Abstract
Background: Multiple sclerosis (MS) rates are increasing in Latin America, and caregiving for an individual with MS is associated with poorer mental and physical health outcomes. No existing research has examined the relation between mental health and health-related quality of life (HRQOL) in MS caregivers in Latin America.
Methods: The present study examined the association between mental health (Patient Health Questionnaire-9, Satisfaction with Life Scale, Rosenberg Self-esteem Scale, State-Trait Anxiety Inventory) and HRQOL (36-item Short Form Health Status Survey) in 81 Mexican MS caregivers.
Results: A canonical correlation analysis uncovered a large, significant overall association between mental health and HRQOL, with 52.7% of the variance shared between the two sets of constructs. When individual canonical loadings were examined in this analysis, the most substantial pattern that emerged was between depression and general health. Four regressions controlling for demographic variables found that HRQOL uniquely accounted for 19.0% of the variance in caregiver anxiety, 32.5% in depression, 13.5% in satisfaction with life, and 14.3% in self-esteem.
Conclusions: These findings demonstrated a strong association between HRQOL and mental health, which points to directions for future studies on interventions for MS caregivers, particularly in Mexican and other Latino populations.
Multiple sclerosis (MS) is one of the most common neurologic diseases in the world,1 and there is growing evidence to suggest that there has been an increase in the rates of diagnosis of MS in Latin America, especially in Mexico.2,3 By the 1990s, MS had become the second most common reason for admission to neurology wards in Latin America, likely due to an improvement in access to services and diagnostic tools.4 Given the relatively early onset and gradual but lifelong course of MS, individuals with this illness often need an informal caregiver.5
Research shows that being an MS caregiver can have a profound effect on one's own mental and physical health.6–12 A variety of studies have shown the deleterious effects that caregiving can have on MS caregiver mental health.9–13 One study, for example, found that of 35 MS caregivers from Greece, 22 met the clinical criteria for anxiety (5 mild and 17 moderate) and 12 were above the clinical threshold for depression (4 mild and 8 moderate).6 In addition, MS caregivers have reported experiencing guilt, anger, resentment, and feelings of inadequacy.13 Research has also shown that self-esteem is linked to various aspects of caregiver reactions (eg, control, challenge), specifically in the context of caring for an individual with MS.11 MS caregiver mental health has been shown to be particularly reduced when patients' quality of life and overall health are low.14,15
In addition to poorer mental health, MS caregivers have reduced health-related quality of life (HRQOL), which refers to the impairment and deficits in functioning that are associated with a particular health problem.16 MS caregivers report significantly worse HRQOL than do noncaregivers,6–8,10 and as many as 72% of MS caregivers would be unable to continue providing care to the patient if their own health began to deteriorate.17 Although most of the MS caregiver research to date has tended to look at mental and physical health separately, one study found an inverse correlation between health state and psychological distress in MS caregivers,6 highlighting the significant association between mental health and physical health. However, this was the only known study published to date that addressed the connections between these two sets of variables in MS caregivers.
Although previous research on MS caregivers is limited, particularly in Latin America, extant research on caregiving in Latino communities provides valuable insight into the potential unique aspects of care in Latin America, which may influence the connections between the physical and mental health of MS caregivers. This link is extremely important because caregiver mental and physical health can affect caregivers' ability to provide high-quality care to individuals with MS.10 The purpose of the present study was, therefore, to examine the associations between mental health (anxiety, depression, satisfaction with life, and self-esteem) and HRQOL in MS caregivers in Mexico.
Methods
Participants
Before commencement of the study, the protocol was reviewed and accepted by the ethics committee at the Mexican Foundation for Multiple Sclerosis. Eighty-six MS caregivers were recruited from the Mexican Foundation for Multiple Sclerosis and the Department of Neurosciences of the University Center for Health Sciences, University of Guadalajara, Guadalajara, Mexico. Medical records were accessed and reviewed at these locations. Individuals were eligible to participate in the study if they had cared for a person with MS for at least 6 months. Caregivers were excluded from the study if they had a previously diagnosed neurologic disorder, psychiatric disorder, or serious developmental disability that would prevent them from completing the measures. Caregivers who met the inclusion criteria were then contacted by telephone. Two master's-level psychologists (AAA, BVRB) were responsible for recruiting and consenting the participants and for verbally administering the assessments. Five of the caregivers who were contacted refused to participate in the study, leading to a final sample size of 81 caregivers. Demographic information for the caregivers and patients (reported by the caregiver) is summarized in Tables 1 and 2, respectively.
Table 1.
