Abstract
Background:
Intervertebral disc herniation is a major cause of low back pain. Several treatment methods are available for lumbar disc herniation including Chemonucleolysis, open surgery, nucleoplasty, laser disc decompression, and intradiscal electrothermal therapy. The high prevalence of lumbar disc herniation necessitates a minimally invasive yet effective treatment method. In this study, we compared the outcomes of open surgery and nucleoplasty method in patients with single lumbar disc herniation.
Materials and Methods:
This study was a noninferiority randomized clinical trial conducted in one of the University Hospitals of Isfahan Medical University; The Alzahra Hospital. About 200 patients with the diagnosis of lumbar disc herniation were recruited and were assigned to either the treatment or control groups using block randomization. One group received open surgery and the other group received nucleoplasty as the method of treatment. Patients were revisited at 14 days, 1, 2, 3 months, and 1-year after surgery and were assessed for the following variables: Lower back pain, lower limb pain, common complications of surgery (e.g., discitis, infection and hematoma) and recurrence of herniation.
Results:
The mean (standard deviation) severity of low back pain was reduced from 6.92 (2.5) to 3.43 (2.3) in the nucleoplasty group (P = 0.04) and from 7.5 (2.2) to 3.04 (1.61) in the discectomy group (P = 0.73). Between group difference was not statistically significant (P = 0.44), however, time and treatment interaction was significant (P = 0.001). The level of radicular pain evaluated 1 year after treatment was reduced from 8.1 (1.2) to 2.9 (1.2) (P = 0.004) and from 7.89 (2.1) to 3.6 (2.5) (P =0.04) in the discectomy and the nucleoplasty groups respectively, significant interaction between time and treatment options was observed (P < 0.001) while there was no significant difference between two treatment groups (P = 0.82).
Conclusion:
Our results show that while nucleoplasty is as effective as open discectomy in the treatment of lumbar disc herniation, it is also less invasive with higher patient compliance. Taking factor such as decreased cost and duration of the surgery, as well as faster recovery in patients into account; we suggest considering nucleoplasty as an effective method of treatment in patients with single-level disc herniation.
Keywords: Intervertebral disc herniation, nucleoplasty, open discectomy
INTRODUCTION
Low back pain is a major cause of patients’ visits to the physicians. This condition can result in considerable morbidity and even disability. It has been reported that around 80% of populations in Western countries have encountered low back pain at least once in their lifetime. Fifty-five percent of patients with low back pains experience radicular pain and symptoms.[1] Less than 5% of all cases of low back pain are caused by disc herniation but disc herniation is the most common cause of radicular pain in patients.[2,3,4,5] The prevalence of lumbar disc herniation is estimated between 3.7% and 5.1%; with 90% and 97% of disc herniations occurring at L4-L5 and L5-S1 levels.[6,7,8]
In neurosurgery, the standard treatment for lumbar disc herniation with radicular pain is open discectomy. Recently, however, there has been a trend toward minimally invasive approaches in the treatment of disc herniation patients.[9]
Plasma-laser nucleoplasty is considered as an effective minimally invasive method for the treatment of lumbar pain due to disc herniation.[10,11,12,13] This technique is considered time-saving and it has less postoperative complications such as bleeding, long-term hospitalization, infection and postoperative hospitalization for wound healing, and removal of the sutures. It also has the added advantage of decreased tissue injury with reduced intraoperation pain and faster rehabilitation compared to other methods.[14]
In conventional radiofrequency instruments, heat is used to destroy the disc[15] but in the nucleoplasty method a plasma laser source is used for destroying the disc and opening of the annulus fibrosus and nucleus pulposus. In this method, radiofrequency energy is used to burn nucleus pulposus in a controlled manner. This energy is also used to decompress the disc without causing injury to the adjacent tissues. Few studies have assessed the long-term effect of nucleoplasty method,[10,11,16,17,18] these, however, have reported encouraging results for the treatment of disc herniation.[18,19,20,21] On the other hand, there are very few studies on the nucleoplasty method using plasma light compared with conventional methods. In this study, we compared the outcomes of open surgery and nucleoplasty method in patients with single lumbar disc herniation. We have also considered the demographic differences, different life styles, as well as different medical care settings, in the design of this study.
