Abstract
Background: People with multiple sclerosis (MS) fall frequently. In 2011, the National Multiple Sclerosis Society launched a multifactorial fall-prevention group exercise and education program, Free From Falls (FFF), to prevent falls in MS. The objective of this study was to assess the impact of participation in the FFF program on balance, mobility, and falls in people with MS.
Methods: This was a retrospective evaluation of assessments from community delivery of FFF. Changes in Activities-specific Balance Confidence scale scores, Berg Balance Scale scores, 8-foot Timed Up and Go performance, and falls were assessed.
Results: A total of 134 participants completed the measures at the first and last FFF sessions, and 109 completed a 6-month follow-up assessment. Group mean scores on the Activities-specific Balance Confidence scale (F1,66 = 17.14, P < .05, η2 = 0.21), Berg Balance Scale (F1,68 = 23.39, P < .05, η2 = 0.26), and 8-foot Timed Up and Go (F1,79 = 4.83, P < .05, η2 = 0.06) all improved significantly from the first to the last session. At the 6-month follow-up, fewer falls were reported (χ2 [4, N = 239] = 10.56, P < .05, Phi = 0.21).
Conclusions: These observational data suggest that the FFF group education and exercise program improves balance confidence, balance performance, and functional mobility and reduces falls in people with MS.
Multiple sclerosis (MS) impairs cognition, muscle strength, muscle tone, sensation, balance, coordination, and gait, all of which are associated with an increased risk of falls. People with MS are also known to fall frequently. More than 50% of people with MS fall in a 3- to 6-month period, and 30% to 50% fall multiple times.1 These falls have adverse consequences. More than 50% of people with MS have been injured by a fall,2–5 and falls in people with MS are associated with loss of confidence and independence, social isolation,6 curtailment of activities,7 risk of more falls,8 and increased use of health-care services.9 Despite falls being common and having significant adverse consequences in people with MS, until recently there has been little research on fall prevention in this population.
Older adults also fall frequently and experience significant adverse consequences from falls. Approximately 30% of older adults fall per year, often resulting in significant injury and curtailment of activity. Fall prevention in older adults has received substantial attention and resources following publication of a fall-prevention guideline for older adults in 2001.10 This guideline recommends addressing the multiple causes of falls with multifactorial interventions, and various multifactorial programs have been developed to implement fall-prevention strategies in older adults.
Given the many similarities between fall risk, fall risk factors, and fall consequences in older adults and people with MS, the National Multiple Sclerosis Society (NMSS) adapted the Oasis Institute's Free From Falls program for fall prevention in older adults to produce the first MS-specific comprehensive fall-prevention program. The Oasis program was chosen because it is multifactorial and includes fall education, exercise, and assessment of outcomes. Oasis' Free From Falls has 28 lay-led 1- to 2-hour sessions with an overview of prevalence and risk factors for falls in older adults; how to ameliorate fall risks and hazards at home; an evidence-based program to address the physical, social, and cognitive issues associated with falls; and exercises to address the physical and sensory needs of older adults to decrease fall risk and prevent falls.11 Oasis allowed the NMSS to use and adapt all the components of their program for free, including its name. The NMSS adapted the program for people with MS by adding information about fatigue and management of energy and body temperature, which are unique considerations for people with MS, and condensing the program to an eight-session, weekly 2-hour group program, with each session including an hour of education followed by an hour of exercise. The NMSS also called their program Free From Falls (FFF).12
The NMSS FFF program is designed to increase awareness of fall prevalence and risk factors in MS, create fall-prevention strategies, develop a personal fall-prevention action plan, increase fall prevention and management confidence, identify community fall-prevention resources, and engage participants in motor and sensory exercises to reduce fall risk. The components of the program align with recommendations from researchers in the field and the International MS Falls Prevention Research Network that fall-prevention programs include information on environment modification (removing hazards, improving lighting), evaluation and adaptation of activity demands, training in the use of compensatory strategies (using a mobility device), and practice of exercises focused on sensory and motor strategies to improve balance.13–15 Assessments of walking and balance are also included in the NMSS version of FFF to show participant progress.
