.9%, 15.8%, and 15.2%, respectively. Among singleton preterm children, the prevalence of EI enrollment was more than twice that of all 3 fertility groups (44.0%, 36.9%, and 36.2% among ART, Subfertile, and Fertile, respectively).
TABLE 2.
EI Enrollment by Fertility Status and Infant and Maternal Characteristics: Massachusetts Singleton Births, July 1, 2004, to December 31, 2008
| Prevalence, % | |||
|---|---|---|---|
| ART (n = 1206 of 6447) | Subfertile (n = 960 of 5515) | Fertile (n = 50403 of 318 305) | |
| Overall EI enrollment | 18.7 | 17.4 | 16.5 |
| Infant characteristics | |||
| Prematurity | |||
| No | 15.9 | 15.8 | 15.2 |
| Yes | 44.0 | 36.9 | 36.2 |
| Gender | |||
| Male | 23.3 | 21.0 | 20.6 |
| Female | 14.0 | 13.7 | 12.1 |
| Abnormal conditions of newborn | |||
| No | 15.7 | 15.6 | 14.9 |
| Yes | 25.3 | 22.0 | 20.9 |
| Maternal characteristics | |||
| Age | |||
| <30 years | 16.5 | 14.5 | 17.7 |
| 30 to <35 years | 17.5 | 17.8 | 14.7 |
| 35 to <40 years | 19.8 | 17.6 | 15.8 |
| 40 to <45 years | 18.8 | 17.7 | 17.0 |
| ≥45 years | 22.2 | 25.5 | 20.7 |
| Race/ethnicity | |||
| Hispanic | 22.2 | 23.7 | 22.2 |
| White non-Hispanic | 18.7 | 17.6 | 15.7 |
| Black non-Hispanic | 20.2 | 15.2 | 17.7 |
| Asian/Pacific Islander | 16.3 | 12.4 | 11.3 |
| Other non-Hispanic | 19.2 | 13.2 | 15.6 |
| Marital status | |||
| Married | 18.7 | 17.3 | 14.2 |
| Not married | 19.0 | 19.3 | 20.8 |
| Education | |||
| Less than or no HS/GED | 20.7 | 19.1 | 20.0 |
| Some college/associate degree | 20.1 | 19.9 | 16.3 |
| Bachelor/postgraduate | 18.1 | 16.5 | 13.2 |
| Nativity | |||
| Foreign-born | 17.0 | 16.9 | 14.1 |
| US-born | 19.1 | 17.5 | 17.4 |
| Delivery payer source | |||
| Private | 18.4 | 17.1 | 13.7 |
| Public | 27.5 | 20.8 | 20.4 |
| Cigarettes during pregnancy | |||
| No | 18.7 | 17.4 | 15.7 |
| Yes | 21.6 | 19.6 | 25.4 |
| Prenatal care | |||
| Inadequate/intermediate | 14.9 | 20.6 | 17.5 |
| Adequate | 16.3 | 15.3 | 14.4 |
| Adequate plus | 21.4 | 18.7 | 18.5 |
| Parity | |||
| 1 | 18.2 | 17.4 | 15.8 |
| 2 | 20.0 | 17.3 | 16.2 |
| ≥3 | 18.3 | 17.8 | 18.4 |
| Complications of labor delivery and risk factors | |||
| No | 15.3 | 14.8 | 14.2 |
| Yes | 20.0 | 18.8 | 17.9 |
HS/GED, high school/general educational development.
Table 3 summarizes the reasons for EI enrollment by fertility status. P values were significant at <.05 for most conditions, with the exception of central nervous system disorder, circulatory disorder, sensory disorder, expressive language, suspected central nervous system abnormality, and clinical judgement.
TABLE 3.