Demographic characteristics of the 81 multiple sclerosis caregivers
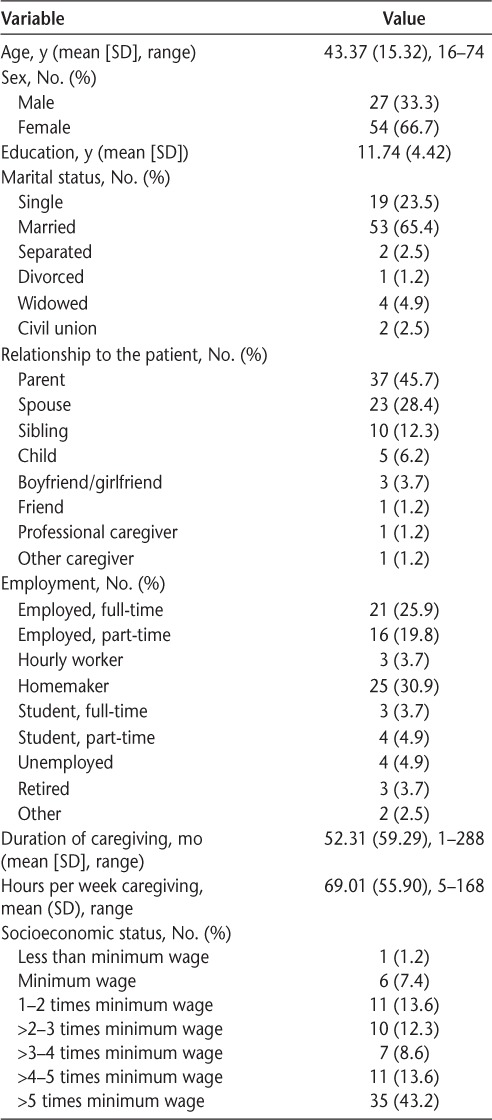
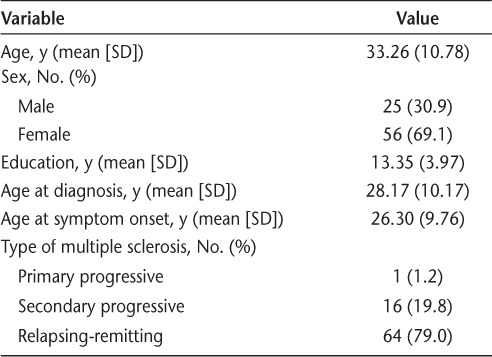
Table 2.
Demographic characteristics of the 81 patients with multiple sclerosis receiving care
Measures
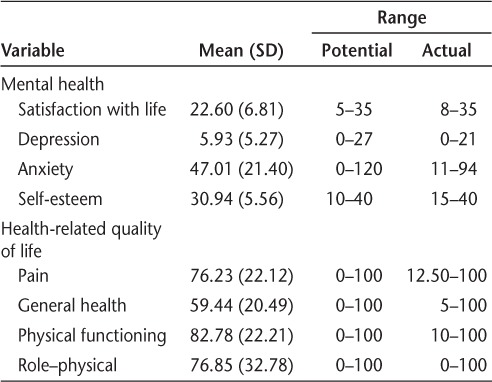
Means, standard deviations, and ranges for all the mental health and HRQOL variables are presented in Table 3.
Table 3.
Psychometric properties of the major study variables
Demographic Characteristics
Caregivers responded to several demographic questions (eg, age, sex, marital status, years of education, relationship to the patient, employment status, duration of caregiving, hours per week providing care, and socioeconomic status). Demographic information was also collected for the patient (eg, age, sex, number of years since diagnosis, and type of MS), as reported by the caregiver.
Short Form Health Status Survey
The 36-item Short Form Health Status Survey (SF-36) is a widely used measure of HRQOL and demonstrates strong psychometric properties.18 For the present study, only four SF-36 physical subscales (physical functioning, role–physical, bodily pain, and general health) were used. Because of their strong association with other mental health outcome variables included in the study (eg, depression), the SF-36 mental health subscales were excluded from these analyses to control for this overlap. Subscale scores range from 0 to 100, with higher scores indicating better HRQOL.19 This measure has been used in studies of MS caregivers and Spanish populations, and it demonstrates strong psychometric properties.20 The internal consistency for the Physical Health domain in the present study was excellent (α = 0.91).
Satisfaction with Life Scale
The Satisfaction with Life Scale is a self-report measure of global life satisfaction.21 It is a five-item scale that instructs participants to rate each item using a 7-point Likert response (1 = strongly disagree and 7 = strongly agree). Scores range from 5 to 35, with higher scores representing greater life satisfaction.22 The Spanish version has demonstrated strong psychometric properties.23 The internal consistency in the present study was good (α = 0.81).
State-Trait Anxiety Inventory
The State-Trait Anxiety Inventory is a 40-item self-report measure of anxiety that assesses state and trait experiences of anxiety.24 Responses are rated on a 4-point Likert scale (0 = not at all and 3 = very much so), with higher scores indicating higher anxiety. For the purpose of this study, the overall score was combined given the correlation between the State and Trait subscales (r = 0.76). The Spanish version25 has demonstrated strong psychometric properties.26 The combined internal consistency of this measure in the present study was excellent (α = 0.94).