The NMSS FFF program was introduced and disseminated to the community through its chapters and was piloted by 19 chapters in 2011. In addition to the three tests that were components of the program, the NMSS also contacted participants 6 months after the program to ask how many times they had fallen in the 6 months since the program. This study evaluated changes in performance on the three tests administered to participants during the first and last sessions in this community administration of the program and evaluated for changes in the number of falls from the beginning of the program to 6 months later. We hypothesized that participants in FFF would show significantly improved self-reported and objectively measured balance and mobility at the end of the program and fewer falls 6 months after the program compared with baseline at the beginning of the program.
Methods
People with MS were recruited to participate in FFF by 19 NMSS chapters across the United States between September 2011 and May 2012. People were recruited by paper flyers, website advertisements, newsletters, and personal mailings. Participation required a physician-verified diagnosis of MS and a signed release. Participants had to be able to walk with unilateral assistance or without assistive devices and were asked to pay $25 to $75 for the 8-week program; NMSS chapters provided scholarships for those unable to pay.
The FFF Program
The NMSS FFF weekly program addresses falls using a multifactorial approach combining education and exercise to minimize the risk of falls in people with MS. The FFF program is designed for groups of approximately 10 to 15 participants. The program consists of eight sessions, each with 1 hour of fall-prevention education followed by 1 hour of exercises focused on sensory and motor strategies to improve balance. The education portion of the classes was facilitated by lay NMSS staff members, an occupational therapist, or a nurse. The education covered the following topics: week 1, causes of falls and understanding balance; week 2, fear of falling, center of gravity, and multisensory training; week 3, optimizing mobility, gait, and flexibility; week 4, managing energy, strength, and endurance; week 5, safety at home and functional fitness; week 6, safety in the community; week 7, recovering from falls and personal fitness; and week 8, putting it all together. Some chapters used mental health professionals to facilitate the “fear of falling” session. The exercise portion was facilitated by a physical therapist. Exercises included warm-up, balance practice, sensory fine-tuning, functional activities, strengthening, and cooldown. Exercises were demonstrated by program instructors and were the same each week, except for options for progression over time. Participants were encouraged to perform the exercises at home between sessions and after program completion. Facilitator manuals from the NMSS include all the instructions for organizing the program, presenting educational and background materials, and performing the standardized outcome testing. Printed materials for the participants include all the information presented, exercise instructions, and homework assignments.12
Outcome Measures
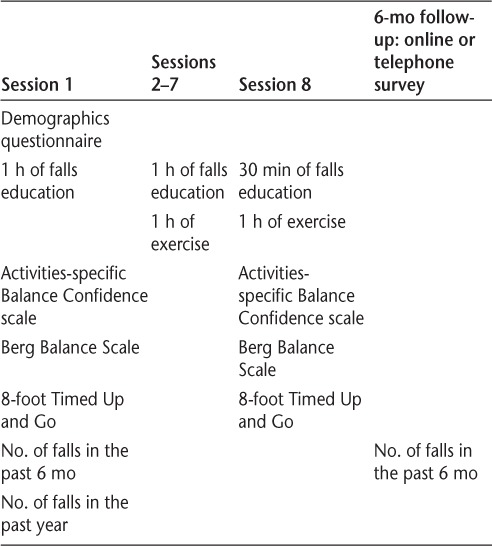
At the first session, participants were asked how often they fell in the previous 6 months, and they completed the 8-foot Timed Up and Go (TUG), the Berg Balance Scale (BBS), and the Activities-specific Balance Confidence (ABC) scale, which provide objective assessment of mobility and balance and self-report of balance confidence, respectively. The TUG, BBS, and ABC scale were repeated at the end of the final FFF session (Table 1). The TUG was also included in the OASIS version of FFF. The TUG and the BBS were administered and scored by the program facilitators; the ABC scale is a self-report questionnaire. These measures have been shown to be valid and reliable in people with MS.16,17
Table 1.