MATERIALS AND METHODS
Study design and participants
This study is a noninferiority randomized clinical trial conducted in 2011-2012, in Alzahra Hospital; a University Hospital in Isfahan, Iran. Participants were selected from individuals who were referred to our center because of lumbar disc herniation and low back pain. Participants included individuals with an established diagnosis of disc herniation who were candidates for open discectomy surgery; patients with <60 years of age who gave informed consent were recruited into the study. Poor response to rest and medication, single lumbar disc herniation, lack of neural impairment, and lack of indications for urgent surgery were considered as other inclusion criteria. Exclusion criteria included: Patients with spinal canal stenosis, patients at high risk for surgical intervention (e.g., damage to the nerve root and thecal sac compression) and those who had any contraindication for receiving the full dose of laser beam for nucleoplasty.
The sample size was calculated taking into consideration a confidence interval of 95% and power of 80%. Standard error of the pain score in patients before surgery was considered as 2 and the least significant difference was set to 0.8 in our study. The sample size was subsequently calculated as 98 patients in each group, with a final decision of recruiting 100 patients for each group.
The trial protocol was approved in the Ethics Committee of the Isfahan University of Medical Sciences (Research Project Number is 393437). Two hundred patients who met the inclusion criteria and did not have any of the exclusion criteria were recruited into the study and were randomly allocated to two groups. Informed consent was obtained from all patients. Demographic data, as well as patient's past history, were documented in data sheets.
Procedures and outcome evaluation
Two hundred study subjects with lumbar disc herniation were recruited and randomly assigned to either of the two groups of 100 participants; in the treatment group, the patients underwent laser nucleoplasty while in the control group they underwent open surgery. All patients were discharged from the hospital 24 h after the surgery and were followed up in 14 days and 1, 2, 3 months and 1-year postoperation to assess their lower back pain and lower limb radicular pain. We also assessed the patients for common complications including discitis, infection, and surgical site hematoma. We assessed the severity of the pain using the numeric pain scale method.
Statistical analysis
Quantitative data were expressed as mean ± standard deviation (SD) while qualitative as frequency (percentage). The normality of quantitative studied variables was evaluated using Q-Q plot and Kolmogorov-Smirnov statistical test. Within and between groups analysis over the study period was conducted using repeated measures ANOVA. Mauchlys Sphericity test was conducted to assess sphericity as a perquisite assumption. Huynh-Feldt correction was applied when this assumption was not satisfied. Within group comparisons at each follow-up time points were tested using repeated contrasts. Between groups analysis in each time point of follow-up period was conducted using independent t-test. The chi-square test was used for comparing the categorical data between two studied groups. All analyses were performed in SPSS (version 16, SPSS Inc., Chicago, IL, USA).
RESULTS
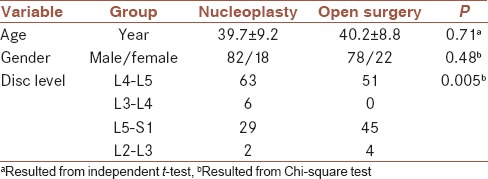
The average (±SD) age of participants in the nucleoplasty and the open discectomy groups were 39.7 ± 9.2 and 40.2 ± 8.8, respectively, (P = 0.71). Gender ratio (male:female) in the nucleoplasty group was 82/18 and in the open discectomy was 78/22. (P = 0.48).