Rosenberg Self-esteem Scale
The Rosenberg Self-esteem Scale is a ten-item questionnaire that asks respondents to rate their overall sense of worth using a 4-point Likert response (1 = strongly disagree and 4 = strongly agree).27,28 Scores range from 10 to 40, with higher scores suggesting greater self-esteem; scores less than 25 indicate clinically significant (low) self-esteem.29 This measure has demonstrated adequate reliability and validity.30 It has also been translated into several languages and has demonstrated good psychometric properties in 53 countries, including Latin American countries, such as Argentina, Bolivia, Brazil, Chile, Mexico, and Peru.28 The internal consistency of this scale in the present study was good (α = 0.86).
Patient Health Questionnaire-9
The Patient Health Questionnaire-9 (PHQ-9) consists of nine items and was used to assess caregiver depression. Respondents are asked to rate, on a 4-point Likert scale (0 = not at all and 3 = nearly every day), how often specific items have bothered them. Scores range from 0 to 27, with higher scores indicating greater symptoms of depression.31 This measure has been shown to be a reliable and valid measurement of depression in Spanish-speaking populations.32 The internal consistency of this measure in the present study was good (α = 0.86).
Data Analysis
A correlation matrix was conducted to examine associations among demographic characteristics and the mental health variables of anxiety, depression, satisfaction with life, and self-esteem to control for these possible associations where possible in follow-up analyses. A canonical correlation was then calculated to examine the pattern of associations between HRQOL and mental health variables. The purpose of a canonical correlation is to extract shared variance from two sets of variables to produce a correlation coefficient (r) that reflects common variance between the two sets, as well as standardized loadings indexing the degree to which the individual variables contribute to the overall relationship between the two sets. Four multiple regressions were then conducted to examine this pattern of connections in more detail, with one of the four mental health variables as the criterion variable in each. In the regressions, step 1 (if necessary) included any demographic variables shown in the correlation matrix to be associated with that regression's mental health criterion variable. Step 2 then included the four HRQOL variables of physical functioning, role–physical, pain, and general health.
Results
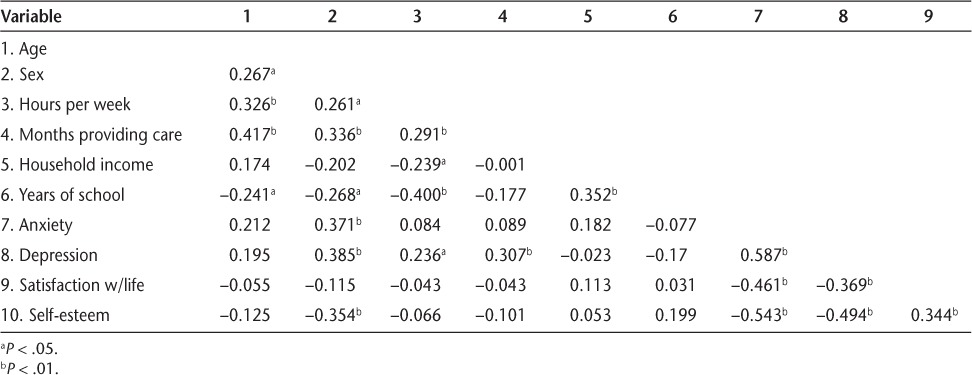
Correlation Matrix
A correlation matrix was calculated to examine associations between demographic characteristics (age, sex, hours per week spent caregiving, duration of caregiving, household income, and years of education) and mental health variables (anxiety, depression, satisfaction with life, and self-esteem) (Table 4). The purpose of this analysis was to identify demographic characteristics to control for in step 1 of each regression, where appropriate. Anxiety was positively associated with female sex. Depression was positively associated with female sex, hours per week spent caregiving, and duration of caregiving. Satisfaction with life was not associated with any demographic characteristics. Finally, male sex was the only demographic characteristic associated with self-esteem.
Table 4.
Correlations among demographic and criterion variables
Canonical Correlation
A canonical correlation was computed to examine which specific aspects of caregiver mental health were most linked to which specific aspects of HRQOL. Figure 1 illustrates the conceptual basis for and results of the first canonical correlation. In this figure, the canonical variates of shared variance in a single variable set (shown in circles) are derivations of the two sets of measured variables (shown in rectangles).
Figure 1.
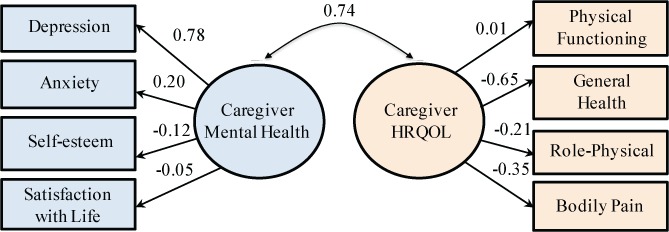
Conceptual model for the canonical correlation between mental health and health-related quality-of-life (HRQOL) variables
The variables in the circles are the two overall sets of variables, and each consists of four individual variables presented in rectangles. This figure captures the common variance between the two sets of variables and standardized canonical coefficients that demonstrate the contributions of the individual measured variables to the overall canonical correlation.