Sequence and timing of activities including Free From Falls sessions and outcome assessments
The ABC scale is a self-report questionnaire that rates balance confidence on a scale from 0 (no confidence) to 100 (fully confident) for 16 daily activities that incorporate static, dynamic, proactive, and reactive balance. The ABC scale's concurrent convergent validity in people with MS has been reported to be moderate to good (0.50 to −0.75), with six balance and walking performance tests, participants' retrospective fall history, a validated walking impairment scale, and use of assistive devices.16,18 The ABC scale discriminated between multiple fallers and nonfallers with MS, and its internal consistency is high (α = 0.95), with interitem correlations between 0.30 and 0.83.16 The ABC scale was completed directly by the participants. Only a final score for this scale was recorded during the FFF program, and, therefore, its reliability in this study was not assessed.
The BBS is a clinician-rated scale of 14 static and dynamic balance tasks ranging in difficulty from unsupported sitting to single-limb standing, each of which is rated from 0 (cannot perform) to 4 (normal performance). The test-retest reliability of the BBS is high in ambulatory individuals with MS (intraclass correlation coefficient [ICC] = 0.96),19 and its internal consistency in this study was also high (Cronbach α = 0.87). The BBS has been reported to identify fallers with MS using cutoff scores of 4516 or 54.8 The program facilitators administered the BBS.
The 8-foot TUG measures the time it takes to rise from a chair, walk 8 feet, turn around, and return to sit in the chair.20 Participants performed this test twice at each test session, and the best performance was used for analysis. The original TUG test uses a 10-foot or 3-m walk.21 Cutoff times for the TUG to identify fallers with MS have not been published. The test-retest reliability of the TUG for people with MS with Expanded Disability Status Scale scores greater than 422 or 5.0 to 6.5 are high (ICCs = 0.88 and 0.97, respectively),19,23 and its internal consistency is high (Cronbach α = 0.88). The program facilitators administered the 8-foot TUG.
At session 1, participants also reported demographics (age, sex, date of diagnosis) and number of falls in the previous 6 months and 1 year (categorized as 0, 1–3, 4–6, 7–10, ≥11 falls). At session 8, participants repeated the ABC scale, the BBS, and the 8-foot TUG. Six months after FFF, participants completed an online or telephone survey about falls in the previous 6 months (Table 1).
The institutional review board at Oregon Health & Science University (Portland) determined that this retrospective analysis of de-identified data was not human subject research, and it was, therefore, exempt from institutional review board approval.
Statistical Analysis
Because not all participants who completed FFF completed the 6-month follow-up assessment, χ2 tests or analyses of variance were conducted to determine statistically significant differences in demographic and other baseline variables between those who completed only sessions 1 and 8 and those who also completed 6-month follow-up measures. Variables found to differ statistically significantly between the groups were included as covariates in the analyses of the outcome measures.
The effects of FFF on the outcome measures were assessed by repeated-measures analysis of variance, with the time points as the within-subjects factors, including significant covariates. A χ2 test was performed to assess the impact of FFF on the proportion of fallers (≥1 falls) and nonfallers (no falls) in the previous 6 months at baseline and at the 6-month follow-up. Assumption testing was conducted on all the outcome variables before these analyses, and no significant violations were found.
Results
Demographic Characteristics
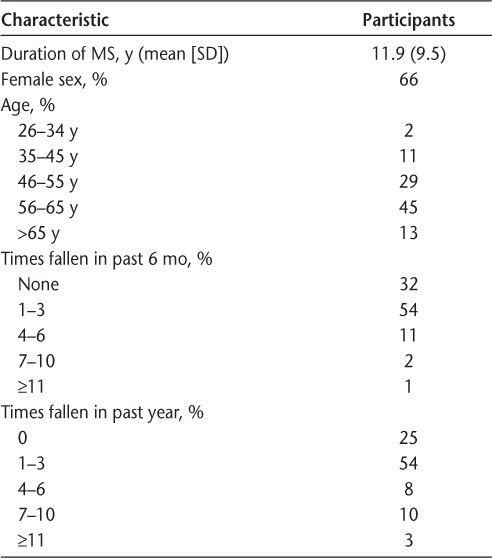
A total of 134 participants completed the measures at sessions 1 and 8, and 109 completed the 6-month follow-up assessment. Of the 134 participants completing sessions 1 and 8, 66% were women; the age range was 26 to older than 65 years, with 58% being older than 55 years. Participants had MS for a mean of 11.91 years (Table 2).