The most common level of disc herniation was at the level of L4-L5 lumbar vertebrae in both groups. In a nucleoplasty group, 29 participants and 45 participants in the open discectomy group had a herniation at the L5-S1 level. In the nucleoplasty group, however, six individuals were diagnosed with L3-L4 level disc herniation. Fischer exact test showed a significant difference in the level of herniation between the two groups (P = 0.005). Table 1 shows the demographic data and the level of disc herniation in two groups.
Table 1.
Demographic data and comparison of the level of disc herniation in two groups
The results of repeated measure ANOVA on lumbar pain data are as follows: A significant difference over the follow-up period for measured lumbar pain (P < 0.001) with decreasing trend was observed in open surgery group (P = 0.04) but no statistically significant in nucleoplasty group (P = 0.73) [Table 2, time effects]. Also, repeated measures ANOVA showed no significant treatment influence (F = 0.59, P = 0.44) on the recorded lumbar pain based on visual analog scale (VAS), in which the level of lumbar pain was similar between two treatment groups [Figure 1 and Table 2; treatment effects]. Statistically significant group differences were not identified between pairwise time points after intervention [Table 2, t-test results]. Within groups comparisons for successive time points using repeated contrast showed that there are significant differences between all after intervention time points and baseline (P < 0.01) in open surgery group, whereas no statistically significant difference were observed in nucleoplasty group. There was statistically significant interaction between treatment and time (F = 6.55, P = 0.001) [Table 2, time × treatment effect].
Table 2.
Mean and SE of the low back pain score and radicular pain score before and up to 3 months postoperation in both groups
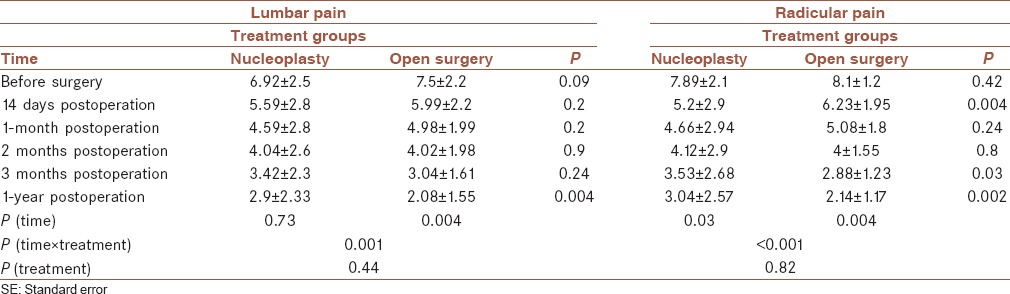
Figure 1.
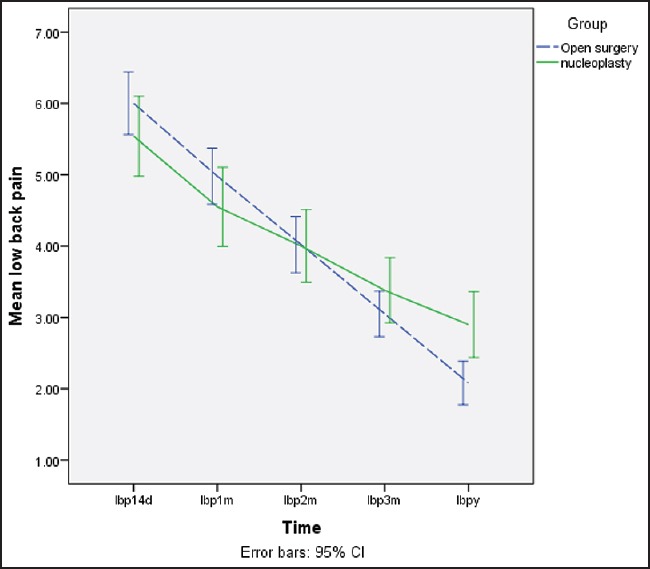
Mean and 95% confidence interval of low back pain in two studied groups during the follow-up period
The results of repeated measure ANOVA showed no statistically significant differences between groups in terms of radicular pain (F = 1.85, P = 0.18). Between group differences were statistically significant only at 14 days and 3 months after intervention during follow-up period [Table 2, results of independent samples t-test, Figure 2]. The time effects in both groups were statistically significant (P = 0.03 for nucleoplasty group and =0.004 for open surgery group) [Table 2 and Figure 2]. Within group differences between successive time points after intervention and baseline in both treatment groups were statistically significant (P < 0.001). Furthermore, no significant difference was observed between two competitor treatments (F = 0.06, P = 0.82, Table 2, treatment effect). Statistically significant interaction was observed between time and interventions (F = 18.73, P < 0.001, Table 2, time × treatment effect). None of the participants developed an infection at the site of surgery or discitis in the 6-month postoperation follow-up. Although, seven patients in the nucleoplasty group and eight patients from the open surgery group exhibited recurrent disc herniation requiring open surgery, which were successfully performed in all of these cases. The recurrence rate was not significantly different between the two groups (P = 0.79).