The first canonical correlation was 0.74 (52.7% overlapping variance) (λ = 0.41, χ216 = 67.37, P < .001). Based on Cohen standards, this correlation is considered a large effect size.33 Standardized canonical coefficients were calculated to examine the contributions of the individual measured variables to the overall canonical correlation. In the first canonical correlation, the standardized canonical coefficients for the caregiver mental health variables showed that depression loaded most highly (0.776), followed by anxiety (0.200), then by self-esteem (−0.122), and last by satisfaction with life (−0.047). Because the depression coefficient was above the traditional cutoff point of 0.40,34 depression was focused on for interpretation. For the HRQOL variables, general health loaded most highly (−0.648), followed by pain (−0.347), then role–physical (−0.213) and physical functioning (0.013). Similar to the mental health coefficients, only one variable, general health, was above the 0.40 cutoff point. This pattern of shared variance suggested that MS caregivers experienced more depression when they had worse general health, which was a unique effect beyond any other possible patterns of connections.
Regressions
Anxiety
The first hierarchical multiple regression tested whether HRQOL would be associated with anxiety after controlling for sex. Sex was entered into the first step of the regression, which was significant (F1,79 = 12.61, P = .001, R2 = 0.138). Inclusion of the second step with the four HRQOL variables (physical functioning, role–physical, pain, and general health) significantly increased the amount of variance explained in anxiety (ΔF4,75 = 5.29, P = .001, ΔR2 = 0.190). The overall model with both steps was significant (F5,75 = 7.30, P < .001, R2 = 0.327). In the overall model, none of the predictors were uniquely significant (P ≥ .056 for all).
Depression
The second hierarchical multiple regression examined whether HRQOL would be associated with depression after controlling for sex, hours per week spent caregiving, and duration of caregiving. The three demographic characteristics were entered into the first step and were significantly associated with depression (F3,77 = 6.18, P = .001, R2 = 0.194). Sex was uniquely associated with depression in this step (β = 0.298, P = .009). Addition of the second step with the four HRQOL variables significantly increased the amount of variance explained in depression (ΔF4,73 = 12.32, P < .001, ΔR2 = 0.325). The overall model with both steps was significant (F7,73 = 11.25, P < .001, R2 = 0.519). In the overall model, general health was a unique predictor of depression (β = −0.428, P = .002) such that lower general health was associated with higher depression. None of the other variables were uniquely associated with depression (P ≥ .063 for all).
Satisfaction with Life
The third regression examined whether HRQOL would be associated with satisfaction with life. None of the demographic characteristics were significantly correlated with satisfaction with life, so there was only one step in this regression. The four HRQOL variables were entered simultaneously, and the model was significant (F4,76 = 2.96, P = .025, R2 = 0.135). None of the HRQOL variables were uniquely associated with satisfaction with life (P ≥ .106 for all).
Self-esteem
The fourth hierarchical multiple regression tested whether HRQOL would be associated with self-esteem after controlling for sex. Sex was entered into the first step, which was significant (F1,79 = 11.29, P = .001, R2 = 0.268). Addition of the second step significantly increased the amount of variance explained in self-esteem (ΔF4,75 = 3.65, P = .009, ΔR2 = 0.143). The overall model with both steps was significant (F5,75 = 5.48, P < .001, R2 = 0.268). In the overall model, general health was a unique predictor of self-esteem (β = 0.467, P = .003) such that caregivers with better general health had higher self-esteem. None of the other HRQOL variables were uniquely associated with self-esteem (P ≥ .183 for all).
Discussion
The present study examined the associations between mental health and HRQOL in MS caregivers in Mexico. A canonical correlation analysis uncovered a large, significant overall association between mental health and HRQOL, with 52.7% of the variance shared between the two sets of constructs. When individual canonical loadings were examined in this analysis, the most substantial pattern that emerged was between depression and general health. Four regressions controlling for demographic variables found that HRQOL uniquely accounted for 19.0% of the variance in caregiver anxiety, 32.5% in depression, 13.5% in satisfaction with life, and 14.3% in self-esteem. Overall, the findings point to directions for future studies on interventions for MS caregivers, particularly in Mexican and other Latino populations.