Table 2.
Baseline characteristics of the 134 Free From Falls participants
These 134 participants attended classes of 6 to 14 people in urban and rural locations around Birmingham, Alabama; Bakersfield, Fresno, Los Angeles, Palo Alto, Rancho Mirage, and Santa Barbara, California; Orlando, Florida; Boston, Massachusetts; St. Paul, Minnesota; St. Louis, Missouri; New York City and Pittsford, New York; Raleigh, North Carolina; Scranton and Sewicky, Pennsylvania; St. George, Utah; and Manassas and Charlottesville, Virginia.
Preliminary analysis demonstrated that at baseline, those who completed the 6-month follow-up assessment reported more falls in the past year than those who did not complete the 6-month follow-up assessment (P < .05). Therefore, falls in the past year was included as a covariate in the outcome analyses. There were no significant differences in demographics or in ABC scale, BBS, or 8-foot TUG scores at baseline between individuals completing and not completing the 6-month follow-up assessment (P > .05).
Outcomes at Completion of FFF
Group mean scores on the ABC scale, BBS, and 8-foot TUG all improved significantly from session 1 to session 8, demonstrating improvements in participants' balance confidence, balance performance, and mobility.
Specifically, for the ABC scale, there was a significant and strong24 main effect (F1,66 = 17.14, P < .05, η2 = 0.21), indicating that participants' balance confidence increased (mean ± SD: from 54.80 ± 19.81 to 66.93 ± 17.40). For the BBS, there was a significant and strong main effect (F1,68 = 23.39, P < .05, η2 = 0.26), indicating that participants' objectively measured balance performance improved (mean ± SD: from 47.44 ± 6.90 to 51.36 ± 5.12). For the 8-foot TUG, there was a significant and moderate main effect (F1,79 = 4.83, P < .05, η2 = 0.06), indicating improved functional mobility (mean ± SD: from 11.22 ± 4.78 seconds to 10.09 ± 4.17 seconds) (Figure 1).
Figure 1.
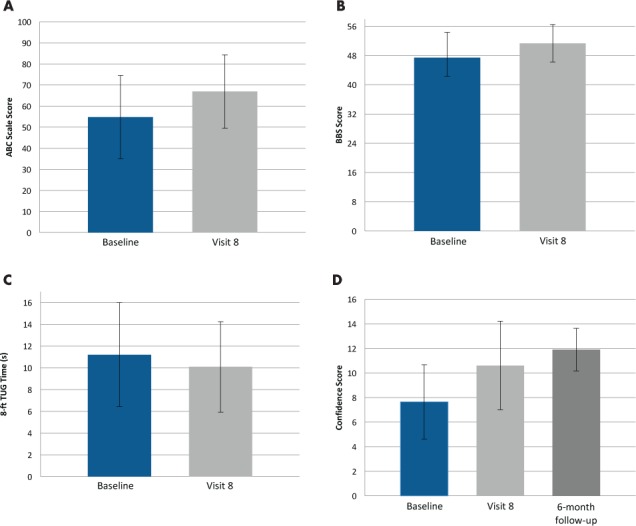
Changes in mean ± SD balance and mobility scores between the first (baseline) and last (visit 8) sessions of the Free From Falls program
A, Activities-specific Balance Confidence (ABC) scale scores increased from 54.8 ± 19.8 to 66.9 ± 17.4 (P < .05). B, Berg Balance Scale (BBS) scores increased from 47.4 ± 6.9 to 51.4 ± 5.1 (P < .05). C, The 8-foot Timed Up and Go (TUG) scores decreased from 11.2 ± 4.8 to 10.1 ± 4.2 seconds (P < .05). D, Fall Prevention Confidence scores increased from 7.7 ± 3.0 (baseline) to 10.6 ± 3.6 (visit 8) to 11.9 ± 1.7 (6-month follow-up).