Figure 2.
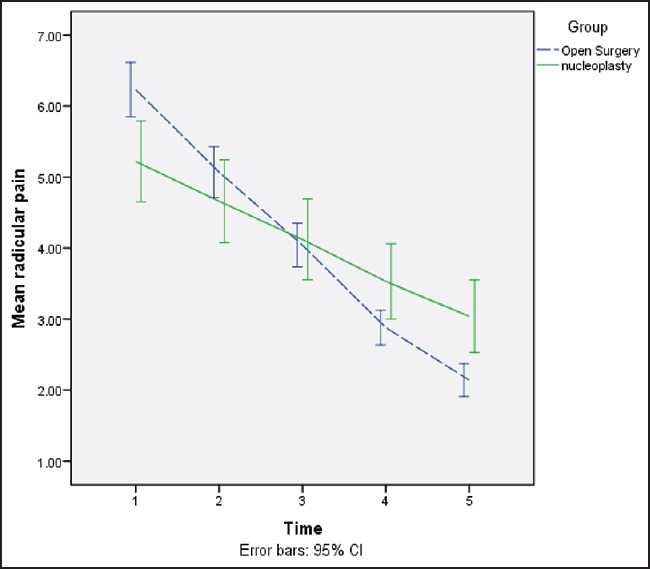
Mean and 95% confidence interval of radicular back pain in two studied groups during the follow-up period
DISCUSSION
The main aim of this study was to compare the outcomes of open discectomy versus plasma laser nucleoplasty in patients with single lumbar disc herniation. In our study, two groups of 100 randomly assigned patients underwent either discectomy or nucleoplasty.
The average age and gender distribution were not significantly different between the two groups.
Our findings suggest that the lumbar pain score is not significantly different in two groups up to 3 months postoperation. Our data also showed that nucleoplasty is not inferior to open surgery in pain reduction. The severity of radicular pain was also reduced significantly in both groups, the intergroup differences, however, were insignificant. Furthermore, the results are suggestive of comparable effectiveness of both methods in pain reduction. Our findings are in accordance with other similar studies evaluating the efficacy of nucleoplasty in pain reduction in individuals diagnosed with disc herniation. For example, Kim et al., showed that in patients who have undergone plasma laser nucleoplasty, during the 21 months postsurgery follow-up, VAS score was reduced from 7.4 ± 1.4 to 1.4 ± 0.7 (P < 0.001). In that study, 41 participants (89.1%) showed considerable improvement, according to MacNab's criteria.[18] In another study conducted by Masala et al., 72 patients with disc herniation underwent nucleoplasty and were followed up for up to 1-year postoperation. Clinical symptoms of patients were assessed and it was shown that the average pain score was reduced from 8.2 before surgery to 4.1 during the 1-year postoperation follow-up with 12 participants (17%) showing complete recovery and 43 (62%) showing considerable improvement.[19] In a cohort study conducted by Singh et al., on 57 patients with discogenic pain, the severity of pain was assessed 1, 3, 6, and 12 months after nucleoplasty and more than 50% of patients showed reduced pain scores. Their results also showed improved functional activity in patients following nucleoplasty.[20]
In another study by Zhu et al., 42 patients with disc herniation who had undergone plasma laser nucleoplasty were followed for up to 2 years and it was shown that the VAS score and Oswestry disability index improved significantly (P < 0.05) and the clinical outcomes showed considerable improvement.[21] In our study 3 months after operation, 7% of patients in the nucleoplasty group and 8% of patients in the open surgery group showed recurrence of disc herniation and underwent repeat open surgery.