Relations Between Mental Health and Caregiver Demographic Characteristics
Correlations demonstrated that anxiety, depression, and self-esteem were all associated with sex such that women experienced higher levels of anxiety and depression and lower self-esteem. These findings are supported by previous research, which suggests that being a female caregiver may be related to more negative psychological and physical outcomes compared with being a male caregiver, and may also be affected by differences in coping strategies.11,12,35–37 Also note that although MS caregivers are often men,38 nearly 67% of caregivers in the present study were women, which may be due to cultural and familial values that are tied to a division of labor such that women often take on the caregiving role.39 Depression was also positively associated with hours per week spent caregiving and total duration of caregiving, which is consistent with previous research, because those who have been in a caregiving role for longer are more likely to experience negative outcomes.7,13,40
Relations Between Mental Health and HRQOL
The canonical correlation revealed a large, significant association between mental health and HRQOL, suggesting the need for future research on interventions that target mental health and HRQOL concurrently because the two sets of variables were very highly related. In this analysis, depression and general health accounted for the largest amount of shared variance. The present study is in line with the previous literature demonstrating high rates of depression6,9 and poorer general health6–8 in MS caregivers. However, this was the first study to find that these two specific constructs were most closely related. This finding suggests that depression and general health could reciprocally influence each other and, as a result, could both be intervention targets.
Analyses were conducted to further explore the relation between mental health and general health. These regressions showed that caregiver HRQOL uniquely accounted for a substantial amount of variance in anxiety (19.0%), depression (32.5%), satisfaction with life (13.5%), and self-esteem (14.3%). Overall, these findings suggest that HRQOL and mental health significantly impact one another and, therefore, need to be studied and incorporated into interventions concurrently.
Despite the lack of previous research that has specifically examined the relation between these mental health variables and general quality of life, the findings herein are generally consistent with other research. For example, although no research on the HRQOL predictors of anxiety has been conducted in MS caregivers, similar research on dementia caregivers did find that physical morbidity is related to higher levels of anxiety,41 which is consistent with findings from the present study. Lower general health was found to be associated with higher depression. Again, although no research has specifically examined this association in MS caregivers, research combining multiple caregiving groups has found that caregivers have higher rates of clinician-rated depression than do noncaregivers, as well as poorer physical health,42 consistent with the present findings.
In terms of satisfaction with life, none of the individual predictors were uniquely significant, indicating that no single aspect of HRQOL is more important than any other in the prediction of MS caregiver satisfaction with life. Previous research with dementia caregivers found that caregiver HRQOL also predicted satisfaction with life, although only role–physical was a significant unique predictor in that study.43 General research on life satisfaction and HRQOL in American adults showed that as life satisfaction decreases, fair/poor general health, disability, physical distress, activity limitation, and pain increase.44 A plausible interpretation in the present study is that MS caregivers who are physically healthier have less to worry about and manage with their own health and, thus, have greater satisfaction with life, perhaps being able to focus more on caring for the individual with MS.
General health was also found to be a unique predictor of self-esteem, indicating that better general health was associated with higher self-esteem. Pinquart and Sörensen42 suggest that competence and confidence may be decreased when one takes on the role of caregiver and is tasked with additional stressors. Although little research has examined self-esteem in the context of MS caregivers, it seems reasonable to suggest that those who report better physical health feel more confident and have greater self-esteem, particularly in the context of caregiving roles and duties.
Limitations and Future Directions
Despite the implications of the present study, it has several limitations and, as a result, directions for future research. First, this study did not address relevant cultural factors and values, which are important constructs to consider regarding caregiving in Latino communities. This is particularly unfortunate because cultural context plays a central part in caregiver expectations, roles, and health.45 There is a dearth of research examining this topic in other countries, which makes it difficult to examine these results compared with other countries with more extensive research available to date on MS caregivers. As a result, future research should look to see whether these patterns differ compared with other cultures with different values, demographic features, and access to resources. The present study did not examine specific cultural constructs that may be unique to the sample surveyed, but they are critical to consider in the context of caregiver functioning in this population in future research.
Second, although this sample size is relatively large for the specific disease population, particularly in Mexico, there are limitations to conducting research with smaller sample sizes. Most importantly, the ability to detect significant differences is decreased and the ability to generalize findings to a larger population is reduced. A third limitation is the overlap that may have occurred between items included in the PHQ-9 and the SF-36, although we tried to reduce this overlap by removing the mental health items of the SF-36 from analyses. Similarly, the PHQ-9 includes somatic symptoms that may overlap with other measured variables. Previous research, however, has supported the notion that the PHQ-9 has only one factor,46 which is why all items were analyzed together as one in the present study.
A fourth limitation is that the present study did not collect information on or control for the medical conditions of caregivers. Although caregivers with neurologic disorders, psychiatric disorders, and severe developmental disabilities were excluded from the present study, specific information about caregiver medical status and previous diagnoses were not considered. This is an important variable to consider in future research given that it likely affects caregiver mental health and HRQOL. A final limitation to the present study is the date range from which references were retrieved. Several of the articles cited in the present study were published more than 10 years ago, which highlights the need for this research in understudied global regions. This is vital to the health of caregivers in these regions and, although a limitation, seems timely for the present study and future research. Finally, the cross-sectional nature of the study makes it correlational, and, as a result, causality cannot be inferred between HRQOL and mental health in this sample of MS caregivers. An alternative approach would have been to run the analyses again with the predictor and criterion variables flipped to examine any additional meaningful results. This alternative approach, however, would likely result in redundant findings. Future studies using cross-lagged panel designs can begin to uncover the potentially causal direction of the relationships found in the present study. With these limitations in mind, the findings demonstrated a strong association between HRQOL and mental health, which points to directions for future studies on interventions for MS caregivers, particularly in Mexican and other Latino populations.