Outcomes 6 Months After FFF
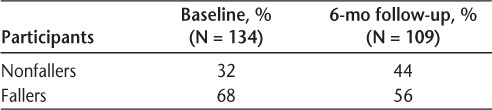
Six months after the FFF program, fewer falls were reported (χ2 [4, N = 239] = 10.56, P < .05, Phi = 0.21). Twelve percent more participants were nonfallers in the past 6 months compared with baseline (P < .10) (Table 3).
Table 3.
Proportion of fallers and nonfallers in the past 6 months at baseline and at 6-month follow-up after the Free From Falls program
Discussion
Participants in the MS FFF multifactorial fall-prevention group exercise and education program improved their balance and functional mobility and had fewer falls. At completion of FFF, self-reported balance confidence, objectively measured balance performance, and functional mobility were significantly improved from baseline, and 6 months later, fewer falls were reported. These findings suggest that FFF may have significant short- and long-term benefits.
Self-reported balance confidence improved, as reflected by a 12-point increase on the ABC scale from 55 to 67, from the beginning to the end of FFF. These scores are similar to previously reported ABC scale scores for people with MS.16,25 The baseline and follow-up scores are better (higher) than the only reported cutoff value of 40 for identifying fallers with MS.16 This suggests that the balance confidence of our sample was likely representative of the population of people with MS and that their balance improved.
Objectively measured balance improved, as reflected by a 4-point increase on the BBS from 47 to 51 from the beginning to the end of FFF. These scores lie between previously identified cutoff scores of 4516 and 548 reported to identify fallers with MS. Previous studies in people with MS have found a ceiling effect with the BBS,8,16,26 and the BBS intrinsically has a floor effect because it cannot measure balance in people unable to sit without support. The minimal detectable change for the BBS in people with MS has been reported to be 3 to 7 points.19 The improvement of 4 points after FFF lies within the reported minimal detectable change for people with MS, suggesting small but important improvements in balance comparable with previous studies.
Objectively measured functional mobility improved, as reflected by a 1-second decrease on the 8-foot TUG from 11 to 10 seconds from the beginning to the end of FFF. This is equivalent to a change from 13.75 to 12.5 seconds on the more commonly performed 10-foot TUG. This initial time is within the range reported previously in a cohort of people with MS23 and much shorter than the 22 seconds for the 10-foot TUG reported in a more disabled group of people with MS.19 This small but statistically significant improvement in the 8-foot TUG score over the 8 weeks of the FFF program is encouraging, although this change is not as high as the published 23% to 24% required to demonstrate a genuine improvement in TUG performance in people with MS.23 Furthermore, because FFF focuses on preventing falls and improving balance, some participants may walk more slowly during the TUG test to improve their safety, particularly because the TUG test instructions are to use a safe and comfortable walking speed. Program participants may be able to walk more safely and more quickly if they continue to implement the home exercise program, but these changes may take longer than 8 weeks to occur.