Reasons for EI Enrollment by Fertility Status: Massachusetts Singleton Births, July 1, 2004 to December 31, 2008
| Distribution of Reasons for EI Enrollmenta,b | |||||
|---|---|---|---|---|---|
| ART | Subfertile | Fertile | Total | P | |
| Enrolled, n | 1206 | 960 | 50 403 | 52 569 | |
| Established conditions, % | 15.3 | 14.5 | 11.2 | 11.3 | <.0001 |
| CNS disorder | 1.7 | 1.9 | 1.5 | 1.5 | .53 |
| Circulatory disorder | 1.1 | 1.4 | 0.8 | 0.8 | .052 |
| Congenital torticollis | 5.5 | 3.7 | 2.7 | 2.8 | <.0001 |
| Sensory disorder | 2.0 | 1.8 | 1.3 | 1.3 | .07 |
| Established delays, % | 85.3 | 86.7 | 83.5 | 83.6 | <.01 |
| Cognition | 22.7 | 16.9 | 21.7 | 21.6 | <.01 |
| Adaptive | 19.3 | 15.9 | 16.3 | 16.4 | .02 |
| Fine motor | 59.0 | 60.5 | 59.5 | 59.5 | .75 |
| Gross motor | 21.8 | 12.3 | 17.3 | 17.3 | <.0001 |
| Expressive language | 32.7 | 25.2 | 22.5 | 22.7 | <.0001 |
| Receptive language | 26.5 | 26.0 | 35.0 | 34.6 | <.0001 |
| Social emotional | 12.0 | 7.5 | 10.1 | 10.1 | <.01 |
| At-risk conditions, % | 38.6 | 34.4 | 49.3 | 48.8 | <.0001 |
| Birth weight <1200 g | 3.5 | 1.9 | 2.0 | 2.0 | <.01 |
| Gestational age <32 weeks | 7.5 | 4.0 | 3.8 | 3.9 | <.0001 |
| NICU admission >5 days | 16.3 | 11.2 | 9.6 | 9.8 | <.0001 |
| Hospital stay >25 days in 6 months | 7.6 | 5.4 | 4.4 | 4.5 | <.0001 |
| Diagnosis of IGUR or SGA | 3.7 | 3.5 | 2.5 | 2.6 | .01 |
| Small size (weight, age, height criteria) | 8.5 | 8.9 | 4.8 | 5.0 | <.0001 |
| Chronic feeding difficulties | 11.1 | 10.5 | 8.7 | 8.8 | <.01 |
| Suspected CNS abnormality | 4.8 | 4.6 | 5.7 | 5.6 | .17 |
| Parental chronic illness/disability | 7.6 | 7.4 | 14.7 | 14.4 | <.0001 |
| Clinical judgement, % | 5.0 | 4.3 | 4.0 | 4.0 | .22 |
CNS, central nervous system; IGUR, intrauterine growth restriction; SGA, small for gestational age.
Percentages sum to >100 because children may be enrolled in EI program for >1 reason.
Not all reasons are presented; only risk factors occurring most frequently within each category are presented.
Table 4 presents the unadjusted ORs and aORs used to establish that our 3 mediation criteria were met. ART children were more likely to be preterm (aOR: 1.45; 95% CI: 1.32–1.59) and enrolled in EI (aOR: 1.34; 95% CI: 1.26–1.44) compared with their Fertile counterparts. After controlling for ART and other covariates, children who were preterm had 2.6 times the odds of being enrolled in EI. Those in the Subfertile group had significantly higher odds of being preterm (aOR: 1.18; 95% CI: 1.06–1.31) and being enrolled in EI (aOR: 1.21; 95% CI: 1.13–1.31) compared with those in the Fertile group.
TABLE 4.