Clinical Implications and Conclusions
The present study highlighted multiple significant associations between mental health and HRQOL that are important targets for interventions. In one study, 72% of caregivers surveyed reported that they would have trouble caring for the individuals with MS if their own health began to deteriorate,17 suggesting that caregiver HRQOL is important throughout the caregiving process. As shown in the present study, general health and depression were closely related, which suggests that these could be targeted concurrently using a biopsychosocial approach. These variables may be operating reciprocally such that the improvement of one may also lead to an improvement in the other, although this assertion needs to be supported in future research.
Previous research on Latino cultural values may point to culturally informed interventions for MS caregivers, particularly in Mexican and other Latino populations. For example, Latino culture typically emphasizes a collectivist orientation, which influences caregiver obligations.47 In Latin America, familismo is a value that individuals show loyalty and support and express solidarity toward an ill or injured family member.48,49 Latino caregivers also often face role engulfment, which is the loss of one's sense of self and identity due to immersion in the caregiving role.50,51 Dilworth-Anderson et al.50 posited that role engulfment is extremely prevalent in Latino families because of perceived obligations surrounding supporting ill family members. Thus, helping MS caregivers in Latin America draw on their collectivist roots to involve other family members in the caregiving process may reduce the burden of care and, as a result, caregiver depression and general health problems, both shown to be particularly prominent in the present study.
PracticePoints.
Health-care providers should target MS caregiver health-related quality of life and mental health concurrently through a biopsychosocial approach because these sets of variables were strongly associated with one another in the present study.
Caregiver general health and depression may be particularly important to screen for and focus on to improve the overall health of caregivers.
Footnotes
Financial Disclosures: The authors have no conflicts of interest to disclose.
References
- 1.World Health Organization, Multiple Sclerosis International Federation. Atlas: Multiple Sclerosis Resources in the World. Geneva, Switzerland: World Health Organization; 2008. [Google Scholar]
- 2.Corona T, Roman GC. Multiple sclerosis in Latin America. Neuroepidemiology. 2006;26:1–3. doi: 10.1159/000089230. [DOI] [PubMed] [Google Scholar]
- 3.Cordova J, Vargas S, Sotelo J. Western and Asian features of multiple sclerosis in Mexican Mestizos. Clin Neurol Neurosurg. 2007;109:146–151. doi: 10.1016/j.clineuro.2006.07.006. [DOI] [PubMed] [Google Scholar]
- 4.Gonzalez O, Sotelo J. Is the frequency of multiple sclerosis increasing in Mexico? J Neurol Neurosurg Psychiatry. 1995;59:528–530. doi: 10.1136/jnnp.59.5.528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.O'Hara L, De Souza L, Ide L. The nature of care giving in a community sample of people with multiple sclerosis. Disabil Rehabil. 2004;26:1401–1410. doi: 10.1080/09638280400007802. [DOI] [PubMed] [Google Scholar]
- 6.Argyriou AA, Karanasios P, Ifanti AA et al. Quality of life and emotional burden of primary caregivers: a case-control study of multiple sclerosis patients in Greece. Qual Life Res. 2011;20:1663–1668. doi: 10.1007/s11136-011-9899-2. [DOI] [PubMed] [Google Scholar]
- 7.Aronson KJ. Quality of life among persons with multiple sclerosis and their caregivers. Neurology. 1997;48:74–80. doi: 10.1212/wnl.48.1.74. [DOI] [PubMed] [Google Scholar]
- 8.Giordano A, Ferrari G, Radice D, Randi G, Bisanti L, Solari A. Health-related quality of life and depressive symptoms in significant others of people with multiple sclerosis: a community study. Eur J Neurol. 2012;19:847–854. doi: 10.1111/j.1468-1331.2011.03638.x. [DOI] [PubMed] [Google Scholar]
- 9.Knight RG, Devereux RC, Godfrey HP. Psychosocial consequences of caring for a spouse with multiple sclerosis. J Clin Exp Neuropsychol. 1997;19:719. doi: 10.1080/01688639708403832. [DOI] [PubMed] [Google Scholar]