This study showed a decrease in falls from baseline to the 6-month follow-up (P < .05) and a decrease in the number of fallers that approached statistical significance (P < .10). These results are encouraging, particularly 6 months after the program. Only two studies have reported on the impact of exercise programs on falls in people with MS, and there are no previous published reports on the impact of education programs on falls in MS. In a pilot study with 44 people, Cattaneo et al.27 found that one-on-one treatment with conventional physical therapy, a balance program with motor strategy training alone, or a balance program with motor and sensory strategy training all resulted in fewer falls and fewer fallers, but the combination of motor and sensory strategy training was most effective. Including motor and sensory strategy training in the exercise component of FFF may have contributed to the reduction in falls observed in the present study.28 A larger study by Coote et al.29 with 111 people with MS who all used bilateral assistance to ambulate outdoors found that group physical therapy focused on balance and strength exercises but not one-on-one physical therapy or yoga resulted in fewer falls and fewer fallers. The group exercise in FFF may have contributed to its benefits for fall prevention. A small study of 30 people with MS found that a fall-prevention education program increased knowledge of fall risk factors, increased knowledge and skills to manage falls and fall risk, and promoted changes in behavior to reduce personal fall risk, but the impact of this program on falls has not been published.13
The present study has several strengths. This is an important first step in evaluating this fall-prevention program adapted from evidence-based information designed to decrease falls in older adults. The sample was large and geographically diverse, including more than 100 people with MS from around the United States. The participant demographics were representative of people with MS: participants were mostly women older than 45 years, and most were not employed. The retrospective observational nature of this study allowed us to evaluate the effectiveness of the FFF program under real-world conditions rather than under the optimized conditions of a clinical trial. In addition, data were available directly after the FFF program and 6 months later, allowing for assessment of sustained benefits of the program.
This study also has several limitations characteristic of most analyses of observational data. Because the data were collected as part of a clinical program and not from a preplanned prospectively designed research study, there are many missing data that may have resulted in ascertainment bias. There was no alternative intervention to control for potential nonspecific effects of the socialization and attention associated with attending FFF or for the effects of the current standard of care for falls in people with MS. Outcome measures were limited to objective measures of balance and walking, self-reports of balance at completion of the program, and self-reports of previous falls 6 months after the program. The accuracy of fall counts is limited by recall bias associated with assessing falls retrospectively for the previous 6 months, and the precision of these fall counts is limited by broad categorization of fall counts. Requiring people to pay to participate in the program has unknown effects. This may have been a deterrent to participation, although NMSS policy is that no one is ever excluded from a program if they are unable to pay the fee. However, payment may have encouraged greater adherence and attendance because of the investment. The results of this study may not generalize to provision of the program for free or to a randomized controlled trial where people are generally paid to participate.
Although this study has many limitations, it is important to understand that the NMSS FFF program, although derived from evidence, similar to many self-management programs in wide distribution and use for many conditions, currently does not have high-quality evidence to support benefit. The study presented herein is an early step in evaluating this program's effectiveness and suggests that the NMSS FFF program prevents falls in people with MS. Although randomized controlled trials of this program that include comparison with an appropriate control intervention, full follow-up of all enrolled participants, objective prospective counting of falls, and measures of participation, quality of life, and fall-related injuries are needed to definitively assess the impact of this and other fall-prevention programs in MS,14,15 this study suggests that the program is clinically beneficial for patients with MS.
Conclusion
This study suggests that the FFF multifactorial fall-prevention group exercise and education program may improve balance and prevent falls in people with MS and that this and similar programs are, therefore, likely to be clinically helpful for people with MS at risk for falls. The FFF program should be subjected to a large randomized controlled trial with falls as the primary outcome to determine effectiveness and, therefore, value in people with MS. Having a proven program to prevent falls is important for health-related quality of life in people living with MS, their health-care providers, and society owing to the high cost of falls.
PracticePoints.
Falls are common in people with MS and result in substantial physical and psychosocial consequences.
People with MS who participated in the Free From Falls multifactorial fall-prevention group exercise and education program demonstrated improved balance and functional mobility and had fewer falls after completing the program.
Well-designed randomized controlled trials are needed to definitively determine whether the Free From Falls program prevents falls and improves participation and quality of life in people with MS.
Acknowledgments
We are grateful to the patients with MS and the NMSS staff members who participated in the FFF program. We also thank Charles Murchison for reviewing the statistical analyses, Dennis Bourdette for reviewing the manuscript, and Kristina Wick for help preparing the manuscript for submission.