Unadjusted ORs and aORs From Logistic Regression Models for Each of the Criteria for the Mediation Analysis: Massachusetts Singleton Births, July 1, 2004, to December 31, 2008
| Criteria for mediation | Unadjusted ORa (95% CI) | P | aORb (95% CI) | P |
|---|---|---|---|---|
| ART versus Fertile (N = 312 790) | ||||
| 1. Relationship between ART and EI enrollment | 1.17 (1.10 – 1.25) | <.001 | 1.34 (1.26 – 1.44) | <.001 |
| 2. Relationship between ART and preterm | 1.70 (1.57 – 1.85) | <.001 | 1.45 (1.32 – 1.59) | <.001 |
| 3. Relationship between preterm and EI enrollment | 3.21 (3.11 – 3.31) | <.001 | 2.60 (2.51 – 2.68) | <.001 |
| Subfertile versus Fertile (N = 311 858) | ||||
| 1. Relationship between Subfertile and EI enrollment | 1.07 (1.00 – 1.15) | .06 | 1.21 (1.13 – 1.31) | <.001 |
| 2. Relationship between Subfertile and preterm | 1.28 (1.16 – 1.42) | <.001 | 1.18 (1.06 – 1.31) | .003 |
| 3. Relationship between preterm and EI enrollment | 3.18 (3.08 – 3.28) | <.001 | 2.57 (2.48 – 2.66) | <.001 |
For the first 2 assumptions, the unadjusted OR is the crude OR of the association. For the third assumption, the unadjusted OR is the association of EI enrollment (outcome) and preterm (mediator), controlling only for fertility status (exposure).
Models adjusted for maternal demographic characteristics (maternal age, race, education, marital status, nativity), insurance, smoking, prenatal care, parity, gender, labor and delivery complications, and abnormal conditions of the newborn.
Table 5 shows the results of the mediation analysis. The NDE indicates that the odds of EI enrollment is 27% higher among ART (ORNDE: 1.27; 95% CI: 1.19–1.36) and 20% higher among Subfertile (ORNDE: 1.20; 95% CI: 1.12–1.29)compared with the Fertile group, even if the rate of preterm birth is the same across the 3 groups. Although the NIEs (odds of EI enrollment among ART group under their observed preterm rate) were statistically significant, the ORs were close to 1 (ORNIE for ART versus Fertile: 1.03; 95% CI: 1.02–1.04; ORNIE for Subfertile versus Fertile: 1.01; 95% CI: 1.00–1.01). The total effect, which is the product of NDE and NIE for Subfertile (ORTotal Effect: 1.21; 95% CI: 1.12–1.30) was equal to the aOR in Table 3. For ART, the total effect (ORTotal Effect: 1.31; 95% CI: 1.22–1.40)] is slightly different from the aOR due to the inclusion of the interaction term in the mediation analysis.
TABLE 5.
Estimates of NDE, NIE, and Total Effect of the Association Between ART and Subfertility and EI Enrollment Mediated Through Preterm Birth: Massachusetts Singleton Births, July 1, 2004, to December 31, 2008
| NDE | NIE | Total Effect | ||||
|---|---|---|---|---|---|---|
| ORa (95% CI) | P | ORa (95% CI) | P | OR (95% CI) | P | |
| ART versus Fertile | 1.27 (1.19 – 1.36) | <.001 | 1.03 (1.02 – 1.04) | <.001 | 1.31 (1.22 – 1.40) | <.001 |
| Subfertile versus Fertile | 1.20 (1.12 – 1.29) | <.001 | 1.01 (1.00 – 1.01) | <.01 | 1.21 (1.12 – 1.30) | <.001 |
Models adjusted for maternal age, race, education, marital status, nativity, delivery payer source, smoking, prenatal care, parity, gender, labor and delivery complications, and abnormal conditions of the newborn. An interaction term was included for the ART versus Fertile comparison.
Discussion
The proportion of singletons born via ART remains substantial in Massachusetts, yet little is known about the long-term health outcomes of these children. The likelihood of EI enrollment among ART and Subfertile groups has not been previously reported. This study presented a unique opportunity to examine child health outcomes through age 3 by using participation in EI programs as a proxy for risk of developmental delays.13 We had hypothesized that EI enrollment among the ART and Subfertile groups could be partially explained by preterm status. However, we found that EI enrollment was mainly due to the NDE of ART and subfertility, which indicates that the ART and Subfertile groups would still have higher odds of EI enrollment, even if the preterm rates remained the same across the fertility groups.