- 10.McKeown L, Porter-Armstrong A, Baxter G. The needs and experiences of caregivers of individuals with multiple sclerosis: a systematic review. Clin Rehabil. 2003;17:234–248. doi: 10.1191/0269215503cr618oa. [DOI] [PubMed] [Google Scholar]
- 11.Pakenham KI. Application of a stress and coping model to caregiving in multiple sclerosis. Psychol Health Med. 2001;6:13–27. [Google Scholar]
- 12.Rivera-Navarro J, Manuel Morales-González J, Benito-León J. Informal caregiving in multiple sclerosis patients: data from the Madrid Demyelinating Disease Group study. Disabil Rehabil. 2003;25:1057–1064. doi: 10.1080/0963828031000137766. [DOI] [PubMed] [Google Scholar]
- 13.Buhse M. Assessment of caregiver burden in families of persons with multiple sclerosis. J Neurosci Nurs. 2008;40:25–31. doi: 10.1097/01376517-200802000-00005. [DOI] [PubMed] [Google Scholar]
- 14.Khan F, Pallant J, Brand C. Caregiver strain and factors associated with caregiver self-efficacy and quality of life in a community cohort with multiple sclerosis. Disabil Rehabil. 2007;29:1241–1250. doi: 10.1080/01443610600964141. [DOI] [PubMed] [Google Scholar]
- 15.Buchanan R, Huang C. Health-related quality of life among informal caregivers assisting people with multiple sclerosis. Disabil Rehabil. 2011;33:113–121. doi: 10.3109/09638288.2010.486467. [DOI] [PubMed] [Google Scholar]
- 16.Nanda U, Andresen EM. Health-related quality of life: a guide for the health professional. Eval Health Prof. 1998;21:179–215. doi: 10.1177/016327879802100204. [DOI] [PubMed] [Google Scholar]
- 17.Wollin JA, Sato A. An international comparison of caregiver burden in multiple sclerosis. Australas J Neurosci. 2001;14:21–25. [Google Scholar]
- 18.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36), I: conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 19.Ware JE, Kosinski M, Dewey JE, Gandek B. SF-36 Health Survey: Manual and Interpretation Guide. Lincoln, RI: Quality Metric Inc; 2000. [Google Scholar]
- 20.Alonso J, Prieto L, Anto J. The Spanish version of the SF-36 Health Survey (the SF-36 health questionnaire): an instrument for measuring clinical results. Med Clin (Barc) 1995;104:771–776. [PubMed] [Google Scholar]
- 21.Diener E, Emmons RA, Larsen RJ, Griffin S. The satisfaction with life scale. J Pers Assess. 1985;49:71–75. doi: 10.1207/s15327752jpa4901_13. [DOI] [PubMed] [Google Scholar]
- 22.Pavot W, Diener E. Review of the satisfaction with life scale. Psychol Assess. 1993;5:164–172. [Google Scholar]
- 23.Pons D, Atienza FL, Balaguer I, Garcia-Merita ML. Satisfaction With Life Scale: analysis of factorial invariance for adolescents and elderly persons. Percept Mot Skills. 2000;91:62–68. doi: 10.2466/pms.2000.91.1.62. [DOI] [PubMed] [Google Scholar]
- 24.Spielberger CD. Manual for the State-Trait Anxiety Inventory STAI (Form Y) (“Self-evaluation Questionnaire”) Palo Alto, CA: Consulting Psychologists Press; 1983. [Google Scholar]
- 25.Spielberger CD, Díaz-Guerrero RI. Inventario de Ansiedad: Rasgo-Estado. México: El Manual Moderno; 1975. [Google Scholar]
- 26.Novy DM, Nelson DV, Smith KG, Rogers PA, Rowzee RD. Psychometric comparability of the English- and Spanish-language versions of the State-Trait Anxiety Inventory. Hisp J Behav Sci. 1995;17:209–224. [Google Scholar]
- 27.Rosenberg M. Society and the Adolescent Self-image. Princeton, NJ: Princeton University Press; 1965. [Google Scholar]
- 28.Schmitt DP, Allik J. Simultaneous administration of the Rosenberg Self-Esteem Scale in 53 nations: exploring the universal and culture-specific features of global self-esteem. J Pers Soc Psychol. 2005;89:623–642. doi: 10.1037/0022-3514.89.4.623. [DOI] [PubMed] [Google Scholar]
- 29.Anson K, Ponsford J. Coping and emotional adjustment following traumatic brain injury. J Head Trauma Rehabil. 2006;21:248–259. doi: 10.1097/00001199-200605000-00005. [DOI] [PubMed] [Google Scholar]
- 30.Gray-Little B, Williams VS, Hancock TD. An item response theory analysis of the Rosenberg Self-Esteem Scale. Pers Soc Psychol Bull. 1997;23:443–451. [Google Scholar]