Footnotes
Financial Disclosures: The authors have no conflicts of interest to disclose.
Funding/Support: Two of the authors (MC and CLH) were supported by funding from the VA Rehabilitation Research & Development Service during preparation of this work. The NMSS FFF program was made possible by unrestricted grants from Acorda Therapeutics, Biogen Idec, Genentech, and Teva Neuroscience. This research received no specific grants from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Gunn HJ, Newell P, Haas B, Marsden JF, Freeman JA. Identification of risk factors for falls in multiple sclerosis: a systematic review and meta-analysis. Phys Ther. 2013;93:504–513. doi: 10.2522/ptj.20120231. [DOI] [PubMed] [Google Scholar]
- 2.Gunn HJ, Creanor S, Haas B, Marsden J, Freeman J. Risk-factors for falls in multiple sclerosis: an observational study. Mult Scler J. 2013;19:1913–1922. doi: 10.1177/1352458513488233. [DOI] [PubMed] [Google Scholar]
- 3.Peterson EW, Cho CC, von Koch L, Finlayson ML. Injurious falls among middle aged and older adults with multiple sclerosis. Arch Phys Med Rehabil. 2008;89:1031–1037. doi: 10.1016/j.apmr.2007.10.043. [DOI] [PubMed] [Google Scholar]
- 4.Cameron MH, Lord S. Postural control in multiple sclerosis: implications for fall prevention. Curr Neurol Neurosci Rep. 2010;10:407–412. doi: 10.1007/s11910-010-0128-0. [DOI] [PubMed] [Google Scholar]
- 5.Bazelier MT, Van Staa T, Uitdehaag BMJ, Cooper C, Leufkens HGM, Vestergaard P. The risk of fracture in patients with multiple sclerosis: the UK general practice research. J Bone Min Res. 2011;26:2271–2279. doi: 10.1002/jbmr.418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Matsuda PN, Shumway-Cook A, Ciol MA, Bombardier CH, Kartin DA. Understanding falls in multiple sclerosis: association of mobility status, concerns about falling, and accumulated impairments. Phys Ther. 2012;92:407–415. doi: 10.2522/ptj.20100380. [DOI] [PubMed] [Google Scholar]
- 7.Peterson EW, Cho CC, Finlayson ML. Fear of falling and associated activity curtailment among middle aged and older adults with multiple sclerosis. Mult Scler. 2007;13:1168–1175. doi: 10.1177/1352458507079260. [DOI] [PubMed] [Google Scholar]
- 8.Nilsagard Y, Lundholm C, Denison E, Gunnarsson LG. Predicting accidental falls in people with multiple sclerosis: a longitudinal study. Clin Rehabil. 2009;23:259–269. doi: 10.1177/0269215508095087. [DOI] [PubMed] [Google Scholar]
- 9.Finlayson M, Plow M, Cho C. Use of physical therapy services among middle-aged and older adults with multiple sclerosis. Phys Ther. 2010;90:1607–1618. doi: 10.2522/ptj.20100072. [DOI] [PubMed] [Google Scholar]
- 10.American Geriatrics Society, British Geriatrics Society, and American Academy of Orthopaedic Surgeons Panel on Falls Prevention. Guideline for the prevention of falls in older persons. J Am Geriatr Soc. 2001;49:664–672. [PubMed] [Google Scholar]
- 11.Oasis. Free From Falls. http://www.oasisnet.org/Network/Downloads/HealthPrograms.aspx. Updated 2006. Accessed April 14, 2014.