Our findings also confirmed that ART was associated with a greater risk of preterm birth. Pooled ORs from systematic reviews with meta-analyses indicated an approximate twofold increase in singletons born at <37 weeks of gestation.10 A recent review reported an OR of 1.5 (95% CI: 1.5–1.6) among singletons,31 which is close to our findings (aOR: 1.45; 95% CI: 1.32–1.59). We also found that preterm birth was higher among Subfertile, but this relationship was not as strong as in the ART group (aOR: 1.18; 95% CI: 1.06–1.31). Consistent with past research, our study also found that children who were born preterm have greater needs for EI services, which have been found to have long-lasting impact on developmental and social outcomes.13,32,33 Although we found a positive association between ART, Subfertile, and EI enrollment, our results differ from several reviews that showed no difference between naturally conceived and ART children in neurocognitive and motor development outcomes after adjusting for prematurity and other risk factors.34–37 However, other registry-based studies have shown greater risk of developmental delays and cerebral palsy.38–40 Given that our study used EI enrollment solely as a proxy for developmental delays, our study should be interpreted with caution. Although we report the most frequent reasons for EI enrollment, we did not assess the effect of ART on these individual developmental outcomes.
The classification of ART, Subfertile, and Fertile was made by using the gold standard, SART CORS clinical treatment data obtained directly from ART clinics and linked to delivery records. The successful linkage of 95% of eligible ART treatment records suggests that the vast majority of ART births in Massachusetts were correctly classified. However, we have no doubt that we might have underestimated the Subfertile group because many women treated in an outpatient setting may not have been included in our estimates. Although the Fertile group may contain a small proportion of women who are actually subfertile, it is unlikely that this small number is sufficient to affect the findings.
Our study has limitations. First, this study was limited to Massachusetts mothers who were residents at the time of delivery anddelivered in Massachusetts hospitals. Second, to estimate the NDEs and NIEs, the mediation analysis required an additional assumption that there was no unmeasured confounding of the preterm birth and EI enrollment relationship by factors due to ART or subfertility. Sensitivity analyses can be used to mimic how findings might be affected by specific unmeasured confounders.41 Although we did not conduct these sensitivity analyses, we did adjust for ART and subfertility to account for the effect of unmeasured factors associated with ART and subfertility. Third, we did not examine EI enrollment for each gestational age <37 weeks to assess the effect of earlier gestational age on enrollment. The risk of EI enrollment increasing with decreasing gestational age has been previously reported.13 Last, this study can only be generalized to singletons born in Massachusetts.
Despite these limitations, our study has several strengths. MOSART is a large, population-based database that includes detailed ART treatment,postbirth hospital utilization, and public health program data.24 Most ART studies in the United States have relied on the national database and clinic-based data, which do not allow investigators to follow children postbirth, nor do they allow them to link with program participation data.24
Our study is unique because it treated preterm birth as a mediator rather than a confounder, which allowed us to parse the total effect of ART and subfertility on EI enrollment into NDEs and NIEs.27 The NIE allowed us to show the extent to which intervening on preterm could better estimate EI enrollment among ART/Subfertile groups, whereas the NDE showed that, regardless of preterm, ART and Subfertile groups still had higher rates of EI enrollment (27% and 20%, respectively). The results from our study suggest that preterm birth is not the primary contributor through which ART and subfertility are associated with EI enrollment.
Our findings have implications for clinical providers, mainly obstetricians as they counsel women about child health outcomes associated with ART or subfertility. These findings can also help pediatricians and neonatologists as they develop discharge plans for these children to include referrals to EI programs and to educate families about the lasting benefit of EI services on children’s health. Finally, given that knowledge of long-term health outcomes among ART children and children born to subfertile mothers has been limited by the lack of longitudinal studies,24,42 our study showing that both ART and being subfertile increase EI enrollment represents a significant step forward. Yet, further research and long-term follow-up are needed to fully understand the health implications and risks on children and their families later in life.
Acknowledgments
We thank Dr Xiaohui Cui, ScD, and Ms Gabriela Kernan, MPH, from the Massachusetts Department of Public Health for analytic and programming contributions. We also thank Ms Thien H. Nguyen, MPH, Project Manager for MOSART, Boston University School of Public Health, for her contributions. SART thanks all of its members for providing clinical information to the SART CORS database for use by patients and researchers. Without the efforts of SART members, this research would not have been possible.