There was one incidence of foot drop due to diabetic neuropathy. We did not notice any other complications in either of the two groups. Our findings are similar to Zhu et al. study where the recurrence of disc herniation was reported as 7.1% at 3 weeks postoperation.[21] Based on the results of this study and evidence from similar studies, we suggest that nucleoplasty shows comparable efficacy to open surgery with lesser invasiveness and much higher patient compliance. Furthermore, this method is more cost effective and the duration of surgery, as well as postoperative rehabilitation time, is reduced.[15]
CONCLUSION
We suggest that nucleoplasty can be considered as a first line method for treatment of patients with single level disc herniation.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
AUTHOR'S CONTRIBUTION
SA contributed in the conception of the work, conducting the study, revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work. MK contributed in the conception of the work, conducting the study, revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work. AM contributed in the conception of the work, drafting and revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work. HT contributed in the conception of the work, conducting the study, revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work. MR contributed in the conception of the work, revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work. AM contributed in the conception of the work, conducting the study, revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work. BG contributed in the conception of the work, revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work. AM contributed in the conception of the work, revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work. EY contributed in the design of the work, revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work. AMK contributed in the conception and design of the work, drafting and revising the draft, approval of the final version of the manuscript, and agreed for all aspects of the work.
REFERENCES
- 1.Jordan JO, Kika K. Herniated lumbar disk. Am Fam Physician. 2006;73:1240–2. [Google Scholar]
- 2.Chen YC, Lee SH, Chen D. Intradiscal pressure study of percutaneous disc decompression with nucleoplasty in human cadavers. Spine (Phila Pa 1976) 2003;28:661–5. doi: 10.1097/01.BRS.0000051920.45671.88. [DOI] [PubMed] [Google Scholar]
- 3.Fardon DF, Milette PC. Combined task forces of the North American spine society, American society of spine radiology, and American society of neuroradiology. Nomenclature and classification of lumbar disc pathology. Recommendations of the Combined task Forces of the North American Spine Society, American Society of Spine Radiology, and American Society of Neuroradiology. Spine (Phila Pa 1976) 2001;26:E93–113. doi: 10.1097/00007632-200103010-00006. [DOI] [PubMed] [Google Scholar]
- 4.Rajeev KP, Rene C. Lumbar degenerative disk disease. [Updated on 2014 Nov 20, Last accessed on 2014 Nov 21]. Available from: http://www.emedicine.medscape.com/article/309767-overview .