- 12.National Multiple Sclerosis Society. Free From Falls: A Comprehensive Fall Prevention Program for People with MS: Program Manual. New York, NY: National Multiple Sclerosis Society; 2013. [Google Scholar]
- 13.Finlayson M, Peterson EW, Cho C. Pilot study of a fall risk management program for middle aged and older adults with MS. NeuroRehabilitation. 2009;25:107–115. doi: 10.3233/NRE-2009-0505. [DOI] [PubMed] [Google Scholar]
- 14.Finlayson M, Cattaneo D, Cameron M et al. Applying the RE-AIM framework to inform the development of a multiple sclerosis falls-prevention intervention. Int J MS Care. 2014;16:192–197. doi: 10.7224/1537-2073.2014-055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cattaneo D, Jonsdottir J, Coote S. Targeting dynamic balance in falls-prevention interventions in multiple sclerosis: recommendations from the International MS Falls Prevention Research Network. Int J MS Care. 2014;16:198–202. doi: 10.7224/1537-2073.2014-062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cattaneo D, Regola A, Meotti M. Validity of six balance disorders scales in persons with multiple sclerosis. Disabil Rehabil. 2006;28:789–795. doi: 10.1080/09638280500404289. [DOI] [PubMed] [Google Scholar]
- 17.Cattaneo D, Jonsdottir J, Repetti S. Reliability of four scales on balance disorders in persons with multiple sclerosis. Disabil Rehabil. 2007;29:1920–1925. doi: 10.1080/09638280701191859. [DOI] [PubMed] [Google Scholar]
- 18.Nilsagard Y, Carling A, Forsberg A. Activities-specific balance confidence in people with multiple sclerosis. Mult Scler Int. 2012;2012:613925. doi: 10.1155/2012/613925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Learmonth YC, Paul L, Miller L, Mattison P, McFadyen AK. The effects of a 12-week leisure centre-based, group exercise intervention for people moderately affected with multiple sclerosis: a randomized controlled pilot study. Clin Rehabil. 2012;26:579–593. doi: 10.1177/0269215511423946. [DOI] [PubMed] [Google Scholar]
- 20.Mathias S, Nayak US, Isaacs B. Balance in elderly patients: the “Get-Up and Go” test. Arch Phys Med Rehabil. 1986;67:387–389. [PubMed] [Google Scholar]
- 21.Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go test. Phys Ther. 2000;80:896–903. [PubMed] [Google Scholar]
- 22.Kurtzke JF. Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS) Neurology. 1983;33:1444–1452. doi: 10.1212/wnl.33.11.1444. [DOI] [PubMed] [Google Scholar]
- 23.Nilsagard Y, Lundholm C, Gunnarsson LG, Denison E. Clinical relevance using timed walk tests and “timed up and go” testing in persons with multiple sclerosis. Physiother Res Int. 2007;12:105–114. doi: 10.1002/pri.358. [DOI] [PubMed] [Google Scholar]
- 24.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- 25.Nilsagard Y, Denison E, Gunnarsson LG, Bostrom K. Factors perceived as being related to accidental falls by persons with multiple sclerosis. Disabil Rehabil. 2009;31:1301–1310. doi: 10.1080/09638280802532639. [DOI] [PubMed] [Google Scholar]
- 26.Jackson K, Mulcare JA, Donahoe-Fillmore B, Fritz I, Rodgers MM. Home balance training intervention for people with multiple sclerosis. Int J MS Care. 2007;9:111–117. [Google Scholar]
- 27.Cattaneo D, Jonsdottir J, Zocchi M, Regola A. Effects of balance exercises on people with multiple sclerosis: a pilot study. Clin Rehabil. 2007;21:771–781. doi: 10.1177/0269215507077602. [DOI] [PubMed] [Google Scholar]
- 28.Cattaneo D, De Nuzzo C, Fascia T, Macalli M, Pisoni I, Cardini R. Risk of falls in subjects with multiple sclerosis. Arch Phys Med Rehabil. 2002;83:864–867. doi: 10.1053/apmr.2002.32825. [DOI] [PubMed] [Google Scholar]
- 29.Coote S, Hogan N, Franklin S. Falls in people with multiple sclerosis who use a walking aid: prevalence, factors, and effect of strength and balance interventions. Arch Phys Med Rehabil. 2013;94:616–621. doi: 10.1016/j.apmr.2012.10.020. [DOI] [PubMed] [Google Scholar]