Glossary
- aOR
adjusted odd ratio
- ART
assisted reproductive technology
- CI
confidence interval
- EI
Early Intervention
- MOSART
Massachusetts Outcomes Study of Assisted Reproductive Technology
- NDE
natural direct effect
- NIE
natural indirect effect
- OR
odds ratio
- PELL
Pregnancy to Early Life Longitudinal
- SART CORS
Society for Assisted Reproductive Technology Clinic Outcome Reporting System
Footnotes
Dr Diop conceptualized and designed the study; interpreted the findings; drafted, reviewed, and wrote the final version of the manuscript; and directed the project overall; Ms Gopal participated in the planning of the study, had full access to all of the data, performed statistical programming and carried out the analyses, contributed to data interpretation, and reviewed the manuscript; Dr Cabral participated in the planning of the study, performed initial statistical programming, and contributed to data interpretation; Drs Belanoff, Declercq, Kotelchuck, Luke, and Stern participated in the planning of the study, contributed to data interpretation, and reviewed the manuscript; and all authors approved the final manuscript as submitted.
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Society of Assisted Reproductive Technology, the Massachusetts Department of Public Health, or the National Institutes of Health.
FINANCIAL DISCLOSURE: Dr Luke reports grants from the National Institutes of Health during the conduct of the study and personal fees from the Society for Assisted Reproductive Technology, outside of the submitted work; Dr Kotelchuck reports grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (grants RO1HD06459501 and RO1HD06727001) during the conduct of the study; the other authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: This study was supported through the Eunice Kennedy Shriver National Institute of Child Health and Human Development grants RO1 HD064595 and RO1 HD067270. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have no conflicts of interest to disclose.
References
- 1.Sunderam S, Kissin DM, Crawford SB, Folger SG, Jamieson DJ, Barfield WD; Centers for Disease Control and Prevention . Assisted reproductive technology surveillance—United States, 2011. MMWR Surveill Summ. 2014;63(10):1–28 [PubMed] [Google Scholar]
- 2.Kupka MS, Ferraretti AP, de Mouzon J, et al. ; European IVF-Monitoring Consortium, for the European Society of Human Reproduction and Embryology . Assisted reproductive technology in Europe, 2010: results generated from European registers by ESHRE. Hum Reprod. 2014;29(10):2099–2113 [DOI] [PubMed] [Google Scholar]
- 3.Henne MB, Bundorf MK. Insurance mandates and trends in infertility treatments. Fertil Steril. 2008;89(1):66–73 [DOI] [PubMed] [Google Scholar]
- 4.Boulet SL, Schieve LA, Nannini A, et al. Perinatal outcomes of twin births conceived using assisted reproduction technology: a population-based study. Hum Reprod. 2008;23(8):1941–1948 [DOI] [PubMed] [Google Scholar]
- 5.Wright VC, Chang J, Jeng G, Macaluso M. Assisted reproductive technology surveillance—United States, 2003. MMWR Surveill Summ. 2006;55(4):1–22 [PubMed] [Google Scholar]
- 6.Barnhart KT. Assisted reproductive technologies and perinatal morbidity: interrogating the association. Fertil Steril. 2013;99(2):299–302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dar S, Librach CL, Gunby J, Bissonnette F, Cowan L; IVF Directors Group of Canadian Fertility and Andrology Society . Increased risk of preterm birth in singleton pregnancies after blastocyst versus day 3 embryo transfer: Canadian ART Register (CARTR) analysis. Hum Reprod. 2013;28(4):924–928 [DOI] [PubMed] [Google Scholar]
- 8.Pharoah P. Neurological outcome in twins. Semin Neonatol. 2002;7(3):223–230 [DOI] [PubMed] [Google Scholar]