- 31.Kroenke K, Spitzer RL, Williams JB. The PHQ-9. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Diez-Quevedo C, Rangil T, Sanchez-Planell L, Kroenke K, Spitzer RL. Validation and utility of the patient health questionnaire in diagnosing mental disorders in 1003 general hospital Spanish inpatients. Psychosom Med. 2001;63:679–686. doi: 10.1097/00006842-200107000-00021. [DOI] [PubMed] [Google Scholar]
- 33.Cohen J. Statistical Power Analysis for the Behavioral Sciences. New York, NY: Academic Press; 2013. [Google Scholar]
- 34.Tabachnick B, Fidell L. Using Multivariate Statistics. Vol 3. Boston, MA: Pearson/Allyn & Bacon; 2007. Multivariate analysis of variance and covariance; pp. 402–407. [Google Scholar]
- 35.DesRosier MB, Catanzaro M, Piller J. Living with chronic illness: social support and the well spouse perspective. Rehabil Nurs. 1992;17:87–91. doi: 10.1002/j.2048-7940.1992.tb01519.x. [DOI] [PubMed] [Google Scholar]
- 36.Gulick EE. Coping among spouses or significant others of persons with multiple sclerosis. Nurs Res. 1995;44:220–225. [PubMed] [Google Scholar]
- 37.Patti F, Amato MP, Battaglia M et al. Caregiver quality of life in multiple sclerosis: a multicentre Italian study. Mult Scler. 2007;13:412–419. doi: 10.1177/1352458506070707. [DOI] [PubMed] [Google Scholar]
- 38.Kristjanson LJ, Aoun SM, Yates P. Are supportive services meeting the needs of Australians with neurodegenerative conditions and their families? J Palliat Care. 2005;22:151–157. [PubMed] [Google Scholar]
- 39.De La Luz Ibarra M. The tender trap: Mexican immigrant women and the ethics of elder care work. Atzlan. 2003;28:87–113. [Google Scholar]
- 40.Buchanan RJ, Radin D, Huang C. Burden among male caregivers assisting people with multiple sclerosis. Gend Med. 2010;7:637–646. doi: 10.1016/j.genm.2010.11.009. [DOI] [PubMed] [Google Scholar]
- 41.Schulz R, O'Brien AT, Bookwala J, Fleissner K. Psychiatric and physical morbidity effects of dementia caregiving: prevalence, correlates, and causes. Gerontologist. 1995;35:771–791. doi: 10.1093/geront/35.6.771. [DOI] [PubMed] [Google Scholar]
- 42.Pinquart M, Sörensen S. Differences between caregivers and noncaregivers in psychological health and physical health: a meta-analysis. Psychol Aging. 2003;18:250–267. doi: 10.1037/0882-7974.18.2.250. [DOI] [PubMed] [Google Scholar]
- 43.Perrin PB, Morgan M, Aretouli E et al. Connecting health-related quality of life and mental health in dementia caregivers from Colombia, South America. J Alzheimers Dis. 2014;39:499–509. doi: 10.3233/JAD-130764. [DOI] [PubMed] [Google Scholar]
- 44.Strine TW, Chapman DP, Balluz LS, Moriarty DG, Mokdad AH. The associations between life satisfaction and health-related quality of life, chronic illness, and health behaviors among US community-dwelling adults. J Community Health. 2008;33:40–50. doi: 10.1007/s10900-007-9066-4. [DOI] [PubMed] [Google Scholar]
- 45.Akkus Y. Multiple sclerosis patient caregivers: the relationship between their psychological and social needs and burden levels. Disabil Rehabil. 2011;33:326–333. doi: 10.3109/09638288.2010.490866. [DOI] [PubMed] [Google Scholar]
- 46.Baas KD, Cramer AO, Koeter MW, van de Lisdonk EH, van Weert HC, Schene AH. Measurement invariance with respect to ethnicity of the Patient Health Questionnaire-9 (PHQ-9) J Affect Disord. 2011;129:229–235. doi: 10.1016/j.jad.2010.08.026. [DOI] [PubMed] [Google Scholar]
- 47.Triandis HC. Individualism and Collectivism. Boulder, CO: Westview Press; 1995. [Google Scholar]
- 48.Delgado M, Tennstedt S. Making the case for culturally appropriate community services: Puerto Rican elders and their caregivers. Health Soc Work. 1997;22:246–255. doi: 10.1093/hsw/22.4.246. [DOI] [PubMed] [Google Scholar]
- 49.Napoles AM, Chadiha L, Eversley R, Moreno-John G. Developing culturally sensitive dementia caregiver interventions: are we there yet? Am J Alzheimers Dis Other Demen. 2010;25:389–406. doi: 10.1177/1533317510370957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dilworth-Anderson P, Williams IC, Gibson BE. Issues of race, ethnicity, and culture in caregiving research: a 20-year review (1980–2000) The Gerontologist. 2002;42:237–272. doi: 10.1093/geront/42.2.237. [DOI] [PubMed] [Google Scholar]
- 51.Skaff MM, Pearlin LI. Caregiving: role engulfment and the loss of self. Gerontologist. 1992;32:656–664. doi: 10.1093/geront/32.5.656. [DOI] [PubMed] [Google Scholar]