- 5.Karasek M, Bogduk N. Twelve-month follow-up of a controlled trial of intradiscal thermal anuloplasty for back pain due to internal disc disruption. Spine (Phila Pa 1976) 2000;25:2601–7. doi: 10.1097/00007632-200010150-00010. [DOI] [PubMed] [Google Scholar]
- 6.Ernst CW, Stadnik TW, Peeters E, Breucq C, Osteaux MJ. Prevalence of annular tears and disc herniations on MR images of the cervical spine in symptom free volunteers. Eur J Radiol. 2005;55:409–14. doi: 10.1016/j.ejrad.2004.11.003. [DOI] [PubMed] [Google Scholar]
- 7.Battié MC, Videman T. Lumbar disc degeneration: Epidemiology and genetics. J Bone Joint Surg Am. 2006;88:3–9. doi: 10.2106/JBJS.E.01313. [DOI] [PubMed] [Google Scholar]
- 8.Battié MC, Videman T, Parent E. Lumbar disc degeneration: Epidemiology and genetic influences. Spine (Phila Pa 1976) 2004;29:2679–90. doi: 10.1097/01.brs.0000146457.83240.eb. [DOI] [PubMed] [Google Scholar]
- 9.Welch WC, Gerszten PC. Alternative strategies for lumbar discectomy: Intradiscal electrothermy and nucleoplasty. Neurosurg Focus. 2002;13:E7. doi: 10.3171/foc.2002.13.2.8. [DOI] [PubMed] [Google Scholar]
- 10.Sharps LS, Isaac Z. Percutaneous disc decompression using nucleoplasty. Pain Physician. 2002;5:121–6. [PubMed] [Google Scholar]
- 11.Singh V, Piryani C, Liao K, Nieschulz S. Percutaneous disc decompression using coblation (nucleoplasty) in the treatment of chronic discogenic pain. Pain Physician. 2002;5:250–9. [PubMed] [Google Scholar]
- 12.Singh V, Piryani C, Liao K. Evaluation of percutaneous disc decompression using coblation in chronic back pain with or without leg pain. Pain Physician. 2003;6:273–80. [PubMed] [Google Scholar]
- 13.Reddy AS, Loh S, Cutts J, Rachlin J, Hirsch JA. New approach to the management of acute disc herniation. Pain Physician. 2005;8:385–90. [PubMed] [Google Scholar]
- 14.Chen YC, Lee SH, Saenz Y, Lehman NL. Histologic findings of disc, end plate and neural elements after coblation of nucleus pulposus: An experimental nucleoplasty study. Spine J. 2003;3:466–70. doi: 10.1016/s1529-9430(03)00143-8. [DOI] [PubMed] [Google Scholar]
- 15.Buy X, Gangi A. Percutaneous treatment of intervertebral disc herniation. Semin Intervent Radiol. 2010;27:148–59. doi: 10.1055/s-0030-1253513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee SC. Radiofrequency treatment in Korea. Pain Pract. 2002;2:185–6. doi: 10.1046/j.1533-2500.2002.20223.x. [DOI] [PubMed] [Google Scholar]
- 17.Slipman CW, Bhat AL, Gilchrist RV, Isaac Z, Garvand C, Chou L, et al. Preliminary results for axial low back pain treated with coblation: A comparison of patients with and without a central focal protrusion. Eur Spinal J. 2002;11:416–7. [Google Scholar]
- 18.Kim SH, Kim SC, Cho KH. Clinical outcomes of percutaneous plasma disc coagulation therapy for lumbar herniated disc diseases. J Korean Neurosurg Soc. 2012;51:8–13. doi: 10.3340/jkns.2012.51.1.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Masala S, Massari F, Fabiano S, Ursone A, Fiori R, Pastore F, et al. Nucleoplasty in the treatment of lumbar diskogenic back pain: One year follow-up. Cardiovasc Intervent Radiol. 2007;30:426–32. doi: 10.1007/s00270-006-0223-4. [DOI] [PubMed] [Google Scholar]
- 20.Singh V, Piryani C, Liao K. Role of percutaneous disc decompression using coblation in managing chronic discogenic low back pain: A prospective, observational study. Pain Physician. 2004;7:419–25. [PubMed] [Google Scholar]
- 21.Zhu H, Zhou XZ, Cheng MH, Shen YX, Dong QR. The efficacy of coblation nucleoplasty for protrusion of lumbar intervertebral disc at a 2-year follow-up. Int Orthop (SICOT) 2011;35:1677–82. doi: 10.1007/s00264-010-1196-0. [DOI] [PMC free article] [PubMed] [Google Scholar]