- 9.Schieve LA, Ferre C, Peterson HB, Macaluso M, Reynolds MA, Wright VC. Perinatal outcome among singleton infants conceived through assisted reproductive technology in the United States. Obstet Gynecol. 2004;103(6):1144–1153 [DOI] [PubMed] [Google Scholar]
- 10.Hansen M, Bower C. The impact of assisted reproductive technologies on intra-uterine growth and birth defects in singletons. Semin Fetal Neonatal Med. 2014;19(4):228–233 [DOI] [PubMed] [Google Scholar]
- 11.Pinborg A, Wennerholm UB, Romundstad LB, et al. Why do singletons conceived after assisted reproduction technology have adverse perinatal outcome? Systematic review and meta-analysis. Hum Reprod Update. 2013;19(2):87–104 [DOI] [PubMed] [Google Scholar]
- 12.Declercq E, Luke B, Belanoff C, et al. Perinatal outcomes associated with assisted reproductive technology: the Massachusetts Outcomes Study of Assisted Reproductive Technologies (MOSART). Fertil Steril. 2015;103(4):888–895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shapiro-Mendoza C, Kotelchuck M, Barfield W, et al. Enrollment in early intervention programs among infants born late preterm, early term, and term. Pediatrics. 2013;132(1). Available at: www.pediatrics.org/cgi/content/full/132/1/e61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Barfield WD, Clements KM, Lee KG, Kotelchuck M, Wilber N, Wise PH. Using linked data to assess patterns of early intervention (EI) referral among very low birth weight infants. Matern Child Health J. 2008;12(1):24–33 [DOI] [PubMed] [Google Scholar]
- 15.Clements KM, Barfield WD, Kotelchuck M, Lee KG, Wilber N. Birth characteristics associated with early intervention referral, evaluation for eligibility, and program eligibility in the first year of life. Matern Child Health J. 2006;10(5):433–441 [DOI] [PubMed] [Google Scholar]
- 16.Clements KM, Barfield WD, Kotelchuck M, Wilber N. Maternal socio-economic and race/ethnic characteristics associated with early intervention participation. Matern Child Health J. 2008;12(6):708–717 [DOI] [PubMed] [Google Scholar]
- 17.Gardner JM, Walker SP, Powell CA, Grantham-McGregor S. A randomized controlled trial of a home-visiting intervention on cognition and behavior in term low birth weight infants. J Pediatr. 2003;143(5):634–639 [DOI] [PubMed] [Google Scholar]
- 18.McCormick MC, Brooks-Gunn J, Buka SL, et al. Early intervention in low birth weight premature infants: results at 18 years of age for the Infant Health and Development Program. Pediatrics. 2006;117(3):771–780 [DOI] [PubMed] [Google Scholar]
- 19.Wang YA, Sullivan EA, Black D, Dean J, Bryant J, Chapman M. Preterm birth and low birth weight after assisted reproductive technology-related pregnancy in Australia between 1996 and 2000. Fertil Steril. 2005;83(6):1650–1658 [DOI] [PubMed] [Google Scholar]
- 20.MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annu Rev Psychol. 2007;58:593–614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fertility Clinic Success Rate and Certification Act of 1992: Public Law 102-493. US Statut Large. 1992;106:3146–3152 [PubMed]
- 22.Luke B, Brown MB, Stern JE, Missmer SA, Fujimoto VY, Leach R. Racial and ethnic disparities in assisted reproductive technology pregnancy and live birth rates within body mass index categories. Fertil Steril. 2011;95(5):1661–1666 [DOI] [PubMed] [Google Scholar]
- 23.Luke B, Brown MB, Wantman E, et al. Cumulative birth rates with linked assisted reproductive technology cycles. N Engl J Med. 2012;366(26):2483–2491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kotelchuck M, Hoang L, Stern JE, Diop H, Belanoff C, Declercq E. The MOSART database: linking the SART CORS clinical database to the population-based Massachusetts PELL reproductive public health data system. Matern Child Health J. 2014;18(9):2167–2178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Declercq ER, Belanoff C, Diop H, et al. Identifying women with indicators of subfertility in a statewide population database: operationalizing the missing link in assisted reproductive technology research. Fertil Steril. 2014;101(2):463–471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Manning SE, Davin CA, Barfield WD, et al. Early diagnoses of autism spectrum disorders in Massachusetts birth cohorts, 2001-2005. Pediatrics. 2011;127(6):1043–1051 [DOI] [PubMed] [Google Scholar]
- 27.Ananth CV, VanderWeele TJ. Placental abruption and perinatal mortality with preterm delivery as a mediator: disentangling direct and indirect effects. Am J Epidemiol. 2011;174(1):99–108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Luke B, Keith LG. The contribution of singletons, twins and triplets to low birth weight, infant mortality and handicap in the United States. J Reprod Med. 1992;37(8):661–666 [PubMed] [Google Scholar]
- 29.Valeri L, Vanderweele TJ. Mediation analysis allowing for exposure-mediator interactions and causal interpretation: theoretical assumptions and implementation with SAS and SPSS macros. Psychol Methods. 2013;18(2):137–150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vanderweele TJ, Vansteelandt S. Odds ratios for mediation analysis for a dichotomous outcome. Am J Epidemiol. 2010;172(12):1339–1348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pandey S, Shetty A, Hamilton M, Bhattacharya S, Maheshwari A. Obstetric and perinatal outcomes in singleton pregnancies resulting from IVF/ICSI: a systematic review and meta-analysis. Hum Reprod Update. 2012;18(5):485–503 [DOI] [PubMed] [Google Scholar]
- 32.Morse SB, Zheng H, Tang Y, Roth J. Early school-age outcomes of late preterm infants. Pediatrics. 2009;123(4). Available at: www.pediatrics.org/cgi/content/full/123/4/e622 [DOI] [PubMed] [Google Scholar]
- 33.Curry AE, Pfeiffer MR, Slopen ME, McVeigh KH. Rates of early intervention referral and significant developmental delay, by birthweight and gestational age. Matern Child Health J. 2012;16(5):989–996 [DOI] [PubMed] [Google Scholar]
- 34.Abdel-Mannan O, Sutcliffe A. I was born following ART: how will I get on at school? Semin Fetal Neonatal Med. 2014;19(4):245–249 [DOI] [PubMed] [Google Scholar]
- 35.Hyrapetian M, Loucaides EM, Sutcliffe AG. Health and disease in children born after assistive reproductive therapies (ART). J Reprod Immunol. 2014;106:21–26 [DOI] [PubMed] [Google Scholar]
- 36.Middelburg KJ, Heineman MJ, Bos AF, Hadders-Algra M. Neuromotor, cognitive, language and behavioural outcome in children born following IVF or ICSI-a systematic review. Hum Reprod Update. 2008;14(3):219–231 [DOI] [PubMed] [Google Scholar]
- 37.Shankaran S. Outcomes from infancy to adulthood after assisted reproductive technology. Fertil Steril. 2014;101(5):1217–1221 [DOI] [PubMed] [Google Scholar]
- 38.Lidegaard O, Pinborg A, Andersen AN. Imprinting diseases and IVF: Danish National IVF cohort study. Hum Reprod. 2005;20(4):950–954 [DOI] [PubMed] [Google Scholar]
- 39.Hvidtjørn D, Grove J, Schendel DE, et al. Cerebral palsy among children born after in vitro fertilization: the role of preterm delivery—a population-based, cohort study. Pediatrics. 2006;118(2):475–482 [DOI] [PubMed] [Google Scholar]
- 40.Strömberg B, Dahlquist G, Ericson A, Finnström O, Köster M, Stjernqvist K. Neurological sequelae in children born after in-vitro fertilisation: a population-based study. Lancet. 2002;359(9305):461–465 [DOI] [PubMed] [Google Scholar]
- 41.Bennett AC, Rankin KM, Rosenberg D. Does a medical home mediate racial disparities in unmet healthcare needs among children with special healthcare needs? Matern Child Health J. 2012;16(suppl 2):330–338 [DOI] [PubMed] [Google Scholar]
- 42.Buck Louis GM, Schisterman EF, Dukic VM, Schieve LA. Research hurdles complicating the analysis of infertility treatment and child health. Hum Reprod. 2005;20(1):12–18 [DOI] [PubMed] [Google Scholar]